Strategies for successful program implementation in community-based organizations serving older Asian Americans include stakeholder engagement, adaptation of program materials, and networking between organizations.
Keywords: Evidence-based intervention, Community-based organizations, Implementation, Consolidated Framework for Implementation Research (CFIR), AAPIs
Abstract
Cardiovascular disease is the second leading cause of death in the USA among Asian Americans and Pacific Islanders (AAPIs) over the age of 65. Healthy Eating Healthy Aging (HEHA), an evidence-based heart health program, can provide culturally appropriate nutrition education to decrease the risk of cardiovascular disease. Community-based organizations (CBOs) are optimal settings to implement community-based programs. However, there is inadequate research on how evidence-based interventions like HEHA are implemented in CBOs. This study examined processes that facilitated the implementation of HEHA among CBOs serving older AAPIs. Twelve representatives from CBOs that implemented the HEHA program were recruited to participate in a semistructured interview. All the participants were CBO directors or senior managers. A semistructured interview guide was created and informed by the Consolidated Framework for Implementation Research (CFIR) to capture how HEHA played into the five domains of CFIR: (a) intervention characteristics, (b) outer setting, (c) inner setting, (d) characteristics of the individuals, and (e) process. Data analysis captured themes under the CFIR domains. All five CFIR domains emerged from the interviews. Under intervention characteristics, three constructs emerged as facilitating the implementation of HEHA: (a) the participant’s beliefs around the quality of the HEHA program and its ability to promote healthy eating, (b) HEHA’s adaptability to different AAPI subgroups, and (c) perceptions of how successfully HEHA was bundled and assembled. Under outer setting, the participants described the community’s need for healthy eating programs and how the HEHA program meets that need. Four constructs emerged under inner setting: (a) the CBO’s structural characteristics and social standing in the community; (b) resources dedicated to the implementation and ongoing operations, including funding, training, education, physical space, and time; (c) the culture of the CBO; and (d) the participant’s commitment and involvement in marketing, promotion, and implementation of HEHA. Under characteristics of individuals, participants’ described their desire to learn the content of HEHA and deliver them successfully. Under process, participants described strategies to engage relevant individuals to facilitate HEHA implementation. The interviews with CBO representatives provided insights into CFIR domain constructs that facilitated the implementation of HEHA. CBOs are key settings for community health education. Understanding processes that lead to the successful implementation of evidence-based interventions among CBOs is critical for accelerating the dissemination and implementation of best practices.
Implications.
Practice: Community-based organizations (CBOs) are key settings for accelerating the dissemination and implementation of evidence-based interventions and reaching minority and immigrant communities.
Policy: Successful implementation of evidence-based interventions must consider factors that enable adoption, including organizations’ characteristics, the organizational culture, and leadership perception of the needs of the program, its effectiveness, adaptability, and access to partnerships.
Research: Future research is needed to examine the generalizability of the factors across CBOs serving different minority groups and geographical settings.
BACKGROUND
Asian Americans and Pacific Islanders (AAPIs) over the age of 65 are the fastest-growing racial/ethnic group in the USA with a total population of 49.2 million in 2016 [1]. Cardiovascular disease is the second leading cause of death among AAPIs. While the standardized mortality rate for this disease has decreased for non-Hispanic Whites in the previous decade, this decline was slower for AAPIs across the same timeframe [2]. Studies consistently show the importance of a healthy diet, noting that a well-balanced diet low in saturated fat and salt and high in fruits and vegetables can lower the risk for cardiovascular disease [3,4].
However, achieving a well-balanced meal may be particularly challenging for older AAPIs for several reasons. First, older AAPIs may lack the language proficiency and knowledge needed to read food labels and deduce sodium content [5]. Second, many foods prepared in AAPI cultures include a high amount of sodium in the form of soy sauce and other sodium-heavy condiments [6]. Third, some older AAPIs lack mobility to prepare their own meals due to physical or cognitive disabilities, therefore, relying on processed foods or meals prepared by other people [5,6]. A culturally and linguistically appropriate program that is tailored to older AAPIs and promotes a well-balanced diet with healthy meal preparation of traditional dishes is critically needed.
Healthy Eating Healthy Aging (HEHA) is a community–academic partnership project focused on promoting healthy eating among older AAPI adults. Adapted from American Heart Association’s Check.Change.Control. program (which focused on reducing risk for cardiovascular disease through blood pressure monitoring and nutrition education), HEHA was developed to provide a comprehensive nutrition education program culturally tailored for older AAPIs [7,8]. Specifically, HEHA aimed to increase nutrition label reading, decrease sodium intake, increase fruit and vegetable intake, and promote healthy meal preparation at home with the overall goal of decreasing cardiovascular disease risk among AAPIs. HEHA used a train-the-trainer model and was led by a large national nonprofit organization; this organization partnered with smaller, local community-based organizations (CBOs) that served older AAPIs and trained them to implement and adapt HEHA to the CBO’s needs. The CBOs were spread across nine states (California, Hawaii, Illinois, Massachusetts, New York, Pennsylvania, Texas, Virginia, and Washington) and the intervention materials were translated into seven languages, including Chinese, Khmer, Korean, Japanese, Samoan, Tagalog, and Vietnamese.
CBOs are key settings for community health education, particularly among immigrant and underserved populations, because of their reach and long-standing, trusted relationship with the communities they serve [9–11]. Most importantly, CBOs are critical settings for community health education where culturally appropriate and linguistically relevant health education on priority health topics is delivered [12]. These qualities make them highly desirable settings to implement evidence-based programs or best practices around community health. However, there is inadequate research on the processes that facilitate the implementation of health programs in CBOs. Guided by the Consolidated Framework for Implementation Research (CFIR) [13], this paper examines processes that facilitated the implementation of HEHA among CBOs serving older AAPIs.
METHODS
Eighteen semistructured interviews were conducted to understand processes that facilitated the implementation of the HEHA program among CBOs across nine states. All the CBOs (n = 18) were located in major metropolitan areas. We recruited two personnel from each CBO, one in a leadership role and another in operations. Twelve individuals in a leadership role (e.g., CEOs, directors, and senior managers) and six individuals in an operations role (e.g., program coordinators, health educators, and volunteers) were interviewed. For this study, only interviews with the leadership were included as most interviewees covered both leadership and operation roles, and all leaders were actively engaged in the day-to-day operations at the CBO. Operations staff focused more on task-based work with less decision-making power and perceived themselves as the “followers” who carried out tasks directed by the leadership. The leaders interviewed came from CBOs in eight of the nine states. Interviews were semistructured to unveil processes that facilitated the implementation of the HEHA program. Data were collected from January 2018 to March 2018. Participants received a $30 gift card upon completion of the interview. The Fred Hutchinson Cancer Research Center Institutional Review Board approved this study.
Recruitment and data collection
Participants were recruited from CBOs involved in the implementation of the HEHA program; participants provided leadership, coordination, or delivery of the program. Two email messages with an invitation to join the study were sent to all 18 CBOs a week apart. When a potential participant responded to the email, the study staff scheduled a phone call with the participant to explain the study. For participants who did not respond to the email message, the study staff contacted the CBO via phone to gauge their interest in participating in the study. When a potential participant showed interest and was deemed eligible, the study staff member obtained a verbal consent, collected demographic data, and scheduled the interview. From the 18 CBOs, 12 leaders were enrolled (67% response rate); 2 refused to participate, 3 did not respond to the emails and calls, and 1 was no longer employed by the CBO. The 12 leaders came from CBOs in eight out of the nine states (none came from Washington). An interview lasted between 30 and 80 min using a semistructured interview guide. All interviews were in English as participants were bilingual (English and one of the AAPI languages). The interviews were audiorecorded and transcribed verbatim.
Semistructured interview guide
The interview guide covered key implementation factors described in the literature, including the five CFIR domains on adoption and implementation and their selected constructs. CFIR is a theoretical framework widely used to understand the implementation processes of best practices [13–15]. CFIR consists of five domains and their associated constructs: (a) intervention characteristics contain key features that contribute to successful implementation with eight constructs relating to intervention characteristics (e.g., evidence strength and quality and adaptability), (b) outer setting comprises the external environment influencing the implementation and includes four constructs (e.g., cosmopolitanism), (c) inner setting consists of attributes of the organization that may influence implementation and includes 12 constructs (e.g., culture and leadership engagement), (d) characteristics of individuals comprise features of an organization that can affect implementation and includes five constructs (e.g., knowledge and beliefs about the intervention and self-efficacy), and (e) implementation process consists of strategies that facilitate implementation and includes eight constructs (e.g., engaging and executing).
Data analysis
Two researchers (J.L. and L.K.K.) independently reviewed each transcript to identify main ideas and meanings. We generated tentative labels to capture each idea’s essence and compared and contrasted notes. We then reviewed the data and clustered similar ideas into themes and codes representative of each theme. The coding scheme was refined throughout data analysis. We also created freehand domain charts mapping the interrelationship between concepts. Interview data were organized using ATLAS.ti, version 7 (Scientific Software Development, Berlin, Germany, 2013).
RESULTS
Demographics and characteristics of the participants
Table 1 presents participant characteristics. Participants’ mean (standard deviation) age was 56.67 (15.95) years and most (75%) were born outside the USA. About half (58%) were female. Most participants had a graduate school degree (83%). All held leadership roles with slightly different titles (e.g., director) at their CBO and worked at their organization for 14.45 (9.55) years.
Table 1.
Demographic characteristics of leaders at Community-based organizations (n = 12)
| n | |
|---|---|
| Age (Mean, SD) | 56.67 (15.95) |
| Place of birth | |
| USA | 3 (25.0%) |
| Outside of the USA | 9 (75.0%) |
| Ethnicity | |
| Hispanic | 0 |
| Non-Hispanic | 12 (100%) |
| Race | |
| Asian | 11 (91.67%) |
| Native Hawaiian/Other Pacific Islanders | 1 (8.33%) |
| Gender | |
| Male | 5 (41.67%) |
| Female | 7 (58.33%) |
| Education status | |
| College graduate | 2 (16.67%) |
| Graduate school degree | 10 (83.33%) |
| Position in the organization | |
| President | 1 (8.33%) |
| Senior program director | 1 (8.33%) |
| Project director | 5 (41.67%) |
| Executive director | 2 (16.66%) |
| Chief financial officer | 1 (8.33%) |
| Administrator | 1 (8.33%) |
| Manager | 1 (8.33%) |
| Years worked in the organization, mean (SD) | 14.45 (9.55) |
| Provide bilingual services | |
| No | 1 (8.33%) |
| Yes | 11 (91.67%) |
| If yes, what language? | |
| Chinese | 4 (33.33%) |
| Korean | 4 (33.33%) |
| Japanese | 1 (8.33%) |
| Samoan | 1 (8.33%) |
| Vietnamese | 1 (8.33%) |
| Location of organization | |
| California | 4 (33.33%) |
| Hawaii | 1 (8.33%) |
| Illinois | 2 (16.67%) |
| Massachusetts | 1 (8.33%) |
| New York | 1 (8.33%) |
| Pennsylvania | 1 (8.33%) |
| Texas | 1 (8.33%) |
| Virginia | 1 (8.33%) |
SD standard deviation.
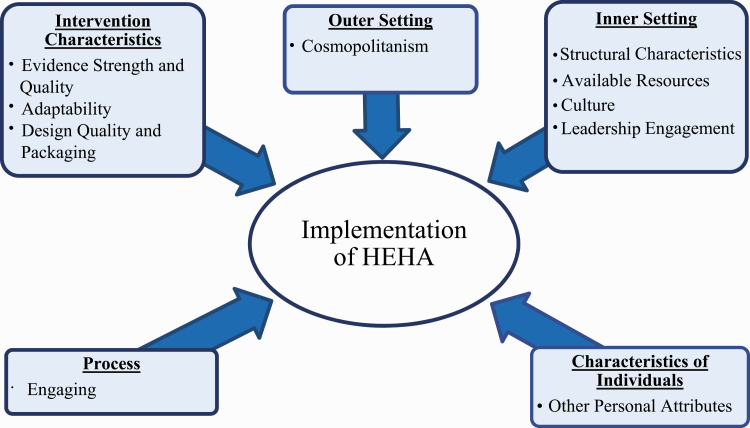
Figure 1 provides a pictorial overview of the results. The five outer boxes denote the five CFIR domains (intervention characteristics, outer setting, inner setting, characteristics of individuals, and process) and how these domains shaped the implementation of HEHA in CBO settings.
Fig 1.
Factors influencing implementation of Healthy Eating Healthy Aging.
Intervention characteristics
Three constructs, (a) evidence strength and quality, (b) adaptability, and (c) design quality and packaging, emerged under the intervention characteristics domain. Evidence strength and quality are defined as the participant’s perception of the quality and validity of the evidence supporting the intervention. Adaptability is the degree to which an intervention is adapted and tailored to meet the needs of the setting. Design quality and packaging are defined as the perceived excellence in how the intervention was assembled and presented to the participants.
Evidence strength and quality
The majority of participants reported that the decision to implement the HEHA program was shaped by their perceptions of the strength of the intervention to improve the health of the community they served. Specifically, they viewed HEHA as being effective in positively changing the AAPI seniors’ perception of healthy food choices. Validating their earlier assessment of the strength of HEHA with what they saw during implementation, one participant shared stories from the seniors who participated in the HEHA program:
You know, and who reads labels? So- after this class, one of the things that people have said is “now I pay-” it’s one of the things I’ve heard multiple times is “now I pay attention, I read the label.”
Adaptability
Across all interviews, participants reported the importance of adapting the interventions based on their seniors’ needs. Some adaptation was focused on content, tailoring the materials to their seniors’ language, traditional meals, and collective cultural values. Others were focused on logistics, including seniors’ mobility, availability with other competing priorities, and having a place for program delivery. For instance, seniors often prioritized personal arrangements, like attending doctor’s appointments, and participants worked to accommodate the seniors. As one participant mentioned, “We worked really hard, I’d say, to work on the class schedule, to fit their [the seniors’] work time.” Another participant chose to incorporate prayers during the class because their seniors believed that health was predetermined by religious beliefs. A different participant chose to deliver the intervention at a temple to attract their Japanese seniors who frequented the temple and held religious values. Another participant also provided examples of foods their AAPI group was familiar with:
We modified it for different types of Asian food by group and by different brands. We’ve got different types of soy sauce and low salt […] and then we did introduce them to some Western food…and I think the seniors really liked that.
Design quality and packaging
When discussing the adaptability of the materials, participants were split on their perceptions of the clarity of the materials and how that impacted adaptation and incorporation of the materials into the CBO’s existing curriculum. One participant stated that the training materials for HEHA were easy to understand, adapt, and deliver, but other participants mentioned the materials were too complex to digest, and they needed to do additional research online to better understand the content before sharing it with their seniors. These participants indicated that the materials were too “medical” and “humongous,” that is, the content was difficult to interpret and condense into digestible information that both the participants and seniors could understand. As a result, two diverging assessments on the packaging of the HEHA intervention were noted.
Outer setting
Cosmopolitanism
Cosmopolitanism, the degree to which the CBO is networked with other external organizations, was the only construct that emerged from the outer setting domain. Cosmopolitanism emerged at two levels. First, the CBO discussed their relationship with the national organization that delivered the initial training. Then, they discussed their relationship with other local organizations and communities in the area they served. Both levels were discussed as being critical to executing and rolling out a new program. Trust building was one of the key aspects discussed in their decision to implement HEHA. A participant stated:
And so I kind of trust NAME [name of the primary leading organization] with their programs when they call me and say, “Do you want to get involved with this?” I look at the program and I say yes, because it’s something specifically for the community we’re trying to serve, the seniors.
Participants stated the importance of CBO partnerships with local, regional, and national organizations, as well as with local communities. CBOs frequently partnered with senior apartment complexes as they often housed large populations of the seniors the CBO served, thus allowing CBOs direct access to the community. Many participants leveraged partnerships with other local CBOs, health coalitions, public health departments, health care systems, and national health organizations. One participant mentioned that partaking in the local healthy aging coalition enabled them to understand how HEHA’s intention aligned with their community’s values. Participants also often knew of an individual at an external organization who was able to provide a needed resource (e.g., cooking classes from a local food bank) or student volunteers to help implement HEHA. The participants also saw themselves as being the gateway to connecting with the community:
And…working in partnership with NAME [name of the primary leading organization] and other agencies that come into our community, it’s like we’re the door into the community. When you really reach the Samoan community, it’s through us.
Inner setting
Four constructs emerged within the domain of inner setting, including structural characteristics, available resources, culture, and leadership engagement.
Structural characteristics
Participants emphasized the importance of the organization’s structural characteristics in facilitating the implementation of HEHA. Characteristics of the CBO, such as maturity of the organization (decades in existence), social standing (positive reputation), and size (number of overall seniors utilizing CBO services) were influential in engaging their seniors in the HEHA program. Because of a CBO’s established reputation in the community, the CBO had greater reach to their seniors about the CBO’s activities, including HEHA. Highlighting their organization’s social standing in the community, one participant stated, “We understand our community. We [are] actually one of the leading organizations in this area. We have the network. We have the infrastructure.”
Available resources
CBOs with a long-standing history in the community generally had access to important resources, including, but not limited to, local radio programs, newspapers with advertisements publicizing health interventions, and staff members with experience in delivering similar health programs. Relationships with regional organizations and local communities also provided the CBO with multilingual teachers. Moreover, grant funding appeared supplementary to the CBOs as they ended up using the grant funding for supplies like pencils, paper, and gift cards. All participants mentioned already having adequate physical space and paid staff members to implement HEHA.
Culture
Organizational missions, norms, and values also played significant roles in facilitating the implementation of HEHA. While the mission of CBOs aligned with serving seniors and providing public health education, many participants reported having a larger vision of elevating the quality of life of seniors who are aging as an immigrant in the USA. For some, the larger vision and the sense of moral obligation to their community served as motivation to adopt and implement HEHA; they believed this program not only helped their seniors’ health but also improved their quality of life. When asked about how HEHA’s objective matched the CBO’s mission, a participant reported:
There’s no question. We are concerned with providing through our program – our mission is to provide quality of life so seniors can live independently and with dignity as long as possible.
Talking about a greater sense of responsibility for seniors aging as immigrants in the USA, one participant mentioned how part of their mission is to help the individuals they serve to “assimilate” into American culture and facilitate interactions with health care providers and health care delivery in the USA. Another mentioned the importance of supporting individuals who are “aging in place,” that is, providing support to seniors who wish to continue living independently in their place of residence; they believed it was the CBO’s duty to help their seniors achieve this.
Leadership engagement
All participants interviewed had leadership roles in their organization and they identified themselves as the champions for advocating and executing the implementation of HEHA in their organization. They also noted marketing the program outside of the organization to draw additional interest. Within their organization, they were strong voices advocating for the intervention at leadership meetings, and they assumed responsibility in leading the classes throughout the program. Some participants promoted HEHA among health care professionals and local politicians at a number of community gatherings, including religious settings and senior housing complexes, to engage seniors to participate in the program.
Characteristics of individuals
One construct, other personal attributes, emerged under the characteristics of individuals domain. This broad construct includes personal traits like motivation, values, competence, and learning style.
Other personal attributes
All participants were very motivated to execute HEHA at their respective CBOs. When the participants received the program materials, they were incredibly resourceful and used this opportunity to learn and make the program their own by adapting and tailoring it to their senior population. A participant mentioned that the materials were “challenging, but at the same time interesting” because it gave them the flexibility to “work around the basic concept.” The same participant continued to describe how he actively sought out resources by completing an “intensive online search” of the content so that he could learn first and then know how to tailor the materials for their clients. Another participant shared a similar sentiment and expressed the importance of experiencing the material first so that they could optimize the delivery to their clients.
I ha[d] to look at myself carefully…I ha[d] to experience it by myself and the Chinese trainer too. So, every step by step, you know, I ha[d] to do myself first. But once I digest it, it [was] very easy to deliver to the senior clients.
Overall, all participants shared high motivation to learn, gain competency of the materials, and adjust the materials to the needs of the senior clients to ensure the best delivery of HEHA.
Process
One construct, engaging, emerged under the process domain. Engaging includes strategies that participants from CBOs used to involve relevant individuals in the implementation of HEHA.
Engaging
Participants engaged key organizations to implement HEHA by forming close partnerships from broad cosmopolitanism networks. In many instances, participants collaborated with the seniors’ neighborhood grocery stores so that they would accept gift cards that were distributed to the seniors during HEHA. Seniors received these gift cards upon completion of the program. These cards were meant to encourage seniors, armed with new knowledge from HEHA, to purchase fresh fruits and vegetables at their local store.
Many participants also noted that a main facilitator to HEHA was attracting volunteers with experience teaching health programs to cultural groups and who had served as champions in heart health education. One partnership between a CBO serving a Japanese community and their local hospital leveraged the expertise of a health care professional. The participant explained:
The Japanese community had a bilingual nurse who works in hospitals here and he took the lead…to go over all the materials that [name of the primary leading organization] sent.
Another participant described partnering with volunteers:
Actually, we have quite a bit of volunteers. Okay? And we select the volunteers to do the different kinds of work and we select the people who have experiences, been a teacher before, and so they understand how to [work] with the audience, how to select the right topics and to control the conversations. So we trained these kind of volunteers to learn from different organizations…diabetes organizations and Alzheimer’s, dementia organizations, American Heart Associations.
DISCUSSION
This study examined the processes that facilitated the implementation of HEHA among CBOs serving older AAPIs. Our findings showed that implementation processes aligned with five domains of the CFIR construct: intervention characteristics, outer setting, inner setting, characteristics of individuals, and process. Among the five aligned domains, the inner setting domain emerged with the most constructs: structural characteristics, available resources, culture, and leadership engagement. The intervention characteristics had three constructs: evidence strength and quality, adaptability, and design quality and packaging. There was one construct that emerged for outer setting (i.e., cosmopolitanism), characteristics of individuals (i.e., other personal attributes), and process (i.e., engaging).
Our findings revealed that the participant’s decision to implement HEHA was rooted in their perception of HEHA’s strength and how they envisioned HEHA elevating their organization’s mission. Once that decision was made, participants were willing to go above and beyond to adapt the intervention content to their seniors, even if that meant additional training, resources, and partnerships. Thus, adaptability did not emerge as being key in the decision to implement but rather as a next step once the decision was made. The constructs noted in our study differ from what is most commonly noted in the literature. Many studies on implementation have noted “relative advantage” as being a common construct under the intervention characteristics’ domain for a variety of evidence-based interventions, including weight management programs, colorectal cancer programs, and Human Papillomavirus vaccination programs [16–18]. These studies also examined implementation in health care settings, where the setting already had an existing program. Therefore, practitioners in the community should first assess whether CBOs have existing programs that may compete with the new evidence-based intervention and, if not, provide data on the strength and quality of the new evidence-based intervention to help facilitate decision-making. Practitioners should remember that adaptations made to optimize intervention delivery are just as critical as the content. Thus, they should allow sufficient time and resources for CBOs to execute the adaptation process during implementation.
There were more constructs identified from CFIR’s inner setting domain than that of the outer setting. Although three inner setting constructs focused on organizational climate (structural characteristics, available resources, and culture) and were noted as being critical, it is noteworthy to highlight leadership engagement in the implementation of evidence-based interventions as participants mentioned going beyond the role of directing and leading to also adopt operational roles. While the implementation of evidence-based interventions in health care settings is dependent on front line health care providers, medical assistants, and students [19,20], this was not the case for CBOs. Leaders of CBOs, such as chief executive officers and executive directors, were involved in multiple steps of the implementation process with some engaging with seniors directly and delivered the health education classes. Other studies examining the implementation of evidence-based interventions in CBOs corroborated the importance of leadership engagement as being predictive of implementation outcome [9,21]. Additionally, the leaders whose values aligned with those of their CBOs were motivated to ensure the success of HEHA. Our findings show that these leaders were willing to go the extra mile to adapt the intervention content (culturally and linguistically) and ensure that the delivery was carefully planned based on their seniors’ needs. While there was a large sentiment that a systematic approach was used to deliver HEHA, many noted lacking a concrete plan as leaders were deeply involved in the day-to-day implementation. Research on implementation science indicates that, within and across organizations, having a formal implementation plan can help organizations prospectively identify goals and strategies, the scope of change, and milestones to track [22]. Future studies may want to explore the use of an implementation plan with CBOs and whether that improves the implementation process and sustained changes with CBOs.
Only one construct was observed for both outer setting (i.e., cosmopolitanism) and process (i.e., engaging) domains. Although these two constructs (cosmopolitanism and engaging) belonged to two different domains, from the organizational perspective, they were highly interrelated. The participants discussed the importance of networking with other national organizations to draw attention to local needs, as well as partnering with local organizations and local volunteers to do the work. Engagement with these networks was critical to the success of their work as resources for human capacity and for covering other costs were often tight. Other studies corroborate this finding: CBOs report frequently partnering with governmental organizations to advocate for solutions that address issues occurring within the community; this partnership helps bring their community’s issues to the government’s agenda and provides the CBO with additional support and increased visibility of the CBO in the community) [23]. Research done in the private industry had similar findings, where collaborating with other private industries provided access to external resources, and industries often aligned or mobilized existing internal resources with the external resources to accomplish greater work [24]. Rather than considering cosmopolitanism as the only outer setting construct, future studies may want to explore other constructs that impact implementation in CBOs.
Strengths and limitations
This study was one of the first to explore the implementation process of an evidence-based intervention in CBOs using the CFIR framework. Another strength is the ability to understand the perspectives of leaders of CBOs who are focused on providing services to vulnerable populations. This study has several limitations. First, CBOs in the study may not be representative of other CBOs who did not partner with a national organization. Therefore, the implementation process may vary across CBOs with different kinds of partnerships. Additionally, although we believe that we reached saturation, future studies should explore other constructs that did not emerge from CFIR, as well as constructs from other implementation frameworks. Finally, the CBOs that participated in HEHA served older AAPIs. CBOs who serve other populations may have organizational structures and processes that differ from those found to be successful in this study.
CONCLUSION
Cardiovascular disease is one of the leading causes of death for AAPIs aged 65 and older. Implementation of evidence-based interventions can help address cardiovascular disease. CBOs are critical settings for community health education. Our study highlights processes that facilitated the implementation of an evidence-based intervention in CBOs that serve older AAPIs. Understanding these processes can help accelerate dissemination and implementation of best practices in CBOs and ultimately address cardiovascular disease disparities among AAPIs
Acknowledgments
We would like to thank the community-based organizations that participated in this study.
Funding
This work was supported by the Fred Hutchinson Cancer Research Center development funds. L.K.K. was partially supported by the National Center for Advancing Translational Sciences of the National Institutes of Health Award number UL1 TR002319 and by Cooperative Agreement number 3 U48 DP005013-01S1A3 from the Centers for Disease Control and Prevention’s, Prevention Research Center’s Program and the National Cancer Institute. J.L. was partially supported by the de Tornyay Center for Healthy Aging Doctoral Scholarship, University of Washington School of Nursing. S.H.J. was fully supported by the National Institutes of Health through a training grant (5T32 CA 92408-18). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Compliance with Ethical Standards
Conflicts of Interest: All authors declare that they have no conflict of interest.
Authors’ Contributions: E.J.L. and L.K.K. contributed to the conceptualization and design of the study. S.K.B., E.V.R.B., L.K.K. and E.J.L. contributed to the implementation of the study and the data collection. S.H.J., J.L., and L.K.K. contributed to the data analysis. S.K.B., E.V.R.B., S.H.J., E.J.L., J.L., and L.K.K. contributed to the interpretation of the data. J.L. and L.K.K. contributed to the manuscript development. All authors contributed to critical revision of the manuscript for important intellectual content.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Institutional Review Board of the Fred Hutchinson Cancer Research Center. This article does not contain any studies with animals performed by any of the authors
Informed Consent: Informed consent (verbal) was obtained because the study presented no more than minimal risk of harm to subjects.
References
- 1. Administration for Community Living. Profile of Asian Americans age 65 and over. 2017. Available at https://acl.gov/sites/default/files/Aging%20and%20Disability%20in%20America/2017OAProfileAsAm508.pdf. Accessibility verified April 1, 2019.
- 2. Jose PO, Frank AT, Kapphahn KI, et al. Cardiovascular disease mortality in Asian Americans. J Am Coll Cardiol. 2014;64(23):2486–2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bazzano LA, Green T, Harrison TN, Reynolds K. Dietary approaches to prevent hypertension. Curr Hypertens Rep. 2013;15(6):694–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wang-Letzkus MF, Washington G, Calvillo ER, Anderson NL. Using culturally competent community-based participatory research with older diabetic Chinese Americans: Lessons learned. J Transcult Nurs. 2012;23(3):255–261. [DOI] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention. Improving health literacy for older adults: Expert panel report. 2009. Available at https://www.cdc.gov/healthliteracy/pdf/olderadults-508.pdf. Accessibility verified March 4, 2019.
- 6. Kwon SC, Rideout C, Patel S, et al. Improving access to healthy foods for Asian Americans, native Hawaiians, and Pacific Islanders: Lessons learned from the STRIVE Program. J Health Care Poor Underserved. 2015;26(2 suppl):116–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. American Heart Association. Check. Change. Control: Self-monitoring blood pressure control. Available at https://www.heart.org/-/media/data-import/downloadables/6/c/e/check-change-control-external-overview-ucm_457465.pdf. Accessibility verified April 4, 2019.
- 8. Lee EJ, Ko LK, Feng A, Bishop S. Healthy eating healthy aging: Community-based intervention program for older Asian American and Pacific Islanders. Innov Aging. 2018;2(suppl 1):458. [Google Scholar]
- 9. Gore R, Patel S, Choy C, et al. Influence of organizational and social contexts on the implementation of culturally adapted hypertension control programs in Asian American-serving grocery stores, restaurants, and faith-based community sites: A qualitative study. Transl Behav Med. 2019. doi: 10.1093/tbm/ibz106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Northridge ME, Kum SS, Chakraborty B, et al. Third places for health promotion with older adults: Using the consolidated framework for implementation research to enhance program implementation and evaluation. J Urban Health. 2016;93(5):851–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bach-Mortensen AM, Lange BCL, Montgomery P. Barriers and facilitators to implementing evidence-based interventions among third sector organisations: A systematic review. Implement Sci. 2018;13(1):103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ramanadhan S, Crisostomo J, Alexander-Molloy J, et al. ; PLANET MassCONECT C-PAC . Perceptions of evidence-based programs among community-based organizations tackling health disparities: A qualitative study. Health Educ Res. 2012;27(4):717–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med. 2012;43(3):337–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Damschroder LJ, Lowery JC. Evaluation of a large-scale weight management program using the consolidated framework for implementation research (CFIR). Implement Sci. 2013;8:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Leeman J, Askelson N, Ko LK, et al. Understanding the processes that federally qualified health centers use to select and implement colorectal cancer screening interventions: A qualitative study. Transl Behav Med. 2020;10(2):394–403. doi: 10.1093/tbm/ibz023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Garbutt JM, Dodd S, Walling E, Lee AA, Kulka K, Lobb R. Barriers and facilitators to HPV vaccination in primary care practices: A mixed methods study using the Consolidated Framework for Implementation Research. BMC Fam Pract. 2018;19(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Northridge ME, Kavathe R, Zanowiak J, Wyatt L, Singh H, Islam N. Implementation and dissemination of the Sikh American Families Oral Health Promotion Program. Transl Behav Med. 2017;7(3):435–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Brook J, McGraw C. Multidisciplinary perspectives: Application of the Consolidated Framework for Implementation Research to evaluate a health coaching initiative. Health Soc Care Community. 2018;26(3):e386–e395. [DOI] [PubMed] [Google Scholar]
- 20. Teeters LA, Heerman WJ, Schlundt D, Harris D, Barkin SL. Community readiness assessment for obesity research: Pilot implementation of the Healthier Families programme. Health Res Policy Syst. 2018;16(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wilcox S, Jake-Schoffman DE, Saunders RP, et al. Predictors of implementation in the Faith, Activity, and Nutrition dissemination and implementation study: Application of the Consolidated Framework for Implementation Research (CFIR) in a statewide initiative. Transl Behav Med. 2020. doi: 10.1093/tbm/ibaa025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lewis CC, Scott K, Marriott BR. A methodology for generating a tailored implementation blueprint: An exemplar from a youth residential setting. Implement Sci. 2018;13(1):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wilson MG, Lavis JN, Guta A. Community-based organizations in the health sector: A scoping review. Health Res Policy Syst. 2012;10:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zhang J, Wu W. Leveraging internal resources and external business networks for new product success: A dynamic capabilities perspective. Ind Mark Manage. 2017;61:170–181. [Google Scholar]