Abstract
Background:
Prosthetic joint infection (PJI) is the second most common cause for revision following hip hemiarthroplasty (HHA) resulting in a mortality rate of 5.6%. The treatment of PJI is both challenging and controversial, without general consensus on best practice. In an attempt to avoid surgery, patients are commonly prescribed antibiotics, reducing the chance of detecting a microorganism, and culture negative infections are reported to occur in up to 21% of all PJI. Two stage revision is arguably the gold standard treatment but frequently these patients are too frail to undergo such extensive procedures. Some surgeons have attempted to avoid this by leaving well fixed implants undisturbed, effectively performing a partial single-stage revision.
Case Presentation:
A previously well 83 -year-old female patient presented with a gradual onset of increasing pain and difficulty walking. Just over 1 year prior to this presentation she fell at home and underwent an uncomplicated bipolar hemiarthroplasty. Clinical examination as well as serological and radiological investigations were suspicious for a periprosthetic infection. Her rapidly deteriorating clinical picture required prompt surgical intervention. In theater the patient underwent a single stage partial exchange arthroplasty leaving the well cemented femoral stem undisturbed. Although multiple samples were taken, no microorganism was identified. The patient has been followed up for 1 year and remains well, with no recurrence of infection. Her inflammatory markers have returned to normal and radiographs demonstrate no evidence of loosening of the total hip replacement.
Conclusion:
The burden of infection following hip hemiarthroplasty is likely to parallel the predicted increase in hip fractures. The combination of physiologic frailty, osteoporosis and multiple medical comorbidities are pertinent factors for consideration in the development of a treatment strategy. A partial single stage revision THR performed by an experienced arthroplasty surgeon, along with expertly led antimicrobial therapy may be considered in carefully selected patients.
Keywords: hip hemiarthroplasty, single stage revision, culture negative, prosthetic joint infection, hip fracture
Introduction
The number of hip fractures worldwide was estimated to be 1.66 million in 1991 and is projected to increase to 6.26 million by 2050 of which approximately half will require hip hemiarthroplasty (HHA).1 Prosthetic joint infection (PJI) is one of the most feared complications following arthroplasty. The rate of prosthetic joint infection following hip hemiarthroplasty is estimated between 1.7 and 7.3%, with a mortality rate of 5.6%.2
The treatment of PJI following HHA can be challenging. Attempts at conservative surgery with debridement, antibiotics and implant retention (DAIR) have had poor results with up to 50% of cases becoming reinfected.3 A staged procedure is an option but this group of patients is often too frail to undergo multiple complex operations. The clinical picture is further complicated by the absence of an identified organism.
We present a case which illustrates the use of partial single-stage revision total hip arthroplasty to successfully treat culture negative (CN) PJI following a bipolar hemiarthroplasty in an octogenarian.
Case History
A previously well 83-year-old female patient sustained a displaced intracapsular fracture of her right hip after falling from a step ladder. She was admitted to the hospital and subsequently underwent an uncomplicated cemented bipolar hemiarthroplasty. Her post-operative recovery being uneventful, she was discharged home 3 days later. At the 2 week postoperative clinic appointment, her incision was well healed with no signs of infection, and she was referred for outpatient physical therapy. Her mobility improved with physical therapy, and at 6 weeks post-surgery she was walking pain-free using a walker. Radiographs of her hip were satisfactory Figure 1.
Figure 1.
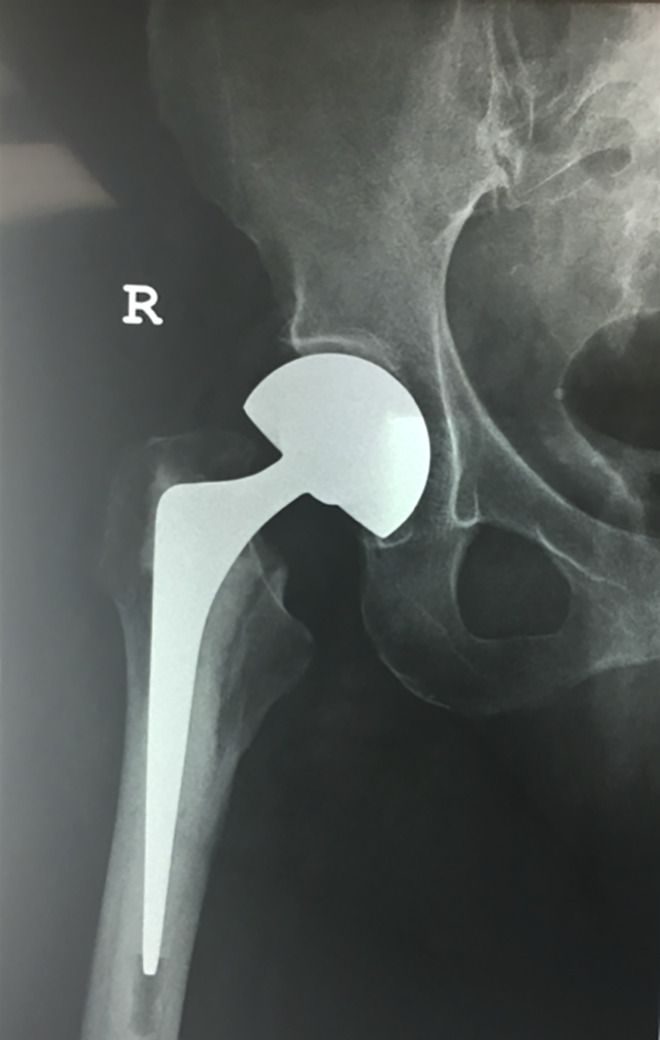
Initial post-operative AP radiograph demonstrating a satisfactory position of the bipolar hemiarthroplasty.
Thirteen months following surgery the patient presented to the clinic with a one-month history of severe right hip pain and difficulty mobilizing. Clinical examination revealed significant swelling, warmth and erythema over the surgical scar with painful limitation of all hip movements. Her white cell count was normal, 7.9 × 109 cells/mm3 (Range 4.0-11.0 × 109 cells/mm3), but the erythrocyte sedimentation rate (ESR) 69 mm (Range 0-22 mm) and C-reactive protein (CRP) 110 mg/dL (Range 0.010 -1.000mg/dL) were markedly raised. Radiographs of her hip revealed severe acetabular chondrolysis associated with a cystic lesion in zone 1 and lateral migration of the prosthesis, however the femoral stem appeared well fixed.4 Figure 2A & B The patient was treated with a nonsteroidal anti-inflammatory drug but no antibiotics were prescribed and she was asked to use a walker to offload the hip joint.
Figure 2.
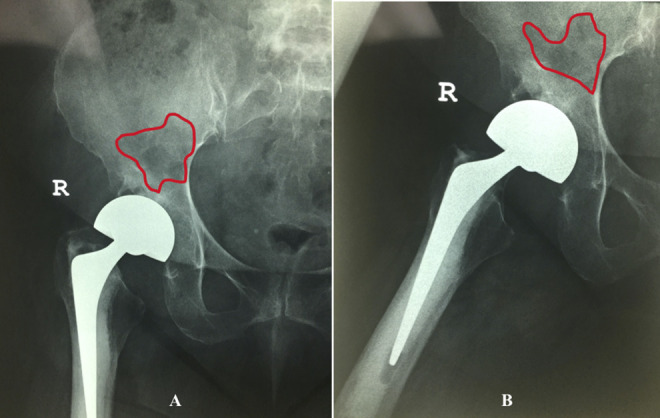
A & B AP and lateral radiographs showing extensive acetabular chondrolysis, with lateral migration of the prosthesis and anterolateral acetabular bone erosion. Note: Outline of lytic area in the ilium indicative of an abscess cavity.
Three days after presentation the patient began to exhibit signs of septicemia with worsening hip pain, and based on her clinical and laboratory findings, we were highly suspicious of a PJI . Following a discussion with the patient, she favored one operation if possible but left the final decision to the treating team.
The patient gave written consent for the use of her information and images in the submission of this report.
Surgical Procedure
Under a combined spinal-epidural anesthetic, a modified Hardinge surgical approach was used to enter the hip, taking care to identify all tissue layers. Under direct vision we aspirated the hip joint, obtaining 8 cc of cloudy synovial fluid which was leukocyte esterase test positive ++ using a URiSCAN Strip (YD Diagnostics, Rep. of Korea) with a white blood cell (WBC) count of 4500 /µL, 85% polymorphonuclear leukocytes (PMN).
A complete capsulectomy was performed followed by dislocation of the hip and removal of the bipolar femoral head. Gross inspection revealed no evidence of trunnionosis, and 6 tissue samples were sent for culture and sensitivity analysis. The femoral stem was found to be well fixed and we then turned our attention to the acetabulum.
Aggressive debridement of periprosthetic tissue was performed, including removal of extensive pulvinar from the acetabulum until the true floor was encountered. Careful inspection revealed a large cyst in the posterior-superior quadrant, which on probing exuded thick pus. The cyst cavity was thoroughly cleared using a series of curettes, followed by pulsatile lavage with 6 L of 0.9% sodium chloride. The surgical field was filled with dilute Betadine® solution 0.35% and left to soak for 5 minutes, then irrigated clear with 0.9% sodium chloride. The surgical field was dried, packed with gauze sponges and sealed with an antimicrobial drape. Contaminated drapes and instruments were removed, the entire surgical team rescrubbed and the patient was prepped for the second part of the operation.
The acetabulum was prepared using concentric reamers and trialing confirmed a good press fit. The acetabular cyst was dried and thoroughly packed with Copal G+V bone cement (Heraeus Medical, Germany) ensuring that cement did not protrude above the opening into the acetabulum as this would interfere with seating of the component. A multi-hole porous coated acetabular shell was implanted using 5 screws for additional fixation. A crossed-linked polyethylene (XLPE) liner was inserted and an Oxinium® femoral head impacted on to the stem after trialing to ensure stability and satisfactory range of movement. Two grams of vancomycin powder was spread within the deep tissues and the wound closed in layers using absorbable sutures.
Postoperatively the patient was placed on intravenous vancomycin and cefuroxime for 5 days. The initial report at 72 hours showed no growth from any of the intraoperative samples, and on advice from the infectious disease specialist, the patient was discharged on oral moxifloxacin and cefuroxime for an initial period of 6 weeks. The final microbiology report after 14 days confirmed that no organism was cultured from the samples.
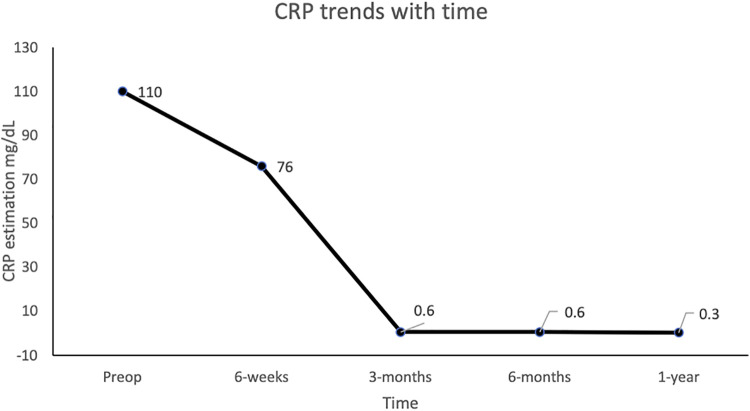
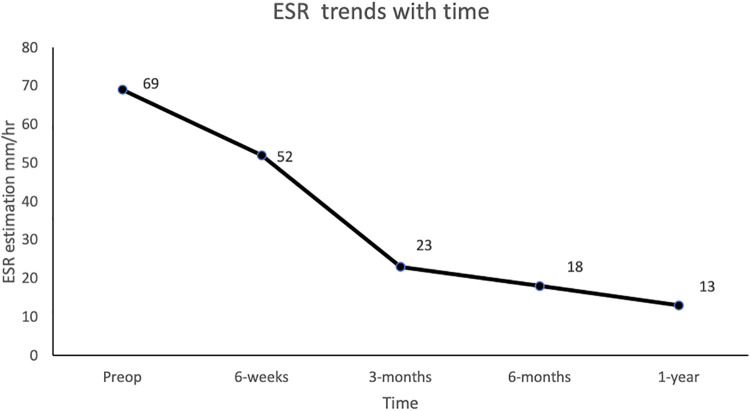
At 6 weeks post-surgery, there was marked clinical improvement with no evidence of infection, and the patient was walking using a cane. Both her CRP and ESR although elevated had fallen below the preoperative values and she was advised to continue for a further 6 weeks on the original antibiotic combination. All antibiotics were stopped at 3 months and serial CRP and ESR estimations were taken at 6 weeks, 3 months, 6 months and 1 year post surgery Figures 3 & 4.
Figure 3.
Graph of CRP changes over time.
Figure 4.
Graph of ESR changes over time.
At one year the patient reported minimal discomfort, she had an excellent range of hip movement and was walking with a mild trendelenburg gait. Her radiographs were satisfactory and her Oxford Hip Score (OHS) was 46, with an EQ-5D of 1.0. Figure 5A & B.
Figure 5.
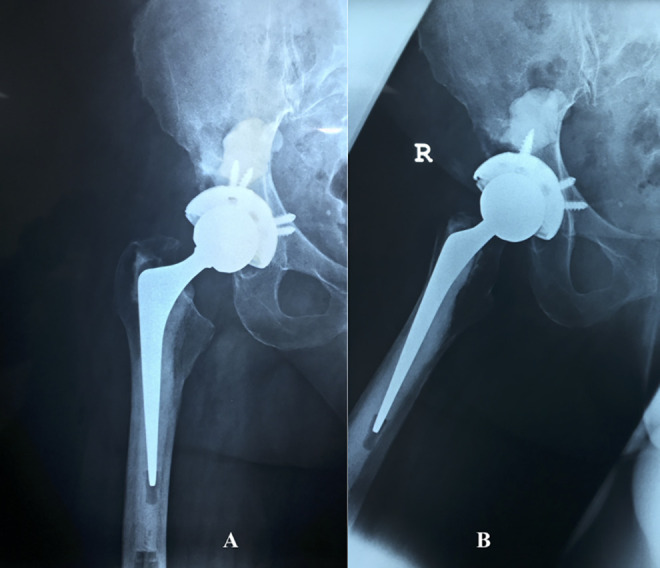
A & B AP and lateral radiographs following partial revision total hip arthroplasty demonstrates incomplete filling of the acetabular abscess cavity with bone cement, and multiple screws stabilizing the acetabular shell.
Discussion
Prosthetic joint infection is one of the most serious complications which can occur following hip arthroplasty. A previous study has suggested that the outcome of PJI in hip hemiarthroplasty (HHA) following a femoral neck fracture is worse than PJI developing after elective total hip arthroplasty (THA).5 Previous studies evaluating deep infection have pooled data from both THA and HHA, ignoring the distinctly different patient populations, which has resulted in conflicting results.6,7
Lora-Tamayo et al examined 210 cases of PJI (62 HHA and 148 THA) treated by debridement with antibiotics and implant retention (DAIR) and observed that there was a 37% failure rate. The overall and infection related mortality in HHA was greater than in THA (35% vs 13%, p = 0.004, 21% vs 4%, p = 0.005).5 Ferguson et al highlighted the poor clinical results in their review of 14 infected cases in 1428 HHAs over a 5-year period. Eight patients were treated by DAIR with a 50% failure rate, and 3 others underwent primary excision arthroplasty. Single stage THA was performed for 2 patients (one developed a recurrent infection) and in one patient no further surgery was needed. The 90-day mortality for this cohort of patients was 36%.3
A 2 stage exchange, long considered the gold standard management approach for PJI is currently being challenged by proponents of a single stage operation.5 One procedure is attractive option to most patients, and offers the advantage of comparable rates of infection control, compared with a 2-stage procedure with decreased morbidity, mortality and health care costs.8,9 In recent years, there has been an increasing amount of literature on single stage procedures, Thakrar et al reviewed the outcome of 962 patients in over 22 studies reporting a recurrent infection rate of between 0%-18%. They concluded that single-stage revision was an acceptable form of management of PJI in a selected patient cohort.10 These studies, although encouraging, however refer to PJI developing in an otherwise healthy group of patients following elective THA. The results therefore cannot be readily extrapolated to PJI following HHA, since we know that these patients have a different demographic and health profile than their elective counterparts.5 Although our patient was 83 years old, she had no medical co-morbidities and expressed a strong preference for a single stage procedure.
To date, there has been little conclusive evidence to guide surgeons in the treatment of an infected HHA. Studies suggest that there are specific risk factors for infection which are different for patients who undergo HHA versus THA.5 Furthermore, patients who undergo a HHA are often older with more medical comorbidities than patients undergoing THA and are less likely to tolerate a 2 stage exchange procedure.5 Conversely, these patients are also poor candidates for an extensive single stage exchange, in which removal of well-fixed implants can be challenging and associated with significant morbidity. An attractive but controversial option is highly selective implant retention, otherwise known as a partial one stage revision procedure. El-Husseiny et al showed a 83.3% (15/18) success rate using this technique to treat the infected total hip arthroplasty.11 In our patient, we found no evidence of trunnionosis, the femoral stem was well cemented and found to be stable during intraoperative testing, for these reasons it was left insitu.12
Baochao et al reported a 87.1% (27/31) success rate using partial single stage revision for the treatment of PJI in total hip arthroplasty.13 Culture negative infections have been reported to occur in 7% to 21% of all PJIs, and was the second largest group in this report, accounting for 22.6% of the cases.14-17 Surprisingly, the rate of reinfection was similar in cases in which the organism was identified preoperatively compared with CN infections (12.5% vs 14.2%).13 Notwithstanding the strong clinical evidence of infection, no microorganism was cultured in this case, and the diagnosis of PJI was therefore based on the 2018 definition of Periprosthetic Hip and Knee Infection by the Musculoskeletal Infection Society (MSIS).18 In a developing country, the rate of culture negative PJI is likely to be much higher than in the United States or Europe for several reasons, including widespread overuse of antibiotics together with the unavailability of advanced methods of microbial detection, and it is our anecdotal experience that this holds true for the Caribbean.
At one year following revision our patient remains asymptomatic, with normal inflammatory markers and no radiological evidence of implant loosening. Our use of a partial single stage revision THR in the presence of a culture-negative infection is controversial and we caution surgeons about its wide application where the outcome may not be as encouraging. Ongoing clinical trials should soon give us a definitive answer to the treatment of prosthetic joint infection following total hip arthroplasty, this may however not be applicable to the cohort of hip fracture patients who develop deep infections, which should be the subject of future research.19
Summary
The burden of infection following hip hemiarthroplasty is likely to parallel the predicted increase in hip fractures. This complication is associated with a high rate of morbidity and mortality in the elderly. The combination of physiologic frailty, osteoporosis and multiple medical comorbidities are pertinent factors for consideration in the development of a treatment strategy. A partial single stage revision THR performed by an experienced arthroplasty surgeon, along with expertly led antimicrobial therapy may be considered in carefully selected patients. Future randomized controlled trials investigating the outcome of surgically treated prosthetic joint infection following hip hemiarthroplasty are needed to validate the best treatment strategy.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Marlon M. Mencia, FRCS  https://orcid.org/0000-0003-4869-7479
https://orcid.org/0000-0003-4869-7479
References
- 1. Cooper C, Campion G, Melton LJ, 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2(6):285–289. doi:10.1007/bf01623184 [DOI] [PubMed] [Google Scholar]
- 2. Noailles T, Brulefert K, Chalopin A, Longis PM, Gouin F. What are the risk factors for post-operative infection after hip hemiarthroplasty? Systematic review of literature. Int orthop. 2016;40(9):1843–1848. doi:10.1007/s00264-015-3033-y [DOI] [PubMed] [Google Scholar]
- 3. Ferguson D, Jones S, Parker J, Aderinto J. Outcome of prosthetic infection following hip hemiarthroplasty surgery for intracapsular neck of femur fractures. Orthop Proc. 2013;95-B(Supp 1):91–91. doi:10.1302/1358-992x.95bsupp_1.Boa2012-091 [Google Scholar]
- 4. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;(121):20–32. [PubMed] [Google Scholar]
- 5. Lora-Tamayo J, Euba G, Ribera A, et al. Infected hip hemiarthroplasties and total hip arthroplasties: differential findings and prognosis. J Infect. 2013;67(6):536–544. doi:10.1016/j.jinf.2013.07.030 [DOI] [PubMed] [Google Scholar]
- 6. Cordero-Ampuero J, de Dios M. What are the risk factors for infection in hemiarthroplasties and total hip arthroplasties? Clin Orthop Relat Res. 2010;468(12):3268–3277. doi:10.1007/s11999-010-1411-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. del Toro MD, Nieto I, Guerrero F, et al. Are hip hemiarthroplasty and total hip arthroplasty infections different entities? The importance of hip fractures. Eur J Clin Microbiol Infect Dis. 2014;33(8):1439–1448. doi:10.1007/s10096-014-2091-1 [DOI] [PubMed] [Google Scholar]
- 8. Negus JJ, Gifford PB, Haddad FS. Single-stage revision arthroplasty for infection—an underutilized treatment strategy. J Arthroplasty. 2017;32(7):2051–2055. doi:10.1016/j.arth.2017.02.059 [DOI] [PubMed] [Google Scholar]
- 9. Rowan FE, Donaldson MJ, Pietrzak JR, Haddad FS. The role of one-stage exchange for prosthetic joint infection. Curr Rev Musculoskelet Med. 2018;11(3):370–379. doi:10.1007/s12178-018-9499-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Thakrar RR, Horriat S, Kayani B, Haddad FS. Indications for a single-stage exchange arthroplasty for chronic prosthetic joint infection: a systematic review. Bone Joint J. 2019;101-b(1_Supple_A):19–24. doi:10.1302/0301-620x.101b1.bjj-2018-0374.r1 [DOI] [PubMed] [Google Scholar]
- 11. El-Husseiny M, Haddad FS. The role of highly selective implant retention in the infected hip arthroplasty. Clin Orthop Relat Res. 2016;474(10):2157–2163. doi:10.1007/s11999-016-4936-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Barrack RL, Mulroy RD, Jr, Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review. J Bone Joint Surg Br. 1992;74(3):385–389. [DOI] [PubMed] [Google Scholar]
- 13. Ji B, Xu B, Guo W, et al. Retention of the well-fixed implant in the single-stage exchange for chronic infected total hip arthroplasty: an average of five years of follow-up. Int orthop. 2017;41(5):901–909. doi:10.1007/s00264-016-3291-3 [DOI] [PubMed] [Google Scholar]
- 14. Berbari EF, Marculescu C, Sia I, et al. Culture-negative prosthetic joint infection. Clin Infect Dis. 2007;45(9):1113–1119. doi:10.1086/522184 [DOI] [PubMed] [Google Scholar]
- 15. Malekzadeh D, Osmon DR, Lahr BD, Hanssen AD, Berbari EF. Prior use of antimicrobial therapy is a risk factor for culture-negative prosthetic joint infection. Clin Orthop Relat Res. 2010;468(8):2039–2045. doi:10.1007/s11999-010-1338-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ji B, Li G, Zhang X, Wang Y, Mu W, Cao L. Effective treatment of single-stage revision using intra-articular antibiotic infusion for culture-negative prosthetic joint infection. Bone Joint J. 2020;102-b(3):336–344. doi:10.1302/0301-620x.102b3.Bjj-2019-0820.R1 [DOI] [PubMed] [Google Scholar]
- 17. Aggarwal VK, Bakhshi H, Ecker NU, Parvizi J, Gehrke T, Kendoff D. Organism profile in periprosthetic joint infection: pathogens differ at two arthroplasty infection referral centers in Europe and in the United States. J Knee Surg. 2014;27(5):399–406. doi:10.1055/s-0033-1364102 [DOI] [PubMed] [Google Scholar]
- 18. Parvizi J, Tan TL, Goswami K, et al. The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplasty. 2018;33(5):1309–1314.e2. doi:10.1016/j.arth.2018.02.078 [DOI] [PubMed] [Google Scholar]
- 19. Strange S, Whitehouse MR, Beswick AD, et al. One-stage or two-stage revision surgery for prosthetic hip joint infection—the INFORM trial: a study protocol for a randomised controlled trial. Trials. 2016;17:90. doi:10.1186/s13063-016-1213-8 [DOI] [PMC free article] [PubMed] [Google Scholar]