Abstract
BACKGROUND
The purpose of this study was to examine the longitudinal association between rising violent crime and elevated blood pressure (BP).
METHODS
We analyzed 217,816 BP measurements from 17,783 adults during a temporal surge in violent crime in Chicago (2014–2016). Serial observations were abstracted from the electronic health record at an academic medical center and paired to the City of Chicago Police Data Portal. The violent crime rate (VCR) was calculated as the number of violent crimes per 1,000 population per year for each census tract. Longitudinal multilevel regression models were implemented to assess elevated BP (systolic BP ≥ 140 mm Hg or diastolic BP ≥ 90 mm Hg) as a function of the VCR, adjusting for patient characteristics, neighborhood characteristics, and time effects. Secondary dependent measures included elevated heart rate, obesity, missed outpatient appointments, all-cause hospital admissions, and cardiovascular hospital admissions.
RESULTS
At baseline, the median VCR was 41.3 (interquartile range: 15.2–66.8), with a maximum rise in VCR of 59.1 over the 3-year surge period. A 20-unit rise in the VCR was associated with 3% higher adjusted odds of having elevated BP (95% confidence interval [CI]: 1.01–1.06), 8% higher adjusted odds of missing an outpatient appointment (95% CI: 1.03–1.13), and 6% higher adjusted odds of having a cardiovascular-related hospital admission (95% CI: 1.01–1.12); associations were not significant for elevated heart rate and obesity.
CONCLUSION
Rising violent crime was associated with increased BP during a temporal crime surge.
Keywords: blood pressure, cardiovascular risk, hypertension, social determinants, stress, violent crime
Numerous US cities experienced a substantial rise in violent crime between 2014 and 2016. In Chicago, despite violent crime rates (VCRs) at historic lows since the early 1990s, the number of shootings increased by 18% in 2015 and 42% in 2016 before eventually downtrending in 2017.1,2 Although this surge in violent crime has been heavily featured in the media and public discourse, its consequences on the health of affected populations have been largely overlooked. Some epidemiological studies have documented a positive association between chronic exposure to violent crime and health conditions, such as obesity and hypertension.3,4 We found in a previous cross-sectional study that patients living in the highest quartile for violent crime had 25% higher adjusted odds of elevated blood pressure (BP) compared with those living in the lowest quartile, even after adjusting for patient-, clinic-, and neighborhood-level characteristics.5
This association has been explained, in part, by the effect of violent crime on health behaviors and disease management activities. For instance, studies have documented an inverse relationship between violent crime and physical activity.4 Piro and colleagues6 examined the physical activity patterns of 3,499 elderly adults and found that fear of violence was associated with inadequate physical activity in women. Other studies have documented reductions in daily fruit and vegetable consumption7 and delays in filling prescription medications.8 Still others have pointed to the body’s response to exogenous psychosocial stressors over time.9 As Bruce McEwen describes, the body can pay a hefty price for being “forced to adapt to adverse psychological or physical situations.” 9,10 This adaptation can trigger aberrant or prolonged adrenergic activity, vascular reactivity, oxidative damage, and downstream cardiovascular processes.9,10
Despite these compelling theoretical mechanisms, studies that quantify the relationship between exposure to violent crime and cardiovascular risk have often been limited. For instance, cross-sectional studies have yielded mixed findings,4,11 possibly owing to the inconsistent use of objective versus subjective measures of both violence exposure and health. Longitudinal studies have generally analyzed relatively small sample sizes or used survey-based measures of violence exposure.12 Importantly, these studies have been limited because many residents experience little change in exogenous exposure to violent crime over time; or, they experience significant change only after moving to a new neighborhood, which can be associated with a number of observed and unobserved confounders due to selective residential sorting.13
The surge in violent crime between 2014 and 2016 created unique conditions to examine the temporal relationship between rising VCRs and elevated BP in a longitudinal sample of urban-dwelling adults. We paired police-recorded VCRs from the City of Chicago Police Data Portal with objective BP measurements abstracted from the electronic health record (EHR). By examining serial BP measurements from a relatively large panel (N = 17,783) of residentially stable adults, we sought to limit the variation of confounding neighborhood effects while maximizing the variation in exposure to violent crime. As a secondary objective, we examined associations between rising VCRs with related cardiovascular risk factors, including elevated heart rate (HR), obesity, missed outpatient appointments, and hospital admissions. We hypothesized positive associations between rising VCRs with elevated BP and related cardiovascular risk factors.
METHODS
This study was conducted using small area analysis of a 295 census tract region in Chicago, overlapping with the medical center’s catchment region. The study population was comprised of a sample of 17,783 patients seen in outpatient clinics at an urban academic medical center between January 2014 and December 2016. Patients were included if they had a stable residential address and were seen more than once during the study period. Patients were excluded if they lacked at least 1 repeated observation (i.e., BP, HR, and body mass index [BMI]) or if they lived in a census tract with fewer than 1,000 BP observations during the study period, to ensure adequate precision of effect estimates. Of the 21,179 patients meeting initial inclusion criteria, 3.0% (n = 628) were excluded due to missing repeated BP measurements and an additional 0.5% (n = 106) were excluded due to missing secondary outcome measurements (i.e., HR and BMI). Of the remaining 20,445 patients, an additional 12.6% (n = 2,662) were excluded for living in a census tract with fewer than 1,000 BP observations, largely reflecting census tracts outside the immediate catchment region of the medical center. The median number of patients per census tract was 85 (interquartile range [IQR]: 46–157) and BP measurements per census tract was 2,801 (IQR: 1,600–5,070).
This study followed the STROBE reporting guideline for observational studies, and was conducted with a waiver of informed consent and approval from the University of Chicago Institutional Review Board.
Data sources and measures
Violent crime data were obtained from the City of Chicago Police Data Portal, a publicly available and geocoded record of every incident reported to the Chicago Police Department. Data are stored by the Chicago Police Department’s Citizen Law Enforcement Analysis and Reporting System and more fully described in previously published work.5,14 These data were linked to the contemporaneous EHR of patients (aged ≥ 18 years) seen in outpatient clinics at an academic medical center.
The primary dependent variables included elevated BP (dichotomous) and systolic BP (continuous). Elevated BP was defined as systolic BP ≥ 140 mm Hg or diastolic BP ≥ 90 mm Hg. Secondary dependent variables included both health conditions and healthcare utilization outcomes. Health conditions included diastolic BP (continuous), HR (HR > 100 beats per minute [bpm] and continuous); and obesity (BMI ≥ 30 kg/m2 and continuous). Annual healthcare utilization outcomes included having at least 1 missed outpatient appointment, all-cause hospital admission, or cardiovascular hospital admission. Hospital admissions were classified as “cardiovascular” if the principal diagnosis code included any of the following: IXX, R00.[0–2, 8–9], R07.[1–2], R07.8[1–2, 9], and R07.9 in ICD-10; 39X-45X, 427.81, 427.89, 785.[0–1, 3], and 786.X in ICD-9.15
The primary independent variable included the census tract VCR per 1,000 population per year. “Violent crime” was defined based on the Chicago Police Department’s Crime Type Categories14 and included assault, battery, criminal sexual assault, robbery, and homicide. Crime counts were aggregated to the census tract level and assigned to patients as a proxy for the level of exposure. A 20-unit increase in the census tract VCR indicates 20 additional crimes per 1,000 population per year. A 20-unit standard was implemented to approximate movement between crime quartiles, given a median baseline VCR of 41. A secondary independent variable included the census tract homicide rate per 1,000 population per year. A 1-unit standard (i.e., 1 additional homicide per 1,000 population per year) was used to analyze homicide because homicides were much rarer in the sample population.
To examine how the broader citywide surge may have differentially impacted patients living in low- vs. high-crime areas, we used the citywide VCR per 100,000 population per year in supplementary analyses. We reasoned that patients living in low-crime areas may still be affected by news of violent crime, even if not occurring in their own neighborhood. A “low-crime” area was defined as a below-median crime rate in each census tract before the surge and a “high-crime” area was defined as an above-median crime rate during the same period.
Covariates, extracted from the EHR, included patient demographic characteristics, including age (continuous), gender (male or female), race/ethnicity (white non-Hispanic, black non-Hispanic, Hispanic or Latino, other race/ethnicity, unknown), and primary insurance status (private, managed care, Medicaid or dual eligible, Medicare, other, none); patient health status, including cholesterol status (total cholesterol less than or greater than 200 mg/dL); BMI (continuous), and treatment with BP medications (treatment or no treatment); neighborhood characteristics (2014 American Community Survey 5-year estimates),16 including ≥40% below the federal poverty level (FPL; high-poverty designation), ≥25% with no high school diploma, ≥50% minority race/ethnicity, and ≥10% with limited English proficiency; and fixed time effects for month and year, to account for seasonal variation and time trends. All patient-level covariates were extracted for each clinical observation (e.g., BP measurement) and may have varied with time.
Statistical analysis
Descriptive statistics were used to characterize the demographic and census tract characteristics of the sample. Primary dependent variables (elevated BP, systolic BP) and secondary dependent variables (diastolic BP, HR, BMI, and healthcare utilization) were examined as a function of the census tract VCR. Longitudinal multilevel regression models included a random effect for patient identifier and robust standard errors clustered by census tract, adjusting for patient characteristics, neighborhood characteristics, and time effects, as described previously. We tested for multicollinearity between neighborhood-level covariates using variance inflation factor (VIF); mean VIF was 1.37 with no values exceeding the standard threshold of 10.17
We also tested the relationship between VCR and dependent variables in stratified analyses by age group (<65 or ≥65 years), gender (male or female), and treatment with BP medications (treatment or no treatment). Interaction effects were tested in the full model. Statistical significance was defined as a P value < 0.05. In models examining citywide crime rates, primary dependent variables (elevated BP, systolic BP) were examined as a function of the interaction between citywide VCR and baseline violent crime status (below or above median VCR). Longitudinal regression models included the same model specifications as described previously.
Data were analyzed using Stata/SE, version 13.1 (StataCorp LP, College Station, TX) and GeoDa, version 1.10.0.12.
RESULTS
The sample population included 17,783 adults with 217,816 BP measurements during the study period (Table 1). Median age was 58 years (IQR: 41–71 years). The majority of participants were black (67%), female (68%) and more than half (52%) were insured by Medicaid and/or Medicare (Table 1). Of the 295 census tracts included in the analysis, 81% had a majority of African American and Hispanic/Latino residents. Few census tracts (9%) had more than 10% of residents with limited English proficiency. Almost one quarter (23%) met criteria for high-poverty (≥40% below FPL).
Table 1.
Patient baseline characteristics from academic outpatient clinics, Chicago, 2014
| Patient characteristics N = 17,783 |
% | |
|---|---|---|
| Age (years) | ||
| 18–34 | 17.0 | |
| 35–49 | 16.7 | |
| 50–64 | 26.6 | |
| 65+ | 39.7 | |
| Gender | ||
| Female | 68.4 | |
| Male | 31.6 | |
| Race | ||
| White non-Hispanic | 23.6 | |
| Black non-Hispanic | 67.0 | |
| Hispanic or Latino | 3.6 | |
| Other | 5.0 | |
| Unknown | 0.7 | |
| Insurance status | ||
| Private | 20.5 | |
| Managed care | 21.1 | |
| Medicaid or dual-eligible | 10.1 | |
| Medicare | 42.2 | |
| None | 4.4 | |
| Other | 1.8 | |
| Health and healthcare characteristics | % | Mean ± SD |
| Blood pressure ([BP] mm Hg) | ||
| Systolic BP < 140 and diastolic BP < 90 | 65.8 | |
| Systolic BP ≥ 140 or diastolic BP ≥ 90 | 34.2 | |
| Mean dystolic BP | 132.0 ± 18.6 | |
| Mean diastolic BP | 75.9 ± 11.0 | |
| Heart rate ([HR] bpm) | ||
| Normal (HR ≤ 100) | 93.8 | |
| Tachycardia (HR > 100) | 6.2 | |
| Mean HR | 78.2 ± 13.7 | |
| Body mass index ([BMI] kg/m2) | ||
| Not obese (BMI < 30) | 61.3 | |
| Obese (BMI ≥ 30) | 38.7 | |
| Mean BMI | 29.4 ± 8.1 | |
| Healthcare utilization | ||
| Missed outpatient appointment (at least 1) | 50.3 | |
| All-cause admission (at least 1) | 16.0 | |
| Cardiovascular-cause admission (at least 1) | 4.2 | |
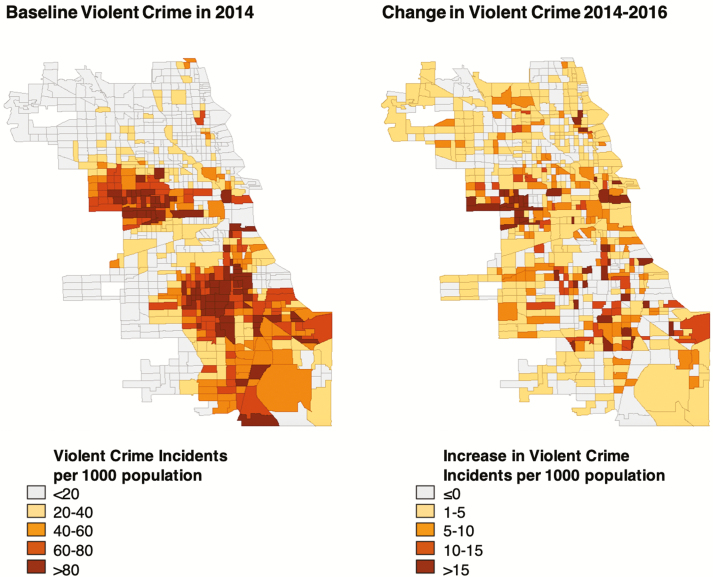
At baseline, the median census tract VCR was 41.3 (IQR: 15.2–66.8); change in the VCR ranged from –31.1 to 59.1 over the 3-year surge period (Figure 1). A 20-unit increase in the VCR was associated with 3% higher adjusted odds of having elevated BP (95% CI: 1.01–1.06) and 0.2 mm Hg higher systolic BP (P = 0.02; Table 2); associations with diastolic BP were not statistically significant (P = 0.65). Associations with elevated HR and obesity were not significant in either logistic or continuous models.
Figure 1.
Baseline violent crime and change in violent crime by census tract, Chicago, 2014–2016. The left panel shows the number of violent crime incidents per 1,000 population in each census tract; the right panel shows the change in violent crime incidents per 1,000 population in each census tract over the crime surge period (2014–2016).
Table 2.
Longitudinal association between census tract crime rate and cardiovascular health, Chicago, 2014–2016
| Systolic blood pressure (BP), mm Hg | Heart rate (HR), bpm | Body mass index (BMI), kg/m2 | ||||
|---|---|---|---|---|---|---|
| Change in crime rate, N = 17,783 | Change in systolic BP (se)a | P-value | Change in HR (se)a | P-value | Change in BMI (se)a | P-value |
| Violent crime rate (20 per 1,000 population) | 0.20 (0.08) | 0.02 | 0.06 (0.07) | 0.39 | 2.56 (3.66) | 0.48 |
| Homicide rate (1 per 1,000 population) | 0.04 (0.15) | 0.81 | 0.01 (0.12) | 0.90 | 3.49 (8.35) | 0.68 |
| Elevated BP, SBP ≥140 or DBP ≥90b | Elevated HR, HR > 100b | Obesity, BMI ≥ 30 kg/m2c | ||||
| Change in crime rate, N = 17,783 | AOR (95% CI)a | P-value | AOR (95% CI)a | P-value | AOR (95% CI)a | P-value |
| Violent crime rate (20 per 1,000 population) | 1.03 (1.01–1.06) | 0.04 | 1.01 (0.97–1.05) | 0.68 | 1.10 (0.80–1.52) | 0.56 |
| Homicide rate (1 per 1,000 population) | 1.01 (0.97–1.05) | 0.68 | 1.01 (0.92–1.11) | 0.85 | 1.01 (0.81–1.27) | 0.93 |
Bold values are statistically significant.
aEstimates derived from longitudinal panel models using generalized least squares, including a random effect for patient and robust standard errors clustered by census tract; adjusted for patient-level characteristics, including age (continuous), gender, race/ethnicity, insurance status, total cholesterol status, BMI (continuous), and treatment with BP medication; neighborhood-level characteristics, including ≥40% poverty, ≥25% no high school diploma, ≥50% minority population, and ≥10% limited English proficiency; and fixed effects for month and year
bDerived from systolic and diastolic blood pressure measurements recorded in the EHR; standard definitions obtained from the Seventh Report of the Joint National Committee
cDerived from height and weight measurements recorded in the Electronic Health Record (EHR); standard definitions obtained from the Centers for Disease Control and Prevention
During the study period, 5,985 unique patients were admitted across 15,468 encounters. One-fifth of encounters had a cardiovascular-related principal diagnosis. Among cardiovascular-related hospital admissions, the most common type was heart failure (22%), followed by chest pain and palpitations (10%), coronary artery disease (9%), atrial fibrillation (8%), and myocardial infarction (4%). A 20-unit rise in the VCR was associated with 8% higher adjusted odds of missing an outpatient appointment (95% CI: 1.03–1.13), 5% higher adjusted odds of having an all-cause hospital admission (95% CI: 1.02–1.09), and 6% higher adjusted odds of having a cardiovascular-related hospital admission (95% CI: 1.01–1.12; Table 3).
Table 3.
Longitudinal association between census tract crime rate and annual healthcare utilization, Chicago, 2014–2016
| Missed outpatient appointment | All-cause hospital admission | Cardiovascular hospital admission | ||||
|---|---|---|---|---|---|---|
| Change in crime rate, N = 17,783 | AOR (95% CI)a | P value | AOR (95% CI)a | P value | AOR (95% CI)a | P value |
| Violent crime rate (20 per 1,000 population) | 1.08 (1.03–1.13) | 0.001 | 1.05 (1.02–1.09) | 0.004 | 1.06 (1.01–1.12) | 0.02 |
| Homicide rate (1 per 1,000 population) | 1.05 (0.96–1.14) | 0.27 | 1.04 (0.95–1.14) | 0.35 | 1.09 (0.94–1.27) | 0.26 |
Bold values are statistically significant.
aEstimates derived from longitudinal panel models using generalized least squares, including a random effect for patient and robust standard errors clustered by census tract; adjusted for patient-level characteristics, including age (continuous), gender, race/ethnicity, insurance status, total cholesterol status, BMI (continuous), and treatment with BP medication; neighborhood-level characteristics, including ≥40% poverty, ≥25% no high school diploma, ≥50% minority population, and ≥10% limited English proficiency; and fixed effects for month and year.
In interaction tests by age, gender, and treatment with BP medications, living in a neighborhood with rising violent crime was associated with a larger effect on BP among non-elderly adults, women, and those without BP treatment (Supplementary Table 1). A 20-unit rise in the VCR was associated with 8% lower adjusted odds of elevated BP (95% CI: 0.87–0.96) and 0.3 mm Hg lower systolic BP (P = 0.04) in elderly adults relative to non-elderly adults; 11% higher adjusted odds of elevated BP (95% CI: 1.06–1.17) and 0.9 mm Hg higher systolic BP (P < 0.001) in women relative to men; and 4% higher adjusted odds of elevated BP (95% CI: 1.00–1.07) in those without treatment relative to those with treatment (Supplementary Table 1). Living in a neighborhood with rising violent crime was associated with a larger effect on missed outpatient appointments among non-elderly adults, and on all-cause hospital admissions among men; no other significant differences in healthcare utilization outcomes were observed by age, gender, or treatment with BP medications (Supplementary Table 2).
For low-crime census tracts, a 20-unit rise in the citywide VCR was associated with 5% higher adjusted odds of having elevated BP (95% CI: 1.02–1.08) and 0.4 mm Hg higher systolic BP (P < 0.001) compared with high-crime census tracts (Supplementary Table 3).
DISCUSSION
We found that exposure to rising violent crime during the 2014–2016 Chicago crime surge was associated with higher BP, missed outpatient appointments, and cardiovascular hospital admissions. Although several prior studies have documented cross-sectional linkages between chronic exposure to community violence and elevated BP,3,5 we documented a temporal relationship, supporting theoretical models in which violence exposure precedes stress responses and maladaptive health behaviors.18 One prior longitudinal study demonstrated mixed associations between violent crime and elevated BP but analyzed a relatively smaller sample size with limited geographic variation because of its use of survey-based data.12 Ours is among the first to document these findings in a relatively large sample of patients across a 295 census tract region. Importantly, we analyzed patients during a dynamic surge in violent crime who had residential stability over the study period, aiming to limit biases that often accompany the process of moving to a new neighborhood.13
Compared to traditional risk factors, such as dietary salt intake, obesity, and sedentary lifestyle, the magnitude of the effect for violent crime was similar in high-exposure census tracts.19 For instance, we observed a 0.2–0.9 mm Hg difference in systolic BP for every 20-unit increase in the census tract VCR. In census tracts with the largest increase in violent crime during the study period, this would indicate a 0.6–2.7 mm Hg difference for the highest risk census tracts at the population level. These differences are comparable to a 0.7–3.0 mm Hg difference documented in observational studies of dietary salt intake.20 Notably, we documented stronger associations among women.5 A rise in the census tract VCR had an over 3-fold larger effect for women than for the general population. These findings corroborate prior literature documenting larger socioeconomic gradients in cardiovascular disease among women relative to men.21 In one meta-analysis, women with lower educational attainment had 10% higher relative risk of cardiovascular disease than men with similar educational attainment.21 It is possible that fear of victimization may also be a more powerful deterrent of health behavior for women than for men.22
In Supplementary analyses, stronger associations were also observed for adults who were <65 years old, not treated with BP medications, and living in typically low-crime regions. Prior evidence has documented that older adult populations, particularly those with disabilities, often perceive themselves to be at higher risk for violence than younger populations.18 We speculate, however, that older adults already feel concerned about violence, and thus the threshold for change is higher during a crime surge. Alternatively, older adults already have higher rates of hypertension,23 and there may be a ceiling effect for higher BP among these individuals. We also found stronger associations between crime surge and elevated BP among those who were not treated with BP medications. It is possible that treatment itself confers a protective effect, or that those who seek and receive treatment tend to manage stress differently than those who do not. In sensitivity analyses at the city level, we identified a larger increase in BP for patients living in typically low-crime areas relative to high-crime areas. It is possible that lower baseline exposure to exogenous stress may result in a larger response to new adversity. As such, efforts to reduce violence may plausibly have benefit for the health of populations residing in both high and low crime regions of a city.
We additionally demonstrated a positive relationship between exposure to violent crime and missed outpatient appointments and increased hospital admissions, with implications for both individual and population-level management of health.24,25 These findings are consistent with prior qualitative research documenting narratives of heightened fear that resulted in physical confinement to the home.18 It is possible that staying home and delaying medical care (e.g., missed appointments) in these high-risk populations can precipitate downstream health consequences and hospital admissions. These findings are especially relevant for health systems that have implemented population health management business models and are now using strategies to identify individuals and communities at elevated risk for hospital care.26,27 The US Centers for Medicare and Medicaid Service and others have advocated for broad implementation of screening for interpersonal violence; 28 and more recently, other groups have advocated for the implementation of trauma-informed care.29 Strategies to identify “high-risk” patients, either through screening or location-based risk indicators, may help to target appropriate resources30 that address the multidimensional consequences of violence.
This study has several limitations. First, this is an observational study of an academic medical center, which limits causal inference. Adults receiving regular care at an academic medical center may be sicker at baseline, necessitating more regular care; or, these patients may have better access to healthcare, possibly limiting the generalizability of our findings. We recommend interpreting the study results as most generalizable to an urban, racial/ethnic minority population with a regular source of care. Second, although use of EHR data enables analysis of a larger sample size across a broader geographic area than in prior studies, we did not have individual-level data on socioeconomic status (SES) or health behaviors (e.g., physical activity, diet). We did adjust for both patient-level insurance type and neighborhood-level SES5,31 to partially mitigate this concern. Importantly, we included only residents with a stable residential address during the study period, thus limiting any unobserved changes in SES associated with moving to a new address. Unmeasured confounders are also possible at the structural level, such as institutional racism and housing policies (e.g., redlining),32,33 which we were unable to include in this study. Finally, our findings are subject to ecological fallacy, as we assigned exposure to crime based on each patient’s residential address. This type of analysis supports conclusions about the population-level impacts of rising crime but does not necessarily support conclusions at the individual level.
CONCLUSIONS
In Chicago, the 2014–2016 crime surge was associated with elevated BP, missed outpatient appointments, and cardiovascular hospital admissions among adults seeking primary care at an academic medical center. As the burden of hypertension and cardiovascular risk continues to rise in the United States, quantifying the health impacts of violence and other social conditions will be critical for targeting solutions and reducing disparities in vulnerable communities.
DISCLOSURES
Dr. Lindau directed a Center for Medicare and Medicaid Innovation Health Care Innovation Award (1C1CMS330997-03) called CommunityRx. This award required development of a sustainable business model to support the model test after award funding ended. To this end, Dr. Lindau is founder and co-owner of NowPow, LLC. Neither the University of Chicago nor the University of Chicago Medicine is endorsing or promoting any NowPow entity or its business, products, or services.
Supplementary Material
ACKNOWLEDGMENTS
This project was supported in part by the Agency for Healthcare Research and Quality K12 grant in patient centered outcomes research 5K12HS023007, by the American Heart Association Scientist Development Grant 17SDG33410656, and by a pilot award from the Center for Data and Computing at the University of Chicago. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the views of any U.S. governmental agencies. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. E.T. and C.T. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. This paper was presented in part at the American Heart Association Scientific Sessions, Chicago, IL, November 2018.
REFERENCES
- 1. Friedman M, Grawert AC, Cullen J.. Crime Trends: 1990–2016. Brennan Center for Justice: New York, NY, 2017. [Google Scholar]
- 2. Chicago Tribune Crime Team. Shootings in Chicago Chicago. Chicago Tribune: IL, 2018. Available from: http://www.chicagotribune.com/news/data/ct-shooting-victims-map-charts-htmlstory.html. Accessed 17 October 2018. [Google Scholar]
- 3. Suglia SF, Sapra KJ, Koenen KC. Violence and cardiovascular health: a systematic review. Am J Prev Med 2015; 48:205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yu E, Lippert AM. Neighborhood crime rate, weight-related behaviors, and obesity: a systematic review of the literature. Sociol Compass 2016; 10:187–207. [Google Scholar]
- 5. Tung EL, Wroblewski KE, Boyd K, et al. . Police-recorded crime and disparities in obesity and blood pressure status in Chicago. J Am Heart Assoc 2018; 7:e008030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Piro FN, Noss O, Claussen B. Physical activity among elderly people in a city population: the influence of neighbourhood level violence and self perceived safety. J Epidemiol Community Health 2006; 60:626–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Russell SJ, Hughes K, Bellis MA. Impact of childhood experience and adult well-being on eating preferences and behaviours. BMJ Open 2016; 6:e007770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Billimek J, Sorkin DH. Self-reported neighborhood safety and nonadherence to treatment regimens among patients with type 2 diabetes. J Gen Intern Med 2012; 27:292–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McEwen B, Lasley EN. Allostatic load: when protection gives way to damage. Adv Mind Body Med 2003; 19:28–33. [PubMed] [Google Scholar]
- 10. McEwen BS. Stress, adaptation, and disease. Allostasis and allostatic load. Ann N Y Acad Sci 1998; 840:33–44. [DOI] [PubMed] [Google Scholar]
- 11. Coulon SM, Wilson DK, Alia KA, Van Horn ML. Multilevel associations of neighborhood poverty, crime, and satisfaction with blood pressure in African-American Adults. Am J Hypertens 2016; 29:90–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mayne SL, Moore KA, Powell-Wiley TM, Evenson KR, Block R, Kershaw KN. Longitudinal associations of neighborhood crime and perceived safety with blood pressure: the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Hypertens 2018; 31:1024–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Clampet-Lundquist S, Massey DS. Neighborhood effects on economic self-sufficiency: a reconsideration of the moving to opportunity experiment. AJS 2008; 114:107–143. [Google Scholar]
- 14. Chicago Police Department. Crime Type Categories: Definition & Description Chicago, IL. Availa ble from: http://gis.chicagopolice.org/clearmap_crime_sums/crime_types.html. Accessed 18 December 2018.
- 15. National Center for Health Statistics. Classification of Diseases, Functioning, and Disability: International Classification of Diseases Atlanta, U.S. Department of Health & Human Services: GA; 2015. Available from: https://www.cdc.gov/nchs/icd/. Accessed 18 December 2018. [Google Scholar]
- 16. U.S. Census Bureau. American Community Survey 5-Year Estimates: American FactFinder; 2014. Available from: http://factfinder.census.gov. Accessed 18 December 2018.
- 17. Kutner MH, Nachtsheim CJ, Neter J. Multicollinearity diagnostics--variance inflation factor. In Applied Linear Regression Models. 4th ed: McGraw-Hill: Irwin; 2004. pp. 406–410. [Google Scholar]
- 18. Tung EL, Johnson TA, O’Neal Y, Steenes AM, Caraballo G, Peek ME. Experiences of community violence among adults with chronic conditions: qualitative findings from Chicago. J Gen Intern Med 2018; 33:1913–1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kornitzer M, Dramaix M, De Backer G. Epidemiology of risk factors for hypertension: implications for prevention and therapy. Drugs 1999; 57:695–712. [DOI] [PubMed] [Google Scholar]
- 20. O’Donnell M, Mente A, Yusuf S. Sodium intake and cardiovascular health. Circ Res 2015; 116:1046–1057. [DOI] [PubMed] [Google Scholar]
- 21. Backholer K, Peters SAE, Bots SH, Peeters A, Huxley RR, Woodward M. Sex differences in the relationship between socioeconomic status and cardiovascular disease: a systematic review and meta-analysis. J Epidemiol Community Health 2017; 71:550–557. [DOI] [PubMed] [Google Scholar]
- 22. Foster S, Giles-Corti B. The built environment, neighborhood crime and constrained physical activity: an exploration of inconsistent findings. Prev Med 2008; 47:241–251. [DOI] [PubMed] [Google Scholar]
- 23. Yoon SS, Burt V, Louis T, et al. . Hypertension Among Adults in the United States, 2009–2010. National Center for Health Statistics: Atlanta, GA. 2015. Available from: https://www.cdc.gov/nchs/products/databriefs/db107.htm. Accessed 13 March 2019. [Google Scholar]
- 24. Kassler WJ, Tomoyasu N, Conway PH. Beyond a traditional payer–CMS’s role in improving population health. N Engl J Med 2015; 372:109–111. [DOI] [PubMed] [Google Scholar]
- 25. Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable health communities–addressing social needs through Medicare and Medicaid. N Engl J Med 2016; 374:8–11. [DOI] [PubMed] [Google Scholar]
- 26. Roski J, Bo-Linn GW, Andrews TA. Creating value in health care through big data: opportunities and policy implications. Health Aff (Millwood) 2014; 33:1115–1122. [DOI] [PubMed] [Google Scholar]
- 27. Gawande A. The Hot Spotters: Can We Lower Medical Costs by Giving the Neediest Patients Better Care? The New Yorker: New York, NY. 2011. [PubMed] [Google Scholar]
- 28. U.S. Preventive Services Task Force. Screening for Intimate Partner Violence and Abuse of Elderly and Vulnerable Adults: U.S. Preventive Services Task Force Recommendation Statement 2013. Available from: https://www.uspreventiveservicestaskforce.org/uspstf12/ipvelder/ipvelderfinalrs.htm. Accessed 2 January 2019.
- 29. Raja S, Hasnain M, Hoersch M, Gove-Yin S, Rajagopalan C. Trauma informed care in medicine: current knowledge and future research directions. Fam Community Health 2015; 38:216–226. [DOI] [PubMed] [Google Scholar]
- 30. Lindau ST, Makelarski J, Abramsohn E, Beiser DG, Escamilla V, Jerome J, Johnson D, Kho AN, Lee KK, Long T, Miller DC. CommunityRx: a population health improvement innovation that connects clinics to communities. Health Aff (Millwood) 2016; 35:2020–2029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Beck AF, Huang B, Ryan PH, Sandel MT, Chen C, Kahn RS. Areas with high rates of police-reported violent crime have higher rates of childhood asthma morbidity. J Pediatr 2016; 173:175–182.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kwate NO, Loh JM, White K, Saldana N. Retail redlining in New York City: racialized access to day-to-day retail resources. J Urban Health 2013; 90:632–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jacoby SF, Dong B, Beard JH, Wiebe DJ, Morrison CN. The enduring impact of historical and structural racism on urban violence in Philadelphia. Soc Sci Med 2018; 199:87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.