Abstract
Background
Ambient nitrogen dioxide (NO2) is a common air pollutant in developing countries and causes skin conditions, but its effect on eczema in subtropical areas is not clear in China.
Object
To measure the effect of short-term exposure of NO2 on the incidence of eczema and the change of outpatient visits.
Methods
Data of daily temperature, air pollutants, and outpatient visits from 2013 to 2018 were collected in a row. The generalized additive model (GAM) and Poisson distribution were used to assess the association between short-term exposure of NO2 and the outpatient visits of patients with eczema. The cumulative exposure effect of lag 0–3 days and the displacement effect of NO2 and other pollutants were considered as well. A single pollutant model was used to examine the independent association, and a two-pollutant model was adopted to control the confounding effect.
Results
The daily outpatient visits of eczema increased from 75.26 to 190.85 from 2013 to 2018 (P < 0.001). The combined influence of NO2 and the related pollutant exerted a stronger influence on the incidence of eczema. The maximum effect of NO2 appeared on the exposed day.
(lag 0) and disappeared on day 4 (lag 3). The children and seniors were more vulnerable to NO2 exposure.
Conclusion
Exposure to NO2 is tightly associated with eczema incidence and outpatient visits. The hospitals should react to the visit fluctuations and adjust physician duty shifts to improve outpatient service efficiency.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-021-10549-7.
Keywords: Eczema, NO2, Outpatient visits, Management
Introduction
Eczema, or atopic dermatitis, is a chronic, relapsing, and severely pruritic skin disorder [1]. It is a common condition at any age, affecting approximately 10–20% of children, and 2–18% of adults worldwide [2]. The prevalence of eczema has been increasing, mostly prevalent in industrialized countries, and closely followed by the developing countries [3]. Eczema has a significant impact on the quality of life and has been increasingly considered a public health problem [4]. The possible causes of eczema include genes, dry skin, immune system or mental problems, and the most important—triggers in the environment, such as low humidity, heat, sweating, as well as air pollutants [5].
The recent studies have just expanded to the influence of nitrogen dioxide (NO2) on eczema incidence. NO2 is a toxic reddish-brown gas, a strong oxidizing agent and common atmospheric pollutant that is produced by combustion, as of fossil fuels, car exhaust, smog, and cigarettes. Since the concentration of NO2 is tightly related to industry development, manufacturing, and transportation, it is a common air pollutant in developing countries and regions that pursue industrialization [6]. The inhale of NO2 damages the respiratory system, and the skin exposure also damages skin integrity and makes eczema happen [7]. The association of ambient air pollution, meteorological factors, and outpatient visits for eczema has been studied in some limited regions in China, such as Shanghai [8]. Currently, there has not any research done in the southeastern subtropical Guangdong Province. The climate is very different between Guangdong in the subtropical zone and Shanghai the temperate zones. In addition, the pollution control measures implemented by the Chinese government has significantly changed the air pollution distribution since 2015. It requires update data to illustrate the new changes.
Eczema, as a common but relapsing condition, has a comparatively stable and repeated “diagnosis—treatment—follow-up—education—readmission” treatment process [9]. If the ambient NO2 is associated with the increased eczema incidence, there may accompany the burst of outpatient visits. It may cause over-crowding at hospital outpatient and emergency departments (OEDs), and require on the outpatient service process arrangement and physician’s on-duty shifts [10]. If the hospital can react to the change of weather and air pollutants, it will improve both the efficiency and patient satisfaction. The study is to discuss how the findings could be used in the management of eczema patients in the outpatient department as well.
Methods and materials
Study setting
Guangdong Province is located in Southeastern China, with latitude 23.02 N, and longitude113.75E. It has a humid subtropical to tropical climate with an annual average temperature of 22 °C (72 °F) and sharp seasonal change of humidity from over 95% in summer to lower than 40% in winter. Guangzhou city, the capital of Guangdong province, locates in the geometrical center of the province, has the typical climate characteristics. Meanwhile, as the local industry and trade center, it suffers the heaviest air pollution. There lacks evidence of how the weather and air pollution affect the prevalence of eczema in Guangdong province.
The study site, Guangdong Dermatology Hospital, is the only provincial-level research center on dermatology in Guangdong province as well as tertiary-level teaching hospital affiliated to Southern Medical University. The hospital is located in Guangzhou City, but it provides outpatient care to patients from the whole province.
Data
We obtained data of daily outpatient visits from Guangdong Dermatology Hospital. Patients who were diagnosed with eczema (IDC-10 code L30.902) were included from January 18, 2013, to December 31, 2018. If the same patient re-visit the outpatient department after the first diagnosed eczema within 21 days, we defined the series of visits as one single visit in accord with the insurance policy.
We included 5 pollutants adopted in this research: NO2, sulfur dioxide (SO2), particulate matter no greater than 10 μm (PM10), particulate matter no greater than 2.5 μm (PM2.5), and daily maximum 8-h ozone (O3). The daily average concentrations of air pollutants were obtained from the public sharing system of Guangzhou Environmental Monitoring Center (http://112.94.64.160:8023/gzaqi_new/RealTimeDate.html). The system synthesized data from 11 national air quality monitoring stations in Guangzhou city, and took the average of all monitoring values. The daily relative humidity and temperature data were obtained from the China Meteorological Data Sharing Service System. The air pollution and meteorology data followed the quality control programs which were mandated by the Chinese government.
The air pollution and meteorological data were ranged from January 18, 2013, to December 31, 2018. Data sources are public and widely used in related studies [11].
Statistical methods
The generalized additive model (GAM) and Poisson distribution were used to assess the association between short-term exposure of NO2 and the outpatient visit of patients with eczema. The cumulative exposure effect of lag 0–3 days, and the displacement effect of NO2 and other pollutants were considered as well.
The single pollutant model was used to examine the independent association, and the two-pollutant model was adopted to control the confounding effect of the other pollutants. The model was expressed as follows:
where mt is the expected eczema outpatients on day t; is the intercept; Xt is the concentrations of pollutant (NO2, SO2, PM2.5, PM10, and O3) with i = 1 in single pollutant model and 2 in two pollutants model respectively; bi stands for the coefficient for Xi. A natural cubic spline function (NS) with three degrees of freedom (df) were applied for temperature and humidity to capture the nonlinear relationships of time trend [12]. An NS with 10 df per year is used for calendar time to adjust for long-term trend and seasonality [13]. Day of week (DOWt) was set in the form of categorical variables in the model, and γ is the effect of DOWt on eczema outpatients [14].
Besides, we conducted stratification analyses by potential individual-level effect modifiers, including gender and age (< 12 years, ≥12 years and < 65 years, ≥65 years) using the above basic models. To find the best degree of freedom used in the above model, the Akaike information criterion for quasi-Poisson (Q-AIC) was employed in the assessment of the goodness of model fits among 3–10 (per year) df for temperature, humidity, and time respectively [13, 15]. The minimum value of Q-AIC represented the best goodness and the optimum df. We also conducted sensitivity analyses to check the robustness of our modeling strategies by changing the df for temperature (2–4), humidity (2–4), and calendar time (9–11 per year) to control the time trend. We excluded holiday effect since there is no holiday breaks in the study hospitals and the number of patient visits was similar between weekdays and holidays.
R software version 4.0.2 was used to conduct all the analyses. P-value < 0.05 was considered to be statistically significant for all statistical tests.
Results
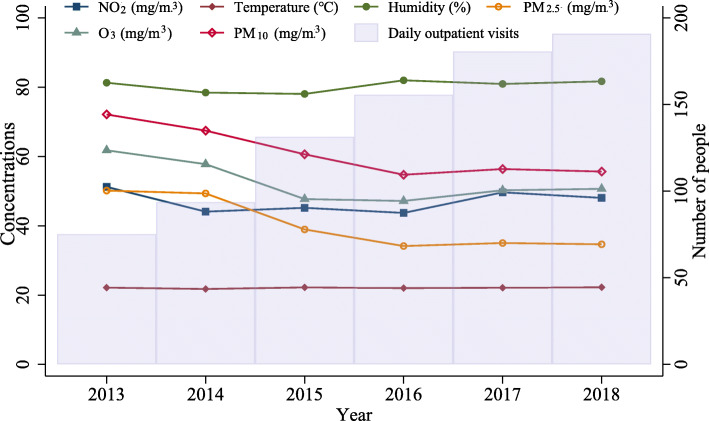
The average concentration of pollutants varied during the time: the concentration of NO2, O3, and PM10 decreased from 2013 to 2016, but increased from 2017 to 2018; while PM2.5 and SO2 kept decreasing from 2013 to 2018, indicating a significant improvement in air quality. The humidity ranged from 78.057 ± 8.907% in 2015 to 81.991 ± 9.698 in 2016 (P < 0.001), but the average ambient temperature was stable around 22 °C (P = 0.905), and the comparative humidity fluctuated around 80% (p < 0.001) in the 6 years. (Fig. 1) The daily outpatient visits for eczema increased significantly from 75.26 in 2013 to 190.85 in 2018 (P < 0.001). There were more male patients than female, and the trend is kept over time (P < 0.001). The majority of patients were aged 12–65 from 2013 to 2018 (P < 0.001). (Table 1).
Fig. 1.
The distribution of air pollutants, temperature, and relative humidity in Guangzhou city, 2013–2018
Table 1.
The daily outpatient visits for eczema, age and gender distribution: in Guangdong Dermatology Hospital, 2013–2018
| 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | F/ χ2 | P | |
|---|---|---|---|---|---|---|---|---|
| Daily outpatient visits | 75.261 ± 23.840 | 93.688 ± 31.839 | 131.406 ± 37.233 | 155.644 ± 43.374 | 180.638 ± 48.581 | 190.845 ± 48.430 | 478.389 | <.001 |
| Sex | ||||||||
| Male | 13,315 (9.0%) | 17,361 (11.8%) | 22,967 (15.6%) | 27,441 (18.6%) | 32,839 (22.2%) | 33,709 (22.8%) | 49.927 | <.001 |
| Female | 12,349 (8.5%) | 16,553 (11.4%) | 23,025 (15.8%) | 27,190 (18.7%) | 32,551 (22.3%) | 34,040 (23.4%) | ||
| Age | 41.530 ± 21.170 | 42.166 ± 21.059 | 42.948 ± 20.796 | 42.134 ± 20.732 | 41.772 ± 21.107 | 41.684 ± 20.946 | 26.794 | <.001 |
| < 12 | 2179 (9.0%) | 2769 (11.4%) | 3509 (14.5%) | 4388 (18.1%) | 5754 (23.8%) | 5587 (23.1%) | 89.416 | <.001 |
| 12–65 | 18,039 (8.8%) | 23,806 (11.6%) | 32,127 (15.6%) | 38,347 (18.6%) | 45,546 (22.1%) | 47,942 (23.3%) | ||
| > 65 | 5446 (8.6%) | 7340 (11.6%) | 10,356 (16.3%) | 11,896 (18.8%) | 14,091 (22.2%) | 14,221 (22.4%) | ||
The concentration of NO2 was negatively related to the temperature but positively related to the concentration of PM2.5, O3, PM10, and SO2 (Table 2). The highest correlation was found between NO2 and PM2.5 and PM10 (Pearson correlation 0.73, 0.8, P < 0.001).
Table 2.
The linear correlation of NO2 and temperature, relative humidity and air pollutants by Pearson analysis
| Temperature | Humidity | PM2.5 | O3 | PM10 | SO2 | NO2 | CO | |
|---|---|---|---|---|---|---|---|---|
| Temperature | – | 0.31** | −0.32** | 0.20** | −0.24** | − 0.15** | − 0.27** | − 0.15** |
| Humidity | – | – | −0.22** | −0.41** | − 0.26** | −0.17** | 0.02 | −0.00 |
| PM2.5 | – | – | – | 0.31** | 0.94** | 0.60** | 0.73** | 0.18** |
| O3 | – | – | – | – | 0.35** | 0.26** | 0.11** | 0.00 |
| PM10 | – | – | – | – | – | 0.44** | 0.80** | −0.05* |
| SO2 | – | – | – | – | – | – | 0.27** | 0.68** |
| NO2 | – | – | – | – | – | – | – | −0.14** |
*p-value < 0.05, **p-value < 0.0001
The smallest Q-AIC was observed in 3, 3, 10 per year df for temperature, relative humidity, and time respectively. Table 3 reported the lag nonlinear model analysis for NO2. The maximum effect of NO2 was at lag 0 day. Every 10 μg/m3 increase of NO2 was associated with a 4.10 percentage (95%CI, 3.80–4.40%) increase of eczema outpatients. The risk decreased gradually from 3.31% (95%CI, 2.99–3.64%) in lag 1 day to 1.64% (95%CI, 1.33–1.95%) in lag 2 day, and then faded away in lag 3 day.
Table 3.
The RR and PC of eczema risk associated with 10 mg/m3 increase of NO2
| Pollutant (per 10 μg/m3) | Lag Day | RR | PC (%) | P-value |
|---|---|---|---|---|
| NO2 | Lag 0 | 1.0410 (1.0380–1.0440) | 4.10 (3.80–4.40) | <.001 |
| Lag 1 | 1.0331 (1.0299–1.0364) | 3.31 (2.99–3.64) | <.001 | |
| Lag 2 | 1.0164 (1.0133–1.0195) | 1.64 (1.33–1.95) | <.001 | |
| Lag 3 | 1.0057 (1.0027–1.0087) | 0.57 (0.27–0.87) | 0.056 |
Note: PC refers to percentage change
The combined influence of NO2 and the other related pollutant exert a stronger influence on the incidence of eczema. The combination with SO2, O3, PM10 and PM2.5 lead to 4.26% (3.9–4.62), 2.04%(1.85–2.23), 1.75% (1.58–1.92), and 2.01% (1.8–2.23) increase of eczema outpatient visits (Table 4). (P < 0.001 for all).
Table 4.
The RR and PC of eczema risk associated with 10 μg/m3 increase of NO2 under a two-pollutant model
| Pollutant (per 10 μg/m3) |
Model type | RR | PC (%) | P-value |
|---|---|---|---|---|
| NO2 | NO2 + SO2 | 1.0426 (1.039–1.0462) | 4.26 (3.9–4.62) | <.001 |
| NO2 + O3 | 1.0204 (1.0185–1.0223) | 2.04 (1.85–2.23) | <.001 | |
| NO2 + PM10 | 1.0175 (1.0158–1.0192) | 1.75 (1.58–1.92) | <.001 | |
| NO2 + PM2.5 | 1.0201 (1.018–1.0223) | 2.01 (1.8–2.23) | <.001 |
Note: PC refers to the percentage change
The short-term exposure of NO2 exerted different influences on patients of different gender and age. The exposure was associated with increased outpatient visits for both male and female for 3 days from lag 0 day to lag 2 day, with PC 4.14(3.83–4.46) to 1.59(1.25–1.92) for male and 4.03(3.7–4.36) to 1.67(1.33–2.02 for female (P < 0.001). The children aged< 12 reported the highest risk in the lag 0 day and lag 1 day PC [7.22% (6.62–7.81), 5.05% (4.41–5.7%), P < 0.001], followed by seniors ≥65 years [4.93(4.46–5.41), 3.69(3.16–4.21), P < 0.001]. (Table 5).
Table 5.
Stratification analysis of the percent change of eczema risk associated with 10 mg/m3 increase of NO2
| Male | Female | < 12 | 12–65 | ≥65 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
Pollutant (per 10 μg/m3) |
Lag Day | PC (%) | P-value | PC (%) | P-valu | PC (%) | P-valu | PC (%) | P-valu | PC (%) | P-valu |
| NO2 | Lag 0 | 4.14 (3.83–4.46) | <.001 | 4.03 (3.7–4.36) | <.001 | 7.22 (6.62–7.81) | <.001 | 3.54 (3.24–3.84) | <.001 | 4.93 (4.46–5.41) | <.001 |
| Lag 1 | 3.35 (3.01–3.7) | <.001 | 3.23 (2.87–3.59) | <.001 | 5.05 (4.41–5.7) | <.001 | 2.96 (2.64–3.28) | <.001 | 3.69 (3.16–4.21) | <.001 | |
| Lag 2 | 1.59 (1.25–1.92) | <.001 | 1.67 (1.33–2.02) | <.001 | 1.1 (0.49–1.71) | 0.07 | 1.62 (1.31–1.93) | <.001 | 1.64 (1.14–2.14) | 0.001 | |
| Lag 3 | 0.4 (0.09–0.72) | 0.201 | 0.73 (0.4–1.05) | 0.027 | −1.13(− 1.7 - -0.56) | 0.05 | 0.64 (0.35–0.94) | 0.029 | 0.86 (0.39–1.35) | 0.071 |
Note: PC refers to the percentage change
The effect of combinations of pollutants were reported in Table 6. The combination of NO2 and SO2 reported the highest effect than other combination for all age and gender groups, and was followed by the combination with PM2.5, PM10 and O3. The female group reported slightly higher PC than male group, and the children aged< 12 and the senior aged≥65 reported higher PC than those aged 12–65.
Table 6.
Stratification analysis of the percent change of exposure risk associated with 10 mg/m3 increase of NO2 in two-pollutant combinations
| Pollutant (per 10 μg/m3) |
Model type | Male | Female | < 12 | 12–65 | ≥65 |
|---|---|---|---|---|---|---|
| NO2 | NO2 + SO2 | 4.21 (3.83–4.59) | 4.27 (3.88–4.67) | 5.55 (4.84–6.27) | 3.87 (3.51–4.23) | 5.02 (4.44–5.6) |
| NO2 + O3 | 2.04 (1.8–2.29) | 2.18 (1.93–2.44) | 3.76 (3.31–4.22) | 1.83 (1.6–2.05) | 2.67 (2.3–3.05) | |
| NO2 + PM10 | 2.25 (2.0–2.51) | 2.42 (2.15–2.68) | 3.38 (2.9–3.87) | 2.07 (1.84–2.31) | 3.03 (2.64–3.41) | |
| NO2 + PM2.5 | 2.46 (2.12–2.79) | 2.6 (2.25–2.94) | 3.71 (3.09–4.34) | 2.22 (1.91–2.54) | 3.65 (3.15–4.16) |
Note: PC refers to the percentage change
Discussion
Our study has found that short-term exposure to ambient NO2 is positively associated with the significant increase of the outpatient visits for patients with eczema. The detrimental effect lasted for 2–3 days after exposure, and is reinforced when combined with other air pollutants like SO2 and PM2.5. The exposure is risk factor for both genders and for.
The findings in this study are consistent with the previous findings. The NO2 has been a proven risk factor for eczema in countries at all development levels, including the US [16], China [8], Japan [17], and Belarus [18]. Most research on NO2 risks have been done in Shanghai. Li et al. reported an association of 10 μg/m3 increase of 7-day (lag 06) average concentrations of NO2 was associated with2.22% (95% CI: 1.27, 3.16%) and 2.31% (95% CI: 1.17, 3.45%) increase in outpatient visits for eczema in Shanghai between 2007 to 2011 [19]. Liu Wei also found a strong association between childhood atopic eczema and the increments of NO2 in the approximate interquartile range (20 μg/m3) during the gestational period in Shanghai from 2011 to 2012 [20]. Our findings showed that Guangzhou city, as the economic and industrial center of South China, is facing increasing demand of eczema treatment from 2013 to 2018, indicating that eczema has become a public health concern and needs to treated seriously. The government should pay attention to air pollutants like NO2 and take measures to manage and control the emissions.
Our study also proved that the combined effect of NO2 and other air pollutant factors exerted attenuated effect on eczema, indicating that the mixture may represent a higher risk than the individual component. The consistent associations have also been proven by previous studies. In western China’s Chengdu city, the combined effect of NO2, SO2 and PM10 showed increased percentage changes in daily outpatient visits for eczema than single effect of NO2 [21]. The study in Beijing reported consistently significant positive associations in two pollutant models, but the effects were lower than those in the single pollutant models [22]. The attenuated risks may be explained by the mechanism of how ambient air pollutants cause adverse effects on skin health. There are 4 generally acknowledged mechanism (a) oxidative stress, (b) alterations of microflora, (c) activation of the aryl hydrocarbon receptor (AhR), and (d) induction of the inflammatory cascade and subsequent impairment of the skin barrier [23]. The mixture of pollutants may activate several pathways simultaneously. For example, SO2 may enhance the production of reactive oxygen species, and further reduces the content of antioxidants in the skin [24]. PM10 may settle on the skin, blocking pores and therefore creating an anaerobic environment for bacteria strain responsible for acne [25]. It would be easier for the negative effect work together to damage the skin function and cause eczema.
We also found children and seniors are the vulnerable population. There are many findings on the eczema incidence for infants and children worldwide [26–28]. The infants and children are eligible to eczema due to the special skin structure and immature immune system, and the comprehensive and systemic measures should be taken to offer careful protection and cares to children [29]. The seniors are vulnerable due to the fragile skin and decreased immune system [30]. The gender-difference is not very significant in our finding, and both genders reported similar effective powers. As for the protective measures for the vulnerable population, the integration of health education and medical care would be more effective. Among all intervention plans, the multidisciplinary age-related structured training educational programs [31], nurse-led workshops, interventions, and care programs [32], as well as structured self-management education training programs [33] are proved efficient in reduction of severity of the condition, improving patient health outcome, and improving coping behaviors.
The lagged accumulative effects showed a sharp rise of outpatient visits in the following 3 days after the short-term NO2 exposure. The highest number of visits come at the current day (lag 0), and decreased gradually in the following 2 days (lag 1 and 2), and turns back to normal on the third day. This change will lead to service burden for physicians serving outpatient and emergency department. This finding is very indicative of the management of the outpatient department of the hospital. AHRQ has developed a series of guides for hospitals on improving the management of outpatient visit flows and reducing emergency department crowding [6]. The hospital of dermatology, as the specialized hospital, should develop an alert, flexible, and fast-reacting system which can predict/estimate the weather and pollution change to maintain high efficiency for the treatment of the common and reemerging conditions [34]. There are a bunch of plans to adopt, such as open a green channel for eczema, set up a standard service package, provide bundled service process, et al. The schedule of human resources is the most important task [35]. Since eczema is mild but relapsing condition that periodically influenced by air pollutants, it might be a proper measure to reorganize an integrated care process and manage the pre-and after outpatient management to serve the patients’ demand for services in hospitals. The integration of information technology and service process can improve the efficiency of patient management, measures include establishing patient files, sending weather alert to patients through social or hospital apps, make follow-up or revisit online, or scheduling the appointment on WeChat, et al.
Despite the organization management strategies, hospitals should cooperate with weather report departments, getting informed and alerted to certain pollutants, and should adopt predictive models to estimate the peaks and valleys of patient visits. Hospitals should manage patients waves, adjust the number of physicians on outpatient duty accordingly, and even consider the opening of eczema outpatient clinic in some certain season. Although we did not make predictions in this study, there are researchers devoted to predictive studies. Gul and Celik made an exhaustive review and analysis on the statistical forecasting methods in the forecasting of hospital emergency departments (EDs) [36]. Yucesan et al. developed a multi-method patient arrival forecasting outline for EDs, combined ARIMA, ANN, and the hybrid methods of the two [37]. The predictive methods can offer reliable evidence for decision-making in hospitals, and will be used in our further research.
Conclusion
The prevalence of eczema has been increasing since 2013 in Guangzhou city and has become a public concern now. The incidence of eczema is tightly associated with the concentration of NO2 and causes the changed patients to flow to outpatient visits. The hospital managers should attach great importance to disease management, hospital resource arrangement with climate change, and take measures to develop an integrated and multidisciplinary process to improve disease and hospital management.
Limitation
First, this study focused on the explored the influence of NO2 on eczema, and merely made shallow discussion about the interaction effects between NO2 and some major air pollutants. We did not include the influence of temperature and humidity, which might be also important to the incidence of eczema. Second, we used a comparatively simple mathematical model to evaluate the increase of outpatient visits in the future instead of using more advanced prospective analysis methods such as machine learning. Instead, we have the plan to made the unfinished analysis in the following studies. Third, the predictive analysis of hospital management needs more concrete data on physicians, patients, and resources, which are not sufficient in this research but will be our research direction for the further stage.
Supplementary Information
Additional file 1. The distribution of major variables: daily hospital admissions, weather, air pollution and particles in Guangzhou from March 1, 2013 to Dec. 31, 2018 (mean ± SD, anova test).
Acknowledgements
Not applicable.
Informed consent
All participants provided written informed consent before enrolment.
Authors’ contributions
ZLW drafted the manuscript. JD conducted data analysis. LQC participated in drafting and revision. SSQ designed the study, collected data and organized the drafting process. The author(s) read and approved the final manuscript.
Funding
This work was supported by The Natural Science Foundation of Guangdong Province (grant number 2018030310559), The Guangdong Province Medical Science and Technology Research Foundation (grant number C2020061), The Guangdong Province Medical Science and Technology Research Foundation (grant number C2020063) and Department of Science and Technology of Guangdong Province (grant number 2020A1414010213).
Availability of data and materials
The air pollution data that support the findings of this study are available on request from the corresponding author, Shuqun Shen. The atopic dermatitis outpatient visits data are not publicly available due to the privacy restriction.
Declarations
Ethics approval and consent to participate
The protocol of study and accessing the hospital admission data was approved by the ethics committee of School of Public Health of Southern Medical University, and was performed by the ethical standards noted in the 1964 Declaration of Helsinki and its later amendments.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Luwen Zhang and Dian Jing contributed equally to this work.
References
- 1.Ngatu NR, Ikeda M: Atopic Dermatitis (or Atopic Eczema). In: Occupational and Environmental Skin Disorders: Epidemiology, Current Knowledge and Perspectives for Novel Therapies. edn. Edited by Ngatu NR, Ikeda M. Singapore: Springer Singapore; 2018: 23–40.
- 2.Flohr C, Mann J. New insights into the epidemiology of childhood atopic dermatitis. Allergy. 2014;69(1):3–16. doi: 10.1111/all.12270. [DOI] [PubMed] [Google Scholar]
- 3.Harrop J, Chinn S, Verlato G, Olivieri M, Norbäck D, Wjst M, Janson C, Zock JP, Leynaert B, DJC G, et al. Eczema, atopy and allergen exposure in adults: a population-based study. 2007;37(4):526–35. [DOI] [PubMed]
- 4.Papadopoulos L, Walker C: Understanding skin problems: acne, eczema, psoriasis and related conditions: John Wiley & Sons; 2003.
- 5.Bryld LE, Hindsberger C, Kyvik KO, Agner T, Menné T. Risk factors influencing the development of hand eczema in a population-based twin sample. Br J Dermatol. 2003;149(6):1214–1220. doi: 10.1111/j.1365-2133.2003.05678.x. [DOI] [PubMed] [Google Scholar]
- 6.Chen X, Situ S, Zhang Q, Wang X, Sha C, Zhouc L, Wu L, Wu L, Ye L, Li C. The synergetic control of NO2 and O3 concentrations in a manufacturing city of southern China. Atmos Environ. 2019;201:402–416. doi: 10.1016/j.atmosenv.2018.12.021. [DOI] [Google Scholar]
- 7.Schikowski T, Krutmann J: [air pollution (particulate matter and nitrogen dioxide) and skin aging]. Der Hautarzt; Zeitschrift fur Dermatologie, Venerologie, und verwandte Gebiete 2019, 70(3):158–162. [DOI] [PubMed]
- 8.Li A, Fan L, Xie L, Ren Y, Li L. Associations between air pollution, climate factors and outpatient visits for eczema in West China hospital, Chengdu, South-Western China: a time series analysis. J Eur Acad Dermatol Venereol. 2018;32(3):486–494. doi: 10.1111/jdv.14730. [DOI] [PubMed] [Google Scholar]
- 9.Gelbard CM, Hebert AA. New and emerging trends in the treatment of atopic dermatitis. Patient Preference Adherence. 2008;2:387. [PMC free article] [PubMed] [Google Scholar]
- 10.Batchelor JM, Ridd MJ, Clarke T, Ahmed A, Cox M, Crowe S, Howard M, Lawton S, McPhee M, Rani A. The eczema priority setting partnership: a collaboration between patients, carers, clinicians and researchers to identify and prioritize important research questions for the treatment of eczema. Br J Dermatol. 2013;168(3):577–582. doi: 10.1111/bjd.12040. [DOI] [PubMed] [Google Scholar]
- 11.Shen S, Li X, Yuan C, Huang Q, Liu D, Ma S, Hui J, Liu R, Wu T, Chen Q. Association of short-term exposure to sulfur dioxide and hospitalization for ischemic and hemorrhagic stroke in Guangzhou, China. BMC Public Health. 2020;20(1):263. doi: 10.1186/s12889-020-8354-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhou M, Wang L, Liu T, Zhang Y, Lin H, Luo Y, Xiao J, Zeng W, Zhang Y, Wang X, et al. Health impact of the 2008 cold spell on mortality in subtropical China: the climate and health impact national assessment study (CHINAs) Environ Health. 2014;13:60. doi: 10.1186/1476-069X-13-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang J, Yin P, Sun J, Wang B, Zhou M, Li M, Tong S, Meng B, Guo Y, Liu Q. Heatwave and mortality in 31 major Chinese cities: definition, vulnerability and implications. Sci Total Environ. 2019;649:695–702. doi: 10.1016/j.scitotenv.2018.08.332. [DOI] [PubMed] [Google Scholar]
- 14.Anderson G, Bell M. Heat waves in the United States: mortality risk during heat waves and effect modification by heat wave characteristics in 43 U.S. communities. Environ Health Perspect. 2011;119(2):210–218. doi: 10.1289/ehp.1002313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yin P, Chen R, Wang L, Liu C, Niu Y, Wang W, Jiang Y, Liu Y, Liu J, Qi J, et al. The added effects of heatwaves on cause-specific mortality: a nationwide analysis in 272 Chinese cities. Environ Int. 2018;121:898–905. doi: 10.1016/j.envint.2018.10.016. [DOI] [PubMed] [Google Scholar]
- 16.Aguilera I, Pedersen M, Garcia-Esteban R, Ballester F, Basterrechea M, Esplugues A, Fernández-Somoano A, Lertxundi A, Tardón A, Sunyer J. Early-life exposure to outdoor air pollution and respiratory health, ear infections, and eczema in infants from the INMA study. Environ Health Perspect. 2013;121(3):387–392. doi: 10.1289/ehp.1205281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.To TM, Gray N, Zhu J, Stieb D, Dell SDM: Association of Air Pollution with Incidence of Asthma, Allergic Rhinitis and Eczema: 10-Year Follow-Up of the Toronto Child Health Evaluation Questionnaire (T-CHEQ) Study. In: A16 AIR POLLUTION AND PEDIATRIC ASTHMA. edn.: American Thoracic Society; 2018: A1021-A1021.
- 18.Belugina I, Yagovdik N, Belugina O, Belugin SJ. Venereology: outdoor environment, ozone, radionuclide-associated aerosols and incidences of infantile eczema in Minsk, Belarus. 2018;32(11):1977–85. [DOI] [PubMed]
- 19.Li Q, Yang Y, Chen R, Kan H, Song W, Tan J, Xu F, Xu J. Ambient air pollution, meteorological factors and outpatient visits for eczema in Shanghai, China: a time-series analysis. Int J Environ Res Public Health. 2016;13(11):1106. doi: 10.3390/ijerph13111106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu W, Cai J, Huang C, Hu Y, Fu Q, Zou Z, Sun C, Shen L, Wang X, Pan J, et al. Associations of gestational and early life exposures to ambient air pollution with childhood atopic eczema in Shanghai, China. Sci Total Environ. 2016;572:34–42. doi: 10.1016/j.scitotenv.2016.07.197. [DOI] [PubMed] [Google Scholar]
- 21.Li A, Fan L, Xie L, Ren Y, LJJotEAoD L. Venereology: Associations between air pollution, climate factors and outpatient visits for eczema in West China Hospital, Chengdu, south-western China: a time series analysis. 2018;32(3):486–94. [DOI] [PubMed]
- 22.Guo Q, Liang F, Tian L, Schikowski T, Liu W, XJESP P. Impacts: Ambient air pollution and the hospital outpatient visits for eczema and dermatitis in Beijing: a time-stratified case-crossover analysis. 2019;21(1):163–73. [DOI] [PubMed]
- 23.Burke KE. Mechanisms of aging and development—a new understanding of environmental damage to the skin and prevention with topical antioxidants. Mech Ageing Dev. 2018;172:123–130. doi: 10.1016/j.mad.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 24.Mancebo SE, Wang SQ. Recognizing the impact of ambient air pollution on skin health. JEADV. 2015;29(12):2326–2332. doi: 10.1111/jdv.13250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Puri P, Nandar SK, Kathuria S, Ramesh V. Effects of air pollution on the skin: a review. Indian J Dermatol Venereol Leprol. 2017;83(4):415–423. doi: 10.4103/0378-6323.199579. [DOI] [PubMed] [Google Scholar]
- 26.Aguilera I, Pedersen M, Garcia-Esteban R, Ballester F, Basterrechea M, Esplugues A, Fernández-Somoano A, Lertxundi A, Tardón A. Sunyer JJEhp: Early-life exposure to outdoor air pollution and respiratory health, ear infections, and eczema in infants from the INMA study. 2013;121(3):387–92. [DOI] [PMC free article] [PubMed]
- 27.Kathuria P, JJPA S. Immunology: Association of pollution and climate with atopic eczema in US children. 2016;27(5):478–85. [DOI] [PubMed]
- 28.To T, Zhu J, Stieb D, Gray N, Fong I, Pinault L, Jerrett M, Robichaud A, Ménard R, van Donkelaar AJERJ: Early life exposure to air pollution and incidence of childhood asthma, allergic rhinitis and eczema. 2020, 55(2). [DOI] [PMC free article] [PubMed]
- 29.Heinl D, Prinsen C, Sach T, Drucker A, Ofenloch R, Flohr C. Apfelbacher CJBJoD: Measurement properties of quality-of-life measurement instruments for infants, children and adolescents with eczema: a systematic review. 2017;176(4):878–89. [DOI] [PubMed]
- 30.Proksch E, Fölster-Holst R, Jensen J-M. JJods: Skin barrier function, epidermal proliferation and differentiation in eczema. 2006;43(3):159–69. [DOI] [PubMed]
- 31.Darsow U, Wollenberg A, Simon D, Taïeb A, Werfel T, Oranje A, Gelmetti C, Svensson A, Deleuran M, Calza AM, et al. ETFAD/EADV eczema task force 2009 position paper on diagnosis and treatment of atopic dermatitis. JEADV. 2010;24(3):317–328. doi: 10.1111/j.1468-3083.2009.03415.x. [DOI] [PubMed] [Google Scholar]
- 32.Thompson D. Best practice guidelines: integrating person and family centred care and client centred learning into practice in a nurse-led eczema clinic. Aust Nurs Midwifery J. 2019;26(8):30–33. [Google Scholar]
- 33.Ridd M, King A, Le Roux E, Waldecker A, Huntley A. Systematic review of self-management interventions for people with eczema. Br J Dermatol. 2017;177(3):719–734. doi: 10.1111/bjd.15601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chang AM, Cohen DJ, Lin A, Augustine J, Handel DA, Howell E, Kim H, Pines JM, Schuur JD, McConnell KJ. Hospital strategies for reducing emergency department crowding: a mixed-methods study. Ann Emerg Med. 2018;71(4):497–505. doi: 10.1016/j.annemergmed.2017.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khanna S, Sier D, Boyle J, Zeitz K. Discharge timeliness and its impact on hospital crowding and emergency department flow performance. Emer Med Australasia. 2016;28(2):164–170. doi: 10.1111/1742-6723.12543. [DOI] [PubMed] [Google Scholar]
- 36.Gul M, Celik E. An exhaustive review and analysis on applications of statistical forecasting in hospital emergency departments. Health Syst. 2018:1–22. [DOI] [PMC free article] [PubMed]
- 37.Yucesan M, Gul M, Celik E. A multi-method patient arrival forecasting outline for hospital emergency departments. Int J Healthc Manag. 2018:1–13.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. The distribution of major variables: daily hospital admissions, weather, air pollution and particles in Guangzhou from March 1, 2013 to Dec. 31, 2018 (mean ± SD, anova test).
Data Availability Statement
The air pollution data that support the findings of this study are available on request from the corresponding author, Shuqun Shen. The atopic dermatitis outpatient visits data are not publicly available due to the privacy restriction.