Abstract
Introduction:
Pneumonia, thromboembolic and ischemic events, urinary tract infections (UTI), delirium and acute kidney injury (AKI) are common complications during the treatment of fragility fractures. In a 2 years-follow-up we determined the according incidence and risk factors of these and other complications in orthogeriatric inward patients, as well as the respective associated mortality.
Methods:
All patients treated on an orthogeriatric co-managed ward over the course of a year were included. Besides injury, therapy and geriatric assessment parameters, we evaluated the inward incidence of common complications. In a 2 years-follow-up the associated death rates were aquired. SPSS (IBM) was used to determine the importance of risk factors predisposing to the respective occurrence of a complication and accordingly determine it’s impact on the patients’ 1- and 2-years-mortality.
Results:
830 orthogeriatric patients were initially assessed with a remaining follow-up cohort of 661 (79.6%). We observed very few cases of thrombosis (0.6%), pulmonary embolism (0.5%), apoplex (0.5%) and myocardial infarction (0.8%). Pneumonia was seen in 42 (5.1%), UTI in 85 (10.2%), delirium in 186 (22.4%) and AKI in 91 (11.0%) patients. Consistently ADL on admission was found to be a relevant risk factor in the development of each complication. After adjustment only AKI showed a significant increased mortality risk of 1.60 (95%CI:1.086-2.350).
Discussion:
In our fracture-independent assessment of complications in the orthogeriatric treatment of inward patients we’ve seen very rare cases of cardiac and thrombotic complications. Typical fragility-fracture associated common events like pneumonia, UTI, delirium and AKI were still more incidental. No complication except AKI was associated to significant increased mortality risk.
Conclusions:
The relevance of orthogeriatric care in prevention and outcome of inward complications seems promising, needing still more controlled studies, evaluating not just hip fracture patients but more diverse groups. Consensus is needed in the scholar evaluation of orthogeriatric complications.
Keywords: orthogeriatric comanagement, fragility fractures, complication, mortality, risk factors, immobility, acute kidney injury, pneumonia, delirium
Introduction
Typical fragility fractures show increasing numbers as the general age of the worldwide population and especially the industrial nations’ rises.1-3 Common osteoporotic fractures as hip fractures, vertebral compression fractures and humeral fractures are associated to correlated morbidity and the incidence of complications.4 Those are often multifactorally caused by immobility, use of indwelling bladder catheters, surgical intervention and hypovolemia.5,6 Typical complications in the context of orthogeriatric treatment are pneumonia, urogenital infections, kidney failure, delirium, stroke, deep venous thrombosis and pulmonary embolism.7,8 There are several studies investigating the development of complications associated to hip fractures, but very few highlighting other fragility fracture types. Complication being a risk factor itself, its occurrence implicates a poorer outcome in terms of survival rate. Pneumonia was identified as a significant risk factor for increased mortality after hip fractures,9,10 whereas urogenital infections were not observed to influence survival in a negative way.7,11 The occurrence of acute kidney failure and the stage of preexisting chronic kidney failure also seem to correlate with higher mortality.12 Delirium and associated negative consequences such as falls and noncompliance are typical in the inpatient context too.13 In order to address comorbidities and complications, orthogeriatric treatment was widely established. Orthogeriatric care of injured old patients has been shown to have a positive influence on treatment’s outcome.14
The first aim of this investigation was to determine the incidence and associated risk factors of complications of inpatients during treatment on an orthogeriatric co-managed ward. Secondly in a 2-years follow-up, respective death rates were assessed in order to calculate the association between complications and mortality.
Methods
All inward patients treated on an orthogeriatric ward in the course of a year from February 2014 to January 2015 were assessed. Admission criteria were age >75 with typical comorbidities like impaired mobility and the necessity to use aids, dementia, acoustic and visual impairments, polypharmacy, frequent falling or sarcopenia. All patients suffered from different types of fragility fractures. There was a positive approval of the concerning institutional review board of the Bavarian state chamber of medicine on the performance of this study (Sign:7/11192). Informed consent of patients and relatives was achieved.
Data Assessment and Follow Up
Primary assessment variables were fracture type, reason for admission, therapy and the below mentioned complications in the course of the treatment. Follow up included a timeframe of 2 years from inward treatment. Patients were addressed through questionnaires by mail. In the case of no response, patients or relatives were called with a maximum of 5 attempts. If the patient had already deceased, the exact month of death was requested from the relatives by call. Consequently, not only 1- and 2-year-mortality, but also its course could be portrayed.
Data Analysis
SPSS (IBM) was used in our statistical analyses. We used T-tests for independent samples and the Chi square test (QST) to evaluate significant influence of the cofactors (stated below). Correlations and Odds ratios of potential risk factors were calculated. We used the Fisher’s exact test (FET) for discrimination of significant differences in mortality. The cox-regression was used to adjust and eliminate the confounding effect of the tested risk factors on mortality. Consequently, the adjusted Hazard ratio’s (HR) was calculated for each complication. In order to calculate the relative mortality risk of the cohort, we used the German statistical office’s mortality tables. The referred risks are stated as standardized mortality ratio (SMR).
Examined Complications
Patients that suffered from pneumonia, apoplexy, deep venous thrombosis, pulmonary embolism and urogenital infections were assessed when there was clinical and diagnostical evidence (X-rays, computed tomography, sonography, urinary samples) about the event in question. Delirium was assessed by clinical aspects as well as the Confusion Assessment method. All types of delirium from active, inactive to fluctuating were summarized.
We assessed acute kidney injury (AKI) by detection of increased creatinine levels and/ or anuria, oliguria and/or related lower limb edema. We did not differentiate between the 3 stages of AKI defined by the KDIGO.
The complications were checked in the initial total patient cohort.
Treatment
Every patient received orthogeriatric comanagement by both an orthopedic and a geriatric specialist. Patients attended daily physio- (twice) and ergotherapy. Fractures of the lower extremities generally underwent surgery, whereas fractures of the upper extremity were mostly addressed operatively (relation surgery/conservative: 5/1). Fractures of the spine were treated operatively to conservatively in a fifty-fifty ratio, the therapeutic decision depending on fracture morphology, clinical course, pain and course of radiographic changes. Rib fractures were treated conservatively. All patients were supported in finding support for their care after discharge. Those suffering from surgically treated spine fractures, lower extremity fractures and pelvic fractures received rehabilitation preferably in an inward setting. Upper extremity fracture patients were mostly advised for outward physiotherapy treatment.
Cofactors
We evaluated age, gender, type of fracture, Parker Mobility Score (PMS), Activities of daily living (ADL), Charlson-Comorbidity-Index (CCI), preexisting dementia and sarcopenia as influential factors on the occurrence and associated mortality of the investigated complications. The fractures were summed up into 2 groups: mostly immobilizing fractures of the lower extremity, pelvis and thoracolumbar spine and mostly non immobilizing fractures of the upper extremities, ribcage and cervical spine.
Results
Table 1 shows the general characteristics of our patients of which we assessed 830 over the course of a year with an average age of 84.5. Gender distribution displays a 3:1 ratio of women to men. The reason for admission is also listed in Table 1.
Table 1.
General Characteristics of the Total and Follow-Up Cohort.
| Total patient cohort | Follow-up cohort | ||
|---|---|---|---|
| Age | 84.5 | 84.6 | |
| Gender | male | 198 | 165 |
| female | 632 | 496 | |
| Injuries | Upper extremity | 119 | 97 |
| Lower extremity | 387 | 306 | |
| Spine | 105 | 85 | |
| pelvis | 45 | 34 | |
| Ribs | 24 | 19 | |
| Infections | 19 | 15 | |
| Multiple injuries | 60 | 44 | |
| Other injuries/causes of admission | 71 | 61 | |
| Immobilizing injury | 614 | 483 | |
| Non immobilizing injury | 216 | 178 | |
Due to loss-to follow up, we acquired follow-up data from 661 patients, resulting in a response rate of 79.6%. Table 1 also displays the general characteristics of our follow-up cohort, showing a mean age of 84.6.
Complication Rates
Overall, we found 5 (0.6%) events of thrombosis, 4 (0.5%) of pulmonary embolism (all of which occurring separately from thrombosis), 4 (0.5%) of stroke and 7 (0.8%) of acute coronary syndrome. We saw pneumonia in 42 (5.1%), urogenital infections in 85 (10.2%) and delirium in 186 (22.4%) cases. 91 (11.0%) patients developed an acute or acute on chronic kidney failure. Table 2 shows the total occurrence of complications and respective rates of the remaining patients in the follow up group. Figure 1 depicts the relative distribution of the occurred complications. Figure 2 shows their relative proportions in both fracture groups depending on immobilization. Table 3 illustrates gender, age and functional score distributions and Table 4 displays mortality values and statistical testing of the respective groups. Table 5 lists Odds-ratios for the development of the more prevalent complications in the presence of any risk factor.
Table 2.
Total Numbers of Observed Complications.
| Total patient cohort | Follow-up cohort | |
|---|---|---|
| Pneumonia | 42 | 34 (81.0%) |
| UTI | 85 | 60 (70.6%) |
| Delirium | 186 | 142 (76.3% |
| AKI | 91 | 76 (83.5%) |
| Thrombosis | 5 | 3 (60.0%) |
| Pulmonary embolism | 4 | 3 (75.0%) |
| Myocardial infarction | 7 | 4 (57.1%) |
| Apoplexy | 4 | 3 (75.0%) |
Figure 1.
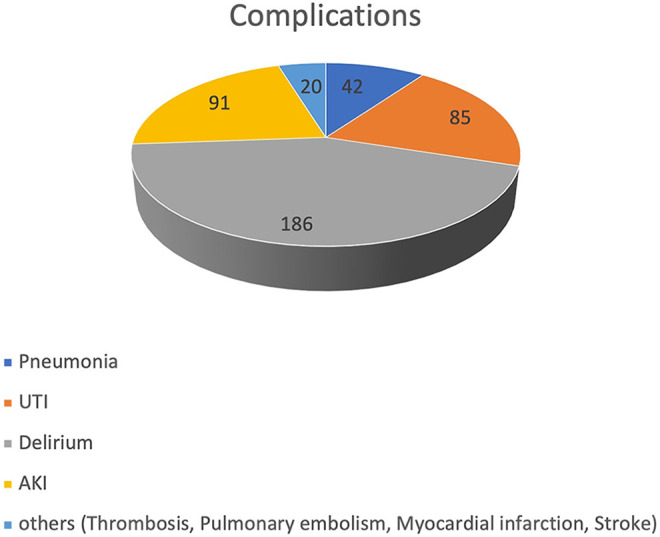
Distribution of observed complications 81x47mm (600 x 600 DPI).
Figure 2.
Distribution of complications among fracture types 152x88mm (600 x 600 DPI).
Table 3.
Age, Gender and Functional Score Distribution for each Complication.
| Age | Male | female | ADL | PMS | ||
|---|---|---|---|---|---|---|
| Pneumonia | no pneumonia | 84.55(84.09-85-01) | 181 | 607 | 26.55(25.33-27.76) | 5.25(5.06-5.44) |
| pneumonia | 84.24(82-12-86.35) | 17 | 25 | 18.86(15.30-22.45) | 4.26(3.30-5.22) | |
| UTI | no UTI | 84.44(83.97-84.91) | 186 | 559 | 26.72(25.47-27.96) | 5.22(5.02-5.42) |
| UTI | 85.33(83.87-86.79) | 12 | 73 | 21.14(17.78-24.49) | 5.03(4.36-5.69) | |
| Delirium | no delirium | 83.98(83.45-84.50) | 144 | 500 | 28.68(27.32-30.04) | 5.43(5.22-5.65) |
| delirium | 86.46(85.70-87.23) | 54 | 132 | 17.71(15.88-19.54) | 4.40(4.03-4.76) | |
| AKI | No AKI | 84.40(83.92-84.88) | 180 | 559 | 26.74(25.47-28.01) | 5.24(5.04-5.44) |
| AKI | 85.59(84.30-86.89) | 18 | 73 | 21.53(18.73-24.34) | 4.90(4.32-5.47) | |
Table 4.
1- and 2-year-Mortality for Each Complication Compared to Their Reference Group.
| p-values | |||||
|---|---|---|---|---|---|
| 1-year-mortality | 2-year-mortality | 1 year | 2 years | ||
| Pneumonia | no pneumonia | 26.6%(167/627) | 38.1%(239/627) | 0.435 | 0.476 |
| pneumonia | 32.4% (11/34) | 44.1%(15/34) | |||
| UTI | no UTI | 26.3%(158/601) | 37.1%(223/601) | 0.285 | 0.036 |
| UTI | 33.3% (20/60) | 51.7%(31/60) | |||
| Delirium | no delirium | 24.3%(126/519) | 34.3%(178/519) | 0.004 |
0.000 |
| delirium | 36.56%(52/142) | 53.5%(76/142) | |||
| AKI | No AKI | 25.0%(146/585) | 36.4%(213/585) | 0.006 | 0.002 |
| AKI | 42.1% (32/76) | 53.9%(41/76) | |||
Table 5.
Odds Ratios (OR) and p-Values Concerning the Displayed Risk Factors in the Development of the Respective Complication.
| Age | Gender | Immobilizing: Non Immobilizing fracture | ADL | PMS | Comorbidities | Dementia | Sarcopenia | |
|---|---|---|---|---|---|---|---|---|
| Pneumonia | p = 0.767 | male:female OR = 2.28(1.32-3.95) p = 0.015 |
OR:0.991(0.53-1.87) p = 1.000 |
p = 0.005 | p = 0.027 | OR = 1.11(0.59-2.09) p = 0.747 |
OR = 1.28(0.64-2.56) p = 0.588 |
OR = 1.01(0.54-1.89) p = 1.000) |
| UTI | p = 0.24 | Female:male OR = 2.02(1.08-3.81) p = 0.031 |
OR = 3.25(1.73-6.12) p = 0.000 |
p = 0.005 | p = 0.562 | OR = 1.22(0.77-1.92) p = 0.411) |
OR = 0.83(5.0-1.37) p = 0.531) |
OR = 1.09(0.74-1.62) p = 0.799) |
| Delirium | p = 0.000 | Male:female OR = 1.42 (0.98-2.05) p = 0.064 |
OR = 1.93(1.27-2.92) p = 0.002 |
p = 0.000 | p = 0.000 | OR = 1.14(0.81-1.59) p = 0.491 |
OR = 3.63(2.52-5.29) p = 0.000 |
OR = 1.46(1.02-2.09) p = 0.042 |
| AKI | p = 0.104 | Female:male OR = 1.31 (0.76-2.25) p = 0.364 |
OR = 2.79(1.58-4.92) p = 0.001 |
p = 0.001 | p = 0.272 | OR = 3.10(1.98-4.87) p = 0.000 |
OR = 0.79(0.49-1.29) p = 0.393 |
OR = 1.27(0.79-2.04) p = 0.328 |
Table 5 As age, PMS and ADL are continuous variables their differences in the respective complication group (complication occurring : complication not occurring) was evaluated with t-tests. For dichotomous risk factors odds ratios were calculated. This risk relation is stated respectively for gender and fracture type. Other relations: Comorbidities CCI≥4 : CCI ≤3, dementia: no dementia, sarcopnia : no sarcopenia.
Relative Mortality Risk
We included the complications pneumonia, kidney failure, urogenital infections, delirium to the cox regression analysis. Thrombosis, stroke, acute coronary syndrome and pulmonary embolism were excluded due to small incidences that would add a bias to the analysis. After adjustment only AKI was associated to an increased death risk of 1.60. The adjusted HR’s and SMR’s are displayed in Table 6.
Table 6.
Adjusted Hazard Ratio and Standardized Mortality Ratio Following Every Complication.
| HR | SMR | |
|---|---|---|
| (95%CI in brackets) | (95%CI in brackets) | |
| Pneumonia | 1.16 (0.627-2.161) | 2.56 (1.266-3.854) |
| UTI | 1.14 (0.712-1.812) | 2.76 (1.787-3.733) |
| Delirium | 1.36 (0.979-1.894) | 2.53 (1.962-3.098) |
| AKI | 1.60 (1.086-2.350) | 2.87(1.991-3.749) |
Pneumonia
We saw pneumonia in 42 (5.1%) cases. Age was not found to be a significant predictor of its development. Respectively more men suffered from pneumonia (Table 3). No significant influence was seen depending on fracture related immobility (p = 1.000), whereas ADL and PMS showed significant impact on the risk of developing pneumonia (Table 4). 1-and 2-year mortality was 32.4% (11/34) a.e. 44.1% (15/34). In contrast patients not suffering from pneumonia showed corresponding values of 26.6% (167/627) and 38.1% (239/627). There was no significant difference in mortality between both groups (Table 5). The adjusted HR was 1.16 (0.627-2.161 p = 0.630). The SMR was 2.56 (95%CI: 1.266-3.854)
Urinary Tract Infections
Urogenital infections were detected in 85 (10.2%) patients. Age did not show a relevant impact on their occurrence, whereas significantly more women suffered from UTI. Immobilizing fractures were also significantly correlated to the development of UTI (p = 0.000), as well as decreased ADL (Table 5). The associated 1- and 2-year mortality was 33.3% (20/60) and 51.7% (31/60). After 2 years the mortality was significantly higher for patients that developed a UTI. The adjusted HR was not significant being 1.14 (0.712-1.812 p = 0.592). The SMR showed a value of 2.76 (95%CI: 1.787-3.733)
Delirium
186 (22.4%) of our patients developed any form of delirium during the course of the treatment. They were significantly older than other patients (Table 3 & 5). Gender distribution was not significantly linked to the occurrence of delirium, but a preference of men was observed. Immobilizing fractures also showed a significant higher predisposition for delirium (p = 0.002). Lower ADL, mobility and the preexistence of dementia or sarcopenia were also significantly correlated to its occurrence (Table 5). 1- and 2-year-mortalitiy was significantly raised for patients suffering from delirium, showing values of 36.6% (52/142) and 53.5% (76/142), but after adjustment, the HR just showed an increased but not significant value of 1.36 (0.979-1.894 p = 0.066). The SMR was 2.53 (95%CI: 1.962-3.098)
Kidney Failure
91 (11.0%) patients developed acute kidney injury. No significant influence of age or gender was found in the distribution of patients with AKI. Immobilizing injuries significantly correlated with the occurrence of AKI (p = 0.000), as well as low ADL on admission and preexisting higher CCI. Both 1- and 2-year mortality of patients who developed AKI was significantly higher in contrast to those who did not, showing values of 42.1% and 53.9%. The adjusted HR was significant being 1.60 (1.086-2.350 p = 0.017). The SMR for AKI was 2.87(95%CI: 1.991-3.749).
Discussion
The goal of this study was to determine incidences and risk factors of common complications associated to inpatient orthogeriatric treatment of fragility fractures and their impact on the patients’ mortality. Data was assessed over the course of a year including 830 patients on a co-managed orthogeriatric ward. By including different fracture types, this investigation is different to the majority of existing studies concerning the topic, which were performed on hip fracture patients exclusively.8 Another difficulty in the comparison of studies evaluating complications in the orthogeriatric context is the missing consensus of the relevant highlighted complications.15
We observed very few numbers of thrombosis, pulmonary embolism, stroke and myocardial infarction, which did not predispose for a reasonable statistical analysis. Knobe et al. confirm our results by having seen a remarkable reduction in cardiorespiratory events in co-managed orthogeriatric inpatients compared to conventional traumatological treatment in a pilot study.16 We’ve seen delirium in every fifth, UTI and AKI in every tenth and pneumonia in every twentieth patient. In the univariate analysis UTI, delirium and AKI were associated to higher death-rates. After correction for confounding risk factors, AKI was the only complication followed by a significant higher mortality risk. All SMR’s showed more than twicely increased death risks by any complication compared to the age-adjusted healthy population.
We’ve found male gender, ADL and mobility as independent risk factors in the development of pneumonia. Its occurrence was independent from the immobilizing character of the fracture type. Roche et al. and Lv et al. describe male gender, age, number of comorbidities and preexisting respiratory disease as according risk factors.9,10 No significantly higher mortality was seen in patients suffering from pneumonia. This is contrary to the existing literature.9,10 A possible explanation is that the mentioned studies analyzed cohorts from 2000-201110 and 1999-2003.9 Being not specific about the treatment, these periods are prior to the implementation of orthogeriatric co-management, which could have been beneficial for patients in our investigation.
Besides mostly women suffering from UTI, main risk factors for its occurence were immobilizing fracture and reduced ADL. This seems plausible, using indwelling catheters more frequently in women and more prolonged in the context of immobilization and reduced capability of self-care. In a meta-analysis catheter use, its duration and female gender were main risk factors among others in the development of UTI.17 We found UTI to be associated with significantly higher mortality after 2 years of observation. This has not been reported in literature before. Hedström et al. and Hälleberg et al. detected no increased death rates after the occurrence of UTI in their hip fracture cohorts.7,18 We have yet seen a significant difference in survival in the late observation period, detecting none in the first year of follow up, which could have been caused by concurring confounding circumstances not necessarily associated to UTI. This assumption is supported by the adjusted HR not being significantly raised.
Delirium was prevalent frequently in our cohort, showing correlations with age, fracture type, impaired ADL, mobility, cognition and preexisting sarcopenia. Age, dementia and decreased functional status were consistently reported to be relevant risk factors in the development of delirium19 after hip fractures, also including acoustic and visual impairments, infections, comorbidities e.g. as renal failure, diabetes and Parkinson’s disease.13,20 Kim et al. described preoperative urinary catheter insertion and polymedication as independently associated to its occurrence.5 We detected a significant correlation of higher mortality rates in our patients suffering from delirium. This association is widely confirmed by Nightingale et al., de Jong et al. and Mitchell et al.19,21,22 Delirium being generally correlated to poorer health status, higher age, less cognition and predisposition to consequent injuries, it seems a legitimate indicator of higher susceptibility to earlier decease. Although after adjustment the HR was not significant, it was distinctly raised.
AKI was correlated with immobilizing injuries as well as lower ADL and more preexisting comorbidities measured by CCI. In association to the first mentioned, we must suppose that these fractures were more often treated surgically, and these surgeries were more often correlated with higher loss in volume than those addressing non-immobilizing fractures. Ulucay et al. detected lower glomerular filtration rate as an according independent risk factor, whereas Bennet et al. found male sex, vascular diseases, hypertension, diabetes, chronic kidney disease and use of nephrotoxic medication to be independently correlated to AKI following hip fractures.23,24 This applies to our analysis as comorbidity-associated risk factors mentioned by Bennet et al. like preexisting chronic kidney disease and diabetes are covered by the CCI. In patients suffering from AKI we’ve seen significantly increased mortality even after correction for confounders. We did not differentiate between the 3 KDIGO stages of AKI and therefore a stage-dependent risk stratification could not be delivered. Pedersen et al. examined a cohort of over 10000 patients suffering from hip fractures for the incidence of AKI, which was found to be 12.7%. The associated death rate was increased showing a 1-year-mortality of 25% and it correlated with the according KDIGO stage.25
The orthogeriatric approach is promising regarding the management and prophylaxis of fragility fracture-associated complications. However, studies have shown sobering results, Kusen et al. and Abrahamsen et al. found no significant reduction in complication rates comparing orthogeriatric to conventional care.14,26 Knobe et al. showed distinct insignificant reductions in cardio-respiratory complications in their orthogeriatric cohort, which is similar to our observation of very low rates of pulmonary embolism, myocardial infarction and stroke.16
We could examine an entire orthogeriatric cohort over the course of a year, deliver complication rates and determine relevant risk factors, as well as the associated 1- and 2-year-mortality. We examined the entirety of fragility fracture entities treated on an orthogeriatric ward, which is unique compared to the existing studies mainly performed on patients suffering from hip fractures.
Limitations
This study was not performed in comparison to a conventionally treated control group, we could therefore not measure the effect of orthogeriatric treatment on the complication rate. Our cohort might be too inhomogeneous for a detailed comparison to other study samples, especially having included different types of injuries. We tried to assess the main relevant complications in the context of fragility fractures, due to the missing consensus as mentioned above, there is a wide variety of risk factors and observed complications in literature, that we did not cover in its completeness. We also missed out in differentiation of AKI stages and different types of delirium for a more detailed stratification.
Conclusion
Pneumonia, UTI, delirium and AKI are relevant complications occuring in the treatment of fragility fractures. We could find ADL on admission to be throughout a significant risk factor. AKI had a significant, delirium a distinct but not significant impact on mortality after correction for confounders in our analyses. We observed very low rates of thrombosis, pulmonary embolism, myocardial infarction and stroke. The importance of orthogeriatric care in the prevention and treatment of complications has still to be evaluated, showing reduction of incidences but not yet delivering significant results. Finally, consensus must be found in determining which specific complications should be systematically evaluated in the scholar assessment of orthogeriatric outcome.
Availability of Data and Material
All data and material are transparent and can be accessible on request.
Consent for Publication
Patients and relatives gave informed consent for publication.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics Approval: Positive Approval by the concerning state chamber of medicine (Sign: 7/11192).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Andreas Wiedl, Dr med  https://orcid.org/0000-0002-3363-9068
https://orcid.org/0000-0002-3363-9068
References
- 1. Friedman SM, Mendelson DA. Epidemiology of fragility fractures, Vol. 30. Clin Geriatr Med. 2014;30(2):175–181. [DOI] [PubMed] [Google Scholar]
- 2. Hernlund E, Svedbom A, Ivergård M, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2013;8(1-2):136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cooper C, Atkinson EJ, Jacobsen SJ, O’fallon WM, Melton LJ. Population-based study of survival after osteoporotic fractures. Am J Epidemiol. 1993;137(9):1001–1005. [DOI] [PubMed] [Google Scholar]
- 4. Prieto-Alhambra D, Reyes C, Sainz MS, et al. In-hospital care, complications, and 4-month mortality following a hip or proximal femur fracture: the Spanish registry of osteoporotic femur fractures prospective cohort study. Arch Osteoporos. 2018;13(1):96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kim JY, Yoo JH, Kim E, et al. Risk factors and clinical outcomes of delirium in osteoporotic hip fractures. J Orthop Surg. 2017;25(3):2309499017739485. [DOI] [PubMed] [Google Scholar]
- 6. Sheehan KJ, Guerrero EM, Tainter D, et al. Prognostic factors of in-hospital complications after hip fracture surgery: a scoping review, Vol 30. Osteoporos Int. 2019;30(7):1339–1351. [DOI] [PubMed] [Google Scholar]
- 7. Hälleberg Nyman M, Johansson JE, Persson K, Gustafsson M. A prospective study of nosocomial urinary tract infection in hip fracture patients. J Clin Nurs. 2011;20(17-18):2531–2539. [DOI] [PubMed] [Google Scholar]
- 8. Folbert EC, Hegeman JH, Gierveld R, et al. Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch Orthop Trauma Surg. 2017;137(4):507–515. [DOI] [PubMed] [Google Scholar]
- 9. Roche JJW. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ [Internet]. 2005;331(7529):1374–1380. Updated August 15, 2020. Accessed August 15, 2020. http://www.bmj.com/cgi/doi/10.1136/bmj.38643.663843.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lv H, Yin P, Long A, et al. Clinical characteristics and risk factors of postoperative pneumonia after hip fracture surgery: a prospective cohort study. Osteoporos Int. 2016;27(10):3001–3009. [DOI] [PubMed] [Google Scholar]
- 11. Bliemel C, Buecking B, Hack J, et al. Urinary tract infection in patients with hip fracture: an underestimated event? Geriatr Gerontol Int. 2017;17(12):2369–2375. [DOI] [PubMed] [Google Scholar]
- 12. Porter CJ, Moppett IK, Juurlink I, Nightingale J, Moran CG, Devonald MAJ. Acute and chronic kidney disease in elderly patients with hip fracture: prevalence, risk factors and outcome with development and validation of a risk prediction model for acute kidney injury. BMC Nephrol. 2017;18(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rizk P, Morris W, Oladeji P, Huo M. Review of postoperative delirium in geriatric patients undergoing hip surgery. Geriatr Orthop Surg Rehabil. 2016;7(2):100–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Abrahamsen C, Nørgaard B, Draborg E, Nielsen MF. The impact of an orthogeriatric intervention in patients with fragility fractures: a cohort study. BMC Geriatr. 2019;19(1):268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liem ISL, Kammerlander C, Suhm N, Kates SL, Blauth M. Literature review of outcome parameters used in studies of geriatric fracture centers, Vol. 134. Arch Orthop Trauma Surg. 2014;132(2):181–187. [DOI] [PubMed] [Google Scholar]
- 16. Knobe M, Böttcher B, Coburn M, et al. Geriatric trauma center DGU®: evaluation of clinical and economic parameters: a pilot study in a German university hospital. Unfallchirurg. 2019;122(2):134–146. [DOI] [PubMed] [Google Scholar]
- 17. Li F, Song M, Xu L, Deng B, Zhu S, Li X. Risk factors for catheter-associated urinary tract infection among hospitalized patients: a systematic review and meta-analysis of observational studies, Vol. 75. J Adv Nur. 2019;75(3):517–527. [DOI] [PubMed] [Google Scholar]
- 18. Hedström M, Gröndal L, Ahl T. Urinary tract infection in patients with hip fractures. Injury. 1999;30(5):341–343. [DOI] [PubMed] [Google Scholar]
- 19. Mitchell R, Harvey L, Brodaty H, Draper B, Close J. One-year mortality after hip fracture in older individuals: the effects of delirium and dementia. Arch Gerontol Geriatr. 2017;72:135–141. [DOI] [PubMed] [Google Scholar]
- 20. Smith TO, Cooper A, Peryer G, Griffiths R, Fox C, Cross J. Factors predicting incidence of post-operative delirium in older people following hip fracture surgery: a systematic review and meta-analysis, Vol. 32. Int J Geriatr Psychiatry. 2017;32(4):386–396. [DOI] [PubMed] [Google Scholar]
- 21. Nightingale S, Holmes J, Mason J, House A. Psychiatric illness and mortality after hip fracture. Lancet. 2001;357(9264):1264–1265. [DOI] [PubMed] [Google Scholar]
- 22. de Jong L, van Rijckevorsel VAJIM, Raats JW, Klem TMAL, Kuijper TM, Roukema GR. Delirium after hip hemiarthroplasty for proximal femoral fractures in elderly patients: Risk factors and clinical outcomes. Clin Interv Aging. 2019;14:427–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ulucay C, Eren Z, Kaspar EC, et al. Risk factors for acute kidney injury after hip fracture surgery in the elderly individuals. Geriatr Orthop Surg Rehabil. 2012;3(4):150–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bennet SJ, Berry OMB, Goddard J, Keating JF. Acute renal dysfunction following hip fracture. Injury. 2010;41(4):335–338. [DOI] [PubMed] [Google Scholar]
- 25. Pedersen AB, Christiansen CF, Gammelager H, Kahlert J, Sorensen HT. Risk of acute renal failure and mortality after surgery for a fracture of the hip: a population-based cohort study. Bone Jt J. 2016;98-B(8):1112–1118. [DOI] [PubMed] [Google Scholar]
- 26. Kusen JQ, Schafroth B, Poblete B, et al. The implementation of a Geriatric Fracture Centre for hip fractures to reduce mortality and morbidity: an observational study. Arch Orthop Trauma Surg. 2019;139(12):1705–1712. [DOI] [PubMed] [Google Scholar]



