Abstract
Objective
Wuhan, the epicentre of the coronavirus diseases (COVID-19) outbreak, has been locked down on January 23, 2020. We conducted a study among the lay public in Wuhan to access their support, understanding of, compliance with, and the psychological impacts of the quarantine.
Methods
We conducted a cross-sectional, online-based survey study between January 28, 2020, and February 2, 2020 among the adult lay public in Wuhan to access their support, understanding of, compliance with, and the psychological impacts of the quarantine. Multivariable logistic analysis was used to identify factors associated with psychological impacts.
Results
Among the 4100 participants investigated, a total of 15.9% were compliant with all the five household prevention measures, whereas 74.4% were compliant with all the three community prevention measures investigated. By demographics, participants of younger age, higher income, residing in an urban area, knowing neighbors infected with COVID-19 reported significantly higher psychological impact score. Participants with a lower level of support for quarantine were more likely to have a higher psychological impact score (OR = 1.45, 95% CI 1.07–1.96). Participants with a lower level of compliance with preventive measures (score of 0–19) reported higher psychological impact (OR = 1.40, 95% CI 1.22–1.60 vs. score 20–24). Participants who had been out of house socializing and attended public events expressed higher psychological impact.
Conclusions
Support, understanding of the rationale for quarantine are essential in ensuring appropriate psychological well-being during the quarantine. Improvements in compliance with preventive measures are highly warranted and may bring about a reduction in psychological distress.
Keywords: Quarantine, Wuhan, Support compliance, Psychosocial impact, COVID-19
1. Introduction
The coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first reported in China in December 2019 [1,2]. The new coronavirus spread at an alarmingly fast rate, and within weeks it was rapidly dispersing through Wuhan and the mainland of China. On January 23, 2020, the central government of the People's Republic of China has imposed a lockdown in Wuhan, the epicentre, to prevent an epidemic. Subsequently, many other cities in Hubei province were also locked down. In more than a month, the rising spread of the coronavirus was contained. The number of new cases reported daily in China has been on a downward trend since the first week of February. In approximately two months, the COVID-19 cases in China has fallen to single digits. As of March 16, the epicentres of Wuhan and Hubei began to lift restrictions, the coronavirus has resulted in over 80 thousand cases and claimed over three thousand deaths in mainland China [3].
Quarantine from leaving a designated area is imposed by Chinese authorities to minimize transmission to others outside the communities. During the coronavirus outbreak in Wuhan, strict social distancing was imposed on entire Wuhan population along with a city-wide lock down and closing of non-essential business. The government also imposed serious fines and penalties for people violating social distancing and home isolation instruction. During the quarantine, the authorities also encourage the residents to practice “self-quarantine” in their homes. They are advised to stay at home and avoid contact with others outside as much as possible. Within household context, self-imposed prevention measures are encouraged, such as wearing facemask when other members are in the house, separating utensils or household hygiene items, avoiding sharing food, or separating potentially ill family members from others in the household. Low compliance with quarantine requirements could result in the ineffectiveness of quarantine as a public health measure to contain the spread of disease [4]. Therefore, it is crucial that people under quarantine support quarantine measures, understand the rationale for quarantine, and, most importantly, adhere to appropriate protective and preventive measures to minimize transmission of infection during the quarantine.
Several studies investigated the psychological distress of people under disease quarantine. Fear, frustration, loneliness, boredom, conflict, and anger have been reported among patients quarantined for the acute respiratory syndrome (SARS) epidemic [[5], [6], [7]]. Furthermore, lesson learned from the Ebola epidemic suggests that mental disorders, including anxiety and depressive disorders, and posttraumatic stress disorder are some of the psychological catastrophes that can result in hazards exceeding the consequence of the outbreak itself [8]. COVID-19 quarantine has undoubtedly caused panic among the residents and has detrimental effects in psychological health. Poor psychological health can weaken a person's immune system and increase susceptibility to various infections [9,10]. Apart from the essentials of maintaining a healthy immune system to defend against the highly infectious SARS-CoV-2, it is also of utmost importance that individual under quarantine continues to adhere to preventive disease recommendation despite being in the state of psychological distress. A study conducted on people under quarantine in Canada during the SARS outbreak in 2003 showed that the psychological impact of quarantine caused increased difficulty with compliance with quarantine requirements, especially among the health-care workers [11]. In contrast, in Hong Kong, a dose-response gradient between anxiety level and uptake of personal protective measures was found during the 2003 outbreak [12].
This study aimed to assess the level of support and understanding of the rationale of quarantine, quarantine behaviour, and psychological impact associated with quarantine among the people under the quarantine in Wuhan.
2. Materials and methods
2.1. Study design and participants
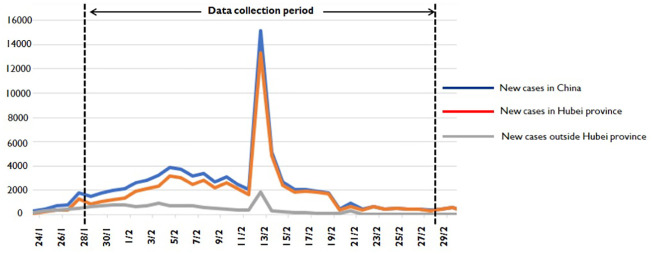
We administered a cross-sectional, web-based survey using an online questionnaire between January 28 and February 2, 2020. Fig. 1 shows the duration of the data collection period and the trend of confirmed COVID-19 cases in Wuhan and mainland China. Inclusion criteria are Chinese residents age above 18 years, currently under quarantine in the city of Wuhan, Hubei.
Fig. 1.
The duration of the data collection period and the trend of confirmed COVID-19 cases in Wuhan and mainland China.
2.2. Procedures
We commenced a cross-sectional, web-based anonymous survey using an online questionnaire. The social network WeChat (the most popular messaging app in China) was used to advertise and circulate the survey link to people in Wuhan. Participants were informed that their participation was voluntary, and consent was implied on completion of the questionnaire. After completing the survey questions, participants were given a small incentive.
The questionnaire was first developed in English and translated into Chinese. Local experts validated the content of the questionnaire, after which it was pilot tested. The survey consisted of five sections that assessed 1) demographic background (7-item), 2) support of provincial and self-imposed quarantine (2-item), 3) understanding the rationale for quarantine (5-item), 4) quarantine behaviour (8-item), and 5) psychological impact associated with quarantine (20-item). The questions on understanding the rationale of quarantine, quarantine behaviour and psychological impact were adapted from the study by Reynolds et al. (2008), [11] which investigated understanding, compliance and psychological impact of the SARS quarantine experience.
Quarantine behaviour part included questions on 1) compliance with household and community preventive measures. The response option was on a four-point Likert scale with items scored as either 0 (never), 1 (seldom), 2 (sometimes), or 3 (often). The total score for preventive measures is obtained by summing across all the items. The possible score ranges from 0 to 24, with higher scores indicating higher compliance with preventive measures.
Psychological impact assessed participants' current feelings and fears associated with being under quarantine for COVID-19, divided into questions assessing psychosocial impact associated with provincial quarantine and self-quarantine, each section containing 10 questions, respectively. The response option was a two-point scale with items scored as either 0 (yes) or 1 (no). The total scale score is obtained by summing across all the items. The possible score ranges from 0 to 20, with higher scores indicating higher psychological distress.
The items of questions on quarantine behaviour and psychological impact in this study are shown in Table 2.
Table 2.
Compliance to transmission prevention and psychological impact of quarantine (N = 4100).
| n |
% |
95CI% |
|
|---|---|---|---|
| Home prevention measures | Often practice | ||
| Used separate towels | 3601 | 87·8 | 86·8–88·8 |
| Wash hand frequently | 2647 | 64·6 | 63·1–66·0 |
| Used separate cutlery | 2424 | 59·1 | 57·6–60·6 |
| Slept in separate rooms | 2406 | 58·7 | 57·2–60·2 |
| Used mask when household member present | 838 | 20·4 | 19·2–21·7 |
| Compliant with all household prevention measures | 651 | 15·9 | 14·8–17·0 |
| Outdoor prevention measures | |||
| Did not go out of house to socialize | 3461 | 84·4 | 83·3–85·5 |
| Did not attend important events | 3458 | 84·3 | 83·2–85·4 |
| Did not allow visitors into home | 3389 | 82·7 | 81·5–83·8 |
| Compliant with all community protective measures | 3051 | 74·4 | 73·1–75·7 |
| Physiological impact |
Yes |
||
|---|---|---|---|
| Provincial quarantine (n = 3958) | |||
| Boredom | 3446 | 87·1 | 86·0–88·1 |
| Isolation | 2442 | 61·7 | 60·2–63·2 |
| Frustration | 2167 | 54·7 | 53·2–56·3 |
| Annoyance | 2865 | 72·4 | 71·0–73·8 |
| Worry | 3538 | 86·3 | 88·4–90·3 |
| Loneliness | 2653 | 67·0 | 65·5–68·5 |
| Helpless | 2582 | 65·2 | 63·7–66·7 |
| Anger | 2203 | 55·7 | 54·1–57·2 |
| Nervousness | 3181 | 80·4 | 79·1–81·6 |
| Sadness | 2705 | 68·3 | 66·9–69·8 |
| Self- imposed quarantine (n = 3838) | |||
| Boredom | 3205 | 83·5 | 82·3–84·7 |
| Isolation | 2385 | 62·1 | 60·6–63·7 |
| Frustration | 2254 | 58·7 | 57·2–60·3 |
| Annoyance | 2700 | 70·3 | 68·9–71·8 |
| Worry | 3213 | 83·7 | 82·5–84·9 |
| Loneliness | 2613 | 68·1 | 66·6–69·6 |
| Helpless | 2515 | 65·5 | 64·0–67·0 |
| Anger | 2187 | 57·0 | 55·4–58·6 |
| Nervousness | 3031 | 79·0 | 77·6–80·3 |
| Sadness | 2607 | 67·9 | 66·4–69·4 |
2.3. Statistical analysis
Normality testing was performed using the Kolmogorov-Smirnov test. The score of compliance with preventive measures and preventive measures were not normally distributed; therefore, all results were expressed as the median and interquartile range (IQR). Descriptive statistics were used to summarize our data. The prevalence of then proportion and their respective 95% confidence interval (CI) was calculated. Frequency tables, charts, and proportions were used for data summarization. Reliability of the compliance with preventive measures and psychological impact items was evaluated by assessing the internal consistency of the items representing the scores. The compliance with preventive measures and psychological impact scores had reliability (Cronbach's α) of 0.655 and 0.970, respectively. The chi-squared statistic was used for testing relationships on categorical variables. Spearman's correlation coefficients were calculated to determine the correlation between compliance with preventive measures and total psychological impact score. Multivariable logistic regression was used to determine the significant association between covariates investigated and psychological impact scores. Variables that are significant in the univariate analyses were selected for multivariable logistic regression analysis and included in the model using a simultaneous forced-entry method. Odds ratios (OR), 95% confidence intervals (95% CI), and p-values were calculated for each independent variable. The model fit was assessed using the Hosmer–Lemeshow goodness-of-fit test [13]. All statistical analyses were performed using the Statistical Package for the Social Sciences, version 20.0 (IBM Corp., Armonk, NY, USA). A p-value of less than 0.05 was considered statistically significant.
2.4. Ethics approval
The authors confirm that the ethical policies of the journal, as noted on the journal's author guidelines page, have been adhered to and the appropriate ethical review committee approval has been received. The study protocol was approved by the Research Ethics Committee of the Fujian Medical University. Respondents were informed that their participation was voluntary, and consent was implied on the completion of the questionnaire.
3. Results
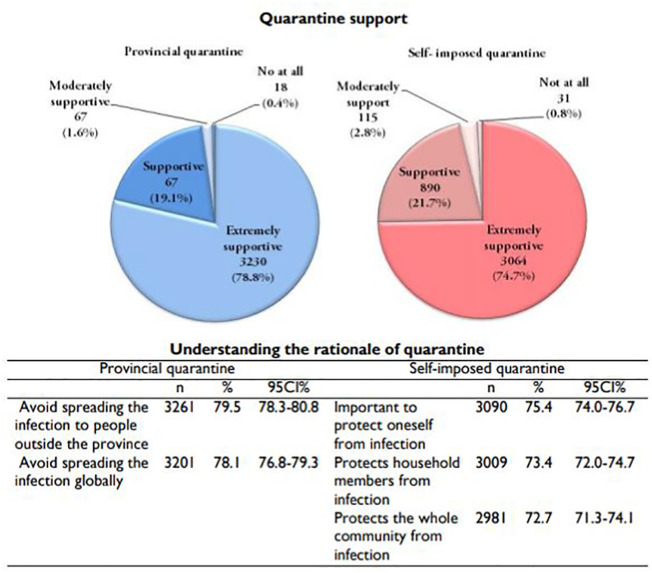
The survey link was disseminated between January 28, 2020 and February 2, 2020, a total of 4100 responses were received. The study received responses from participants of diverse demographics, shown in Table 1 . A total of 1.7% reported knowing family members infected with SARS-CoV-2, and 11.5% reported knowing neighbors infected with SARS-CoV-2. Fig. 2 shows the results for participants' support of provincial and self-imposed quarantine, as well as their understanding of the rationale for quarantine. A total of 78.8% were “extremely supportive,” and 17.1% reported “supportive” of provincial quarantine. A slightly lower proportion (74.7%) reported “extremely supportive” of self-imposed quarantine. Of note, among those that responded “extremely supportive” of provincial quarantine, significantly higher proportion were of the secondary level (81.2%) and high school (81.9%) education compared to those with university degrees (77.0%) (chi-squared [χ2] = 10.193, degree of freedom [df] =2, p = 0.006). The income group below RMB 50,000 (80.8%) and RMB 50,000–120,000 (78.5%) reported higher proportion “extremely supportive” of provincial quarantine than those of income above RMB 120,000 (76.4%) (χ2 = 10.193, df = 2, p = 0.003). There is a gradual increase in proportion that reported “extremely supportive” of provincial quarantine by age group; 18–25 years (75.3%), 26–35 years (77.3%), 36–45 (80.9%), over 45 (82.6%) (χ2 = 18.424, df = 3, p < 0.001). Findings on the understanding of quarantine showed that most participants agreed that provincial quarantine was imposed to avoid spreading the infection to people outside the province (79.5%) and globally (78.1%). Similarly, most participants agreed that self-imposed quarantine was important to protect themselves (75.4%), their household members (73.4%), and the community (72.7%) from infection.
Table 1.
Participant characteristics (N = 4100).
| n | % | 95% CI | |
|---|---|---|---|
| Socio demographic characteristics | |||
| Age group (yrs) | |||
| 18–25 | 870 | 21·2 | 20·0–22·5 |
| 26–35 | 1451 | 35·4 | 33·9–36·9 |
| 36–45 | 894 | 21·8 | 20·5–23·1 |
| >45 | 885 | 21·6 | 20·3–22·9 |
| Gender | |||
| Male | 1666 | 40·6 | 39·1–42·2 |
| Female | 2434 | 59·4 | 57·8–60·9 |
| Highest educational level | |||
| Secondary school and below | 690 | 16·8 | 15·7–18·0 |
| High school | 1122 | 27·4 | 26·0–28·8 |
| University | 2288 | 55·8 | 54·3–57·3 |
| Occupation type | |||
| Health professionals | 127 | 3·1 | 2·6–3·7 |
| Food-handling workers/Farmers | 338 | 8·2 | 7·4–9·1 |
| Industrial workers | 831 | 20·3 | 19·0–21·5 |
| Officers | 1414 | 34·5 | 33·0–36·0 |
| Housewife/ Retiree/ Others | 1046 | 25·5 | 24·2–26·9 |
| Students | 344 | 8·4 | 7·6–9·3 |
| Average monthly household income (RMB) | |||
| <RMB 50,000 | 1427 | 34·8 | 33·3–36·3 |
| RMB 50,000-120,000 | 1679 | 41·0 | 39·4–42·5 |
| >RMB 120,000 | 994 | 24·2 | 22·9–25·6 |
| Location of current workplace/study place | |||
| Urban | 3286 | 80·1 | 78·9–81·4 |
| Sub-urban/rural | 814 | 19·9 | 18·6–21·1 |
| Knowing someone infected with 2019-nCov infection | |||
| Known of family members infected with 2019-nCov | |||
| Yes | 71 | 1·7 | 1·4–2·2 |
| No/Don't know | 4029 | 98·3 | 97·8–98·6 |
| Known of neighbor infected with 2019-nCov | |||
| Yes | 473 | 11·5 | 10·6–12·6 |
| No/Don't know | 3627 | 88·5 | 87·4–89·4 |
Fig. 2.
Proportion of responses for support and understanding of provincial quarantine and self-imposed quarantine (N = 4100).
The summary of responses for compliance with preventive measures is shown in Table 2 . The highest proportion of home prevention measures was the use of separate towels (87.8%). A total of 64.6% reported washing hands frequently, and only 20.4% reported using a mask at home when household members were present. A total of 15.9% of the participants in the study were compliant with all the five household prevention measures. Among the participants who reported compliance with all the household prevention measures, the highest proportion was recorded among the age group 18–25 years (25.6%), compared to those of age 26–35 years (14.1%), 36–45 years (12.4%), and over 45 years (13.8%) (χ2 = 64.293, df = 3, p < 0.001). A higher proportion of participants with secondary school (21.6%) and high school (17.6%) level of education reported compliance with all the household prevention measures compared to university graduates (13.3%) (χ2 = 31.165, df = 2, p < 0.001). The income groups below RMB 50,000 (19.6%) and RMB 50,000–120,000 (15.5%) reported a higher proportion compliant with all the household prevention measures than those with income above RMB 120,000 (11.1%) (χ2 = 32.434, df = 2, p < 0.001).
The majority of the participants did not go out of the house to socialize (84.4%), did not attend important events (84.3%), and did not allow visitors into their home (82.7%). A total of 74.4% of the participants were compliant with all three community prevention measures. Among the participants who reported compliance with all the community prevention measures, the lowest proportion was recorded among the age group of 18–25 years (65.7%), compared to those of age 26–35 years (75.3%), 36–45 years (80.9%), and over 45 years (75.4%) (χ2 = 55.085, df = 3, p < 0.001). A higher proportion of participants with the highest level of education–university graduates (76.4%)–reported compliance with all the community prevention measures compared to those with secondary school (72.2) and high school (72.2%) level of education (χ2 = 9.256, df = 2, p = 0.01). The group with income above RMB 120,000 (77.1%) reported higher compliance with all community prevention measures than groups with an income level below RMB 50,000 (72.0%) and RMB 50,000–120,000 (75.1%) (χ2 = 8.309, df = 2, p = 0.016).
The total score for compliance with household and community prevention measures ranged from 0 to 24. The median score was 20 (IQR 17 to 22). The total score for compliance was categorized into two groups, 0–19 and 20–24, based on the median split; a total of 1637 (45.0%) had a score of 0–19 and 2042 (55.0%) had a score of 20–24.
Findings on items of the psychological impact associated with quarantine are shown in Table 2. The three highest psychological impacts associated with provincial quarantine were “boredom” (87.1%), “worry” (86.3%), and “nervousness” (80.4%). Only slightly over half (54.7%) reported the feeling of “frustration.” The self-imposed quarantine results in the three highest psychological distress categories: worry (83.7%), boredom (83.5%), and annoyance (70.3%). In total, 3715 participants reported practicing self-imposed quarantine. The total score of the psychological distress associated with provincial and self-imposed quarantine among these participants ranged from 0 to 20. The median score was 17 (IQR 8 to 20). The median score was 20 (IQR 17 to 22). The total score for psychological impact was divided into two groups, 0–16 or 17–20, based on the median split; a total of 1794 (48.3%) had a score of 0–16 and 1921 (51.7%) had a score of 17–20.
Table 3 shows the Spearman's rank correlation coefficients of compliance with prevention measures and total psychological impact score. There is a significant negative correlation between all the compliance with prevention measures and the total psychological impact score. On the whole, higher correlation coefficients were found on community prevention measures compared to household prevention measures. The highest correlation coefficient was found between not going out of the house to socialize and the total psychological impact score (r = −0.132, p < 0.01). Spearman's rank correlation coefficients for not attending important events and the total psychological impact score was −0.107 (p < 0.01).
Table 3.
Spearman correlation coefficients of compliance to prevention measures and total psychological impact score N = 3715.
| Used separate towels | Wash hand frequently | Used separate cutlery | Slept in separate rooms | Used mask when household member present | Did not go out of house to socialize | Did not attend important events | Do not allow visitors into the home | Total psychological impact score | |
|---|---|---|---|---|---|---|---|---|---|
| Used separate towels | 1 | ||||||||
| Wash hand frequently | ·301⁎⁎ | 1 | |||||||
| Used separate cutlery | ·327⁎⁎ | ·420⁎⁎ | 1 | ||||||
| Slept in separate rooms | ·248⁎⁎ | ·235⁎⁎ | ·346⁎⁎ | 1 | |||||
| Used mask when household member present | ·114⁎⁎ | ·242⁎⁎ | ·357⁎⁎ | ·316⁎⁎ | 1 | ||||
| Did not go out of house to socialize | ·076⁎⁎ | ·026 | -·013 | -·005 | -·071⁎⁎ | 1 | |||
| Did not attend important events | ·074⁎⁎ | ·031⁎ | -·015 | -·004 | -·081⁎⁎ | ·754⁎⁎ | 1 | ||
| Did not allow visitors into the home | ·068⁎⁎ | ·094⁎⁎ | ·029 | -·007 | -·018 | ·542⁎⁎ | ·546⁎⁎ | 1 | |
| Total psychological impact score | -·055⁎⁎ | -·058⁎⁎ | -·079⁎⁎ | -·044⁎⁎ | -·039⁎ | -·132⁎⁎ | -·107⁎⁎ | -·083⁎⁎ | 1 |
*p < 0·05, **p < 0·01, ***p < 0·001.
The univariable and multivariable analyses of factors associated with the psychological impact score are shown in Table 4 . In the univariate analyses, almost all covariates, except knowing family members infected with SARS-CoV-2, were significantly associated with psychological impact score. Of important note, in the multivariable analysis, participants of younger age groups reported significantly higher psychological impact score than those above 45 years old. Participants of average monthly household income RMB 50,000–120,000 reported significantly higher psychological impact score than those with income below RMB 50,000 (adjusted OR = 1.21, 95% CI 1.03–1.41). Participants in the urban area reported a higher psychological impact score than rural (OR = 1.24, 95% CI 1.05–1.48).
Table 4.
Factors associated with psychological impact score (N = 3715).
| Univariate analysis |
Multivariable analysisa |
||||
|---|---|---|---|---|---|
| Psychological impact score |
Psychological impact score 17–20 vs 0–16 |
||||
| Covariates | Frequency (%) | Score 17–20 (n = 1921) | Score 0–16 (n = 1794) | P | OR (95% CI) |
| Socio demographic characteristics | |||||
| Age group (years) | |||||
| 18–25 | 781 (21·0) | 431 (55·2) | 350 (44·8) | 2·13 (1·67–2·71)*** | |
| 26–35 | 1318 (35·5) | 748 (56·8) | 570 (43·2) | 1·81 (1·49–2·19)*** | |
| 36–45 | 812 (21·9) | 406 (50·0) | 406 (50·0) | p < 0·001 | 1·38 (1·13–1·69)** |
| >45 | 804 (21·6) | 336 (41·8) | 468 (58·2) | Ref | |
| Gender | |||||
| Male | 1503 (40·5) | 810 (53·9) | 693 (46·1) | 1·09 (0·94–1·25) | |
| Female | 2212 (59·5) | 1111 (50·2) | 1101 (49·8) | 0·030 | Ref |
| Highest educational level | |||||
| Secondary school and below | 607 (16·3) | 282 (46·5) | 325 (53·5) | Ref | |
| High school | 1038 (27·9) | 517 (49·8) | 521 (50·2) | 0·001 | 1·00 (0·81–1·23) |
| University | 2070 (55·7) | 1122 (54·2) | 948 (45·8) | 0·98 (0·79–1·21) | |
| Occupation type | |||||
| Health professionals | 107 (2·9) | 58 (54·2) | 49 (45·8) | 1·49 (0·93–2·40) | |
| Food-handling workers/Farmers | 313 (8·4) | 150 (47·9) | 163 (52·1) | 1·32 (0·92–1·89) | |
| Industrial workers | 757 (20·4) | 410 (54·2) | 347 (45·8) | 1·67 (1·21–2·27)** | |
| Officers | 1271 (34·2) | 693 (54·5) | 578 (45·5) | 0·013 | 1·45 (1·07–1·96)* |
| Housewife/ Retiree/Others | 957 (25·8) | 460 (48·1) | 497 (51·9) | 1·41 (1·03–1·93)* | |
| Students | 310 (8·3) | 150 (48·4) | 160 (51·6) | Ref | |
| Average monthly household income (RMB) | |||||
| <RMB 50,000 | 1308 (35·2) | 616 (47·1) | 692 (52·9) | Ref | |
| RMB 50,000-120,000 | 1523 (41·0) | 824 (54·1) | 699 (45·9) | p < 0·001 | 1·21 (1·03–1·41)* |
| >RMB 120,000 | 884 (23·8) | 481 (54·4) | 403 (45·6) | 1·15 (0·95–1·40) | |
| Location of current workplace/study place | |||||
| Urban | 2980 (80·2) | 1584 (53·2) | 1396 (46·8) | p < 0·001 | 1·24 (1·05–1·48)** |
| Sub-urban/rural | 735 (19·8) | 337 (45·9) | 398 (54·1) | Ref | |
| Knowing someone affected with 2019-nCov infection | |||||
| Family members infected with 2019-nCov | |||||
| Yes | 61 (16·4) | 39 (63·9) | 22 (36·1) | ||
| No/Don't know | 3654 (98·4) | 1882 (51·5) | 1772 (48·5) | 0·070 | |
| Neighbor infected with 2019-nCov | |||||
| Yes | 415 (11·2) | 256 (61·7) | 159 (38·3) | p < 0·001 | 1·55 (1·24–1·93)*** |
| No/Don't know | 3300 (88·8) | 1665 (50·5) | 1635 (49·5) | Ref | |
| Support for provincial and self-quarantine | |||||
| Support for quarantine | |||||
| Extremely supportive | 3159 (85·0) | 1564 (49·5) | 1595 (50·5) | p < 0·001 | Ref |
| Supportive/ Moderately supportive/not at all | 556 (15·0) | 357 (64·2) | 199 (35·8) | 1·45 (1·07–1·96)* | |
| Understanding of provincial and self-quarantine | |||||
| Agree | 3189 (85·8) | 1588 (49·8) | 1601 (50·2) | p < 0·001 | Ref |
| Disagree | 526 (14·2) | 333 (63·3) | 193 (36·7) | 1·22 (0·90–1·65) | |
| Compliance | |||||
| Preventive measure score | |||||
| Score of 0–19 | 1673 (45·0) | 954 (57·0) | 719 (43·0) | p < 0·001 | 1·40 (1·22–1·60)*** |
| Score of 20–24 | 2042 (55·0) | 967 (47·4) | 1075 (52·6) | Ref | |
OR: Odds ratio; CI: Confidence interval.
*p < 0·05, **p < 0·01, ***p < 0·001.
Hosmer & Lemeshow test, chi-square:7·694, p-value: 0·464; Nagelkerke R2: 0·059.
In this study, only 61 (16.4%) participants reported knowing family members infected with SARS-CoV-2. Knowing family members infected with SARS-CoV-2 is not significantly associated with psychological impact score in multivariable analysis; however, knowing a neighbor infected with SARS-CoV-2 is a significant influencing factor for having a higher psychological impact score (OR = 1.55, 95% CI 1.24–1.93). Participants with a lower level of support for provincial and self-quarantine were more likely to have a higher psychological impact score (OR = 1.45, 95% CI 1.07–1.96). Lastly, participants with a lower level of compliance with preventive measures (score of 0–19) reported a higher psychological impact (OR = 1.40, 95% CI 1.22–1.60) vs. score 20–24.
4. Discussion
The outbreak of COVID-19 in China has caused public panic and mental health stress [14]. This study aimed to understand the psychological impact of people under quarantine for COVID-19 in the epicentre Wuhan. Evidence of the general public's psychobehavioral responses plays a crucial role in providing insights and recommendations for the Chinese government in the implementation of public health interventions. Understanding local community psychobehavioral responses is important to provide insights into the development of risk communication messages to the general public to execute outbreak prevention and control [12,15].
On the day of the onset of our survey on January 28, 2020, a total of 4314 confirmed cases and 106 deaths was reported by the National Health Commission of China. On the last day of our data collection, February 2, 2020, around three fold-increase in confirmed cases (14,380) and deaths (304) were reported [16]. On a positive note, this study found that the majority of residents in Wuhan under quarantine expressed support for the provincial quarantine practice carried out by the authority. The study also indicated that the majority had a good understanding of the rationale for quarantine practices. Importantly, this study found that the participants with higher educational background, higher income, and people of older age group expressed lesser support for provincial quarantine providing important evidence-based information for targeted intervention.
On February 8, the Shanghai government held a press conference suggesting aerosol transmission of SARS-CoV-2 [17]. The evidence suggesting transmission of the SARS-CoV-2 by droplets and aerosols. [17,18] indicates that adhering to measures that prevent transmission within the household and in the community is extremely crucial. This study found that, although compliance with each community prevention measure separately was high (>80%), only 74.4% (95% CI 73.2–75.7) were compliant with all the community prevention measures. In contrast, compliance with household prevention measures was poor. In particular, less than one-quarter reported the use of masks at home when household members present and only 15.9% (95% CI 14.8–17.0) compliant with all the household prevention measures. Low compliance with household preventive measures was also reported during SARS outbreak [11]. High transmission of the coronavirus within households perhaps due to difficulty with compliance to household preventive measures. The gaps in household prevention measures identified in this study may inform future health interventions.
Of important note, the study was conducted approximately a week after the lockdown of Wuhan city and during the escalating rise of COVID-19 cases. The findings show overall high compliance in prevention measures among the people in Wuhan. The good compliance in prevention measures perhaps led to the beginning of the decline in COVID-19 outbreak in Wuhan from the second week of February onwards. The demographic disparities in compliance with preventive measures found in the study warrant considerable attention. Of note, household prevention measures were higher among the younger age group, the lower educated and lower-income group. In contrast, community prevention measures were higher among the older age groups, higher educated, and higher-income groups. Thus there is a need for prevention interventions according to the identified target groups.
This study found a considerably high level of the psychological impact associated with provincial and self-imposed quarantine in just slightly over a week after the imposition of quarantine. By demographics, multivariable analysis showed that participants of younger age, higher-income group, residing in the urban areas, and knowing a neighbor infected with SARS-CoV-2 were more likely to have a higher psychological impact. There is a significant gradient increase in the psychological impact score by increasing the educational level, although education is not a significant covariate in the multivariable analysis. The younger people, higher educated and with higher income, were probably more exposed to the highly circulated information in social media about the current crisis that leads to a higher awareness of the severity of the outbreak risk, thus leading to higher psychological distress. Given these circumstances, it is important to disseminate the message carefully to avoid eliciting public anxiety and psychological distress. The Chinese government had responded fast to prevent psychological crisis among the people. The Peking University prepared a mental health handbook for the public for guidance for dealing and coping with stress and other psychological problems due to the COVID-19 outbreak [14]. The vulnerable groups at risk for psychological distress identified in this study provide valuable information for public health authorities and stakeholders to coordinate their targeted mental health interventions.
One of the important findings of this study is the significant influence of support for quarantine on the psychological impact in the multivariate analysis. People having lesser support for quarantine expressed higher psychological distress. Further, a significantly higher proportion of people with a lower understanding of quarantine express a higher level of psychological impact in the univariate analysis. Both findings imply the importance of people under quarantine for COVID-19 to maintain a positive, supportive, and acceptive attitudes towards the quarantine recommendation by the Chinese government. It is vitally important to dispel the myths and misinformation about the rationale for quarantine and to engender strong public support for quarantine and other recommended restrictive measures [19]. Likewise noted in a recent review, in situations where quarantine is deemed necessary, providing clear rationale for quarantine to the public may help reduce psychological impacts [20].
Lastly, lower preventive measure scores significantly associated with higher psychological impact may probably imply that people who have not been compliant with recommended preventive measures have increased feelings of anxiety about the possibility of infection.This conclusion is further supported by the significant correlation between those who have gone out to socialize and attended events and those who reported a higher level of psychological impact. Thus, public health intervention strategies need to provide a channel for people who suspect being infected with SARS-CoV-2, to provide advice and deliver psychological health support to ease their anxiety [21]. However, the cross-sectional design used in this study cannot determine causal relationship. It is also possible that people with greater psychological consequences suffer behavioral functioning [22] and unable to undertake recommended preventive measures. Future studies are warranted to evaluate this association using experimental research designs.
The current study has several limitations. The first limitation is that the study is cross-sectional. Thus, it cannot be used to infer causality. The second limitation is that the responses were based on self-reporting of data and may be subject to self-reporting bias and a tendency to report socially desirable responses. Third, the online survey method used in this study can lead to selection bias. Nevertheless, during the outbreak crisis period, survey using WeChat, the largest social media platform in China, is extremely effective in reaching a broad coverage of the quarantined population in a short time. The collected sample is of diverse demographics and is reflective of the general population in Wuhan city. Despite these limitations, the study contributes tremendously to the understanding of the psychological well-being of people under quarantine.
5. Conclusions
In conclusion, this paper identified the psychological impact associated with quarantine for COVID-19 in Wuhan, the epicentre of COVID-19. The findings outline the important role of support, understanding the rationale for quarantine, and compliance with preventive measures for ensuring optimal psychological well-being of residents under quarantine. Findings also suggest that improvements in compliance with preventive measures are highly warranted and may bring about a reduction in psychological distress. It is equally important to mitigate the effects of quarantine and understand the psychological needs of public under quarantine for infectious disease. Mental health professionals play an important role to curb the consequences of quarantine on mental wellbeing of the public.
Funding
This study was supported by the Pilot Project of the Fujian Provincial Department of Science and Technology (No. 2020Y0005); Fujian Medical University's Rapid Response Funding Call for COVID-19 Related Research (No. 2020YJ003). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors would like to thank all participants of the study for their participation in the investigation.
Ethical approval
The study protocol was approved by the Research Ethics Committee of the Fujian Medical University. Respondents were informed that their participation was voluntary, and consent was implied on the completion of the questionnaire.
Availability of data and material
All data for this study is available upon reasonable request to corresponding author.
Author contributions
LP.W., Y.L. and Z.H. planned the study. Y.L. obtained the data. LP.W. and H.A. performed the statistical analysis and data summarization. LP.W. drafted the manuscript. All authors discussed the results and contributed to the final manuscript.
Declaration of Competing Interest
The authors declare no conflict of interest.
References
- 1.Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J. Med. Virol. 2020;92(4):401–402. doi: 10.1002/jmv.25678. 31950516 PMC7166628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hui D.S., Madani T.A., Ntoumi F., Kock R., Dar O., et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health - The latest 2019 novel coronavirus outbreak in Wuhan, China. International journal of infectious diseases. IJID. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO . (COVID-19) Situation Report. 2019. Coronavirus disease.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200316-sitrep-56-covid-19.pdf?sfvrsn=9fda7db2_6 Available online. (Accessed on 16 March 2020) [Google Scholar]
- 4.Rothstein M.A., Coughlin C.N. Ensuring compliance with quarantine by undocumented immigrants and other vulnerable groups: public health versus politics. Am. J. Public Health. 2019;109(9):1179–1183. doi: 10.2105/AJPH.2019.305201. 31318598 PMC6687239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maunder R., Hunter J., Vincent L., Bennett J., Peladeau N., Leszcz M., et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168(10):1245–1251. (PubMed PMID: 12743065; PubMed Central PMCID: PMC154178) [PMC free article] [PubMed] [Google Scholar]
- 6.Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. 15324539 PMC3323345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robertson E., Hershenfield K., Grace S.L., Stewart D.E. The psychosocial effects of being quarantined following exposure to SARS: a qualitative study of Toronto health care workers. Can. J. Psychiatr. 2004;49(6):403–407. doi: 10.1177/070674370404900612. 15283537 [DOI] [PubMed] [Google Scholar]
- 8.Shultz J.M., Baingana F., Neria Y. The 2014 Ebola outbreak and mental health: current status and recommended response. Jama. 2015;313(6):567–568. doi: 10.1001/jama.2014.17934. (PubMed PMID: 25532102.) [DOI] [PubMed] [Google Scholar]
- 9.Marshall G.D., Jr. The adverse effects of psychological stress on immunoregulatory balance: applications to human inflammatory diseases. Immunol. Allergy Clin. N. Am. 2011;31(1):133–140. doi: 10.1016/j.iac.2010.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Segerstrom S.C., Miller G.E. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol. Bull. 2004;130(4):601–630. doi: 10.1037/0033-2909.130.4.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reynolds D.L., Garay J.R., Deamond S.L., Moran M.K., Gold W., Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol. Infect. 2008;136(7):997–1007. doi: 10.1017/S0950268807009156Pubmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leung G.M., Ho L.M., Chan S.K., Ho S.Y., Bacon-Shone J., Choy R.Y., et al. Longitudinal assessment of community psychobehavioral responses during and after the 2003 outbreak of severe acute respiratory syndrome in Hong Kong. Clin. Infect. Dis. 2005;40(12):1713–1720. doi: 10.1086/429923. 15909256 [DOI] [PubMed] [Google Scholar]
- 13.Hosmer D.W., Jr., Lemeshow S., Sturdivant R.X. 3rd edition. John Wiley & Sons; New Jersey, USA: 2013. Applied Logistic Regression. [Google Scholar]
- 14.Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224) doi: 10.1016/S0140-6736(20)30309-3. e37-e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vaughan E., Tinker T. Effective health risk communication about pandemic influenza for vulnerable populations. Am. J. Public Health. 2009;99(Suppl. 2):S324–S332. doi: 10.2105/AJPH.2009.162537. 19797744 PMC4504362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Health Commission of the People’s Republic of China . Available online; 2020. Update on epidemic situation of novel coronavirus-infected pneumonia.http://www.nhc.gov.cn/xcs/yqfkdt/202002/17a03704a99646ffad6807bc806f37a4.shtml (Accessed on 16 March 2020) [Google Scholar]
- 17.Zhao C., Wang O., Liew L. Available online; 2020. Shanghai adds aerosol infection to coronavirus risk list.https://www.scmp.com/news/china/society/article/3049623/coronavirus-hubei-province-reports-81-new-deaths-and-2841 (Accessed on 16th March 2020) [Google Scholar]
- 18.Lu C.W., Liu X.F., Jia Z.F. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395(10224):e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tracy C.S., Rea E., Upshur R.E. Public perceptions of quarantine: community-based telephone survey following an infectious disease outbreak. BMC Public Health. 2009;9:470. doi: 10.1186/1471-2458-9-470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xiang Y.T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robinson O.J., Vytal K., Cornwell B.R., Grillon C. The impact of anxiety upon cognition: perspectives from human threat of shock studies. Front. Hum. Neurosci. 2013;7:203. doi: 10.3389/fnhum.2013.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data for this study is available upon reasonable request to corresponding author.