Abstract
Objective
To investigate the association between discordant β-amyloid (Aβ) PET and CSF biomarkers at baseline and the emergence of tau pathology 5 years later.
Methods
We included 730 Alzheimer's Disease Neuroimaging Initiative (ADNI) participants without dementia (282 cognitively normal, 448 mild cognitive impairment) with baseline [18F]florbetapir PET and CSF Aβ42 available. Aβ CSF/PET status was determined at baseline using established cutoffs. Longitudinal data were available for [18F]florbetapir (Aβ) PET (baseline to 4.3 ± 1.9 years), CSF (p)tau (baseline to 2.0 ± 0.1 years), cognition (baseline to 4.3 ± 2.0 years), and [18F]flortaucipir (tau) PET (measured 5.2 ± 1.2 years after baseline to 1.6 ± 0.7 years later). We used linear mixed modeling to study the association between Aβ CSF/PET status and tau pathology measured in CSF or using PET. We calculated the proportion of CSF+/PET− participants who during follow-up (1) progressed to Aβ CSF+/PET+ or (2) became tau-positive based on [18F]flortaucipir PET.
Results
Aβ CSF+/PET+ (n = 318) participants had elevated CSF (p)tau levels and worse cognitive performance at baseline, while CSF+/PET− (n = 80) participants were overall similar to the CSF−/PET− (N = 306) group. Five years after baseline, [18F]flortaucipir PET uptake in the CSF+/PET− group (1.20 ± 0.13) did not differ from CSF−/PET− (1.18 ± 0.08, p = 0.69), but was substantially lower than CSF+/PET+ (1.48 ± 0.44, p < 0.001). Of the CSF+/PET− participants, 21/64 (33%) progressed to Aβ CSF+/PET+, whereas only one (3%, difference p < 0.05) became tau-positive based on [18F]flortaucipir PET.
Conclusions
Aβ load detectable by both CSF and PET seems to precede substantial tau deposition. Compared to participants with abnormal Aβ levels on both PET and CSF, the CSF+/PET− group has a distinctly better prognosis.
β-Amyloid (Aβ) plaques and neurofibrillary tau tangles are considered the pathologic hallmarks of Alzheimer disease (AD).1 Aβ pathology can be measured in vivo directly by quantifying the fibrillary depositions using PET, or indirectly by detecting the decrease of soluble Aβ42 in CSF. Although these 2 measures are sometimes considered interchangeable,2–4 10%–20% of cases show discordant results, especially at earlier stages of AD.5–7 Therefore, it has been proposed that decreased Aβ42 in CSF without significant tracer uptake on PET (i.e., Aβ CSF+/PET−) marks the pathologic beginnings of Aβ accumulation.8,9 This provides a powerful model to study the dynamic changes in Aβ as well as tau pathology during the earliest stages in the disease course of AD. Although CSF tau biomarkers have been available for over 2 decades,10 tau PET using radiotracers such as [18F]flortaucipir11,12 has only more recently been developed. Tau PET offers the unique opportunity to study the spatial distribution of tau aggregates in vivo.
An open question to date is whether isolated Aβ positivity in CSF is followed by significant tau deposition already at this stage, or whether it will be subsequent to more advanced Aβ pathology detectable by both modalities (i.e., CSF and PET). As tau has a stronger correlation to neurodegeneration and cognitive function than Aβ accumulation,13,14 this is of high clinical relevance. Furthermore, a better understanding of the interplay between the AD hallmark pathologies in early disease stages is crucial for the timing of interventions, as emerging treatments will likely be most effective when substantial neurodegeneration has not yet developed.15 The aim of this study was therefore to use multimodal tau biomarkers and cognitive tests to explore the Aβ CSF/PET discordance.
Methods
Participants
Data for this study were downloaded from the Alzheimer's Disease Neuroimaging Initiative (ADNI) website (adni.loni.usc.edu/), which also includes information about ADNI inclusion criteria and the procedure of biomarker acquisition.16 We selected all ADNI participants who had at least 1 [18F]florbetapir Aβ PET scan and a CSF Aβ42 analysis available within 1 year. The diagnosis closest to baseline [18F]florbetapir PET within 1 year was used as the baseline diagnosis. In total, we included 730 participants without dementia, of whom 282 were cognitively normal (CN) and 448 had mild cognitive impairment (MCI) at baseline.
We used the Mini-Mental State Examination (MMSE) to assess global cognition and composite z scores to assess memory17 and executive functioning.18 Longitudinal cognitive assessment was available for 711 (97%) participants, with a median follow-up time of 4.2 years (interquartile range [IQR] 2.9, 5.9). Similarly, a follow-up diagnosis was available for 724 (99%) participants, with a median interval between baseline and follow-up of 4.1 years (IQR 2.2, 5.9).
Standard protocol approvals, registrations, and patient consents
Written informed consent was obtained for all participants, and study procedures were approved by the institutional review board at each of the participating centers. ADNI is listed in the ClinicalTrials.gov registry (ADNI-1: NCT00106899; ADNI-GO: NCT01078636; ADNI-2: NCT0123197).
[18F]Florbetapir PET
Acquisition and processing of [18F]florbetapir PET using Freesurfer was performed as described previously.19,20 At least one follow-up PET scan was available for 579 (79%) participants with a median follow-up time of 4.1 years (IQR 2.1, 5.9). We used a neocortical composite score provided by ADNI consisting of the mean uptake in the frontal, cingulate, parietal, and temporal regions. We created standardized uptake value ratios (SUVRs) using whole cerebellum as the reference region and used an SUVR cutoff of 1.11 to determine binarized Aβ status based on PET.21,22 For longitudinal linear mixed modeling, we additionally used SUVR values in 34 regions from the Desikan-Killiany atlas using the whole cerebellum23 and a composite white matter region as reference regions, because the latter has been shown to be more reliable in longitudinal analyses.24 Finally, we used an early composite region identified in a recent study25 (including bilateral precuneus, posterior cingulate, insula, and medial and lateral orbitofrontal regions) to capture the early accumulation of Aβ.
CSF studies
Lumbar punctures were performed as previously described.26 CSF samples were frozen on dry ice after collection and transported to the UPenn Medical Center ADNI Biomarker Core laboratory. Thereafter, 0.5 mL aliquots were prepared and stored in polypropylene tubes at −80°C. CSF samples were analyzed for Aβ42, total tau (t-tau), and phosphorylated tau (p-tau) using the AlzBio3 assays (Fujirebio) on the xMAP platform (Luminex). In case samples were reanalyzed, we used the median value of those results. A cutoff of 192 pg/mL was used to determine Aβ status based on CSF.26,27 Longitudinal CSF analyses were available for 297 (41%) of participants with median follow-up time of 2.0 years (IQR 2.0, 2.0).
[18F]Flortaucipir PET
[18F]Flortaucipir PET was performed at each ADNI site according to standardized protocols. Images were acquired via 4 × 5 minute frames from 80 to 100 minutes after injecting ∼370 MBq of [18F]flortaucipir. [18F]Flortaucipir PET was available for 253 (35%) participants and was performed a median of 5.2 years (IQR 4.2, 6.1) after baseline [18F]florbetapir PET, allowing measuring tau pathology at a significantly later time point. Of these participants, 110 had 1 follow-up scan after 1.3 years (IQR 1.0, 2.1). We used Freesurfer-defined Desikan-Killiany atlas regions provided by ADNI that were created by coregistering the [18F]flortaucipir image with a previously parcellated and segmented MRI magnetization-prepared rapid gradient echo from the same time.28 Thereafter, we created 3 bilaterally volume-weighted composite regions to cover the full spectrum of tau aggregation: entorhinal cortex, temporal meta–region of interest (ROI) reflecting Braak stage I to IV (including entorhinal, parahippocampal cortex, amygdala, fusiform, inferior and middle temporal cortices), and Braak stage V and VI (including wider neocortical areas).29–31 Cutoffs (1.39, 1.34, and 1.28 SUVR, respectively) obtained using a similar PET pipeline were used to determine [18F]flortaucipir positivity.32
Statistical analysis
We selected the first available [18F]florbetapir PET as baseline Aβ PET, and CSF Aβ42 closest in time within 1 year to the [18F]florbetapir PET as baseline CSF. Thereafter, we created 4 groups based on the binarized Aβ status on PET and CSF: concordantly amyloid-negative (CSF−/PET−), concordantly amyloid-positive (CSF+/PET+), discordantly amyloid-positive based on CSF (CSF+/PET−) or PET (CSF−/PET+). Participant groups were compared using χ2 tests, 2-sample t tests, and Wilcoxon rank-sum tests. Statistical analysis was performed using R software version 3.6.3.33–36
We used linear mixed modeling to investigate longitudinal changes for (1) regional Aβ burden assessed by [18F]florbetapir PET, (2) tau pathology assessed by CSF t-tau, p-tau (measured from baseline), and [18F]flortaucipir PET (first measured 5 years after baseline), and (3) cognitive measures (MMSE, and ADNI memory and executive composite scores). The models included time in years as a continuous variable, Aβ CSF/PET group, and an interaction between time * CSF/PET group. All models also included terms for age and sex. The models predicting regional Aβ PET and tau pathology based on CSF or PET were additionally adjusted for MMSE to account for clinical disease severity. The models predicting cognitive test results were additionally adjusted for education. We used a random intercept and a random slope for all models. We first selected CSF−/PET− as the reference group and interpreted the main effect of CSF/PET group status (CSF−/PET+ and CSF+/PET−) in the models as difference at baseline, and the CSF/PET group * time interaction term as the change over time. Thereafter, we repeated this analysis with CSF+/PET+ as the reference group. We also tested whether these effects are consistent (1) when using random samples from the CSF+/PET+ group in order to achieve a similar 50%/50% CN/MCI ratio compared the other groups or (2) when covarying for APOE ɛ4 carriership. We then performed Kaplan-Meier survival analyses to investigate the association between Aβ CSF/PET status and clinical progression for CN participants (progression to MCI or dementia) and participants with MCI (progression to dementia). We additionally conducted Cox regression analyses to obtain post hoc hazard ratios (HRs) for each of the Aβ CSF/PET profiles.
Finally, we performed 2 analyses in CSF+/PET− participants only. First, to investigate subthreshold levels of tau pathology in the Aβ CSF+/PET− group, we performed linear regression models with Aβ pathology measured by [18F]florbetapir PET (globally as well as in early accumulating regions25) at baseline as the predictor, with cross-sectional tau pathology measured by either CSF t-tau or p-tau (at baseline) or the 3 composite regions of [18F]flortaucipir PET (5 years later) as the outcome. Second, we investigated our hypothesis that progression from Aβ CSF+/PET− to CSF+/PET+ occurs at a higher rate than progression to tau positivity based on [18F]flortaucipir PET. We calculated the proportions of CSF+/PET− participants who (1) during the follow-up period converted into the CSF+/PET+ group based on the last available [18F]florbetapir PET scan and CSF analysis and (2) whose last available [18F]flortaucipir PET was positive in any of the 3 composite regions. We compared these outcomes by testing for overlapping 95% confidence intervals (CIs) on estimated proportions. Last available [18F]flortaucipir PET was performed a median of 6.0 years (IQR 5.5, 6.8) after baseline and 0.0 years (−2.0, 1.4) from last available [18F]florbetapir PET.
Data availability
All imaging, demographic, and neuropsychological data used in this article are publicly available and were downloaded from the ADNI website (adni.loni.usc.edu). Upon request, we will provide a list of ADNI participant identifications for replication purposes.
Results
Study participants
Of the study participants, 306 (42%) were CSF−/PET−, 80 (11%) CSF+/PET−, 26 (4%) CSF−/PET+, and 318 (44%) CSF+/PET+. Characteristics were overall similar between CSF−/PET− and the 2 discordant groups. Participants in the CSF+/PET+ group were older at baseline and at symptom onset, had a higher proportion of APOE ε4 carriers, were more often diagnosed with MCI, and had lower cognitive scores, higher CSF (p)tau levels at baseline, and higher [18F]flortaucipir PET uptake 5 years later (table; data available from Dryad, table 2, doi.org/10.5061/dryad.c59zw3r49).
Table.
Study participants
Accumulation of Aβ
First, we assessed regional [18F]florbetapir patterns across groups (figure 1; data available from Dryad, table 3, doi.org/10.5061/dryad.c59zw3r49). Although the CSF−/PET+ group had more tracer uptake at baseline than CSF−/PET−, they did not accumulate significantly more Aβ over time on PET. Over time, CSF+/PET− group had widespread increase of tracer uptake compared to CSF−/PET− irrespective of the reference region. Additionally, CSF+/PET− had slightly more tracer uptake at baseline than CSF−/PET−. These findings were consistent when covarying for APOE ɛ4 status (data available from Dryad, figure 5, doi.org/10.5061/dryad.c59zw3r49).
Figure 1. Accumulation of β-amyloid measured by [18F]florbetapir PET.
Results obtained from linear mixed models, with the colors indicating β-coefficients relative to the CSF−/PET− group. The 3 sections show the difference between the group of interest (CSF+/PET−, CSF−/PET+, or CSF+/PET+) and CSF−/PET−. The first column shows the β-coefficient for the baseline effect of the CSF/PET group when using whole cerebellum as the reference region. The second and third columns show the β-coefficients for the interaction between CSF/PET group and time as the longitudinal change when using whole cerebellum or composite white matter as the reference, respectively. Only regions with p < 0.05 are shown. Image was created using the ggseg package in R.
Longitudinal trajectories of tau and cognition
Next, we investigated longitudinal trajectories of tau pathology (CSF and PET) and cognition (figure 2; data available from Dryad, table 4, doi.org/10.5061/dryad.c59zw3r49). Compared to the Aβ CSF+/PET+ group, participants with discordant CSF/PET Aβ status at baseline had significantly lower levels of CSF t-tau and p-tau measures (both p < 0.001) and better cognitive test scores (MMSE: p = 0.001 for CSF+/PET−, p = 0.201 for CSF−/PET+; memory: both p < 0.001; executive functioning: p = 0.010 for CSF+/PET−, p < 0.001 for CSF−/PET+). Longitudinally, participants in both CSF/PET groups showed slower decline in cognitive test scores (all p < 0.001 for both), compared to the CSF+/PET+ group. [18F]Flortaucipir PET was first performed 5 years after baseline. Participants in both discordant CSF/PET groups had less [18F]flortaucipir uptake in entorhinal cortex (both p < 0.001), temporal meta-ROI (p < 0.001 for CSF+/PET−, p = 0.006 for CSF−/PET+), and Braak V/VI (p = 0.002 for CSF+/PET−, p = 0.274 for CSF−/PET+) compared to CSF+/PET+. Longitudinally, discordant CSF/PET groups had lower rates of increase in [18F]flortaucipir uptake in temporal meta-ROI (p = 0.010 for CSF+/PET−, p = 0.031 for CSF−/PET+) and Braak V/VI composite areas (p = 0.022 for CSF+/PET−). CSF+/PET− participants additionally had at baseline worse executive functioning than participants in the CSF−/PET− group (p = 0.034) group. The CSF/PET discordant groups were otherwise similar to CSF−/PET−. These findings were consistent when drawing random samples from the CSF+/PET+ group in order to achieve a 50/50 CN/MCI ratio in the CSF+/PET+ group and when covarying for APOE ɛ4 status (data available from Dryad, tables 5 and 6, respectively, doi.org/10.5061/dryad.c59zw3r49).
Figure 2. Longitudinal trajectories of tau pathology and cognition.
Results obtained from linear mixed models investigating the effect of β-amyloid CSF/PET discordance on (A) tau pathology assessed by CSF total tau (t-tau) and phosphorylated tau (p-tau), (B) tau pathology based on regional [18F]flortaucipir PET, and (C) cognitive trajectories measured by Mini-Mental State Examination (MMSE), Alzheimer's Disease Neuroimaging Initiative memory, and executive composite scores. CSF tau was assessed from baseline to median 2.0 years; [18F]flortaucipir PET was first performed a median of 5.2 years after baseline and was followed up a median of 1.3 years later; cognitive tests were assessed at baseline, and followed up for a median of 4.2 years. Difference from CSF+/PET+ is illustrated by black triangles (for CSF+/PET−) or circles (for CSF−/PET+) with the number of symbols indicating statistical difference (1: p < 0.05; 2: p < 0.01; 3: p < 0.001). Symbols on the left side of a plot show difference in intercept (main effect of CSF/PET group in the model), and symbols on the right side show a difference in slope (interaction between CSF/PET group and time). CSF+/PET− participants also had at baseline worse executive functioning than participants in the CSF−/PET− group (p = 0.034). Image was created using the ggeffects package in R. ROI = region of interest.
Clinical progression
Next, we investigated the association between Aβ CSF/PET status and clinical progression using Kaplan-Meier estimates and Cox regression analyses (figure 3; data available from Dryad, table 7, doi.org/10.5061/dryad.c59zw3r49). Progression from MCI to dementia occurred less often in Aβ CSF+/PET− (7%, HR 0.10 [0.03, 0.32], p < 0.001) and CSF−/PET− (8%, HR 0.11 [0.06, 0.20], p < 0.001) participants, compared to the CSF+/PET+ (48%) group. Similarly, in CN participants, clinical progression to MCI or dementia occurred most often in CSF+/PET+ (30%), compared to CSF−/PET− (12%, HR 0.33 [0.18, 0.62], p < 0.001), CSF−/PET+ (15%, HR 0.42 [0.10, 1.77], p = 0.236), or CSF+/PET− (21%, HR 0.55 [0.24, 1.22], p = 0.141). No participants with Aβ CSF−/PET+ progressed to dementia.
Figure 3. Kaplan-Meier curves for clinical progression.
Results obtained from the Kaplan-Meier estimate investigating the association between β-amyloid CSF/PET profile and clinical progression for cognitively normal (CN) participants (progression to MCI or dementia; A) or participants with mild cognitive impairment (MCI) (progression to dementia; B). Tables below the figures report the number of participants with available follow-up data per year.
Replication involving only participants with available [18F]flortaucipir PET
We repeated the previous analyses involving only the 253 participants with available [18F]flortaucipir PET (data available from Dryad, tables 8–10, doi.org/10.5061/dryad.c59zw3r49). The effects of Aβ CSF/PET groups on regional [18F]florbetapir uptake (figure 6 and table 11 from Dryad, doi.org/10.5061/dryad.c59zw3r49), trajectories of CSF tau and cognition (figure 7 and table 12 from Dryad, doi.org/10.5061/dryad.c59zw3r49), and clinical progression (figure 8 and table 13 from Dryad, doi.org/10.5061/dryad.c59zw3r49) were consistent with the aforementioned findings in the full sample.
Associations between Aβ and tau in CSF+/PET− participants
We then assessed whether continuous [18F]florbetapir uptake in the subthreshold range is correlated with tau measures in the Aβ CSF+/PET− group (figure 4). [18F]florbetapir tracer uptake globally and in early accumulating regions was associated with higher baseline CSF t-tau (p = 0.001 and p = 0.003) and higher [18F]flortaucipir uptake in entorhinal cortex (p = 0.003 and p = 0.010) and marginally in the temporal meta-ROI (p = 0.062 and p = 0.091).
Figure 4. Correlation between baseline [18F]florbetapir PET and tau pathology based on CSF and PET.
Plotted is the association between [18F]florbetapir PET, based on (A) total composite and (B) early accumulating regions composite on the x axis, and cross-sectional tau pathology, measured by either CSF total tau (t-tau) or phosphorylated tau (p-tau) at baseline or [18F]flortaucipir PET a median of 5.2 years after baseline on the y axis. R2 and p values are reported from the linear regression models, which were also adjusted for the times between baseline [18F]florbetapir PET and the outcome modality. ROI = region of interest.
Accumulation of Aβ and tau in CSF+/PET− participants
Finally, we investigated whether CSF+/PET− participants progress to CSF+/PET+ or become tau-positive first. Based on the last available [18F]florbetapir Aβ PET scan and CSF Aβ42 analysis, 21/64 (33%) of the baseline Aβ CSF+/PET− participants progressed to CSF+/PET+. Of 34 CSF+/PET− participants with [18F]flortaucipir PET available, 11/34 (32% [95% CI 17%, 48%]) progressed to CSF+/PET+, but only 1 (3% [95% CI −3%, 9%], difference in proportions p < 0.05) turned tau-positive based on entorhinal or temporal meta-ROI regions, and none in Braak V/VI. For comparison, 2/123 (2%, p = 1.00) of Aβ CSF−/PET−, 0/16 (0%, p = 1.00) CSF−/PET+, and 47/80 CSF+/PET+ (59%, p < 0.001) were tau-positive based on last available [18F]flortaucipir PET.
Discussion
We investigated the association between discordant CSF/PET Aβ biomarkers on tau pathology and clinical progression. Our main finding was that although Aβ CSF+/PET− participants showed longitudinal accumulation of Aβ based on PET, they had significantly less tau pathology based on both CSF at baseline and [18F]flortaucipir 5 years later compared to participants with CSF+/PET + Aβ status. Similarly, discordant Aβ status was associated with better cognitive outcome and a lower risk of clinical progression than CSF+/PET+. We also showed that during follow-up, CSF+/PET− participants frequently progressed to Aβ CSF+/PET+, whereas only one participant reached the threshold of tau positivity based on [18F]flortaucipir PET. Finally, we showed a correlation between tau measures and global Aβ PET tracer uptake, indicating possible subthreshold accumulation of AD pathology in CSF+/PET− participants. Taken together, our findings suggest that CSF+/PET− Aβ status is associated with a distinctly better prognosis than CSF+/PET+, and that a sufficient Aβ load detectable by both CSF and PET seems to precede significant tau deposition.
Using both CSF tau measures and [18F]flortaucipir PET, we found that participants with discordant CSF/PET Aβ status had less tau pathology than CSF+/PET+ Aβ participants, and comparable tau load as observed in concordant Aβ-negative participants. It has been proposed that CSF+/PET− status can be caused by CSF Aβ42 being able to detect Aβ at an earlier stage due to the decrease of soluble Aβ42 in CSF preceding fibrillary depositions visualized by PET. This is supported by higher rates of CSF+/PET− compared to CSF−/PET+ across several studies.7,37,38 Previous longitudinal PET studies have shown that participants with CSF+/PET− Aβ status show significant accumulation of Aβ over time.8,9,39 We replicated this finding in our study, further supporting the notion that CSF+/PET− Aβ status identifies the beginnings of Aβ accumulation. Although participants with CSF−/PET+ Aβ status had higher [18F]florbetapir tracer uptake at baseline, they did not show significant accumulation of Aβ over time. Combined with the lack of clinical progression in this group, these observations suggest that isolated Aβ PET positivity might be caused by nonspecific tracer uptake in the white matter, processing errors, or other unknown factors.6 In CSF+/PET− participants, the lack of substantial tau pathology based on CSF tau measures at baseline and on [18F]flortaucipir PET 5 years later, accompanied by lack of cognitive decline and clinical progression, suggests these participants have a distinctly more favorable prognosis than CSF+/PET+ participants. This is likely caused by the remarkably slow course of AD, which is characterized by gradual accumulation of pathology over time.40,41 Accounting for the more benign prognosis of CSF+/PET− participants is important for the timing of future interventions at the earliest stages of AD pathology.
Current hypothetical biomarker models suggest that accumulation of Aβ pathology is followed by detectable cortical tau pathology, subsequently leading to neurodegeneration and cognitive decline.42,43 Although it has been proposed that CSF+/PET− is followed by conversion to CSF+/PET+,8,44 the exact timing of CSF+/PET− status in regard to that timeline, in particular towards accumulation of tau, is unknown. We found that within 5 years, one-third of the CSF+/PET− participants progressed to CSF+/PET+, whereas at that time only one participant exhibited suprathreshold early to intermediate stage tau pathology based on [18F]flortaucipir PET and none showed widespread neocortical uptake (i.e., Braak stage V/VI regions). This finding has at least 2 implications. First, as the majority of CSF+/PET− participants did not progress to CSF+/PET+ within 5 years, this indicates that in the majority of cases the CSF+/PET− Aβ status lasts for several years. Second, accumulation of sufficient Aβ detectable by both CSF and PET seems to precede significant accumulation of tau pathology.45,46 However, we also found a correlation between baseline regional Aβ PET and tau pathology in the CSF+/PET− group, suggesting that there already might be interaction present between Aβ and tau. This supports previous work emphasizing the importance of considering subthreshold accumulation of pathology to better understand disease mechanisms of early preclinical stages of AD.47–49
Our study has some limitations. Although ADNI is one of the largest cohorts with both available Aβ PET and CSF analysis, only a relatively small number of participants with discordant CSF/PET Aβ status were available. Second, our main outcome measures of tau pathology based on CSF and PET were assessed at different time points. Although that reduces the direct comparability of these findings, they also complement each other and allow us to measure tau pathology both at baseline and several years later. Relatively short follow-up periods were available for both CSF tau measures and [18F]flortaucipir PET. Therefore, it is possible that with longer follow-up periods, participants with discordant Aβ status might show diverging trajectories compared to the CSF−/PET− group. Our interpretation of the study could also be affected by the possibility that CSF+/PET− status might reflect a different subtype of AD, although no evidence for that exists. Finally, cutoffs of biomarkers as well as defining Aβ PET status based on global SUVR are important considerations when evaluating these results. As suboptimal cutoffs might result in misclassification,50 we used applied widely used and validated cutoffs for both PET and CSF.
Our findings indicate that a sufficient Aβ load detectable by both PET and CSF seems to precede substantial tau deposition. Participants with CSF+/PET− Aβ profile are at a significantly earlier clinical and biological disease stage than those with CSF+/PET+, and have a distinctly better prognosis for at least 5 years.
Acknowledgment
J.R. thanks Sergei Nazarenko, the International Atomic Energy Agency, and the North Estonia Medical Centre for their contribution to his professional development. The authors thank Nicholas Cullen for support in statistical analysis.
Glossary
- Aβ
β-amyloid
- AD
Alzheimer disease
- ADNI
Alzheimer's Disease Neuroimaging Initiative
- CI
confidence interval
- CN
cognitively normal
- HR
hazard ratio
- IQR
interquartile range
- MCI
mild cognitive impairment
- MMSE
Mini-Mental State Examination
- p-tau
phosphorylated tau
- ROI
region of interest
- SUVR
standardized uptake value ratio
- t-tau
total tau
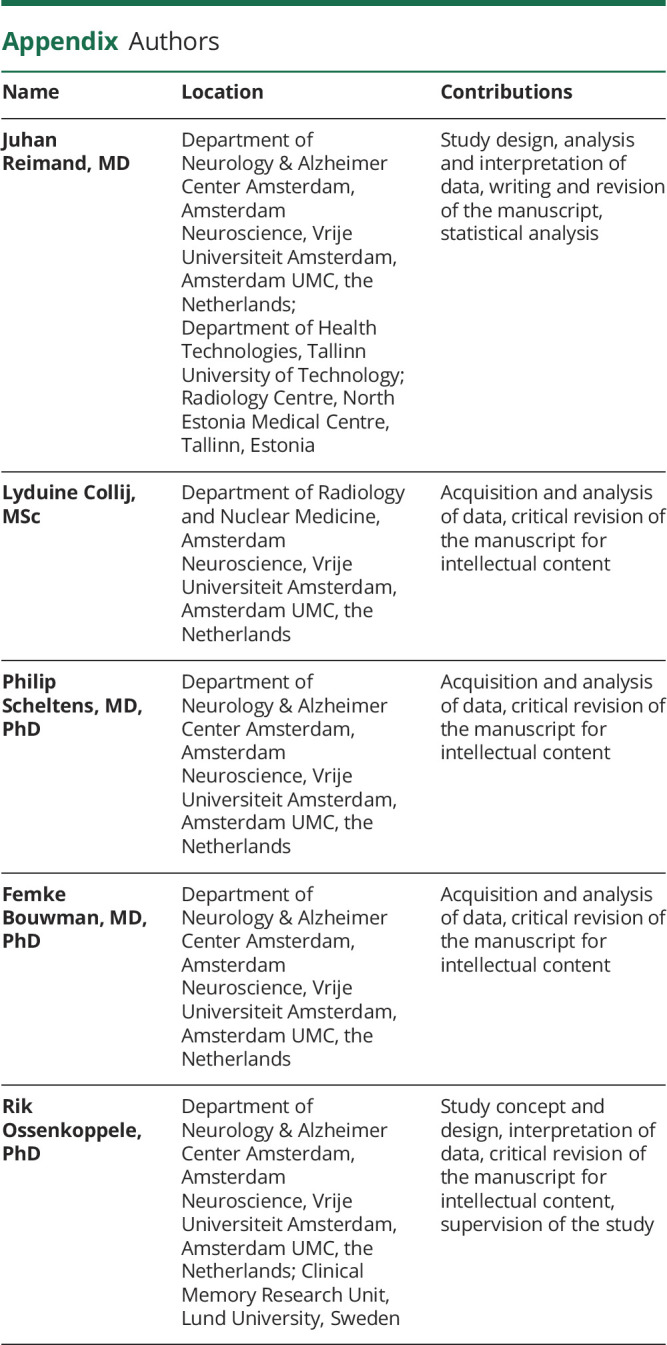
Appendix. Authors
Sutdy funding
Data collection and sharing for this project was funded by the Alzheimer's Disease Neuroimaging Initiative (ADNI) (NIH grant U01 AG024904) and Department of Defense ADNI (Department of Defense award number W81XWH-12-2-0012). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through contributions from the following: AbbVie, Alzheimer's Association, Alzheimer's Drug Discovery Foundation, Araclon Biotech, BioClinica, Inc., Biogen, Bristol-Myers Squibb Company, CereSpir, Inc., Cogstate, Eisai Inc., Elan Pharmaceuticals, Inc., Eli Lilly and Company, EuroImmun, F. Hoffmann-La Roche Ltd and its affiliated company Genentech, Inc., Fujirebio, GE Healthcare, IXICO Ltd., Janssen Alzheimer Immunotherapy Research & Development, LLC, Johnson & Johnson Pharmaceutical Research & Development LLC, Lumosity, Lundbeck, Merck & Co., Inc., Meso Scale Diagnostics, LLC, NeuroRx Research, Neurotrack Technologies, Novartis Pharmaceuticals Corporation, Pfizer Inc., Piramal Imaging, Servier, Takeda Pharmaceutical Company, and Transition Therapeutics. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the NIH (fnih.org). The grantee organization is the Northern California Institute for Research and Education and the study is coordinated by the Alzheimer's Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California. The Alzheimer Center Amsterdam is supported by Alzheimer Nederland and Stichting VUmc fonds. Research performed at the Alzheimer Center Amsterdam is part of the neurodegeneration research program of Amsterdam Neuroscience. The funding sources were not involved in the writing of this article or in the decision to submit it for publication.
Disclosure
J. Reimand and L. Collij report no disclosures relevant to the manuscript. P. Scheltens has received consultancy/speaker fees (paid to the institution) from Biogen, People Bio, Roche (Diagnostics), and Novartis Cardiology and is PI of studies with Vivoryon, EIP Pharma, IONIS, CogRx, AC Immune, and Toyama; the funding sources were not involved in the writing of this article or in the decision to submit it for publication. F. Bouwman and R. Ossenkoppele report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.Braak H, Braak E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol 1991;82:239–259. [DOI] [PubMed] [Google Scholar]
- 2.Jack CR, Bennett DA, Blennow K, et al. NIA-AA Research Framework: toward a biological definition of Alzheimer's disease. Alzheimers Dement 2018;14:535–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging–Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011;7:270–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging–Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011;7:263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zwan M, van Harten A, Ossenkoppele R, et al. Concordance between cerebrospinal fluid biomarkers and [11C]PIB PET in a memory clinic cohort. J Alzheimers Dis 2014;41:801–807. [DOI] [PubMed] [Google Scholar]
- 6.Mattsson N, Insel PS, Donohue M, et al. Independent information from cerebrospinal fluid amyloid-β and florbetapir imaging in Alzheimer's disease. Brain 2015;138:772–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Wilde A, Reimand J, Teunissen CE, et al. Discordant amyloid-β PET and CSF biomarkers and its clinical consequences. Alzheimers Res Ther 2019;11:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Palmqvist S, Mattsson N, Hansson O. Cerebrospinal fluid analysis detects cerebral amyloid-β accumulation earlier than positron emission tomography. Brain 2016;139:1226–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Palmqvist S, Schöll M, Strandberg O, et al. Earliest accumulation of β-amyloid occurs within the default-mode network and concurrently affects brain connectivity. Nat Commun 2017;8:1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blennow K, Wallin A, Ågren H, Spenger C, Siegfried J, Vanmechelen E. Tau protein in cerebrospinal fluid. Mol Chem Neuropathol 1995;26:231–245. [DOI] [PubMed] [Google Scholar]
- 11.Chien DT, Bahri S, Szardenings AK, et al. Early clinical PET imaging results with the novel PHF-tau radioligand [F-18]-T807. J Alzheimers Dis 2013;34:457–468. [DOI] [PubMed] [Google Scholar]
- 12.Lowe VJ, Wiste HJ, Senjem ML, et al. Widespread brain tau and its association with ageing, Braak stage and Alzheimer's dementia. Brain 2018;141:271–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ossenkoppele R, Schonhaut DR, Schöll M, et al. Tau PET patterns mirror clinical and neuroanatomical variability in Alzheimer's disease. Brain 2016;139:1551–1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bejanin A, Schonhaut DR, La Joie R, et al. Tau pathology and neurodegeneration contribute to cognitive impairment in Alzheimer's disease. Brain 2017;140:3286–3300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hardy J, Bogdanovic N, Winblad B, et al. Pathways to Alzheimer's disease. J Intern Med 2014;275:296–303. [DOI] [PubMed] [Google Scholar]
- 16.Petersen RC, Aisen PS, Beckett LA, et al. Alzheimer's Disease Neuroimaging Initiative (ADNI): clinical characterization. Neurology 2010;74:201–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crane PK, Carle A, Gibbons LE, et al. Development and assessment of a composite score for memory in the Alzheimer's Disease Neuroimaging Initiative (ADNI). Brain Imaging Behav 2012;6:502–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gibbons LE, Carle AC, Mackin RS, et al. A composite score for executive functioning, validated in Alzheimer's Disease Neuroimaging Initiative (ADNI) participants with baseline mild cognitive impairment. Brain Imaging Behav 2012;6:517–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Landau S, Jagust W. Florbetapir processing methods. Los Angeles: Alzheimer’s Disease Neuroimaging Institute; 2015. [Google Scholar]
- 20.Jagust WJ, Landau SM, Koeppe RA, et al. The Alzheimer's Disease Neuroimaging Initiative 2 PET Core: 2015. Alzheimers Dement 2015;11:757–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Landau SM, Breault C, Joshi AD, et al. Amyloid-β imaging with Pittsburgh compound B and florbetapir: comparing radiotracers and quantification methods. J Nucl Med 2013;54:70–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clark CM, Pontecorvo MJ, Beach TG, et al. Cerebral PET with florbetapir compared with neuropathology at autopsy for detection of neuritic amyloid-β plaques: a prospective cohort study. Lancet Neurol 2012;11:669–678. [DOI] [PubMed] [Google Scholar]
- 23.Joshi AD, Pontecorvo MJ, Clark CM, et al. Performance characteristics of amyloid PET with florbetapir F 18 in patients with Alzheimer's disease and cognitively normal subjects. J Nucl Med 2012;53:378–384. [DOI] [PubMed] [Google Scholar]
- 24.Landau SM, Fero A, Baker SL, et al. Measurement of longitudinal β-amyloid change with 18F-florbetapir PET and standardized uptake value ratios. J Nucl Med 2015;56:567–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mattsson N, Palmqvist S, Stomrud E, Vogel J, Hansson O. Staging β-amyloid pathology with amyloid positron emission tomography. JAMA Neurol 2019;76:1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shaw LM, Vanderstichele H, Knapik-Czajka M, et al. Cerebrospinal fluid biomarker signature in Alzheimer’s Disease Neuroimaging Initiative subjects. Ann Neurol 2009;65:403–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shaw LM, Vanderstichele H, Knapik-Czajka M, et al. Qualification of the analytical and clinical performance of CSF biomarker analyses in ADNI. Acta Neuropathol 2011;121:597–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Landau S, Jagust W. Flortaucipir (AV-1451) processing methods. Los Angeles: Alzheimer’s Disease Neuroimaging Institute; 2016. [Google Scholar]
- 29.Jack CR, Wiste HJ, Weigand SD, et al. Defining imaging biomarker cut points for brain aging and Alzheimer's disease. Alzheimers Dement 2017;13:205–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schöll M, Lockhart SN, Schonhaut DR, et al. PET imaging of tau deposition in the aging human brain. Neuron 2016;89:971–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson KA, Schultz A, Betensky RA, et al. Tau positron emission tomographic imaging in aging and early Alzheimer disease. Ann Neurol 2016;79:110–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ossenkoppele R, Palmqvist S, Mattsson N, Janelidze S, Santillo A, Ohlsson T. Discriminative accuracy of [18F]flortaucipir positron emission tomography for Alzheimer disease vs other neurodegenerative disorders. JAMA 2018;320:1151–1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.R Core Team. R: A Language and Environment for Statistical Computing. 2018. Available at: R-project.org/. Accessed July 1, 2019. [Google Scholar]
- 34.Bates D, Mächler M, Bolker BM, Walker SC. Fitting linear mixed-effects models using lme4. J Stat Softw 2015;67:1–48. [Google Scholar]
- 35.Mowinckel A, Pineiro DV. Ggseg Package for R. 2018. Available at: github.com/LCBC-UiO/ggseg. Accessed December 14, 2019. [Google Scholar]
- 36.Lüdecke D. ggeffects: Tidy data frames of marginal effects from regression models. J Open Source Softw 2019;76:1319. [Google Scholar]
- 37.Fagan AM, Mintun MA, Shah AR, et al. Cerebrospinal fluid tau and ptau181 increase with cortical amyloid deposition in cognitively normal individuals: implications for future clinical trials of Alzheimer's disease. EMBO Mol Med 2009;1:371–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blennow K, Mattsson N, Schöll M, Hansson O, Zetterberg H. Amyloid biomarkers in Alzheimer's disease. Trends Pharmacol Sci 2015;36:297–309. [DOI] [PubMed] [Google Scholar]
- 39.Vlassenko AG, McCue L, Jasielec MS, et al. Imaging and cerebrospinal fluid biomarkers in early preclinical Alzheimer disease. Ann Neurol 2016;80:379–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Villemagne VL, Burnham S, Bourgeat P, et al. Amyloid β deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer's disease: a prospective cohort study. Lancet Neurol 2013;12:357–367. [DOI] [PubMed] [Google Scholar]
- 41.Jack CR, Wiste HJ, Schwarz CG, et al. Longitudinal tau PET in ageing and Alzheimer's disease. Brain 2018;141:1517–1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jack C. Hypothetical pathological cascade in Alzheimer’s disease. Lancet 2010;9:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jack CR, Holtzman DM. Biomarker modeling of Alzheimer’s disease. Neuron 2013;80:1347–1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reimand J, de Wilde A, Teunissen CE, et al. PET and CSF amyloid-β status are differently predicted by patient features: information from discordant cases. Alzheimers Res Ther 2019;11:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mattsson-Carlgren N, Andersson E, Janelidze S, et al. Aβ deposition is associated with increases in soluble and phosphorylated tau that precede a positive Tau PET in Alzheimer's disease. Sci Adv 2020;6:eaaz2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jack CR, Wiste HJ, Botha H, et al. The bivariate distribution of amyloid-β and tau: relationship with established neurocognitive clinical syndromes. Brain 2019;142:3230–3242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Leal SL, Lockhart SN, Maass A, Bell RK, Jagust WJ. Subthreshold amyloid predicts tau deposition in aging. J Neurosci 2018;38:4482–4489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Landau SM, Horng A, Jagust WJ. Memory decline accompanies subthreshold amyloid accumulation. Neurology 2018;90:E1452–E1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Insel PS, Ossenkoppele R, Gessert D, et al. Time to amyloid positivity and preclinical changes in brain metabolism, atrophy, and cognition: evidence for emerging amyloid pathology in Alzheimer’s disease. Front Neurosci 2017;11:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McRae-McKee K, Udeh-Momoh CT, Price G, et al. Perspective: clinical relevance of the dichotomous classification of Alzheimer's disease biomarkers: should there be a “gray zone”? Alzheimers Dement 2019;15:1348–1356. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All imaging, demographic, and neuropsychological data used in this article are publicly available and were downloaded from the ADNI website (adni.loni.usc.edu). Upon request, we will provide a list of ADNI participant identifications for replication purposes.







