Abstract
Parent stress has been associated with negative outcomes for youth and may be particularly high during adolescence. Mindfulness interventions have the potential to reduce parent stress and to improve parenting behavior and parent-child relationship quality. The present randomized controlled study examined effects of a parenting-focused mindfulness intervention, the Parenting Mindfully (PM) intervention, for highly stressed parents of adolescents. Eighty three mothers of 12–17 year olds reporting high stress were randomly assigned to the PM intervention or to a minimal-intervention Parent Education (PE) control group. At pre- and post-intervention, mothers reported on their mindfulness, stress, parenting stress, mindful parenting, and parent-adolescent relationship quality. At pre- and post-intervention, mothers’ observed parenting behaviors and reported negative emotional responses to a laboratory parent-adolescent interaction task (PAIT) were also collected. Findings indicated that the PM intervention, compared to PE, increased mothers’ mindfulness, reduced parenting stress in two domains, increased mindful parenting related to emotional awareness in parenting, and improved parent-adolescent relationship quality. For mothers of girls (but not mothers of boys), the PM intervention also decreased negative parenting behavior and decreased negative emotional responses in PAIT. Effects sizes were medium to large. In sum, findings support parenting-focused mindfulness training as a viable intervention strategy for highly-stressed parents.
Keywords: Mindfulness, Parenting, Family-based intervention, Adolescence
Parent stress has been identified as a critical risk factor for child and adolescent adjustment, with high parent stress associated with poor parenting and increased risk for child psychopathology (Deater-Deckard 1998). A separate literature has found that mindfulness-based interventions can significantly reduce stress levels in adults (Kabat-Zinn et al. 1992). Thus, mindfulness-based interventions may represent a promising approach for reducing parent stress and improving parenting and child outcomes. However, few randomized controlled trials (RCTs) have tested mindfulness interventions for parents, particularly parents of adolescents.
High levels of parent stress (parents’ perceived general stress levels) and parenting stress (parents’ perceived stress associated with the demands of parenting) have been linked to increased child and adolescent psychopathology, substance use, and risk behavior outcomes (Crnic et al. 2005; Kelley 1992; Visconti et al. 2002). High parent stress and parenting stress can lead parents to engage in more maladaptive parenting behaviors (e.g., low parental warmth, high harsh/negative parenting) (Belsky et al. 1996; Chan 1994) and can lead to diminished parent-child bonding (Deater-Deckard 1998), both of which are predictors of child psychopathology and risk behaviors (Barnes et al. 2000; Galambos et al. 2003). Also, parent stress can impact how parents view their child’s behaviors, leading them to interpret normative variation in child emotion and behavior as negative, which, in turn, may exacerbate child behavior problems. In sum, parents with high levels of parent stress and parenting stress are at heightened risk for maladaptive family environments and negative child outcomes.
Parent stress and parenting stress may be particularly salient when children go through adolescence. Starting in early adolescence, parenting becomes more stressful due to several changes, with adolescents starting to spend less time with family and more time with peers, asserting autonomy in family interactions, and experiencing heightened emotional arousal as a result of multiple biological and social changes (Laursen & DeLay 2011; Steinberg 2001). In fact, many parents report that adolescence is the most stressful period of parenting (Pasley & Gecas 1984). At the same time as parent stress levels increase and family relationships experience strain, adolescents still require close family relationships as they encounter cognitive, emotional, and social changes and navigate peer and school networks that introduce risky behaviors (Steinberg et al. 1994; Wills & Yaeger 2003). Given the high levels of parent stress and parenting stress during adolescence and the importance of the family environment in adolescence, interventions that can reduce parent stress during adolescence are needed.
Mindfulness-based interventions (e.g., Mindfulness-Based Stress Reduction [MBSR], Kabat-Zinn 1982, 1990; Mindfulness-Based Cognitive Therapy [MBCT], Segal et al. 2002) have been shown to reduce stress in adults (e.g., Kabat-Zinn et al. 1992) and thus may have promise for reducing parent stress and thereby improving parenting behaviors, parent-child relationship quality, and adolescent outcomes. Mindfulness has been defined as “the practice of focusing full attention on the present moment intentionally and without judgement” (Kabat-Zinn 1990). The practice of mindfulness is hypothesized to reduce perceived stress and biological stress reactivity by increasing one’s awareness of and ability to tolerate thoughts and emotions. Mindfulness may help decrease distress and over-reactivity to events and increase the ability to respond to events in ways that one consciously chooses (rather than through automatic “mindless” behaviors) and in ways that are open to experiencing a range of emotions, including closeness with others.
Mindfulness-based interventions for adults include meditation-focused interventions such as MBSR and MBCT and programs that include a focus on mindfulness without a strong meditation component (e.g., Acceptance and Commitment Therapy [ACT], Hayes et al. 2006). Meditation-focused mindfulness interventions teach mindfulness through meditation practice (including seated meditation, walking meditation, and yoga), cultivation of present-minded awareness in everyday life, and discussions of mindfulness applications to stress physiology, coping, and relationships. RCTs with adults have shown that these interventions are effective in reducing subjective and physiological reactivity to stress as compared to cognitive-behavior therapy (Brewer et al. 2009) and in reducing stress-related disorders including psoriasis, anxiety, and relapse to depression as compared to no-treatment, treatment as usual, minimal intervention, or attention control groups (Hoge et al. 2013; Kabat-Zinn et al. 1998; Teasdale et al. 2000).
Given evidence for mindfulness interventions in reducing stress in adults, developmental scientists have called for the use of mindfulness interventions with parents (Sawyer-Cohen & Semple 2010). Parenting is stressful; on a daily basis, parents are presented with internal and external challenges to their ability to regulate emotions in order to calmly select parenting behaviors that are consistent with their parenting goals, to show compassion for their child, and to engage in child-focused parenting (Dix 1991; Dumas 2005; LaGasse et al. 2005). There are a number of parent training interventions that teach effective parenting practices and have been shown to improve parenting behaviors and reduce child behavior problems (e.g., Shelleby & Shaw 2014; Spoth et al. 2001). However, it can be difficult to engage parents in these interventions, particularly if they are highly stressed (Dumas 2005). Mindfulness training is an additional option that can particularly help parents cope with their own stress to improve parenting.
Mindfulness interventions for parents can decrease parent over-reactivity, increase positive parenting, and increase closeness and bonding in parent-adolescent relationships (Dumas 2005; Duncan et al. 2009; Kabat-Zinn & Kabat-Zinn 1997). By helping parents tolerate normative changes in adolescent emotion and behavior (e.g., emotional lability and bids for autonomy) without over-reactivity or judgment, they can help parents view adolescents more positively. They can also help parents to be more “present” in interactions with adolescents and more aware of adolescents’ and their own emotions. Moreover, mindfulness interventions can help parents to be more compassionate towards youth (and towards themselves as parents) (Coatsworth et al. 2010; Duncan et al. 2009). These increases in parent present-centered awareness, emotional awareness, and compassion, and reductions in parent reactivity and judgement of adolescent behaviors can lead to improved parenting, improved parent-adolescent relationship quality, and lower adolescent psychopathology risk. Indeed, parents who report using more of these mindful parenting practices in their daily lives show more positive and supportive parenting practices, greater positive emotion in parenting, lower negative parenting practices (de Bruin et al. 2014; Parent et al. 2016; Turpyn & Chaplin 2016) and have children who show lower levels of child internalizing and externalizing problems (e.g., Geurtzen et al. 2015; Parent et al. 2016).
Despite the potentially important application of providing mindfulness training to parents, empirical evaluations of mindful parenting interventions have only recently begun. Non-controlled pilot studies have found initial evidence that mindfulness-based parenting interventions increase parent mindfulness in parents of preschoolers (Altmaier & Maloney 2007), increase positive parenting and decrease parenting stress and child internalizing and externalizing symptoms in families of 2–21 year-olds (Bögels et al. 2014), and increase parenting satisfaction and child compliance in families of preschoolers with developmental delays or ADHD (Singh et al. 2006, 2007, 2010).
In addition to non-controlled trials, there are a handful of published RCTs of mindful parenting interventions. First, two RCTs examined mindfulness training for parents of preschool to school-aged children with special needs or developmental delays compared to a no-intervention control. They found that mindfulness training decreased parent stress and increased parent mindfulness (Benn et al. 2012; Neece 2014) and reduced child behavior problems (Neece 2014). Second, Felver et al. (2017) found that a mindfulness intervention delivered to both parents and children increased children’s attention regulation abilities compared to a wait-list control group in 9–12 year olds. Third, Coatsworth et al. conducted a pilot (2010) and a large-scale (2015) RCT of a parent-training program infused with mindfulness training for parents of 10–14 year olds. They found that the mindfulness-infused parent training program produced stronger effects than parent training alone (in the 2010 study) and stronger and more sustained effects than parent training alone for fathers (in the 2015 study) on mindful parenting and some aspects of parent-child relationship quality (e.g., parent support/understanding) and parenting behaviors (e.g., parental effective monitoring). While these initial studies are promising, additional RCTs are needed on mindful parenting interventions for parents of adolescents, given the importance of this developmental period for family stress and youth development. In addition, examination of whether mindfulness training interventions alone (without the parent training component) affect changes in parenting behaviors and parent-child relationship quality would be of interest.
In addition to examining effects of mindful parenting interventions, it is useful to also examine whether these effects are stronger for some families than others. Several prior studies of traditional parent training interventions have found moderation by child gender, with some finding better effects of parenting programs on child behavior problems for boys and some for girls (Gardner et al. 2010; Lavigne et al. 2007). Other studies have found moderation by child age, with greater benefits for younger than older children (Gardner et al. 2010; Lundahl et al. 2006).
The present study tested a parenting-focused mindfulness training intervention, the Parenting Mindfully (PM) intervention, with highly-stressed mothers of 12–17 year olds. We used a randomized controlled design to examine effects from pre- to post-intervention of the PM intervention compared to a Parent Education (PE) minimal intervention control group on mother-reported mindfulness, parent stress, parenting stress, mindful parenting, and parent-adolescent relationship quality. In addition, we used a laboratory parent-adolescent conflict interaction task to examine intervention effects on mothers’ observed parenting behavior and negative emotional responses in the lab task. We hypothesized that mothers in PM would show greater improvements from pre- to post-intervention in mindfulness, mindful parenting, parent-adolescent relationship quality, and observed maternal warmth, and would show greater decreases in parent stress, parenting stress, and observed negative parenting and negative emotional responses in the lab task compared to mothers in the PE control group. We also examined whether adolescent gender or age moderated intervention effects.
Method
Participants
Highly stressed parents and their adolescents were recruited from a suburban community in the mid-Atlantic U.S. Participants were 83 parents of 12–17 year olds (M age = 14.04, SD = 1.56; 40 boys, 43 girls) who reported high levels of stress. Both mothers and fathers were invited to participate in the intervention groups and to complete questionnaires. However, only 5 fathers attended intervention groups with mothers. Thus, the present report focuses on outcome data for mothers/female primary caregivers (94% biological mothers, 3.6% adoptive mothers, 2.4% grandmothers), referred to throughout as “mothers.” Mean age of mothers was 47.4 years (SD = 6.3) and 79.8% were currently married. Adolescent race was 65.1% Non-Hispanic White, 12.0% Mixed-Race, 9.6% Hispanic, 4.8% African-American, 4.8% Asian, 3.6% Other/Not Reported, similar to the local community. Median household income was >$100,000/yr (63.9% of families), consistent with median income for the local county, with the remaining 36.1% of families ranging from under $15,000 to between $75,000 and $100,000.
Families were recruited through: 1) a large community behavioral health services provider for children and adolescents, which asked all families receiving services if they would like to participate in this study, 2) flyers posted at a second community behavioral health center, 3) mailings to representative households in the area. 53.7% of adolescents were engaged in psychotherapy (in addition to the intervention) at the time of the intervention.
Interested parents were contacted and screened by phone for inclusion criteria. Inclusion criteria were family with an adolescent between 11–16 years old (note: 3 adolescents turned 17 between screening and the first session), adequate English proficiency to complete questionnaires for at least one parent and the adolescent, and elevated parent stress levels (mean score of at least 3 [on a 1–5 scale] for two questions adapted from parent stress and parenting stress measures: “In the last month, how often have you felt stressed?” and “In the last month, how often have you felt stressed by parenting your teenager or worried about your teenager?”). Exclusion criteria were diagnosis of intellectual disability or psychotic disorder (for adolescent) or medical condition that would preclude participation in gentle yoga (for parents).
One hundred thirteen families were screened for the study. All 113 met inclusion criteria. Of these, 100 families agreed to participate and completed pre-intervention sessions. Just after the pre-intervention sessions, 4 families dropped from the study due to lack of interest. The remaining 96 families were randomized to condition and completed the intervention phase. Of the 96 families remaining in the study, 83 families completed the post-intervention assessment. The other 13 families were unable to attend post assessments due to lack of interest in the study (n = 2) or scheduling difficulties (n = 11). The 83 families who completed pre and post sessions had lower parent stress (t[97]= 2.32, p = .02) and lower parenting stress related to incompetence/guilt (t[97]= 2.12, p = .04) at pre-intervention than non-completers. There were no other differences on demographics or study variables.
Of the 83 families in the study, six did not complete the post-intervention lab task, because adolescent refused to complete it (2) or because the family was unable to come in person and completed questionnaires online (4) and so are not included in the parent negative emotional response to the lab task analyses. The 77 families with lab task data had higher parent mindfulness and lower mindful parenting related to present-centered emotional awareness and present-centered attention at pre-intervention than non-completers (t’s = 2.21 to 2.81, p’s = .01-.02). There were no other differences on demographics or study variables. In addition, four parents had missing observational parenting data at pre or post-intervention due to technical problems with video-recording (1) or missing video-recordings (3) and so are not included in observed parenting analyses. The 73 families with observational parenting data were not different from the N of 83 on demographic or study variables.
Procedures
Families were randomly assigned to the Parenting Mindfully (PM) group (n = 41) or the minimal-intervention Parent Education (PE) control group (n = 42) using a computer-generated random numbers sequence. Families completed pre-intervention sessions, the 8-week intervention phase, and post-intervention sessions. Pre- and post- sessions included questionnaires and the PAIT. Intervention groups were held in the two behavioral health centers that were used for recruitment.
Intervention content and structure.
PM and PE interventions were group interventions, with 10–16 parents assigned per group. PM groups met for 2 hours once per week for 8 weeks, similar to prior mindfulness interventions (e.g., MBSR, MBCT). PM groups focused on cultivating and encouraging mindfulness, including mindfulness in daily life and in parenting interactions, based on mindfulness-based stress reduction programs for adults and the mindful parenting literature (e.g., Dumas 2005; Duncan et al. 2009). The PM intervention was based on meditation-focused mindfulness interventions (MBSR, MBCT) and thus focused on formal and informal meditation practice and discussions of applications of mindfulness. Sessions focused on: 1. Increasing present-focused awareness in daily life (e.g., while driving) and in interacting with the adolescent, 2. Increasing awareness of emotions in self and in adolescent, 3. Nonjudgmental acceptance of experiences, including non-judgmental acceptance of adolescent and of self as parent, 4. Non-reactivity to experience, including non-reactivity to normative adolescent behaviors (and selecting parenting behaviors consistent with parenting values), and 5. Increasing compassion for self and adolescent. Notably, PM did not include explicit parenting information or training in parenting techniques (e.g., praising positive behavior, developing a reward system) beyond practicing present-focused awareness and non-reactivity and reflecting on parents’ own parenting values. For example, if a parent asked a group leader, “What should I do to discipline my son when he refuses to clean his room?” the group leader would gently direct the group members to ask themselves “What does your parenting wise mind say?” The group leader would not offer specific advice, but rather would ask group members to reflect on the emotions present and/or consistency with their parenting values.
Specific content of each session is summarized in the Supplementary Material. Each session included: 1. Formal mindfulness practice (meditation or gentle yoga), 2. Discussion of and practice in activities to foster informal mindfulness practice including cultivating present-focus in daily life and while parenting, 3. Group discussions of mindfulness applications to parenting, and 4. Group discussion of homework. Homework involved 30 minutes of formal mindfulness practice and 15–30 minutes of informal mindfulness practice during parent-adolescent interactions, 6 days per week. In session 6, adolescents were invited to attend the group. They participated with parents in formal meditation activities and then parents and adolescents practiced present-focused awareness during a parent-adolescent discussion.
The PE condition was modeled on brief interventions/informational handouts that have been used successfully in prior prevention work (e.g., Turrisi et al. 2009). PE was intended as a control for some non-specific factors, including expectancies for improvement and attendance in group sessions. However, as it was modeled on brief interventions, it included fewer sessions and less contact time than the PM groups. As this was the first study of the PM intervention we used a limited control group, however future trials should use more intensive control groups. PE groups met 3 times for 30 minutes each. At each group, the group leader handed out a 3 page packet of information, provided a power-point presentation, and answered parent questions. PE groups provided information on: 1. adolescent development and parenting, 2. changes in family and peer relations and monitoring of youth, and 3. adolescent risk behaviors and keeping open communication. Content was based on information pamphlets created by NIH for parents (e.g., NIDA 2012; Robertson et al. 2003). Like PM, PE did not include explicit instruction on behavioral parent training techniques (e.g., praising positive behavior) beyond a brief overview of tips on monitoring adolescent behaviors and avoiding criticizing teens.
Intervention leaders.
PM Groups were co-led by two leaders. PM group leaders were the study co-Investigator (co-I), who has expertise in mindfulness interventions, and one doctoral student in clinical psychology or two doctoral students in clinical psychology. Doctoral students received at least 16 hours of training in delivery of the PM intervention and were supervised weekly by the co-I. PE group leaders were the study Principal Investigator (PI) and/or one doctoral student in clinical psychology, who was trained and supervised by the PI.
Measures
Parent stress.
The Perceived Stress Scale (PSS; Cohen et al. 1983) is a 14-item self-report of the degree to which parents perceive situations in their lives in the past month as stressful (α = .88; e.g., “In the last month, how often have you felt nervous and ‘stressed’?”). Mothers rated each item from 0–4 for how often they perceived the situation as stressful. Items were summed. The PSS is widely used and has good reliability and validity (Cohen et al. 1983).
Parent mindfulness.
The Mindfulness Attention Awareness Scale (MAAS; Brown & Ryan 2003) is a 15-item self-report of mindfulness that measures the extent to which individuals experience present-focused awareness and attention currently (α = .90; e.g., “I find myself doing things without paying attention.” [reverse-scored]). Mothers rated each item on a scale from 1 to 6. Items were scored such that higher scores reflected higher mindfulness and summed. The MAAS shows convergent validity with well-being measures and is sensitive to mindfulness intervention effects (Brown & Ryan 2003).
Parenting stress.
Parenting stress was assessed with three subscales that focus on parenting stress from the Stress Index for Parents of Adolescents (SIPA; Sheras et al. 1998). The subscales are: Parent life restrictions (10 items; α = .90; e.g., “Since my child became a teenager, I feel that I am almost never able to do things that I like to do”), Parent incompetence/guilt, (8 items; α = .83; e.g., “When my child misbehaves or gets in trouble, I feel responsible, as if I didn’t do something right”), and Relationship with spouse/partner (9 items; α = .90; e.g., “I frequently argue with my spouse/partner about how to raise my child”). Six mothers did not have a current partner and so left items blank for the Relationship with spouse/partner subscale. Mothers rated each item on a scale from 1 to 5. Items were scored such that higher scores reflected higher parenting stress and summed. These subscales show good internal consistency, test-retest reliability, and convergent validity (Sheras et al. 1998).
Mindful parenting.
Mothers reported on current levels of mindful parenting on the original version of the Interpersonal Mindfulness in Parenting Scale (IM-P; Duncan 2007). The IM-P is an 8-item self-report of mindful parenting, including four subscales reflecting: Present-centered emotional awareness in parenting (2 items, α = .50; e.g., “I am aware of how my moods affect the way I treat my child”), Present-centered attention in parenting (2 items, α = .70; e.g., “I find myself listening to my child with one ear because I am busy doing or thinking about something else at the same time” [reverse scored]), Non-reactivity/low-reactivity in parenting (2 items, α = .61; e.g., “When I am upset with my child, I notice how I am feeling before I take action”), and Non-judgmental acceptance in parenting (2 items, α = .73; e.g., “I listen carefully to my child’s ideas, even when I disagree with them”). Notably, while the present study’s alpha was low for Present-centered emotional awareness in parenting, this alpha is consistent with prior work (Coatsworth et al. 2015), and we retained this subscale due to its importance to mindful parenting. Each item was rated on a scale from 1 to 5 and items were summed to create subscale scores. Higher scores reflected greater mindful parenting. The IM-P has shown convergent validity with other measures of mindfulness (Duncan 2007).
Parent-adolescent relationship quality.
The Adolescent-parent relationship domain subscale from the SIPA (Sheras et al. 1998) is a parent-report of parent’s relationship quality with the target adolescent, including the amount of affection and communication between them (16 items, α = .88; e.g., “I expected to have closer and warmer feelings for my child at this age than I do”). Mothers rated each item on a scale from 1 to 5. Items were scored such that higher scores reflected higher parent-adolescent relationship quality and summed. The adolescent-parent relationship domain subscale shows good reliability and correlates with other measures of parent-youth closeness (Sheras et al. 1998).
Parent-adolescent interaction (PAIT) laboratory task.
Upon arriving for the pre- and post-intervention assessment sessions, mothers and adolescents first completed the laboratory task. For this task, the mother and adolescent went to separate rooms and each completed the Issues Checklist (IC; Prinz et al. 1979), a checklist of common family conflict topics (e.g., cleaning bedroom). Mothers and adolescents endorsed topics discussed in the past month and the anger level they felt during the discussion. After completing the IC, there was a 20-minute adaptation period during which mothers and adolescents listened to a 5-minute relaxation audio recording and were told to relax. Then, mothers (and also adolescents) completed pre-task assessments, including a self-report of negative emotions.
Following the pre-task assessments, the mother was brought into the adolescent’s room and seated next to the adolescent for the PAIT task. The mother and adolescent were asked to discuss their mutually highest-rated conflict issue from the IC for 10 minutes (following prior work- Sheeber et al. 1997). During the discussion, mothers and adolescents were video-recorded and recordings were later coded for parenting behaviors. Following the PAIT task, the mother returned to her room and post-task assessments (including reported negative emotion) were collected. After post-task assessments, the mother completed study questionnaires (see above).
Observed parenting behaviors.
Maternal parenting behaviors during the discussion were coded by trained coders using the PAIT Coding System (First Author 2010). Maternal warmth (e.g., mother nods head, makes eye contact, praises adolescent), and maternal negative parenting (e.g., mother criticizes, mocks, or interrupts adolescent, uses harsh vocal tone) were coded, based on the parenting literature (e.g., Gottman et al. 1997). Coders viewed the discussion and rated the parenting behaviors on a scale from 1–5 (“none present” to “high level”), based on facial expressions, behaviors, vocal tone, and speech content. Coders received at least 10 hours of training in the coding system and met for weekly coding meetings to discuss coding questions. Nineteen percent of videotaped interactions were randomly chosen, double-coded, and checked for inter-rater reliability. Reliability was acceptable to good, with intra-class correlation coefficients of 0.68 for warmth and 0.77 for negative parenting.
Parent negative emotional response.
Mothers reported on their current experience of sadness, anger, fear, joy, and anxiety immediately prior to the PAIT task (pre-task) and on their experience of these emotions during and immediately after the PAIT task at post-task using the Differential Emotions Scale-Short form (DES-S; Izard 1972) and also rated their experience of frustration and anxiety using two additional items, each on a 10-point scale. The DES-S includes five adjectives to describe each emotion state (a total of 25 items) and mothers rated on a 5-point scale the extent to which each adjective described the way she feels/felt. The DES-S shows good internal consistency and validity (Izard 1972) and has been used to assess emotional reactivity to lab tasks (e.g., Chaplin et al. 2008). The present study used a sum of three of the negative emotion scales of the DES (sadness, anger, anxiety) and the frustration and anxiety items (which were standardized to put them on the same scale) to create an overall negative emotion scale at pre- and post-task. Fear was not included because very few mothers reported fear. The composite variable showed good internal consistency (α = .76). Analyses examined post-task negative emotion scores minus pre-task scores to reflect response to PAIT. This change from baseline approach is consistent with prior work examining responses to emotion-eliciting tasks (e.g., Rudolph et al. 2010).
Data Analyses
Prior to analyses, data inspection was done. Continuous variables were examined for outliers (values > 3 SDs above the mean) and winsorized (outliers set to equal 3 SDs above the mean). Parent negative emotional responses to PAIT had 2 outlier cases and were winsorized. Observed negative parenting was skewed and square root transformed for analyses (raw data reported in table/figure for ease of interpretation).
To examine effects of the PM intervention, compared to the PE intervention, on outcome variables, ANCOVAs were conducted with post-intervention scores as the dependent variable, group (PM vs. PE) as the independent variable, and pre-intervention scores as the covariate. To examine whether adolescent gender or age moderated intervention effects, ANCOVAs were conducted testing interactions between intervention group and gender (male, female) or age (early adolescence [age 11–13] vs. middle adolescence [age 14–17]) on post-intervention scores, covarying pre-intervention scores. We also considered family income level as a moderator, given prior research (Lundahl et al. 2006), however we did not have sufficient variability in income. For effect sizes, Cohen’s d values were calculated by dividing the difference in the estimated marginal means (from the ANCOVAs) by the pooled standard deviation. Following conventions by Hyde (2005), we labeled d’s of .11–.24 as “small,” .25–.34 as “small to medium,” .35–.64 as “medium,” and .65 and above as “large.”
We used a complete-case analysis approach, such that analyses were based on the 83 families that had data at both pre- and post-intervention assessments (or, for the laboratory data, the 77 that had pre and post data and, for the laboratory observational data, the 73 that had pre and post data). However, because complete-case analysis can yield biased estimates due to potential systematic patterns in missing data (Little & Rubin 2002), we also conducted secondary analyses using multiple imputation (MI) with the 96 families that completed pre-intervention sessions and the intervention phase. For MI analyses, fifty imputed datasets were generated using a fully conditional Markov Chain Monte Carlo (MCMC) method via SPSS version 25.0.0 (SPSS Inc., USA).
Results
Intervention Group Differences
There were no significant differences between PM and PE participants on demographic variables, adolescent therapy status (in therapy vs not), or any other study measure at pre-intervention. There were also no adolescent gender or age (the moderator variables) differences on any variable at pre-intervention.
Session Attendance and Intervention Fidelity
Of the 83 mothers, 78.3% attended at least one intervention session (80.5% PM, 76.2% PE). For those that attended sessions, the average number of sessions attended was 4.65 (SD = 2.32; 58.1%) for PM and 2.16 (SD = 0.77; 71.9%) for PE (notably, there were fewer PE than PM sessions), consistent with other group-based interventions (e.g., Gillham et al. 2007). There were not differences in intervention attendance by adolescent gender, age, or other demographic variables. The study co-I and PI listened to audio tapes of the PM and PE intervention sessions and rated intervention fidelity (whether or not each of 6–10 concepts/activities was covered) on a scale from 1 (concept absent) to 3 (concept present). Mean fidelity for PM was 2.96 (SD = 0.05) and for PE was 3.00 (SD = 0).
Intervention Effects
ANCOVAs were conducted predicting outcome measures at post-intervention, with pre-intervention scores covaried.
Questionnaire measures.
As shown in Table 1, ANCOVAs found a significant intervention group effect on parent mindfulness, with mothers in PM reporting higher mindfulness at post-intervention than mothers in PE, with a medium effect size. In secondary MI analyses, this finding fell to a trend (p < .10) with a medium effect size. The intervention group effect on parent stress was not significant.
Table 1.
Means by Intervention Group and Time-Point and Intervention Effects on Parent Stress, Mindfulness, Parenting Stress, Mindful Parenting, Parent-Adolescent Relationship Quality, and Observed Parenting and Negative Emotion in PAIT Task
| Pre-Intervention | Post-Intervention | PM versus PE (ANCOVA) | |||||
|---|---|---|---|---|---|---|---|
| PM M (SD) | PE M (SD) | PM M (SD) | PE M (SD) | F value | d value | MI d value | |
| Questionnaires (n = 83) | |||||||
| Parent stress | 27.05 (6.78) | 25.98 (7.36) | 22.36 (8.16) | 22.40 (7.33) | 0.43 | −0.14 | −0.09 |
| Parent mindfulness | 32.76 (14.25) | 32.43 (10.30) | 33.68 (14.48) | 29.10 (9.24) | 4.20* | 0.45 | 0.37 |
| Parenting stress: | |||||||
| Parent life restrictions | 22.98 (7.44) | 25.29 (9.18) | 21.49 (8.44) | 26.53 (9.02) | 5.82* | −0.53 | −0.44 |
| Parent incompetence/guilt | 21.05 (5.93) | 19.93 (5.68) | 19.61 (6.21) | 18.21 (5.46) | 0.40 | 0.14 | 0.13 |
| Relationship with spouse/partner | 21.22 (7.75) | 24.21 (8.31) | 19.62 (6.94) | 24.46 (8.29) | 7.05* | −0.59 | −0.37 |
| Mindful parenting: | |||||||
| Present-centered emotional awareness | 7.44 (1.30) | 7.83 (1.25) | 7.90 (1.11) | 7.52 (1.33) | 6.65* | 0.57 | 0.46 |
| Present-centered attention | 6.73 (1.32) | 6.57 (1.47) | 6.73 (1.36) | 6.93 (1.33) | 1.87 | −0.30 | −0.25 |
| Non-reactivity | 6.24 (1.32) | 6.50 (1.44) | 6.98 (1.27) | 6.90 (1.32) | 0.83 | 0.20 | 0.10 |
| Non-judgemental acceptance | 7.95 (1.28) | 7.69 (1.35) | 8.05 (1.34) | 7.98 (1.33) | 0.28 | −0.12 | −0.12 |
| Parent-adolescent relationship quality | 47.18 (9.57) | 46.90 (9.64) | 50.41 (7.74) | 47.17 (10.27) | 6.51* | 0.56 | 0.45 |
| PAIT measures | |||||||
| Observed parental warmth (n = 73) | 3.05 (1.09) | 2.79 (0.84) | 2.97 (1.04) | 2.76 (0.83) | 0.65 | 0.19 | 0.12 |
| Observed negative parenting (n = 73) | 1.25 (0.44) | 1.46 (0.55) | 1.32 (0.78) | 1.41 (0.64) | 0.07 | −0.06 | −0.03 |
| Parent negative emotion response (n = 77) | 18.43 (15.00) | 17.31 (16.87) | 12.37 (12.61) | 17.50 (15.75) | 3.93† | −0.45 | −0.33 |
Note. PM indicates Parenting Mindfully, PE indicates Parent Education, MI indicates Multiple Imputation. PM versus PE (ANCOVA) indicates intervention group effects on post-intervention measures, covarying pre-intervention measures.
p < .05,
p < .10
For parenting stress, ANCOVAs found significant intervention group effects for two subscales. Mothers in PM reported lower parenting stress related to parent life restrictions and to relationship with spouse/partner than PE mothers at post-intervention, with medium effect sizes (see Table 1). Significant intervention effects were not found for parenting stress related to parent incompetence/guilt. In secondary MI analyses, the parent life restrictions finding remained significant with a medium effect size, but the relationship with spouse/partner finding fell to a trend but with a medium effect size.
For mindful parenting, ANCOVAs found a significant intervention group effect for one subscale. Mothers in PM reported higher present-centered emotional awareness in parenting than mothers in PE at post-intervention, with a medium effect size (see Table 1). In secondary MI analyses, this finding remained significant with a medium effect size. Significant intervention effects were not found for the other three mindful parenting subscales (present-centered attention, non-reactivity, non-judgmental acceptance).
For parent-adolescent relationship quality, a significant intervention group effect was found, with mothers in PM reporting higher relationship quality than mothers in PE at post-intervention with a medium effect size. In secondary MI analyses, this finding remained significant with a medium effect size.
Laboratory PAIT task measures.
Significant intervention effects were not found for observed parenting behavior or parent negative emotional responses in PAIT.
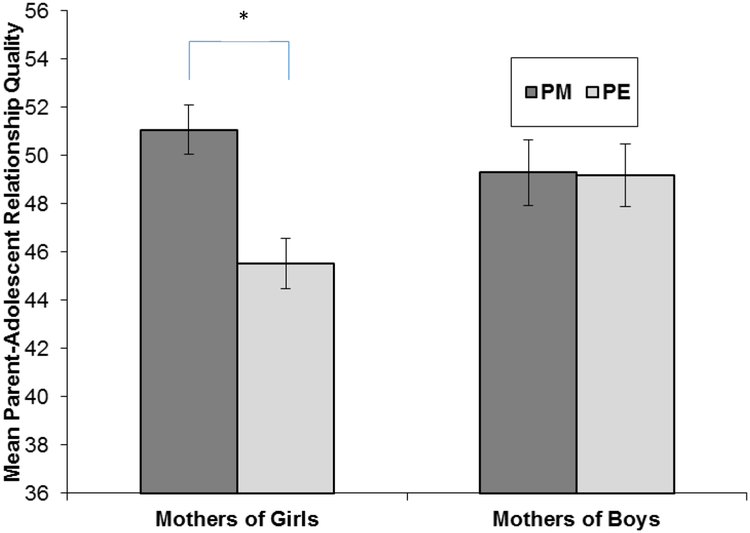
Moderation by Adolescent Gender and Age
ANCOVAs found significant adolescent gender moderation of intervention effects for three outcomes. Moderation by adolescent age was not found for any outcome. First, ANCOVAs found a significant intervention group by adolescent gender interaction effect on parent-adolescent relationship quality, F(1, 78) = 5.15, p = .03 (see Figure 1). Follow-up ANCOVAs were conducted separately for mothers of girls and mothers of boys. For mothers of girls, mothers in PM reported better relationship quality than mothers in PE at post-intervention, F(1, 40) = 14.31, p = .001, with a large effect size (d = 1.16). Intervention effects were not significant for mothers of boys, F(1, 37) = .004, p = .95. In secondary MI analyses, the group by gender interaction for parent-adolescent relationship quality fell out of significance (p = .16).
Fig. 1.
Estimated marginal means for parent-adolescent relationship quality for mothers of girls and mothers of boys in the Parenting Mindfully (PM) and Parent Education (PE) groups at post-intervention, controlling for pre-intervention scores
* indicates significant difference (p < .05) between two groups
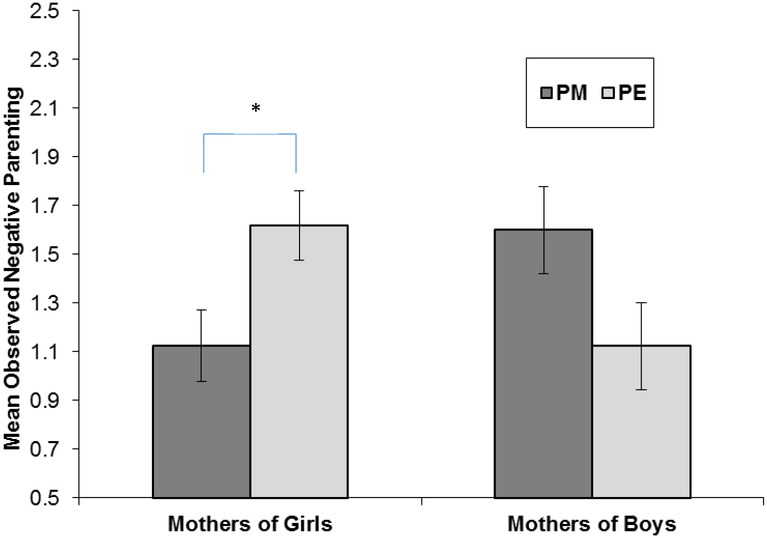
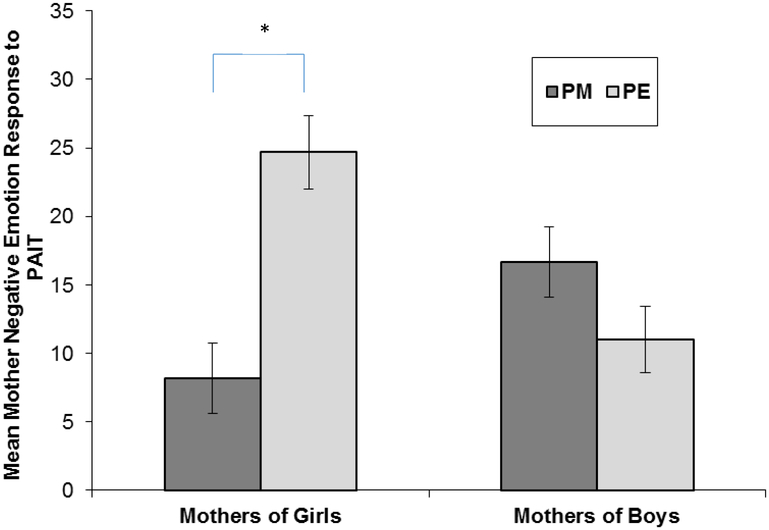
Second, ANCOVAs found a significant intervention group by adolescent gender effect on observed negative parenting in the laboratory PAIT task, F(1, 68) = 10.15, p = .002 (see Figure 2). In secondary MI analyses, this finding remained significant (p < .02). For mothers of girls, mothers in PM showed less negative parenting than mothers in PE at post-intervention, F(1, 34) = 6.20, p = .02, with a large effect size (d = −0.82, d in MI analysis = −0.65). Intervention effects were not significant for mothers of boys (F[1, 33] = 4.00, p = .05), but the pattern of results for boys suggested, unexpectedly, higher negative parenting for mothers of boys in PM versus the PE group. Third, ANCOVAs found a significant intervention group by adolescent gender effect on mothers’ negative emotional responses to PAIT, F(1, 72) = 18.99, p < .001. In secondary MI analyses, this finding remained significant (p = .002). For mothers of girls, mothers in PM reported lower negative emotion in response to PAIT than mothers in PE at post-intervention, F(1, 36) = 19.77, p < .001, with a large effect size (d = −1.43), d in MI analysis = −1.04. Intervention effects were not significant for mothers of boys, (F(1, 35) = 2.61, p = .12.
Fig. 2.
Estimated marginal means for observed maternal negative parenting behavior in PAIT task for mothers of girls and mothers of boys in the Parenting Mindfully (PM) and Parent Education (PE) groups at post-intervention, controlling for pre-intervention scores
* indicates significant difference (p < .05) between two groups
Discussion
The present study was one of the first randomized controlled trials (RCTs) examining effects of a parenting-focused mindfulness intervention for highly stressed parents of adolescents. In addition, the study uniquely examined intervention effects both on reported parenting stress/mindful parenting and on in-the-moment parenting behaviors and emotional responses in a laboratory parent-adolescent interaction task (PAIT). Findings indicated that the Parenting Mindfully (PM) intervention, compared to a minimal-intervention Parent Education (PE) control, increased mothers’ own mindfulness, positively impacted several (but not all) domains of parenting stress and mindful parenting, and improved parent-adolescent relationship quality from pre- to post-intervention. The PM intervention also decreased observed negative parenting behavior and negative emotional responses in PAIT for mothers of girls, but not mothers of boys. Effects sizes for PM intervention effects were medium to large and findings did not differ across adolescent age group from early to middle adolescence.
PM Intervention Effects
The finding that the PM intervention increased mothers’ mindfulness with a medium effect size (although it fell to a trend in secondary MI analyses) is consistent with (and extends to adolescents) Benn et al.’ (2012) RCT of mindfulness training for parents and teachers of special-needs school-aged children and with Altmaier and Maloney’s (2007) non-controlled study of a mindful parenting program for parents of preschoolers. It is also consistent with theory that practice in meditation and informal mindfulness should increase present-centered awareness and attention (Shapiro et al. 2006). PM mothers’ increased mindfulness may have affected their parenting, leading to the improvements found in mindful parenting and parent-adolescent relationship quality. Inconsistent with prior RCT studies of mindfulness training interventions delivered to parents (Benn et al. 2012; Neece 2014), the PM intervention did not significantly decrease parent stress (general perceived life stress), although it decreased two aspects of parenting stress (stress related to parenting). The particular focus in PM on applying mindfulness to parent-youth interactions may have more strongly affected parenting stress than general life stress.
The PM intervention, compared to PE, decreased parenting stress related to perceiving that one has a high level of life restrictions due to caring for the adolescent and related to negative effects of parenting on one’s relationship with one’s spouse or partner with medium effect sizes (although the latter finding fell to a trend in the MI analyses). These findings are consistent with Coatsworth et al.’ (2015) RCT finding that mindfulness-enhanced parenting training reduced parenting stress (as indexed by daily hassles related to parenting), although Coatsworth et al.’ finding was stronger for fathers than mothers. Inconsistent with one prior study (Bögels et al. 2014), the PM intervention did not significantly reduce parenting stress related to incompetence/guilt. As shown in Table 1, parenting stress related incompetence/guilt decreased slightly (approximately 1 unit) for both PM and PE mothers, suggesting that the education provided on adolescent development and the family may have been equivalent to mindfulness training in leading to greater perceived competence. In contrast, the PM intervention’s focus on meditation and increasing compassion and non-judgmental acceptance may have specifically enabled parents to have greater acceptance and tolerance for changes in their adolescent’s behavior that could restrict their lives and to have greater tolerance for behaviors of their spouse/partner.
The PM intervention, compared to PE, improved mothers’ mindful parenting in the domain of present-centered emotional awareness in parenting, which includes awareness of one’s own emotions during parenting and awareness of the adolescent’s emotions. The PM intervention did not significantly affect present-centered attention, non-reactivity, and nonjudgmental acceptance in parenting. The PM intervention may have the strongest effects on emotional aspects of parenting, including emotional awareness and also mothers’ negative emotional reactivity to PAIT for mothers of girls (as discussed below). Consistent with this, Coatsworth et al. (2015) found that mindfulness-enhanced parent training improved several aspects of mindful parenting for fathers, but the most consistent improvements (across time-point and reporter) were for emotional awareness of youth. It may be that our focus on meditation particularly affected bottom-up emotional arousal systems rather than top-down attentional systems.
Finally, the PM intervention, compared to PE, led to increases in parent-adolescent relationship quality, including closeness and warmth in the relationship. Notably, this effect was largely driven by mothers of girls (as discussed below). This finding is consistent with theory that mindful parenting interventions may especially help improve closeness in relationships with children through leading parents to be open to experiencing closeness with others, and having lower judgment and greater compassion for youth (e.g., Duncan et al. 2009).
Moderation by Gender
We found moderation of intervention effects by adolescent gender, for mother-reported parent-adolescent relationship quality (although this fell out of significance in MI analyses) and for mothers’ observed negative parenting behaviors and negative emotional responses in the laboratory PAIT interaction task. Adolescent gender did not moderate intervention effects on mother’s mindfulness, parenting stress, and mindful parenting, suggesting that gender differences were most pronounced for relationship closeness and in-the-moment negative behaviors and emotions. Our finding of moderation is consistent with research finding gender moderation of effects of traditional parent training interventions (e.g., Barrera et al. 2002) and builds on this by finding gender moderation of a parenting-focused mindfulnessg intervention.
Since the present study only included mothers, adolescent gender moderation essentially reflected that mother-daughter dyads benefitted more than mother-son dyads. Mother-daughter relationships tend to be more intimate in childhood and adolescence than other family dyads (Russell & Saebel 1997). Mother-daughter relationships also, paradoxically, tend to be more conflictual than other family dyads during adolescence (Furman & Buhrmester 1992). Thus, increasing parent mindfulness, including decreasing negative emotional reactivity to normative adolescent behavior and increasing compassion towards the adolescent, may have been particularly impactful in decreasing conflict and improving relationship quality for the close but conflictual mother-daughter relationships.
Limitations
While the present study had several strengths (e.g., RCT design, use of a laboratory interaction task), there are a few limits. First, the study examined pre- to post-intervention effects on parenting stress and parenting. Future studies should examine whether these effects on parenting prevent adolescent psychological symptoms through a longer follow-up. Second, the present study did not include fathers. Third, the PE control group was a minimal intervention control with only 3 sessions. Future RCTs should compare PM to a more intensive control group. Finally, parents with higher stress levels were less likely to complete post-intervention sessions. It may be that they dropped from the study because the PM intervention did not work well for them. To explore this, we examined (for the completers) if parent stress moderated intervention outcomes. We found that parents with higher stress benefitted equally or more than low-stress parents, suggesting that their attrition was not due to lack of PM benefit. However, future studies should explore this.
Summary and Implications
This study extends prior research on mindfulness programs for parents of young children and three trials for parents of early adolescents to suggest that mindfulness programs also work for parents of early to middle adolescents and can affect both reported parenting and in-the-moment observed parenting and parent emotion in the laboratory. This study found that the Parenting Mindfully (PM) intervention improved parent mindfulness, reduced aspects of parenting stress, and improved present-focused emotional awareness in parenting and parent-adolescent relationship quality for highly stressed mothers of adolescents from pre- to post-intervention compared to a minimal intervention control. The PM intervention also reduced observed negative parenting and negative emotional reactivity in a laboratory parent-adolescent interaction task for mothers of girls. Given the established association between parenting stress/parenting and adolescent psychopathology (Barnes et al. 2000), PM intervention effects on parenting stress and parenting may lead to prevention of psychopathology in adolescents.
Notably, the PM intervention particularly impacted emotional aspects of parenting, including increasing emotional awareness in parenting and feelings of relationship closeness, and decreasing negative emotion in parent-adolescent interactions (for girls). Mindfulness training may uniquely impact emotional functioning in parenting and thus may be a good complement to more cognitively-mediated parent training programs. Given the importance of emotional aspects of parenting to child development, mindfulness interventions thus may have important utility. In addition, the present study findings that effects of PM on observed negative parenting, parent negative emotional responses to PAIT, and parent-adolescent relationship quality were moderated by adolescent gender suggests that adolescent gender is an important factor to consider in designing and testing mindful parenting interventions. Future research should examine this further to develop gender-sensitive interventions. Overall, by reducing parenting stress, improving emotional awareness in parenting, improving parent-adolescent relationship closeness, and, for mothers of girls, reducing negative parenting behavior and parent emotion, these results suggest that mindful parenting interventions have potential to prevent the increases in psychological problems and risk behaviors that occur in middle to late adolescence.
Supplementary Material
Fig. 3.
Estimated marginal means for mother negative emotional response to PAIT task for mothers of girls and mothers of boys in the Parenting Mindfully (PM) and Parent Education (PE) groups at post-intervention, controlling for pre-intervention scores
* indicates significant difference (p < .05) between two groups
Parenting-focused mindfulness intervention reduces stress and improves parenting in highly-stressed mothers of adolescents
Acknowledgements
The authors gratefully acknowledge the study sponsor, the participating families, and the study research assistants, particularly Fran Faundez, Juliana Jacangelo, Corynne Ross, and Amysue Hansen.
Funding: Support for this project was provided by the National Institute on Drug Abuse (NIDA) through grants R34-DA-034823 (PI: Chaplin) and F31-DA-041790 (PI: Turpyn).
Footnotes
Compliance with Ethical Standards
The present study was approved by the University’s Institutional Review Board and therefore was performed in accordance with the ethical standards laid of the institutional review board and with the 1964 Helsinki declaration and its later amendments.
Informed Consent Statement
Informed consent was obtained for all individual participants included in the study.
Conflicts of Interest: Author Sinha is on the scientific advisory board for Embera NeuroTherapeutics, Inc. There are no other conflicts of interest to declare.
Contributor Information
Tara M. Chaplin, Department of Psychology, George Mason University, Fairfax, VA 22030;.
Caitlin C. Turpyn, Department of Psychology, George Mason University, Fairfax, VA 22030;
Sarah Fischer, Department of Psychology, George Mason University, Fairfax, VA 22030;.
Alexandra M. Martelli, Department of Psychology, George Mason University, Fairfax, VA 22030;
Corynne E. Ross, Department of Psychology, George Mason University, Fairfax, VA 22030;
Richard N. Leichtweis, Inova Kellar Center, Fairfax, VA 22030;
Adam Bryant Miller, Department of Psychology, George Mason University, Fairfax, VA 22030;.
Rajita Sinha, Department of Psychiatry, Yale University School of Medicine, New Haven, CT 06511.
References
- Altmaier E, & Maloney R (2007). An initial evaluation of a mindful parenting program. Journal of Clinical Psychology, 63(12), 1231–1238. [DOI] [PubMed] [Google Scholar]
- Barnes GM, Reifman AS, Farrell MP, & Dintcheff BA (2000). The effects of parenting on the development of adolescent alcohol misuse: A six-year wave latent growth model. Journal of Marriage & the Family, 62(1), 175–186. [Google Scholar]
- Barrera M, Biglan A, Taylor TK, Gunn BK, Smolkowski K, Black C, et al. (2002). Early elementary school intervention to reduce conduct problems: A randomized trial with Hispanic and non-Hispanic children. Prevention Science, 3(2), 83–94. [DOI] [PubMed] [Google Scholar]
- Belsky J, Woodworth S, & Crnic K (1996). Trouble in the second year: Three questions about family interaction. Child Development, 67(2), 556–578. [PubMed] [Google Scholar]
- Benn R, Akiva T, Arel S, & Roeser RW (2012). Mindfulness training effects for parents and educators of children with special needs. Developmental Psychology, 48(5), 1476. [DOI] [PubMed] [Google Scholar]
- Bögels SM, Hellemans J, van Deursen S, Römer M, & van der Meulen R (2014). Mindful parenting in mental health care: Effects on parental and child psychopathology, parental stress, parenting, coparenting, and marital functioning. Mindfulness, 5(5), 536–551. [Google Scholar]
- Brewer JA, Sinha R, Chen JA, Michalsen RN, Babuscio TA, Nich C, et al. (2009). Mindfulness training and stress reactivity in substance abuse: Results from a randomized, controlled Stage I pilot study. Substance Abuse, 30(4), 306–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW & Ryan RM (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84(4), 822–848. [DOI] [PubMed] [Google Scholar]
- Chan Y (1994). Parenting stress and social support of mothers who physically abuse their children in Hong Kong. Child Abuse and Neglect, 18(3), 261–269. [DOI] [PubMed] [Google Scholar]
- Chaplin TM, Hong KA, Bergquist K, & Sinha R (2008). Gender differences in response to emotional stress: An assessment across subjective, behavioral, and physiological domains and relations to alcohol craving. Alcoholism: Clinical and Experimental Research, 32(7), 1242–1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coatsworth JD, Duncan LG, Greenberg MT, & Nix RL (2010). Changing parent’s mindfulness, child management skills and relationship quality with their youth: Results from a randomized pilot intervention trial. Journal of Child and Family Studies, 19(2), 203–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coatsworth JD, Duncan LG, Nix RL, Greenberg MT, Gayles JG, Bamberger KT, et al. (2015). Integrating mindfulness with parent training: Effects of the mindfulness-enhanced strengthening families program. Developmental Psychology, 51(1), 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. [PubMed] [Google Scholar]
- Crnic KA, Gaze C, & Hoffman C (2005). Cumulative parenting stress across the preschool period: Relations to maternal parenting and child behaviour at age 5. Infant and Child Development, 14(2), 117–132. [Google Scholar]
- Deater-Deckard K (1998). Parenting stress and child adjustment: Some old hypotheses and new questions. Clinical Psychology: Science and Practice, 5(3), 314–332. [Google Scholar]
- de Bruin EI, Zijlstra BJ, Geurtzen N, van Zundert RM, van de Weijer-Bergsma E, Hartman EE, et al. (2014). Mindful parenting assessed further: Psychometric properties of the Dutch version of the Interpersonal Mindfulness in Parenting Scale (IM-P). Mindfulness, 5(2), 200–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dix T (1991). The affective organization of parenting: Adaptive and maladaptive processes. Psychological Bulletin, 110(1), 3–25. [DOI] [PubMed] [Google Scholar]
- Dumas JE (2005). Mindfulness-based parent training: Strategies to lessen the grip of automaticity in families with disruptive children. Journal of Clinical Child & Adolescent Psychology, 34(4), 779–791. [DOI] [PubMed] [Google Scholar]
- Duncan LG (2007). Assessment of mindful parenting among parents of early adolescents: Development and validation of the Interpersonal Mindfulness in Parenting Scale. Doctoral dissertation, The Pennsylvania State University. Retrieved from https://etda.libraries.psu.edu/ [Google Scholar]
- Duncan LG, Coatsworth JD, & Greenberg MT (2009). A model of mindful parenting: Implications for parent-child relationships and prevention research. Clinical Child and Family Psychology Review, 12(3), 255–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felver JC, Tipsord JM, Morris MJ, Racer KH, & Dishion TJ (2017). The effects of mindfulness-based intervention on children’s attention regulation. Journal of Attention Disorders, 21(10), 872–881. [DOI] [PubMed] [Google Scholar]
- Furman W, & Buhrmester D (1992). Age and sex differences in perceptions of networks of personal relationships. Child development, 63(1), 103–115. [DOI] [PubMed] [Google Scholar]
- Galambos NL, Barker ET, & Almeida DM (2003). Parents do matter: Trajectories of change in externalizing and internalizing problems in early adolescence. Child Development, 74(2), 578–594. [DOI] [PubMed] [Google Scholar]
- Gardner F, Hutchings J, Bywater T, & Whitaker C (2010). Who benefits and how does it work? Moderators and mediators of outcome in an effectiveness trial of a parenting intervention. Journal of Clinical Child & Adolescent Psychology, 39(4), 568–580. [DOI] [PubMed] [Google Scholar]
- Geurtzen N, Scholte RH, Engels RC, Tak YR, & van Zundert RM (2015). Association between mindful parenting and adolescents’ internalizing problems: Nonjudgmental acceptance of parenting as core element. Journal of Child and Family Studies, 24(4), 1117–1128. [Google Scholar]
- Gillham JE, Reivich KJ, Freres DR, Chaplin TM, Shatté A, Samuels B, et al. (2007). School-based prevention of depressive symptoms: Effectiveness and specificity of the Penn Resiliency Program. Journal of Consulting and Clinical Psychology, 75(1), 9–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottman JM, Fainsilber Katz L, & Hooven C (1997). Meta-emotion: How families communicate emotionally. Mahwah, NJ: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, & Lillis J (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44(1), 1–25. [DOI] [PubMed] [Google Scholar]
- Hoge EA, Bui E, Marques L, Metcalf CA, Morris LK, Robinaugh DJ, et al. (2013). Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: Effects on anxiety and stress reactivity. The Journal of clinical psychiatry, 74(8), 786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyde JS (2005). The gender similarities hypothesis. American Psychologist, 60(6), 581–592. [DOI] [PubMed] [Google Scholar]
- Izard CE (1972) Patterns of emotions: A new analysis of anxiety and depression. New York, NY: Academic Press, Inc. [Google Scholar]
- Kabat-Zinn J (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General hospital psychiatry, 4(1), 33–47. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J (1990). Full castrophe living: Using the wisdom of your body and mind to face stress, pain and illness. New York, NY: Delacorte Press. [Google Scholar]
- Kabat-Zinn M & Kabat-Zinn J (1997). Everyday blessings: The inner work of mindful parenting. New York, NY: Hyperion. [Google Scholar]
- Kabat-Zinn J, Massion A, Kristeller J, Peterson L, Fletcher K, Pbert L, et al. (1992). Effectiveness of a meditation-based stress reduction program on the treatment of anxiety disorders. American Journal of Psychiatry, 149(7), 936–943. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J, Wheeler E, Light T, Skillings Z, Scharf MJ, Cropley TG, et al. (1998). Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy (PUVA). Psychosomatic Medicine, 60(5), 625–632. [DOI] [PubMed] [Google Scholar]
- Kelley SJ (1992). Parenting stress and child maltreatment in drug-exposed children. Child Abuse & Neglect, 16(3), 317–328. [DOI] [PubMed] [Google Scholar]
- LaGasse LL, Neal AR, & Lester BM (2005). Assessment of infant cry: Acoustic cry analysis and parental perception. Developmental Disabilities Research Reviews, 11(1), 83–93. [DOI] [PubMed] [Google Scholar]
- Laursen B, & DeLay D (2011). Parent-child Relationship. Encyclopedia of adolescence (Vol. 2, pp. 233–240). London, England: Elsevier Inc. [Google Scholar]
- Lavigne JV, LeBailly SA, Gouze KR, Cicchetti C, Jessup BW, Arend R, et al. (2007). Predictor and moderator effects in the treatment of oppositional defiant disorder in pediatric primary care. Journal of Pediatric Psychology, 33(5), 462–472. [DOI] [PubMed] [Google Scholar]
- Little RJA, & Rubin DB (2002). Statistical analysis with missing data (2nd ed.). New York, NY: John Wiley & Sons, Inc. [Google Scholar]
- Lundahl B, Risser H, & Lovejoy MC (2006). A meta-analysis of parent training: Moderator and follow up effects. Clinical Psychology Review, 26(1), 86–104. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. (2012). Family Checkup: Positive Parenting Prevents Drug Abuse. Bethesda, MD: National Institutes of Health. Retrieved from https://www.drugabuse.gov/family-checkup [Google Scholar]
- Neece CL (2014). Mindfulness‐based stress reduction for parents of young children with developmental delays: Implications for parental mental health and child behavior problems. Journal of Applied Research in Intellectual Disabilities, 27(2), 174–186. [DOI] [PubMed] [Google Scholar]
- Parent J, McKee LG, Rough JN, & Forehand R (2016). The association of parent mindfulness with parenting and youth psychopathology across three developmental stages. Journal of Abnormal Child Psychology, 44(1), 191–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasley K, & Gecas V (1984). Stresses and satisfactions of the parental role. Journal of Counseling & Development, 62(7), 400–404. [Google Scholar]
- Prinz RJ, Foster S, Kent RN, & O’Leary KD (1979). Multivariate assessment of conflict in distressed and nondistressed mother-adolescent dyads. Journal of Applied Behavioral Analysis, 12(4), 691–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson EB, David SL, & Rao SA (2003). Preventing drug use among children and adolescents: A research-based guide for parents, educators, and community leaders. Bethesda, MD: National Institute on Drug Abuse. [Google Scholar]
- Rudolph KD, Troop-Gordon W, & Granger DA (2010). Peer victimization and aggression: Moderation by individual differences in salivary cortisol and alpha-amylase. Journal of Abnormal Child Psychology, 38(6), 843–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell A, & Saebel J (1997). Mother–son, mother–daughter, father–son, and father–daughter: Are they distinct relationships? Developmental Review, 17(2), 111–147. [Google Scholar]
- Sawyer-Cohen JA, & Semple RJ (2010). Mindful parenting: A call for research. Journal of Child and Family Studies, 19(2), 145–151. [Google Scholar]
- Segal ZV, Williams JMG, & Teasdale JD (2012). Mindfulness-based cognitive therapy for depression. New York, NY: Guilford Press. [Google Scholar]
- Shapiro SL, Carlson LE, Astin JA, & Freedman B (2006). Mechanisms of mindfulness. Journal of clinical psychology, 62(3), 373–386. [DOI] [PubMed] [Google Scholar]
- Sheeber L Hops H, Alpert A, Davis B, & Andrews J (1997). Family support and conflict: Prospective relations to adolescent depression. Journal of Abnormal Child Psychology, 25(4), 333–344. [DOI] [PubMed] [Google Scholar]
- Shelleby EC, & Shaw DS (2014). Outcomes of parenting interventions for child conduct problems: A review of differential effectiveness. Child Psychiatry & Human Development, 45(5), 628–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheras PR, Abidin RR, & Konold TR (1998) Stress Index for Parents of Adolescents. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Singh NN, Lancioni GE, Winton ASW, Fisher BC, Wahler RG, McAleavey K, et al. (2006). Mindful parenting decreases aggression, noncompliance, and self-injury in children with autism. Journal of Emotional and Behavioral Disorders, 14, 169–177. [Google Scholar]
- Singh NN, Lancioni GE, Winton ASW, Singh J, Curtis WJ, Wahler RG, et al. (2007). Mindful parenting decreases aggression and increases social behavior in children with developmental disabilities. Behavior Modification, 31(6), 749–771. [DOI] [PubMed] [Google Scholar]
- Singh NN, Singh AN, Lancioni GE, Singh J, Winton ASW, & Adkins AD (2010). Mindfulness training for parents and their children with ADHD increases the children’s compliance. Journal of Child and Family Studies, 19(2), 157–166. [Google Scholar]
- Spoth R, Redmond C, & Shin C (2001). Randomized trial of brief family interventions for general populations: Adolescent substance use outcomes 4 years following baseline. Journal of Counseling and Clinical Psychology, 69(4), 627–642. [DOI] [PubMed] [Google Scholar]
- Steinberg L (2001). We know some things: Parent–adolescent relationships in retrospect and prospect. Journal of Research on Adolescence, 11(1), 1–19. [Google Scholar]
- Steinberg L Fletcher A & Darling N (1994). Parental monitoring and peer influences on adolescent substance use. Pediatrics, 93(6), 1060–1064. [PubMed] [Google Scholar]
- Teasdale JD, Segal Z, Williams JM, Ridgeway VA, Soulsby JM, & Lau M (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology, 68(4), 615–623. [DOI] [PubMed] [Google Scholar]
- Turpyn CC, & Chaplin TM (2016). Mindful parenting and parents’ emotion expression: Effects on adolescent risk behaviors. Mindfulness, 7(1), 246–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turrisi R, Larimer ME, Mallett KA, Kilmer JR, Ray AE, Mastroleo NR, et al. (2009). A randomized clinical trial evaluating a combined alcohol intervention for high-risk college students. Journal of Studies on Alcohol and Drugs, 70(4), 555–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visconti KJ, Saudino KJ, Rappaport LA, Newburger JW, & Bellinger DC (2002). Influence of parental stress and social support on the behavioral adjustment of children with transposition of the great arteries. Development and Behavioral Pediatrics, 23(5), 314–321. [DOI] [PubMed] [Google Scholar]
- Wills TA & Yeager AM (2003). Family factors and adolescent substance use: Models and mechanisms. Current Directions in Psychological Science, 12(6), 222–226. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.