An international panel of experts identified 11 core communication competencies all healthcare providers should acquire to effectively support patients to make healthier lifestyle choices.
Keywords: Delphi process, Motivational communication, Behavioral change counseling, Physician training
Abstract
Poor health behaviors (e.g., smoking, poor diet, and physical inactivity) are major risk factors for noncommunicable chronic diseases (NCDs). Evidence supporting traditional advice-giving approaches to promote behavior change is weak or short lived. Training physicians to improve their behavior change counseling/communication skills is important, yet the evidence for the efficacy and acceptability of existing training programs is lacking and there is little consensus on the core competencies that physicians should master in the context of NCD management. The purpose of this study is to generate an acceptable, evidence-based, stakeholder-informed list of the core communication competencies that physicians should master in the context of NCD management. Using a modified Delphi process for consensus achievement, international behavior change experts, physicians, and allied health care professionals completed four phases of research, including eight rounds of online surveys and in-person meetings over 2 years (n = 13–17 participated in Phases I, III, and IV and n = 39–46 in Phase II). Eleven core communication competencies were identified: reflective listening, expressing empathy, demonstrating acceptance, tolerance, and respect, responding to resistance, (not) negatively judging or blaming, (not) expressing hostility or impatience, eliciting “change-talk”/evocation, (not) being argumentative or confrontational, setting goals, being collaborative, and providing information neutrally. These competencies were used to define a unified approach for conducting behavior change counseling in medical settings: Motivational Communication. The results may be used to inform and standardize physician training in behavior change counseling and communication skills to reduce morbidity and mortality related to poor health behaviors in the context of NCD prevention and management.
Implications.
Practice: “LEARN THE BASICS” proposes a simple way to introduce behavioral change counseling (BCC) in a fast-paced, time-efficient clinical setting and suggest that its successful application could significantly improve patient–provider relationships, chronic disease management, and health outcomes.
Policy: Implementing this training within Continuing medical education (CME)-accredited programs is expected to improve patient care and reduce morbidity and mortality related to poor health behaviors in noncommunicable chronic disease (NCD) patients.
Research: This study responds to the need for the development of an evidence-based, stakeholder-driven, and time-efficient communication style that may be used to improve BCC in the context of NCD management, and results from this study will be used to develop, in collaboration with stakeholders, an innovative Sequential Multiple Assignment Randomized Trial (SMART) that will allow to pragmatically test the clinical effectiveness of these BCC competencies to ensure longitudinal research engagement, which is critical for the future success of “LEARN THE BASICS”.
INTRODUCTION
According to the World Health Organization (WHO), nearly 71% of deaths worldwide are the result of noncommunicable chronic diseases (NCDs), including cardiovascular disease, cancer, chronic lung disease, diabetes, and obesity [1–5]. NCDs are heavily influenced by a cluster of common health risk behaviors, that is, smoking, poor diet, and physical inactivity [2,5–8], which have become the focus of treatment efforts among primary care and specialist physicians [9–11]. Traditionally, physicians have relied upon giving “persuasive information, education, and advice” as their primary approach to encourage patients to change health risk behaviors [12,13]. While well intentioned, this approach is met with low success rates [12,14], probably, because it fails to address issues related to motivation and confidence, both of which are critical for successful behavior change [15].
Despite the urgent need to address health risk behaviors in the context of NCD management, training in evidence-based behavior change counseling (BCC) techniques is not routinely offered as part of standard medical curricula [16–19]. This has led to an increased demand for BCC training through continuing medical education programs. Results from a recent systematic review focusing on the efficacy of BCC training programs for physicians in the context of NCD management suggests that these programs have been generally successful [20]. However, this review highlighted several important limitations of this literature, including the largely atheoretical nature of the training programs, as well as significant heterogeneity in terms of training structure and content. For example, 28 skills were taught across the nine studies reviewed; programs taught an average of 12 skills (range 6–21), and no study assessed the same training program or skill set more than once. Reporting quality was also very poor, which undermines reproducibility and hinders our ability to define appropriate “core” BCC training content and modalities for physicians. Furthermore, the studies reviewed did not appear to adhere to recommendations regarding stakeholder engagement and an integrative knowledge translation approach to program design, which may have led to the development of competencies that are of limited relevance to the end user [21,22]. Emerging evidence suggests that engaging relevant stakeholders play a key role in improving the translation and uptake of the results of interventions into clinical practice [23], a major criticism of BCC interventions for NCD management [24,25]. While existing programs may have demonstrated efficacy to improve BCC skills, the lack of stakeholder involvement in the development process (combined with no consensus on core content) will likely perpetuate the failure to translate effective BCC strategies into clinical practice as target audience “buy-in” is key to implementation success.
Despite the limitations highlighted by our previous review [20], results suggested that the most frequently taught BCC skills included the use of open-ended questions, eliciting “change-talk”, and, more broadly, using “motivational interviewing (MI) like” techniques (which includes the use of open-ended questions and eliciting “change-talk”, as well as reflective listening and collaborative goal setting). Despite its popularity and efficacy, there has been some resistance among physicians to undergo training in MI due to it being viewed as an “interviewing” technique that falls within the domain of psychosocial counseling, psychology, psychiatry, and “self-help” approaches [26]. MI has also been criticized as being too rigid, time consuming, and impractical for use in busy medical settings [27]. Finally, there is little research on the long-term uptake and maintenance of these techniques among physicians’ postmotivational interviewing training, and evidence suggests that even with ongoing training, supervision, and follow-up, proficiency levels rarely exceed beginner level [28].
There are a number of established theories that underlie BCC and motivational interviewing [15,29–31], and a systematic integrative knowledge translation approach could leverage these to determine the core set of BCC competencies that physicians should acquire to, then, define a new BCC approach for medical settings. In this study, the Canadian Network for Health Behavior Change and Promotion (CAN-Change, www.can-change.ca) has endeavored to make BCC training more appealing and acceptable to physicians by defining a new approach called Motivational Communication (MC). The purpose of this study was: (a) to determine the core content of a BCC training program in terms of the specific communication competencies to teach physicians and (b) to determine expert consensus on the definition of MC as an evidence-based communication approach for improving BCC in the context of NCD management.
METHODS
We conducted an international, modified Delphi study to determine expert consensus on the core communication competencies that physicians would need to acquire to effectively deliver BCC in practice. The Delphi method is a widely accepted group communication process for gathering information within a domain of expertise for the purpose of achieving a convergence of opinion on a specific issue [32–34]. The modified Delphi process is similar to the full Delphi in terms of procedure and purpose, the major difference being that the modified process begins with a set of carefully selected questions [32]. The advantages of this approach are that it improves the initial response rate and provides a solid theoretical grounding in previous work [32,35]. The present study was conducted as part of a larger program aimed at determining the core set of BCC competencies that physicians should acquire in the context of NCD prevention and management, which will form the basis of a training program that will undergo formal efficacy testing. This study represents the initial competency definition phase (consistent with ORBIT Model Phase I: define and refine phases) [36].
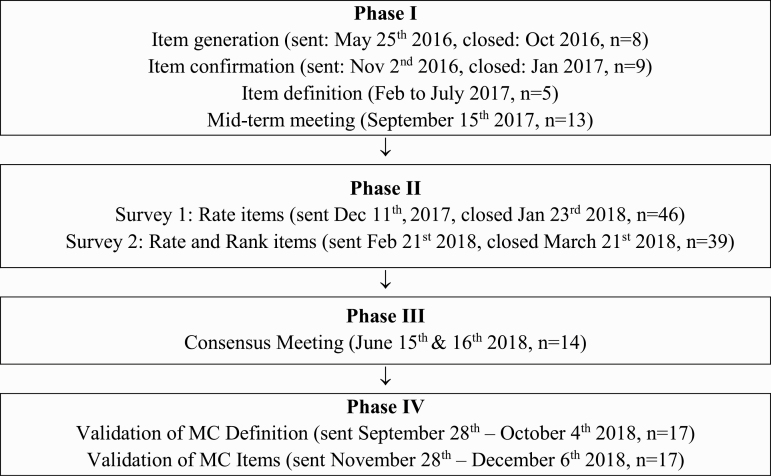
In the present study, the Delphi process involved four iterative phases (see Fig. 1): (a) generation, confirmation, and definition of all potentially relevant BCC attitudes and skills by a core development panel, culminating in a mid-term meeting with additional stakeholders to achieve consensus on the initial round of competencies that would be evaluated by an international panel of experts; (b) a two-round electronic survey among a larger sample of international experts to rank the competencies in order of importance for behavior change; (c) a consensus meeting with an expanded development panel (including physician stakeholders) to finalize the list of core BCC competencies and define a new BCC approach for physicians: MC; and (d) a final validation phase of the definition of MC through email correspondence with consensus-meeting participants. Ethical approval was provided from the Centre Intégré Universitaire de Santé et Services Sociaux du Nord-de-l’Ile-de-Montréal, Hôpital du Sacré-Coeur de Montréal, and all participants signed informed consent.
Fig 1.
Delphi process flow.
Participants
All behavior change experts included in this study were recruited by accessing relevant research networks and mailing lists through the International Behavioural Trials Network (IBTN; https://ibtnetwork.org/) and Can-Change [20]. In order to standardize the level of expertise, all behavioral experts were selected on the basis of being recognized experts in their field (e.g., having verifiable experience designing or delivering behavior change interventions), ≥7 years of clinical and/or research experience in the area of health behavior change, and self-rating their behavior change expertise as ≥7 on a 0 (no expertise) to 10 (expert) point Likert Scale. Participants were contacted by email with directions on how to access an electronic survey platform (Lime Survey). Once they had accessed the platform, they were invited to provide informed consent and complete the surveys. In total, 46 international behavior change experts and physicians completed eight rounds of surveys or in-person meetings (5–46 participants per round, 2 completing all 8 rounds; see Tables 1 and 3).
Table 1.
Demographic information
| Phase I | Phase II | Phase III | Phase IV | |||||
|---|---|---|---|---|---|---|---|---|
| Generation round | Confirmation round | Definition round | Mid-term meeting | Survey 1 | Survey 2 | Consensus meeting | Validation round | |
| Total (n) | 8 | 9 | 5 | 13 | 46 | 39 | 14 | 17 |
| Female (n, %) | 4 (50) | 5 (55) | 3 (60) | 6 (46) | 29 (63) | 25 (64) | 7 (50) | 8 (47) |
| Age (m, range) | 44 (29–61) | 44.2 (29–61) | 38.4 (27–44) | 40.1 (26–62) | 45 (28–68) | 44 (28–68) | 41.2 (24–62) | 45.6 (24–63) |
| Self-identified primary profession (n, %) | ||||||||
| University professor | 4 | 4 | 2 | 3 | 25 (54.3) | 23 (59) | 2 | 3 |
| Clinical psychologist | 4 | 5 | 0 | 3 | 13 (28.3) | 12 (30.1) | 2 | 3 |
| Other | 0 | 0 | 2 | 2 | 11 (23.9) | 9 (23) | 2 | 2 |
| Senior grad psyc student | 0 | 0 | 1 | 3 | 4 (8.7) | 3 (7.7) | 4 | 3 |
| Physician | 0 | 0 | 0 | 1 | 3 (6.5) | 3 (7.7) | 4 | 6 |
| Nurse | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Division of work for (average %)a | ||||||||
| Research | 48.8 | 48.9 | 75 | 47.5 | 49.6 | 51.6 | 47.5 | 42.9 |
| Teaching | 24.4 | 21.7 | 12.5 | 20.7 | 24.4 | 23.8 | 11.3 | 15.4 |
| Clinical | 18.8 | 22.2 | 7.5 | 23.8 | 15 | 16.9 | 34.4 | 34.5 |
| Other | 8.2 | 7.2 | 5 | 8.2 | 11 | 7.6 | 6.9 | 7.1 |
| Years of experience in behavior changea | ||||||||
| Average | 20 | 20 | 19 | 17.8 | 14.9 | 14.3 | 16.3 | 18.8 |
| Experience self-ratinga | ||||||||
| Average | 9.1 | 9 | 9 | 8.9 | 8.07 | 8.10 | 8.5 | 8.3 |
| Country of origin | ||||||||
| Canada | 8 | 9 | 5 | 13 | 30 | 25 | 14 | 17 |
| USA | – | – | – | – | 1 | 1 | – | – |
| Europe | – | – | – | – | 14 | 12 | – | – |
| Belgium | – | – | – | – | 1 | 1 | – | – |
| France | – | – | – | – | 2 | 2 | – | – |
| Ireland | – | – | – | – | 3 | 3 | – | – |
| Israel | – | – | – | – | 1 | 1 | – | – |
| Netherlands | – | – | – | – | 2 | 2 | – | – |
| Sweden | – | – | – | – | 1 | 1 | – | – |
| United Kingdom | – | – | – | – | 4 | 2 | – | – |
| Middle East | – | – | – | – | 1 | 1 | – | – |
| Saudi Arabia | – | – | – | – | 1 | 1 | – | – |
aScores of students and staff members were not included in the calculations as they did not qualify as behavioral change counseling experts. Other professions included: physiotherapist, dietician, nurse, occupational therapist, and social worker. Other type of work division included: consulting, administrative, and program development. All participants in Survey 2 took part in Survey 1.
Table 3.
Ratings of communication competencies cut after Phase III, Survey 1 and 2
| Survey 1 | Survey 2 | |||||
|---|---|---|---|---|---|---|
| Rating | ||||||
| Communication competencies | Low (%) | Med (%) | High (%) | Low (%) | Med (%) | High (%) |
| Negatively judging or blaming | 10.9 | 0.0 | 89.1 | 0 | 0 | 100 |
| Active listening | 2.2 | 10.9 | 87.0 | 0 | 12.8 | 87.2 |
| Displaying hostility and impatience | 10.9 | 2.2 | 87.0 | 0 | 0 | 100 |
| Acceptance, tolerance, and respect | 6.5 | 13.0 | 80.4 | 2.6 | 2.6 | 94.9 |
| Empathy | 2.2 | 19.6 | 78.3 | 0 | 7.7 | 92.3 |
| Setting goals | 0.0 | 28.3 | 71.7 | 0 | 15.4 | 84.6 |
| Willingness to understand | 6.5 | 21.7 | 71.7 | 0 | 25.6 | 74.4 |
| Responding to resistance | 6.5 | 23.9 | 69.6 | 0 | 10.3 | 89.7 |
| Eliciting “change-talk” | 2.2 | 30.4 | 67.4 | 0 | 12.8 | 87.2 |
| Collaboration/working toward a common goal | 4.3 | 28.3 | 67.4 | 2.6 | 20.5 | 87.2 |
| Guilting or shaming patients | 13 | 26.1 | 60.9 | 0 | 25.6 | 74.4 |
| Evocation | 4.3 | 39.1 | 56.5 | 0 | 20.5 | 79.5 |
| Responding to ambivalence | 4.3 | 39.1 | 56.5 | 0 | 10.3 | 61.5 |
| Being argumentative or confrontational | 15.2 | 28.3 | 56.5 | 2.6 | 20.5 | 76.9 |
| Reflective listening/using reflections | 2.2 | 47.8 | 50.0 | 0 | 10.3 | 59.0 |
| Open questions | 0 | 50.0 | 50.0 | 0 | 43.6 | 56.4 |
| Affirmation | 6.5 | 43.5 | 50.0 | 0 | 53.8 | 46.2 |
| Guiding relational style | 10.9 | 41.3 | 47.8 | – | – | – |
| Reinforcement management | 23.9 | 32.6 | 43.5 | – | – | – |
| Providing information (in a Socratic manner) | 6.5 | 54.3 | 39.1 | – | – | – |
| Behavior shaping | 10.9 | 52.2 | 37.0 | – | – | – |
| Stimulus control | 21.7 | 47.8 | 30.4 | – | – | – |
| Telling patients what to do (being prescriptive)/advice giving | 19.6 | 67.4 | 13.0 | – | – | – |
Delphi phases
Phase I: item generation, confirmation, and definition and mid-term meeting
Item generation.
A total of nine behavior change experts were contacted, of which eight (89% response rate) participated in the item generation phase of the Delphi process and formed our core development panel. Participant characteristics can be found in Table 1. The aim of the survey was to select the attitudes and skills that would ultimately form the core content of a BCC training program for physicians. Respondents were asked to answer the following question: “In a health care setting, what are the key attitudes and skills (behaviours) of the healthcare provider that facilitate or inhibit behavior change among patients?” Participants were invited to draw from the existing literature of evidence-based competencies for behavior change. In general, Behaviour change techniques found in Michie’s Taxonomy [37] and meta-analyses observing positive effects for MI-consistent communication skills [20,38] were considered evidence based. All items generated by the participants were accepted in the first list without any exceptions. The survey was launched in May 2016 and was closed in October 2016.
Item confirmation.
The same nine behavior change experts were contacted (100% response rate, eight of which were continuing from the previous round) and completed the confirmation round, which consisted of completing a second online survey. This round was composed of two questions. For the first question, all the attitudes and skills identified in the previous round were presented and the participants were asked to confirm that the list was exhaustive and that the results reflected their expert opinion on the core facilitative and inhibitory attitudes and skills for behavior change. No items were cut at this stage, only added. For the second question, participants were asked to rank all the attitudes and skills in order of their importance in facilitating or inhibiting behavior change in medical settings. The survey began in November 2016 and was closed in January 2017.
Item definition.
Our research team (A.I.D., K.L.L., S.L.B., and G.S.) worked to provide a working operational definition for each of the attitudes and skills identified by consulting behavior change theory and intervention literature [37,39–42]. Items were removed from the list if the group determined that their definitions overlapped significantly (agreement achieved by consensus).
Mid-term meeting.
A total of 13 behavior change experts (five of whom were part of the core development panel) were invited to attend an in-person mid-term meeting that was held during September 14–16, 2017 (see Table 1 for participant characteristics). All participants were supported to attend (if living outside Montreal) with study research funds. At this stage, more physician stakeholders were included to gather feedback from targeted end users. The aim of the meeting was to reduce redundancy between the different attitudes and skills and to confirm their operational definitions. The meeting started with a visual presentation detailing the results from the initial surveys, during which operational definitions of attitudes and skills were discussed and modified according to the discussion and validated by the group. Item redundancy was also discussed, and the panel voted to determine which items should be retained or removed from the list. Consensus was obtained for item inclusion or exclusion for all items discussed.
Phase II: Delphi surveys
This phase was conducted with the goal of distilling the information generated during the previous phase to arrive at an international consensus about which core attitudes and skills should be included in a BCC training program targeting physicians. In Survey 1, participants were presented the list of attitudes and skills (and their definitions) and asked to rate their importance (low importance = item is helpful but behavior change could be achieved without it [bottom third]; medium importance = item is desired for behavior change but not essential [middle third]; high importance = item is essential for effective behavior change [top third]). Survey 1 also included a brief demographic questionnaire, gathering information on: sex, country of residence/practice, number of years of research or clinical experience in behavior change, and self-ratings of expertise level (0 = no expertise and 10 = expert). Survey 1 was live from December 11, 2017, to January 23, 2018, and complete data were received from 46 participants (see Table 1).
Thirty days after they completed Survey 1, all participants were contacted by email and invited to complete Survey 2. Participants were presented with their previous personal rating, as well as the groups’ average rating from Survey 1 and asked to rate the importance of each attitude and skill (low, medium, or high). Participants were also asked to rank each attitude and skill according to their relative importance to each other. Survey 2 was live from February 21 to March 21, 2018, and 39 participants completed the survey (85% of which also completed Survey 1).
For both surveys, cutoff scores for the inclusion of the attitudes and skills into the next round were established prior to examining the data. There is no universally accepted standard for the minimum percentage of agreement. Consensus, which can be either agreement or disagreement with a statement, is defined as a percentage higher than the average percentage of majority opinion, where majority is defined as a percentage above 50% [43,44]. In this study, it was determined that attitudes and skills rated “high” less than 50% of the time in Survey 1 and less than 75% in Survey 2 would be excluded from the final list. Consensus thresholds chosen are similar to those adopted in other Delphi studies [45,46]. In Survey 2, a more conservative threshold was chosen to maximize the degree of stakeholder endorsement of the items present on the final list (see Table 3).
Phase III: final consensus meeting
A total of 14 participants (including 12 who attended the mid-term meeting and 5 from the core development panel) met in person from June 15 to 16, 2018 (see Table 1 for participant characteristics). All participants were supported to attend. Data from all phases of the process was presented and discussed until consensus on the final core list of attitudes and skills was achieved, and a working definition of MC was drafted. An independent qualitative research expert acted as a moderator for the meeting in order to ensure that all meeting objectives could be discussed within the available timeframe and all participants had an opportunity to share their views regarding every discussion point.
Phase IV: definition validation
Following the consensus meeting, the core list of communication competencies and the final definition of MC were emailed to all consensus-meeting participants for validation. All participants had 2 months (September 28–December 6, 2018) to provide feedback. Consensus was achieved on the core list of competencies and MC definition before concluding this phase of the research.
RESULTS
Phase I: item generation, confirmation, and definition
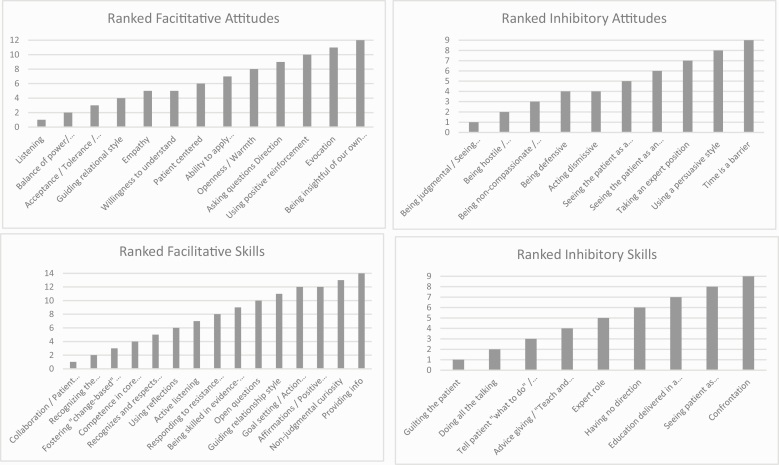
The item generation and confirmation rounds yielded 47 items (13 facilitative interpersonal attitudes, 10 inhibitory interpersonal attitudes, 15 facilitative communication skills, and 9 inhibitory communication skills; see Fig. 2). Following these two rounds, results showed that “Listening,” “Collaboration,” and “Tolerance” were the most highly endorsed attitudes considered to facilitate behavior change. Moreover, adopting a “Patient-centred counseling style,” “Understanding patients’ values,” and “Responding to ambivalence” were the most highly endorsed skills considered to facilitate behavior change. Regarding inhibitory attitudes, “Being judgmental” was the most highly endorsed inhibitory attitude, while “Shaming the patient,” “Doing all the talking,” and “Using a prescriptive counseling style” were the most highly endorsed inhibitory skills. Some items appeared as both “attitudes” and “skills” (e.g., “Listening,” Taking an expert role,” and “Guiding relational style). Though the distinction between “interpersonal attitudes” and “communication skills” was useful in the Generation and Confirmation rounds, following the Definition round, duplicate items were removed from the list in order to avoid redundancy and the “attitude versus skill” distinction was eliminated, with all items being, henceforth, referred to as communication competencies. Thus, following the Definition round, 39 communication competencies remained (see Supplementary Tables 1 and 2).
Fig 2.
Results from Phase I Rank of each facilitative and inhibitory attitudes and skills, where the smaller the number, the higher the item was ranked on average.
Phase II: mid-term meeting
During this phase, participants discussed further reducing redundancy in the list of communication competencies by grouping them into categories according to their definition. The aim was to ensure minimal overlap between the different items (i.e., every item is a unique competency not otherwise represented by another). This phase reduced their number from 39 to 23 (17 facilitative and 5 inhibitory communication competencies; see Table 2).
Table 2.
Phase II: mid-term meeting
| Category | Communication competencies |
|---|---|
| Listening | Active listening |
| Reflective listening/using reflections | |
| Empathy | Empathy |
| Nonjudgmental curiosity | Evocation |
| Open questions | |
| Eliciting “change-talk” | |
| Providing information (in Socratic manner) | Providing information |
| Assess and recognize readiness for change | Responding to resistance |
| Responding to ambivalence | |
| Goal setting | |
| Behavior shaping | |
| Stimulus control | |
| Reinforcement management | |
| Fostering a change-based relationship | Acceptance, tolerance, and respect |
| Guiding relational style | |
| Collaboration/working toward a common goal | |
| Willingness to understand | |
| Affirmation | |
| Taking on the expert role | Telling patients what to do (being prescriptive)/advice giving |
| Manipulating | Guilting or shaming patients |
| Being argumentative or confrontational | |
| Negatively judging and blaming | |
| Displaying hostility and impatience |
Phase III: Delphi surveys
A total of 256 behavioral experts were contacted, 90 of whom returned answers (35% response rate). Of these, 24 were excluded because they did not meet cutoff criteria for sufficient expertise in BCC and 20 were excluded because they provided only partial responses to the questionnaire. Survey 1 was completed by 46 individuals, and 39 of those (85%) completed Survey 2. Demographic information on participants who completed Surveys 1 and 2, respectively, is summarized in Table 1. Following the cutoff criteria previously described, 17 communication competencies remained after Survey 1, and 11 communication competencies after Survey 2 (see Table 3).
Phase IV: consensus meeting
A consensus meeting was held in Montreal on June 15 and 16, 2018, which began with a summary presentation of the results of the previous phases. Each of the 11 communication competencies that were identified in Phases I–III was individually discussed and a vote was held to determine consensus on whether each item should be included in the set of core communication competencies that should be taught to physicians. Consensus was reached regarding the inclusion of the 11 communication competencies. However, some participants suggested that “providing information neutrally” was a critical competency that should be returned to the list, despite it having been excluded during Survey 1. After a group discussion, a consensus was reached on readmitting this item to the list. Then, while discussing the overlapping operational definitions of “Evocation” and “Eliciting change-talk”, it was also agreed to merge these items into “Evocation of change-talk.” Other small modifications were made to the labeling and definitions of the different competencies to ensure uniformity of the list (see Supplementary Table 3). This left the following 11 items:
(1) Reflective listening
(2) Expressing empathy
(3) Demonstrating acceptance, tolerance, and respect
(4) Responding to resistance
(5) (not) Negatively judging or blaming
(6) (not) Expressing hostility or impatience
(7) Evocation of “change-talk”
(8) (not) Being argumentative or confrontational
(9) Setting goals
(10 ) Being collaborative
(11 ) Providing information neutrally.
The second objective of the consensus meeting was to determine and agree upon a definition of MC based on the core communication competencies identified in Phases I–III. All participants were asked to suggest elements that should be included in this definition. The following elements arose:
“should be a communication style”;
“developed to enhance the typical provider-patient interaction”;
“for multidisciplinary health-care providers”;
“approach informed by the behavioural sciences”;
“facilitates a long-term provider-patient relationship”;
“tailored to and consistent with meeting the patient’s needs, values, preferences and priorities”;
“facilitates informed decision-making by patients”;
“is time efficient and not an “add-on” intervention”;
“focuses on targeted outcomes: long-term behaviour change promotion/reduced risk behaviours/maintenance of changes/moving patients through the process of change”;
“achieves three goals: increases patients’ awareness of the ‘behavioural’ problem(s); their motivation to change behaviour; and their confidence in their ability to change behaviour.”
Using this list of elements identified, the research team drafted the following working definition of MC: “Motivational Communication (MC) is defined as an evidence-based, time-efficient communication style used by health care providers to promote sustained patient engagement and self-management of chronic conditions. It is informed by the behavioural sciences and emphasizes shared decision-making that is tailored to patients’ preferences, goals and values.”
Phase V: definition validation
In the early fall after the June consensus meeting (September 28, 2018), the working definition of MC was circulated by email to all consensus-meeting participants, in addition to three behavioral experts involved in earlier phases of the study (n = 17) for final validation. Consensus was achieved on the following definition of MC:
“Motivational Communication (MC) is defined as an evidence-based, time-efficient communication style used by health care providers to promote patient engagement, adoption of healthy behaviours, and sustained self-management of chronic conditions. It is informed by the behavioural sciences and emphasizes shared decision-making that is tailored to patients’ preferences, goals and values.”
Final mnemonic for the MC BCC program
Upon obtaining consensus on the communication competencies to be included in a definition of MC, the mnemonic LEARN THE BASICS was generated by considering the first letters of each competency (see Figure 3) to describe a new physician training program that would be developed to teach these competencies to physicians.
Fig 3.
Mnemonic for the 11 motivational communication competencies.
DISCUSSION
The purpose of this study was: (a) to determine the set of core communication competencies that validly represent MC as a BCC approach that can be used by physicians (and other health care providers) and (b) to achieve expert consensus on the definition of MC as an evidence-based approach for improving BCC in physicians working in the context of NCD management.
We sought feedback from an international sample of behavioral experts using a rigorous, structured methodology (which included a Delphi consensus process and several face-to-face meetings) to achieve consensus on a core set of communication competencies and a final definition of MC. We were able to confirm 11 communication competencies consistent with that definition. These competencies can be summarized by the simple mnemonic LEARN THE BASICS: Listening, Empathy, Acceptance, tolerance, and respect, Responding to resistance, (not) Negatively judging, (not) Expressing Hostility or impatience, Evocation of “change-talk,” (not) Being argumentative, Setting goals, Information, and Collaboration. To our knowledge, this is the first study to use a systematic consensus approach incorporating the views of relevant multidisciplinary stakeholders (e.g., behavioral experts, physicians, nurses, and health administrators) to achieve consensus on what core BCC communication competencies physicians should acquire in the context of NCD management. While this set of competencies was developed to target the promotion of good health behaviors in the context of NCD, these communication skills may be valuable in the context of other medical settings and conditions where there are behavioral issues to address (e.g., vaccination, medication adherence, and practicing safe sexual practices).
Training in evidence-based BCC and interest in patient–provider communication has been gaining attention in recent years. In 2015, the Royal College of Physicians and Surgeons of Canada presented CanMEDS, a framework outlining the core competencies physicians need to acquire to effectively meet the health care needs of the people they serve [38] (http://www.royalcollege.ca/rcsite/canmeds/canmeds-framework-e). Consistent with this, we generated a definition of MC that represents the needs of relevant stakeholders, which emphasizes MC as a communication (rather than interview) strategy. MC and its core competencies align with that of the role of a “communicator” described by CanMEDS. This provides support for MC’s pertinence and likely acceptability and suggests that physicians may be more likely to undergo BCC training if the terminology used to describe the approach is in line with national training frameworks. Finally, the competencies that make up MC can be used alone or in combination (depending on the therapeutic goals). This lends them to be seamlessly incorporated into practice without increasing consultation length, which was deemed important to physician stakeholders and may further increase their uptake in practice. Although stakeholder (physician) input does not guarantee widespread acceptance of the program by physicians, we believe that our stakeholder engagement approach was a critical first step to increasing the acceptance and uptake of the approach in practice.
Results from this study are being used to develop, in collaboration with key stakeholders, a MC-based BCC training program targeting physicians. This program will be developed to be delivered both in person and online to increase reach and impact. The first iteration of the program will undergo proof-of-concept testing to determine the minimum dose of training needed for physicians to achieve competency in these skills (followed by pilot testing and efficacy testing as per ORBIT [36]). Since this is a newly defined approach for BCC, we are also developing, in parallel, a competency assessment tool to objectively assess physician competencies in these core skills [47]. We are also developing this tool using an integrated knowledge translation approach that engages relevant stakeholders (i.e., physicians) in the development and testing process, which we believe will increase physician engagement and optimize the efficacy of these important training programs.
Study limitations and strengths
The Delphi process is an effective and valid technique to achieve the convergence of expert opinion on a specific question [33]. However, the results of this study should be interpreted within the context of certain limitations. First, the experts included in the initial Delphi round were selected from a small group of experts from a single Canadian network (Can-Change). While a limited number of experts generated the initial list, participants were from four Canadian provinces (Alberta, Ontario, Quebec, and Nova Scotia) and were both English (n = 6) and French (n = 2) speaking, which increases generalizability. The survey was then extended to international experts by leveraging the IBTN (343 members across 6 continents), which permitted an increase in participant heterogeneity in subsequent Delphi phases.
Second, the format of the Delphi can be a lengthy process for participants, who are contacted multiple times to verify the data collected and offer their input to further the process. This feature could impact the retention rate of participants from one phase to the next (though we only lost seven participants from Survey 1 to 2). Lastly, there is no standardized definition of what ‘consensus’ is and when it is reached. This indicates that there may be some measure of bias in decision-making as the consensus moderator must decide when a sufficient level of consensus has been reached. However, if the moderator is independent of the study and the clinical question is defined prior to the start of the project and the criteria for consensus are determined prior to examining the data, this can minimize bias [34].
Despite some limitations, this study also has a number of notable strengths. First, the Delphi process is a highly structured method providing rigorous guidelines for achieving consensus. It offers a convenient alternative to other qualitative research methods, such as focus groups and in-person interviews, which can be highly burdensome [48]. Second, the stakeholder involvement in the development process represents a major strength guaranteeing successful translation of BCC strategies into clinical practice. Moreover, the sampling of views from multiple stakeholders from around the world and chosen to respond to rigorous expertise criteria increases both the validity and representativeness of the views expressed. Finally, the Delphi surveys protect the participant’s anonymity within the group and eliminate the possibility of bias that can occur in in-person group conversations [34].
CONCLUSION
The burden of NCDs and the role of poor health behaviors in their development and progression is well documented as is the role of patient–health care provider communication. This study responds to the need for the development of an evidence-based, stakeholder-driven, and time-efficient communication style that may be used to improve BCC in the context of NCD management. We used an international iterative Delphi process to achieve consensus on the core communication competencies that physicians should acquire to improve BCC with NCD patients that were informed by physicians and deemed physician relevant and practice specific. These competencies were summarized to define “Motivational Communication.” Results from this study indicate that there are 11 communication competencies that represent the basic elements to master in order to achieve competency in BCC and represent, by extension, the core content of a training program for physicians. Maintaining longitudinal physician engagement will be critical for the future success of the “LEARN THE BASICS” program, and eventual implementation of this training within Continuing medical education-accredited programs is expected to improve patient care and reduce morbidity and mortality related to poor health behaviors in NCD patients.
Supplementary Material
Funding
This study was funded by Canadian Institutes of Health Research [325647].
Compliance with Ethical Standards
Conflicts of Interest: A.I.D., V.G.B., S.L.B., C.G., G.S., G.G., C.R., D.R., J.G.D., and W.G. declare that they have no conflict of interest. M.T.V. has received research grants from Bausch Health and Novo Nordisk. M.T.V. is a consultant to Lifescan, Novo Nordisk, Abbvie, and Bausch Health. M.T.V. has received a speaker honorarium from Nov Nordisk, Abbvie, Lifescan, Baush Health, and Merck. S.K.L. is a consultant for Janssen, Astellas, Astra-Zeneca, Novartis, and Boehringer Ingelheim. K.L.L. has received honorarium from Janssen, Astellas, Astra-Zeneca, Novartis, Boehringer Ingelheim, Bayer, and Abbvie (all for presentations given in the area of motivational communication, behavior change for chronic disease prevention, or stress and chronic disease). K.C. has received a speaker honorarium from Novo Nordisk and Janssen.
Authors’ Contributions
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
References
- 1. World Health Organization (WHO). Noncommunicable diseases: Fact sheet. 2018. Available at http://www.who.int/en/news-room/fact-sheets/detail/noncommunicable-diseases. Accessibility October 23, 2018.
- 2. Stallones RA. The association between tobacco smoking and coronary heart disease. Int J Epidemiol. 2015;44(3):735–743. [DOI] [PubMed] [Google Scholar]
- 3. González K, Fuentes J, Márquez JL. Physical inactivity, sedentary behavior and chronic diseases. Korean J Fam Med. 2017;38(3):111–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Micha R, Shulkin ML, Peñalvo JL, et al. Etiologic effects and optimal intakes of foods and nutrients for risk of cardiovascular diseases and diabetes: Systematic reviews and meta-analyses from the Nutrition and Chronic Diseases Expert Group (NutriCoDE). PLoS One. 2017;12(4):e0175149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ng R, Sutradhar R, Yao Z, Wodchis WP, Rosella LC. Smoking, drinking, diet and physical activity—Modifiable lifestyle risk factors and their associations with age to first chronic disease. Int J Epidemiol. 2019:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lavoie KL, Bacon SL, Labrecque M, Cartier A, Ditto B. Body mass index is associated with worse asthma control and quality of life among adult asthma patients. Respir Med. 2006;100(4):648–657. [DOI] [PubMed] [Google Scholar]
- 7. Strine TW, Balluz LS, Ford ES. The associations between smoking, physical inactivity, obesity, and asthma severity in the general US population. J Asthma. 2007;44(8):651–658. [DOI] [PubMed] [Google Scholar]
- 8. Forno E, Celedón JC. The effect of obesity, weight gain, and weight loss on asthma inception and control. Curr Opin Allergy Clin Immunol. 2017;17(2):123–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Beaglehole R, Bonita R, Horton R, et al. ; Lancet NCD Action Group; NCD Alliance . Priority actions for the non-communicable disease crisis. Lancet. 2011;377(9775):1438–1447. [DOI] [PubMed] [Google Scholar]
- 10. Bonita R, Magnusson R, Bovet P, et al. ; Lancet NCD Action Group . Country actions to meet UN commitments on non-communicable diseases: A stepwise approach. Lancet. 2013;381(9866):575–584. [DOI] [PubMed] [Google Scholar]
- 11. Glantz S, Gonzalez M. Effective tobacco control is key to rapid progress in reduction of non-communicable diseases. Lancet. 2012;379(9822):1269–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Elder JP, Ayala GX, Harris S. Theories and intervention approaches to health-behavior change in primary care. Am J Prev Med. 1999;17(4):275–284. [DOI] [PubMed] [Google Scholar]
- 13. Rollnick S, Butler CC, McCambridge J, Kinnersley P, Elwyn G, Resnicow K. Consultations about changing behaviour. BMJ. 2005;331(7522):961–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Damrosch S. General strategies for motivating people to change their behavior. Nurs Clin North Am. 1991;26(4):833–843. [PubMed] [Google Scholar]
- 15. Deci E, Ryan RM. Intrinsic Motivation and Self-Determination in Human Behavior. New York, NY: Springer; 1985. [Google Scholar]
- 16. Vanderhoek AJ, Hammal F, Chappell A, Wild TC, Raupach T, Finegan BA. Future physicians and tobacco: an online survey of the habits, beliefs and knowledge base of medical students at a Canadian University. Tob Induc Dis. 2013;11(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Richmond R, Zwar N, Taylor R, Hunnisett J, Hyslop F. Teaching about tobacco in medical schools: A worldwide study. Drug Alcohol Rev. 2009;28(5):484–497. [DOI] [PubMed] [Google Scholar]
- 18. Weiler R, Chew S, Coombs N, Hamer M, Stamatakis E. Physical activity education in the undergraduate curricula of all UK medical schools: Are tomorrow’s doctors equipped to follow clinical guidelines? Br J Sports Med. 2012;46(14):1024–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Twardella D, Brenner H. Lack of training as a central barrier to the promotion of smoking cessation: A survey among general practitioners in Germany. Eur J Public Health. 2005;15(2):140–145. [DOI] [PubMed] [Google Scholar]
- 20. Dragomir AI, Julien CA, Bacon SL, Boucher VG, Lavoie KL; Canadian Network for Health Behavior Change and Promotion (CAN-Change) . Training physicians in behavioural change counseling: A systematic review. Patient Educ Couns. 2019;102(1):12–24. [DOI] [PubMed] [Google Scholar]
- 21. Frank L, Forsythe L, Ellis L, et al. Conceptual and practical foundations of patient engagement in research at the patient-centered outcomes research institute. Qual Life Res. 2015;24(5):1033–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gagliardi AR, Berta W, Kothari A, Boyko J, Urquhart R. Integrated knowledge translation (IKT) in health care: A scoping review. Implement Sci. 2016;11:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Goodman MS, Sanders Thompson VL. The science of stakeholder engagement in research: Classification, implementation, and evaluation. Transl Behav Med. 2017;7(3):486–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kristensen N, Nymann C, Konradsen H. Implementing research results in clinical practice—The experiences of healthcare professionals. BMC Health Serv Res. 2016;16:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dragomir AI, Bacon, SL, Boucher VG, Szczepanik G, Lavoie KL. 2018 International Behavioural Trials Network (IBTN) Conference Abstracts. Ann Behav Med. 2019;53(3):296–298. [Google Scholar]
- 26. Adler KG. The unexpected challenge of motivational interviewing. Fam Pract Manag. 2016;23(5):9. [PubMed] [Google Scholar]
- 27. Miller WR, Amrhein P, Yahne CE, Tonigan JS. A Motivational Interviewing Failure: Hazards of a Therapy Manual? New Mexico: Clinical Research Branch, University of New Mexico Center on Alcoholism, Substance Abuse and Addictions (CASAA); 2011. [Google Scholar]
- 28. Weisner C, Satre DD. A key challenge for motivational interviewing: Training in clinical practice. Addiction. 2016;111(7):1154–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. [DOI] [PubMed] [Google Scholar]
- 30. Beck AT. The current state of cognitive therapy: A 40-year retrospective. Arch Gen Psychiatry. 2005;62(9):953–959. [DOI] [PubMed] [Google Scholar]
- 31. Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38–48. [DOI] [PubMed] [Google Scholar]
- 32. Custer RL, Scarcella JA, Stewart BR. The modified Delphi technique—A rotational modification. J Voc Tech Educ. 1999;15(2):50–58. [Google Scholar]
- 33. Hsu C-C, Sandford BA. The Delphi technique: Making sense of consensus. Pract Assess Res Eval. 2007;12(10):1–8. [Google Scholar]
- 34. Murry JW, Hammons JO. Delphi: A versatile methodology for conducting qualitative research. The Review of Higher Education. 1995;18(4):423–436. [Google Scholar]
- 35. Elwyn G, O’Connor A, Stacey D, et al. Developing a quality criteria framework for patient decision aids: Online international Delphi consensus process. BMJ. 2006;333(7565):417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Czajkowski SM, Powell LH, Adler N, et al. From ideas to efficacy: The ORBIT model for developing behavioral treatments for chronic diseases. Health Psychol. 2015;34(10):971–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. [DOI] [PubMed] [Google Scholar]
- 38. Lundahl B, Moleni T, Burke BL, et al. Motivational interviewing in medical care settings: A systematic review and meta-analysis of randomized controlled trials. Patient Educ Couns. 2013;93(2):157–168. [DOI] [PubMed] [Google Scholar]
- 39. Miller WR, Rollnick S. Motivational Interviewing, Third Edition: Helping People Change. New York, NY: Guilford Publications; 2012. [Google Scholar]
- 40. Rollnick S, Miller WR. What is motivational interviewing? Behav Cogn Psychother. 1995;23(4):325–334. [DOI] [PubMed] [Google Scholar]
- 41. Rollnick S, Miller WR, Butler C. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York, NY: Guilford Press; 2008. [Google Scholar]
- 42. Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: A systematic review and meta-analysis. Br J Gen Pract. 2005;55(513):305–312. [PMC free article] [PubMed] [Google Scholar]
- 43. von der Gracht HA. Consensus measurement in Delphi studies. Technol Forecasting Soc Change. 2012;79(8):1525–1536. [Google Scholar]
- 44. Stewart D, Gibson-Smith K, MacLure K, et al. A modified Delphi study to determine the level of consensus across the European Union on the structures, processes and desired outcomes of the management of polypharmacy in older people. PloS One. 2017;12(11):e0188348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Byrne M, O’Connell A, Egan AM, et al. A core outcomes set for clinical trials of interventions for young adults with type 1 diabetes: An international, multi-perspective Delphi consensus study. Trials. 2017;18(1):602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Terwee CB, Prinsen CAC, Chiarotto A, et al. COSMIN methodology for evaluating the content validity of patient-reported outcome measures: a Delphi study. Qual Life Res. 2018;27(5):1159–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Boucher VG, Gemme C, Dragormir AI, Szczepanik G, Bacon SL, Lavoie KL. The development of an evaluation tool for assessing the acquisition of motivational communication skills among physicians using an integrated KT approach. International Behavioural Trials Network Conference Abstracts. Ann Behav Med. 2019;53(3):296–298. [Google Scholar]
- 48. Dalkey N, Helmer O. An experimental application of the Delphi method to the use of experts. Manage Sci. 1962;9:458–467. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.