Abstract
An evolutionary perspective provides a unifying explanation for the modifiable risk factors and lifestyle-based interventions for the leading causes of morbidity and mortality globally. Non-communicable diseases develop from an evolutionary mismatch between the prior environment and modern patterns of behavior; however, it is unclear whether an evolutionary mismatch narrative could promote positive behavior change in patients. We hypothesize that educating patients about evolutionary mismatch could augment efforts to improve healthful behavior. Specifically, explaining the ‘why’ behind what is being recommended could promote health literacy and adherence. Furthermore, we offer suggestions of how clinicians could educate patients about evolutionary mismatch for key-lifestyle factors, diet and physical activity, as well as several specific modern diseases. We also consider how to sidestep patients’ skepticism of evolutionary theory. Here, we lay the groundwork for research on how educating patients with an evolutionary mismatch narrative could impact health behaviors and improve outcomes.
Keywords: evolutionary mismatch, patient education, lifestyle medicine, behavior change
INTRODUCTION AND CLINICAL NEED
Clinician recommendations do not always translate directly into patient behavior change [1]; however, patient education remains a necessary step for behavior change [2]. It is possible that an evolutionary medicine (EM) perspective may promote positive behavior change. EM applies evolutionary theory to better understand why humans are vulnerable to diseases and how to improve the prevention and treatment of those diseases [3]. For example, EM principles have shown great promise in transforming cancer treatment [4] and management of antibiotic resistance [5]. However, there is a glaring gap between the use of EM in research settings and the implementation of EM principles into lifestyle medicine and behavior change.
Clinicians can use EM principles in their patient education to increase health literacy. The Institute of Medicine defines ‘Health Literacy’ as the degree to which individuals have the capacity to obtain, process, and understand basic health information and services to make appropriate health decisions [6]. Two types of evidence increase health literacy among patients: statistical and narrative evidence. Statistical evidence provides quantitative information, whereas narrative evidence presents a cohesive story to educate the patient [7]. A meta-analysis comparing the effectiveness of these two educational strategies revealed that narrative evidence produces greater intentions for behavioral change among patients [8]. Moreover, strong evidence shows narrative interventions actually increase health-promoting behaviors [9]. We propose that adding an evolutionary perspective to narrative evidence could augment behavior change, which has not been directly tested.
Elucidating the ultimate causes of disease may empower patients to apply EM to their lifestyle in areas where mechanistic explanations have fallen short in the past. Evolutionary mismatch provides a unifying framework for understanding the epidemiological patterns and lifestyle-based treatments of the most prevalent ‘diseases of civilization’ (e.g. type 2 diabetes, cardiovascular disease, obesity; [10]). Here, we explore the hypothesis that providing an evolutionary narrative behind pathologies arising from evolutionary mismatch will grant patients a deeper understanding that will in turn facilitate meaningful behavior change. We describe how education on evolutionary mismatch might motivate behavior change by increasing adherence to various lifestyle prescriptions. We then provide practical materials for clinicians to incorporate evolutionary theory into their practice while avoiding controversy by tailoring explanations to a patient’s particular level of evolutionary acceptance. Finally, we consider how future investigators might implement this behavior change hypothesis into a research setting.
SUPPORT FOR EVOLUTIONARY MISMATCH EDUCATION
The field of medicine has largely focused on the proximate, or mechanistic, causes of many chronic diseases. However, an evolutionary perspective explores why we are vulnerable to disease in the first place. For example, the main mechanistic cause of obesity is a surplus of calories, whereas numerous evolutionary hypotheses have been presented for its ultimate cause, such as humans’ ability to store calories for potential future famines [11]. While the effects of evolutionary mismatch education on medical patients has yet to be tested, several EM advocates have stated the potential benefits of educating patients on EM or mismatch (see Table 1). Future research is needed to assess the efficacy of this education.
Table 1.
Support in the literature for educating patients on evolutionary mismatch
| Author | Excerpt |
|---|---|
| Enam and Hasmi, 2018 [46] | ‘It is…doctors (and their patients) to whom understanding the evolutionary basis of disease is most relevant’. |
| Eaton and Eaton, 2017 [47] | ‘The public has been told ad nauseum that exercise and weight control are essential for preventing T2DM, but they have not been provided an understandable, convincing link between these factors and T2DM’s biological basis. An evolutionary perspective, together with the concept of insulin receptor competition, may fill that need’. |
| Perlman, 2013 [3] | ‘…evolutionary explanations of disease are important because patients often want to know why they have the diseases they have’. |
| Perlman, 2011 [48] | ‘Nonetheless, understanding that manifestations of disease may be adaptations provides a richer understanding of these manifestations, and it may be helpful to patients to learn that their symptoms, though distressing, are part of their healthy coping with their disease’. |
| Naugler, 2009 [49] | ‘…a basic knowledge of evolutionary medicine might help in explaining the causation of diseases to patients’. |
| Eaton et al., 2002 [50] | ‘…providing accurate health advice is less than half the battle; at least as important is achieving patient compliance. Providing an explanation for health promotion based on a coherent theory of how disease arises from the mismatch between our original design and our current circumstances should help’. |
The idea of evolutionary mismatch has not been confined to academia. Since the early 2000s, there has been growing interest in nutritional and exercise guidelines intended to mimic those of our ancestors, commonly known as the ‘Paleo’ or ‘Ancestral Health Movement’ [12]. The Modern Paleo Diet (MPD) is a food-group-based approach to health improvement which calls for the elimination of any foods that were not consumed by ancestral hunter-gatherers [13, 14]. Konner and Eaton [15] applied the mismatch framework to humans and developed the ‘evolutionary discordance hypothesis’, which states that the prevalence of chronic disease has increased due to a departure from the hunter-gatherer lifestyles for which we are well-adapted. The MPD is a direct application of the evolutionary discordance hypothesis [10, 16]. While there is controversy surrounding the diet’s evolutionary justification (including the fact that there is no singular ancestral diet) [17, 18], the popularity of this movement indirectly illustrates how a patients’ understanding of the mismatch hypothesis can promote changes in physical activity and nutritional behaviors [19]. Though the MPD is grounded in evolutionary theory, only four studies explicitly reported giving participants an evolutionary explanation (see Supplementary Table S1) [20–23]. MPD studies that did not specifically report giving participants an evolutionary rationale still showed physiological improvements [24–26]. Thus, the impact of mismatch education on behavior change is plausible, but unproven; nevertheless, the popularity of this dietary pattern highlights the public’s appetite for an evolutionary basis for health advice.
LIFESTYLE BEHAVIOR CHANGE VIA AN EVOLUTIONARY MISMATCH NARRATIVE
Data on the ability of lifestyle education alone to affect meaningful behavior change is mixed. A 2005 meta-analysis examined the efficacy of lifestyle intervention education in adults with diabetes and found that the intervention group had a 50% lower risk of incidence of type 2 diabetes after a 1-year follow-up [27]. In contrast, a 2013 meta-analysis found no evidence for improvement in all-cause mortality or cardiovascular outcomes in adults with type 2 diabetes following an education-based lifestyle intervention [1]. Furthermore, in a systematic review of the impact of knowledge of genetic risk on behavior, Heshka et al. [28] report that current methods of patient education are insufficient to induce favorable outcomes and that improved education strategies are needed. An evolutionary narrative can serve as a novel education strategy for translating education into behavior change.
To our knowledge, there is a single study that explored how evolutionary mismatch education impacts intentions to change behavior. Sherry (2018) [29] found that a one-time brief introduction to evolutionary biology produced a shift in high school students’ perceptions of healthy eating and led to intended dietary changes. Although, actual behavior was not measured. Sherry (2018) [29] found that explaining nutrition in an evolutionary context was necessary to change students’ perceptions of healthy eating. Our hypothesis builds upon these encouraging results.
STRATEGIES FOR CLINICIANS TO IMPROVE ADHERENCE TO BEHAVIOR CHANGE PRESCRIPTIONS
The transtheoretical model (stages of behavior change)
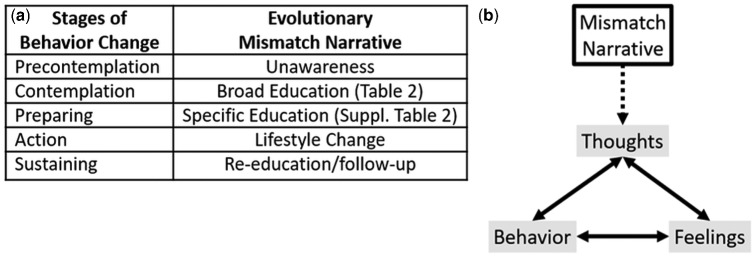
There are many ways clinicians could apply evolutionary mismatch education in clinical settings. Pairing the evolutionary mismatch narrative with evidence-based behavior change models may be an effective strategy. The transtheoretical model (TTM) describes a sequence of cognitive and behavioral steps that individuals take to change behavior ([30]; see Fig. 1a). Much work has been done to apply the TTM to nutrition and diet change [31]. A recent 2017 study found that dietary knowledge significantly motivated participants to move into later stages of behavior change, which in turn improved the outcome of glycemic control among patients with type 2 diabetes [32]. As Sherry (2018) suggests, an evolutionary perspective may cognitively promote progression in stages of behavior change. An evolutionary narrative may impact several stages of behavior change: a patient’s attitude, perception of specific behaviors, and increase self-efficacy, all of which are the precursors to lifestyle modification [33].
Figure 1.
Applying evolutionary mismatch narrative to (a) the stages of behavior change and (b) the Cognitive Behavior Change Model (CBT).
Cognitive behavior therapy model
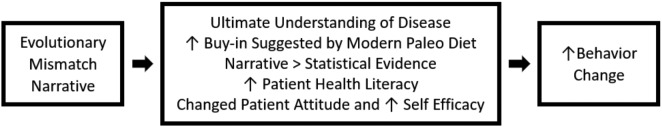
Evidence for Cognitive Behavior Therapy’s (CBT) effects on changing behavior is strong [34, 35]. Briefly, CBT is a psychotherapy treatment method that improves health behaviors by changing the way one thinks. Numerous studies have highlighted the effectiveness of CBT in improving diet, health [36, 37], and physical activity [38]. The ability of CBT to change behavior highlights the importance of education, which can alter a patient’s attitude and increase self-efficacy [33], an important step for behavior change. By explaining the ‘why’ of the patient’s disease, a mismatch narrative can help reframe a patient’s thoughts to influence their feelings and behavior in keeping with CBT (see Fig. 1b). In addition, due to the broadness of an evolutionary mismatch narrative, an integrative approach that incorporates other education techniques, specific to the patient, should be paired with this narrative to better promote behavior change [39]. A summary of the evidence to support the use of an evolutionary mismatch narrative can be found in Fig. 2.
Figure 2.
Summary of the evidence supporting the use of an evolutionary mismatch narrative to promote behavior change.
MISMATCH EDUCATION FOR DIET, PHYSICAL ACTIVITY AND VARIOUS DISEASES
Poor diet and low physical activity are strong risk factors for numerous diseases and addressing them can have a beneficial impact on disease risk or treatment. Often a ‘natural’ diet and lifestyle is thought to be healthful; however, what qualifies as ‘natural’ is unclear [40]. As Konner and Eaton (2010) [15] stated, the evolutionary (hunter-gatherer) perspective is the answer to what is a ‘natural’ diet and lifestyle for humans. Therefore, a diet and lifestyle that prevents mismatch disease would be a lifestyle that is natural. The intuitive nature of eating a ‘natural’ diet is easy to understand and lends itself to encouraging the consumption of whole, unprocessed foods that are widely recognized as inherently healthful [41]. Furthermore, sedentarism is a strong risk factor for metabolic disease that is also produced via mismatch [42]. Mismatch education may help to alleviate sedentarism by encouraging a physical activity regimen which resembles those prior to modern times. Moreover, this evolutionary mismatch perspective already aligns with numerous public health recommendations (e.g. promoting physical activity and consumption of minimally-processed whole foods; [43]). However, care must be taken to avoid the misapplication of an evolutionary perspective; for example, low-glycemic foods promoted by the MPD has been taken to an extreme and interpreted by some to mean an ultra-low carbohydrate (e.g. a carnivore diet). In rushed encounters between clinicians and patients, important nuances in dietary advice may be missed.
The implications of a mismatch narrative extend well past just diet and physical activity as mismatch contributes to numerous diseases. Supplementary Table S2 presents explanations for mismatch diseases that clinicians may find useful in explaining the specific nature of a disease to each patient. Also included is supporting evidence that treatment based on the evolutionary mismatch hypothesis is effective in alleviating each condition. A clinician could use the broader mismatch as a hook (Fig. 3) and then focus on a specific disease (Supplementary Table S2). Moreover, specific phrases can be used within patient education that convey or imply mismatch without specifically talking about evolution. Pairing examples from Supplementary Table S2 with behavior change models (Fig. 1) can provide patients with a new understanding of their diagnosis and potentially motivate them to adhere to clinicians’ recommendations. It should be noted that clinicians often recognize that education alone does not necessarily lead to behavior change, but education, per se, can be effective for some patients. To determine the effectiveness of this evolutionary mismatch narrative education, future research should compare this narrative to other education interventions and measure behavior change.
Figure 3.
Examples of words and statements and level of detail within explanations of an evolutionary mismatch narrative based on a patient’s acceptance of evolution and level of knowledge.
POTENTIAL LIMITATIONS DUE TO CONTROVERSY SURROUNDING EVOLUTION
Despite overwhelming evidence and scientific consensus, many US citizens remain unconvinced or opposed to the theory of evolution by natural selection [44]. This disconnect is an important barrier to incorporation of evolutionary explanations into patient education. For example, a survey of nutrition and dietetics professionals and students found that less than half reported that they were likely to provide an evolutionary explanation of a condition or disease to a patient or client [45]. We therefore explore how the mismatch narrative can be tailored to avoid provoking controversy among patients with barriers to acceptance of evolution. Fig. 3. outlines examples of words and statements for explaining the evolutionary narrative to patients with varying levels of evolutionary acceptance. Clinicians can still communicate evolutionary mismatch without invoking controversial perspectives that might impede patient adherence or jeopardize the patient-clinician relationship. For example, to convey change over time, a comparison between the ancestral and modern environment could be used without mentioning evolution (see Fig. 3). A clinician can solely use language intended for people who reject evolution to avoid any possible conflict. Evolutionary mismatch education does not require either the clinician or patient to have a comprehensive understanding of evolutionary theory. However, we do recognize that some clinicians may unintentionally apply evolutionary theory to excuse racist/eugenic ways of thinking. This underscores the need for including accurate evolutionary theory in medical education as well as recognition of the ableist and racist past of the medical field through misuse of evolutionary theory.
CONCLUSIONS
Evolutionary mismatch education may improve patients’ health behavior by deepening their understanding. While not always sufficient, education is a necessary step of lifestyle change. Reframing the patient’s perspective by providing an evolutionary mismatch narrative to focus on the ultimate cause—rather than just a mechanistic explanation—of a chronic disease may motivate beneficial lifestyle behavior change because patients will understand the theory behind their lifestyle prescriptions. Although evolutionary theory can be polarizing, there are simple ways that clinicians can sidestep this controversy. Given the burden of chronic diseases of civilization, research exploring this hypothesis has broad implications.
Supplementary data
Supplementary data is available at EMPH online.
Supplementary Material
Acknowledgements
The authors would like to acknowledge Diana S. Sherry and Daniel Z. Grunspan for their feedback on the manuscript.
Conflict of interest: None declared.
REFERENCES
- 1. Schellenberg ES, Dryden DM, Vandermeer B. et al. Lifestyle interventions for patients with and at risk for type 2 diabetes: a systematic review and meta-analysis. Ann Intern Med 2013;159:543–51. [DOI] [PubMed] [Google Scholar]
- 2. Arlinghaus KR, Johnston CA.. Advocating for behavior change with education. Am J Lifestyle Med 2018;12:113–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Perlman R. Evolution and medicine. Perspect Biol Med 2013;56:167–83. [DOI] [PubMed] [Google Scholar]
- 4. Aktipis CA, Boddy AM, Gatenby RA. et al. Life history trade-offs in cancer evolution. Nat Rev Cancer 2013;13:883–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Read AF, Woods RJ.. Antibiotic resistance management. Evol Med Public Heal 2014;2014:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Institute of Medicine. Health Literacy: A Prescription to End Confusion. Washington, DC: The National Academies Press, 2004. [PubMed] [Google Scholar]
- 7. Allen M, Preiss RW.. Comparing the persuasiveness of narrative and statistical evidence using meta-analysis. Int J Phytoremediation 1997;14:125–31. [Google Scholar]
- 8. Zebregs S, van den Putte B, Neijens P. et al. The differential impact of statistical and narrative evidence on beliefs, attitude, and intention: a meta-analysis. Health Commun 2015;30:282–9. [DOI] [PubMed] [Google Scholar]
- 9. Perrier MJ, Martin Ginis KA.. Changing health-promoting behaviours through narrative interventions: a systematic review. J Health Psychol 2018;23:1499–517. [DOI] [PubMed] [Google Scholar]
- 10. Carrera-Bastos P, Fontes O. et al. The western diet and lifestyle and diseases of civilization. Res Reports Clin Cardiol 2011;2011:15. [Google Scholar]
- 11. Speakman JR. Evolutionary perspectives on the obesity epidemic: adaptive, maladaptive, and neutral viewpoints. Annu Rev Nutr 2013;33:289–317. [DOI] [PubMed] [Google Scholar]
- 12. Schwartz DB, Stapell HM.. Modern cavemen? Stereotypes and reality of the ancestral health movement. J Evol Heal 2013;1:3. [Google Scholar]
- 13. Cordain L. The Paleo Diet. Hoboken: John Wiley & Sons, 2002. [Google Scholar]
- 14. Basile A, Schwartz D, Stapell HM.. Paleo then and now: a five-year follow-up survey of the ancestral health community. J Evol Heal an Ancestral Heal Soc Publ 2020;5:1–42. [Google Scholar]
- 15. Konner M, Eaton SB.. Paleolithic nutrition twenty-five years later. Nutr Clin Pract 2010;25:594–602. [DOI] [PubMed] [Google Scholar]
- 16. Cordain L, Eaton SB, Sebastian A. et al. Origins and evolution of the Western diet: health implications for the 21st century. Am J Clin Nutr 2005;81:341–54. [DOI] [PubMed] [Google Scholar]
- 17. Veile A. Hunter-gatherer diets and human behavioral evolution. Physiol Behav 2018;193:190–5. [DOI] [PubMed] [Google Scholar]
- 18. Turner BL, Thompson AL.. Beyond the Paleolithic prescription: incorporating diversity and flexibility in the study of human diet evolution. Nutr Rev 2013;71:501–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Crittenden AN, Schnorr SL.. Current views on hunter-gatherer nutrition and the evolution of the human diet. Am J Phys Anthropol 2017;162:84–109. [DOI] [PubMed] [Google Scholar]
- 20. Jönsson T, Granfeldt Y, Lindeberg S. et al. Subjective satiety and other experiences of a Paleolithic diet compared to a diabetes diet in patients with type 2 diabetes. Nutr J 2013;12:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jönsson T, Granfeldt Y, Ahrén B. et al. Beneficial effects of a Paleolithic diet on cardiovascular risk factors in type 2 diabetes: a randomized cross-over pilot study. Cardiovasc Diabetol 2009;8:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jönsson T, Ahrén B, Pacini G. et al. A Paleolithic diet confers higher insulin sensitivity, lower C-reactive protein and lower blood pressure than a cereal-based diet in domestic pigs. Nutr Metab (Lond) 2006;3:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lindeberg S, Jönsson T, Granfeldt Y. et al. A Palaeolithic diet improves glucose tolerance more than a Mediterranean-like diet in individuals with ischaemic heart disease. Diabetologia 2007;50:1795–807. [DOI] [PubMed] [Google Scholar]
- 24. Genoni A, Lo J, Lyons-Wall P. et al. A Paleolithic diet lowers resistant starch intake but does not affect serum trimethylamine-N-oxide concentrations in healthy women. Br J Nutr 2019;121:322–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Otten J, Ryberg M, Mellberg C. et al. Postprandial levels of GLP-1, GIP and glucagon after 2 years of weight loss with a Paleolithic diet: a randomised controlled trial in healthy obese women. Eur J Endocrinol 2019;180:417–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Frassetto L, Pra M, Thomas B. et al. The VA Beach Diet Study: a comparison of the effects of Plant-based, Mediterranean, Paleolithic, and DASH Diets on cardiovascular disease risk. J Evol Heal 2019;3:1–4. [Google Scholar]
- 27. Yamaoka K, Tango T.. Efficacy of lifestyle education to prevent type 2 diabetes: a meta-analysis of randomized controlled trials. Diabetes Care 2005; 28:2780–6. [DOI] [PubMed] [Google Scholar]
- 28. Heshka JT, Palleschi C, Howley H. et al. A systematic review of perceived risks, psychological and behavioral impacts of genetic testing. Genet Med 2008;10:19–32. [DOI] [PubMed] [Google Scholar]
- 29. Sherry DS. Does knowledge of evolutionary biology change high school students’ attitudes about healthy eating? Evol Educ Outreach 2019;12:1–11. [Google Scholar]
- 30. Prochaska JO, Velicer WF.. The transtheoretical model of health behavior change. Am J Health Promot 1997;12:38–48. [DOI] [PubMed] [Google Scholar]
- 31. Spahn JM, Reeves RS, Keim KS. et al. State of the evidence regarding behavior change theories and strategies in nutrition counseling to facilitate health and food behavior change. J Am Diet Assoc 2010;110:879–91. [DOI] [PubMed] [Google Scholar]
- 32. Tseng H-M, Liao S-F, Wen Y-P. et al. Stages of change concept of the transtheoretical model for healthy eating links health literacy and diabetes knowledge to glycemic control in people with type 2 diabetes. Prim Care Diabetes 2017;11:29–36. [DOI] [PubMed] [Google Scholar]
- 33. Sheeran P, Maki A, Montanaro E. et al. The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: a meta-analysis. Heal Psychol 2016;35:1178–88. [DOI] [PubMed] [Google Scholar]
- 34. Hofmann SG, Asnaani A, Vonk IJJ. et al. The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognit Ther Res 2012;36:427–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Butler AC, Chapman JE, Forman EM. et al. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev 2006;26:17–31. [DOI] [PubMed] [Google Scholar]
- 36. Miri SF, Javadi M, Lin C-Y. et al. Effectiveness of cognitive-behavioral therapy on nutrition improvement and weight of overweight and obese adolescents: a randomized controlled trial. Diabetes Metab Syndr 2019;13:2190–7. [DOI] [PubMed] [Google Scholar]
- 37. Garcia-Silva J, N Navarrete N, Peralta-Ramírez MI. et al. Efficacy of cognitive behavioral therapy in adherence to the Mediterranean diet in metabolic syndrome patients: a randomized controlled trial. J Nutr Educ Behav 2018;50:896–904. [DOI] [PubMed] [Google Scholar]
- 38. Barrett S, Begg S, O’Halloran P. et al. Integrated motivational interviewing and cognitive behaviour therapy for lifestyle mediators of overweight and obesity in community-dwelling adults: a systematic review and meta-analyses. BMC Public Health 2018;18:1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Minich DM, Bland JS.. Personalized Lifestyle Medicine: relevance for Nutrition and Lifestyle Recommendations. Sci World J 2013;2013:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Siipi H. Is Natural Food Healthy? J Agric Environ Ethics 2013;26:797–812. [Google Scholar]
- 41. Katz DL, Meller S.. Can we say what diet is best for health? Annu Rev Public Health 2014;35:83–103. [DOI] [PubMed] [Google Scholar]
- 42. Owen N, Sparling PB, Healy GN. et al. Sedentary behavior: emerging evidence for a new health risk. Mayo Clin Proc 2010;85:1138–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pontzer H, Wood BM, Raichlen DA.. Hunter-gatherers as models in public health. Obes Rev 2018;19:24–35. [DOI] [PubMed] [Google Scholar]
- 44. Miller JD, Scott EC, Okamoto S.. Science communication. Public acceptance of evolution. Science 2006;313:765–6. [DOI] [PubMed] [Google Scholar]
- 45. Basile AJ, Schwartz DB, Rigdon J. et al. Status of evolutionary medicine within the field of nutrition and dietetics. Evol Med Public Heal 2018;2018:201–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Enam SF, Hashmi S.. The importance of evolutionary medicine in developing countries: a case for Pakistan’s medical schools. Evol Med Public Heal 2018;2018:26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Eaton SB, Eaton SB.. Physical inactivity, obesity, and type 2 diabetes: an evolutionary perspective. Res Q Exerc Sport 2017;88:1–8. [DOI] [PubMed] [Google Scholar]
- 48. Perlman RL. Evolutionary biology: a basic science for medicine in the 21st century. Perspect Biol Med 2011;54:75–88. [DOI] [PubMed] [Google Scholar]
- 49. Naugler CT. Evolutionary medicine: update on the relevance to family practice. Can Fam Physician 2008;54:1265–9. [PMC free article] [PubMed] [Google Scholar]
- 50. Eaton SB, Strassman BI, Nesse RM. et al. Evolutionary health promotion. Prev Med (Baltim) 2002;34:109–18. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.