Background:
Although multiple prospective comparative studies exist for adults with midshaft clavicle fractures, few comparative studies exist in older children and adolescents. This study compares intermediate-term functional, pain, radiographic, and complication outcomes in children and adolescents with midshaft clavicle fractures treated operatively or nonoperatively.
Methods:
Children and adolescents who were 10 to 18 years of age with midshaft clavicle fractures treated from 2006 to 2017 were identified through electronic picture archiving and communication system (PACS) radiographic and chart review. Closed injuries with a minimum of 1 year from the time of the injury were included. Patients completed patient-reported outcome measures and a focused questionnaire. The primary outcome was the abbreviated Disabilities of the Arm, Shoulder and Hand Questionnaire (QuickDASH) score; the secondary outcomes included the University of California Los Angeles (UCLA) Activity Scale, Patient-Reported Outcomes Measurement Information System (PROMIS) Pain Interference (PI) and PROMIS Physical Function (PF) Upper Extremity (UE), Hospital for Special Surgery Pediatric Functional Activity Brief Scale (HSS Pedi-FABS), Numeric Rating Scale (NRS) for Pain, and rates of implant removal, nonunion, and refracture. Univariate comparisons between the operatively treated group and the nonoperatively treated group were performed.
Results:
In this study, 302 patients were identified; of these, 79 patients (43 operatively treated and 36 nonoperatively treated) or their parent or legal guardian consented and the patients completed the study protocol. The mean age (and standard deviation) at the time of the injury was 16.0 ± 1.7 years for the operatively treated group and 13.5 ± 1.8 years for the nonoperatively treated group (p < 0.001). The median follow-up was 3.8 years. The patient-reported outcome scores were similar (p > 0.05 for all comparisons) between the operatively treated group and the nonoperatively treated group, even for patients at or near skeletal maturity and those with shortening of ≥15 mm or ≥100% translation. There were no nonunions. The refracture rate was 5% (2 of 43) for the operatively treated group and 3% (1 of 36) for the nonoperatively treated group (p = 1.00). There were 19% (8 of 43) who underwent implant removal. Responders were similar to nonresponders, other than female patients (p < 0.001) and surgically treated patients (p = 0.049) being more likely to respond.
Conclusions:
In the subset of this cohort who responded and completed the study, both operatively and nonoperatively treated patients had excellent functional and pain outcomes, similar refracture rates, and no nonunions. Even in widely displaced and translated fractures, and in those at or near skeletal maturity, outcomes were similar. Operative management should potentially be reserved for special circumstances. A prospective comparative study of older adolescents (female patients who are 14 to 18 years of age and male patients who are 16 to 20 years of age) with displaced midshaft clavicle fractures is warranted.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
The incidence of clavicle fractures in children is 13 to 19 fractures per 10,000 children1, with 90% of clavicle fractures occurring in the midshaft2,3. Traditionally, even displaced midshaft clavicle fractures in children and adolescents were not treated operatively because of documented excellent remodeling potential of the clavicle4. Although surgical treatment gained popularity for displaced fractures in adults after improved functional outcomes and lower nonunion rates were reported in a randomized trial5, few comparative studies exist in older children and adolescents, resulting in widespread controversy in the management of midshaft clavicle fractures in this population.
A survey of the Pediatric Orthopaedic Society of North America (POSNA) members demonstrated greater support for operative fixation in older adolescents and in severe fracture patterns. Adult literature was the greatest factor influencing treatment preference6. Over 90% of POSNA members were in favor of nonoperative treatment for nondisplaced midshaft clavicle fractures, but there was notable disagreement about the need for operative fixation of segmental fractures in adolescents6.
Recent meta-analyses identified a nonunion rate in patients <19 years of age of <1% to 2% for nonoperative management and <1% to 3% for operative management7,8. Gao et al. reported faster union, earlier return to sports, a higher Constant score, higher rates of complication, and a high rate of secondary surgical procedures with operative management7. In contrast, Nawar et al. reported no difference in time to union, return to activity, or complications between operative and nonoperative management8. Both meta-analyses concluded that excellent outcomes followed both operative and nonoperative management. The original studies contributing to these meta-analyses were limited by notably small series or lack of sufficient patient-reported outcomes to fully compare functional and pain outcomes between groups1,9-21.
The primary aim of this study was to determine if intermediate-term functional outcomes were improved with operative treatment compared with nonoperative treatment, measured by the abbreviated Disabilities of the Arm, Shoulder and Hand Questionnaire (QuickDASH) score. The secondary aims included comparison of union, implant removal, and refracture rates, as well as additional functional outcomes measured by the University of California Los Angeles (UCLA) Activity Scale, Patient-Reported Outcomes Measurement Information System (PROMIS) Physical Function (PF) Upper Extremity (UE), and Hospital for Special Surgery Pediatric Functional Activity Brief Scale (HSS Pedi-FABS) scores, and pain measured by the PROMIS Pain Interference (PI) score and by the Numeric Rating Scale (NRS) for Pain score. It was hypothesized that scores would be similar for patient-reported outcome measures (PROMs) between operative and nonoperative groups.
Materials and Methods
Patients who were 10 to 18 years of age at the time of a closed midshaft clavicle fracture treated between 2006 and 2017 with a minimum 1-year follow-up were identified through billing records and a picture archiving and communication system (PACS) radiographic search. Patients were treated at the Hospital for Special Surgery (HSS) and/or New York Presbyterian (NYP)-Weill Cornell Medical Center. Through chart reviews, demographic, radiographic, and treatment data were extracted, and patients were identified as having been treated operatively with plate fixation or having been treated nonoperatively with a sling. Fracture classification, translation, and shortening were measured by 2 senior orthopaedic surgery residents and were confirmed by a board-certified pediatric orthopaedic surgeon. Fracture shortening was measured from cortex to cortex22. Study introduction was by mail and email. This was followed by a telephone contact to discuss study details and obtain oral informed consent. A minimum of 5 attempts were made to contact patients before considering them lost to follow-up.
Consent was obtained from the patients or their parent or legal guardian as appropriate. PROMs, including QuickDASH, UCLA Activity Scale, PROMIS PI and PROMIS PF UE scores, HSS Pedi-FABS, and NRS for Pain, were administered by an email link to the Outcomes Based Electronic Research Database (OBERD) website, whereby forms could be completed electronically. A brief questionnaire given by telephone surveyed complications relating to their management, including the requirement for an additional surgical procedure or treatment for nonunion, refracture, or a symptomatic implant.
The primary outcome was the QuickDASH score21, and secondary outcomes included the UCLA Activity Scale, PROMIS PI, PROMIS PF UE physical function, HSS Pedi-FABS, NRS Pain scores, and nonunion, implant removal, and refracture rates. The QuickDASH is scaled from 0 to 100 points, with a higher score indicating greater disability23. The normative value for the QuickDASH in adults who were 20 to 29 years of age has been reported at 5 for men and women24. The UCLA Activity Scale ranges from 1 to 10, with a higher score reflecting greater sports participation25. The HSS Pedi-FABS is an 8-item construct that evaluates the frequency of activity (“less than 1 time per month” to “more than 4 times per week”)26. Normative data have revealed a mean score (and standard deviation) of 15.4 ± 8.5 points and the maximum is 30 points27. PROMIS CATs (Computer Adaptive Tests) were used to minimize question fatigue. The PROMIS PI assesses the impact of pain on daily living over the past 7 days28. The measure is on a scale of 0 to 100 points (normative mean, 50 ± 10 points), with higher scores indicating greater pain interference29. The PROMIS PF UE evaluates activities requiring the use of an upper extremity (shoulder, arm, or hand)30. The PROMIS PF UE is also on a scale of 0 to 100 points (normative mean, 50 ± 10 points), in which higher scores indicate better function31. The NRS for Pain records pain ratings corresponding to a patient’s best (lowest) pain and worst pain level over the past 24 hours, scored from 0 (no pain) to 10 (worst pain imaginable)32,33.
Statistical Analysis
Descriptive statistics were calculated for sex, laterality of injury, radiographic shortening, translation (percentage of midshaft bone diameter), age at the time of the injury, and age at the time of the telephone follow-up. The Mann-Whitney U test was used to compare time from the injury to follow-up and PROM scores (QuickDASH, NRS for Pain, HSS Pedi-FABS, UCLA, PROMIS PI, PROMIS PF UE). Univariate comparisons between the operatively treated group and the nonoperatively treated group were performed using a t test for normally distributed continuous variables, Mann-Whitney U test for non-normally distributed continuous variables, and Fisher exact test for categorical variables. Demographic characteristics and limited outcomes of nonresponders were compared with study participants. All analyses were conducted using Python 2.7 (Python Software Foundation). This study was powered using expected QuickDASH scores for operative and nonoperative treatment informed by the Canadian Orthopaedic Trauma Society (COTS) study5. An effect size of 10 points was considered significant34. Sample-size analysis determined that 9 patients were required per group for 80% power and significance of 0.05.
Results
Patient Demographic Characteristics
In this study, 302 patients met inclusion criteria, we obtained consent from 120 patients (40%) or their parents or guardians, and 79 patients (26%) completed PROMs and questionnaires. Of the 302 patients, 9% (28 patients) declined participation and 51% (154 patients) were lost to follow-up. Based on chart and radiographic review alone for the nonresponders, the nonresponders were of similar age, and refracture and implant removal rates were similar compared with study participants. Female patients were more likely to participate than male patients (35% female participants compared with 16% female nonresponders; p < 0.001), as were those treated surgically (54% of participants were treated operatively compared with 41% of nonresponders treated operatively; p = 0.049).
The majority of patients were male and left-sided fractures were more common (Table I). The mean age at the time of the injury was 14.9 ± 2.1 years. Patients in the operative group were older than in the nonoperative group (mean age, 16.0 compared with 13.5 years; p < 0.001). The median time to follow-up for all patients was 3.8 years (range, 1.0 to 10.1 years). The mean age at the time of follow-up was 19.3 ± 3.4 years: 20.7 ± 3.3 years for the operatively treated group and 17.6 ± 2.7 years for the nonoperatively treated group. Forty-one (95%) of 43 operatively treated patients were treated by an adult orthopaedic surgeon, and 30 (83%) of 36 nonoperatively treated patients were treated by a pediatric orthopaedic surgeon.
TABLE I.
Patient Demographic Characteristics and Time to Follow-up
| All Patients | Nonoperatively Treated Group | Operatively Treated Group | P Value | |
| Female sex | 35% | 39% | 33% | 0.639 |
| Left laterality | 57% | 58% | 56% | 1.000 |
| Age at injury* (yr) | 14.9 ± 2.1 | 13.5 ± 1.8 | 16.0 ± 1.7 | <0.001 |
| Follow-up† (yr) | 3.8 (1.0 to 10.1) | 3.5 (1.4 to 10.1) | 4.2 (1.0 to 9.9) | 0.440 |
| Age at follow-up* (yr) | 19.3 ± 3.4 | 17.6 ± 2.7 | 20.7 ± 3.3 | <0.001 |
The values are given as the mean and the standard deviation.
The values are given as the median, with the range in parentheses.
Radiographic Comparison
The complete radiographic data for 63 patients are presented in Table II.
TABLE II.
Radiographic Shortening and Translation
| All Patients | Nonoperatively Treated Group | Operatively Treated Group | P Value | |
| Shortening | 0.057 | |||
| <15 mm | 50 (79%) | 32 (89%) | 18 (67%) | |
| ≥15 mm | 13 (21%) | 4 (11%) | 9 (33%) | |
| Translation | 0.005 | |||
| <100% | 27 (43%) | 21 (58%) | 6 (22%) | |
| ≥100% | 36 (57%) | 15 (42%) | 21 (78%) |
Union, Refracture, and Implant Removal
There were no nonunions in either group. There were 1 ipsilateral refracture in the nonoperatively treated group (3%) and 2 ipsilateral refractures in the operatively treated group (5%) (p = 1.00). Eight patients (19%) treated operatively underwent removal of the implant during the study period.
Patient-Reported Outcomes
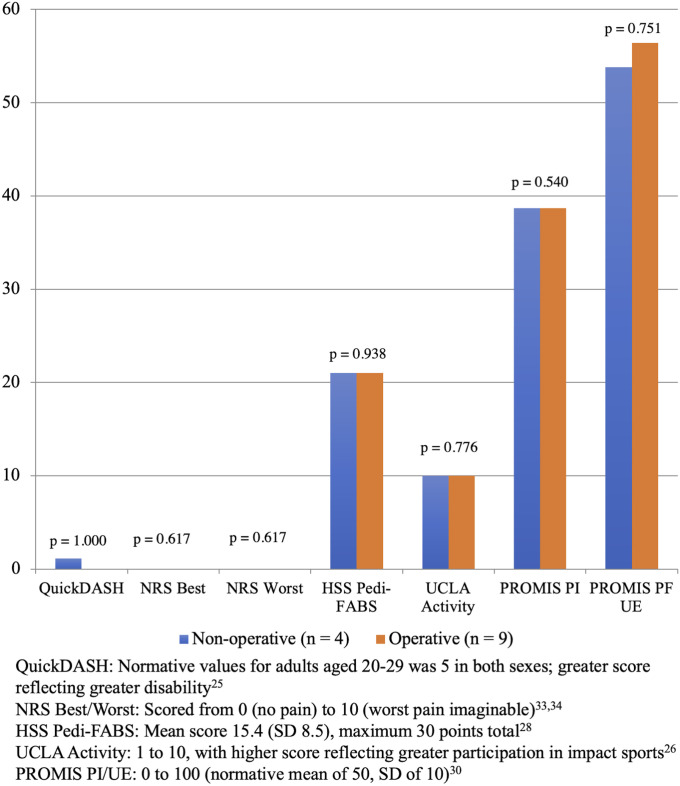
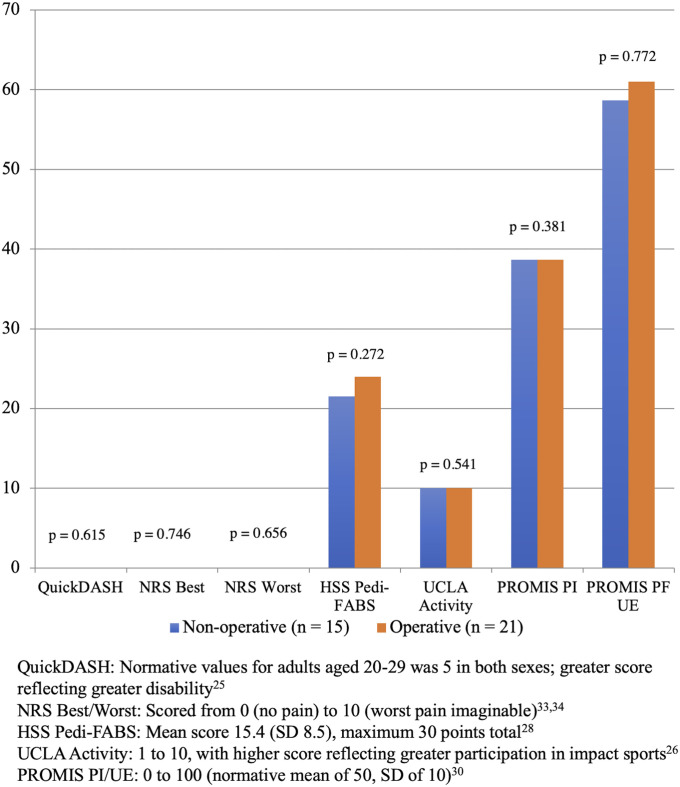
PROM scores were similar comparing patients who were treated operatively and those who were treated nonoperatively (Fig. 1). Patients with ≥100% translation were more likely to be treated operatively (p = 0.005), yet patients with shortening of ≥15 mm or translation of ≥100% demonstrated PROM scores that were similar to those below this threshold (p > 0.05 for all comparisons) (Figs. 2 and 3). Operative treatment was used for 81% (26 of 32) of older adolescents (female patients ≥14 years of age and male patients ≥16 years of age at the time of the injury), yet PROM scores were similar (p > 0.05 for all comparisons) between operatively and nonoperatively treated older adolescents (Fig. 4).
Fig. 1.
Median PROMs.
Fig. 2.
Median PROMs for patients with shortening of ≥15 mm.
Fig. 3.
Median PROMs for patients with translation of ≥100%.
Fig. 4.
Median PROMs for female patients ≥14 years of age and male patients ≥16 years at the time of the injury.
Discussion
The goal of this study was to determine, at the intermediate-term follow-up, whether functional, pain, union, implant removal, and refracture outcomes were improved in children and adolescents with midshaft clavicle fractures treated operatively compared with nonoperatively. Scores were similar between groups; at the intermediate-term follow-up, patients in both groups had no pain and were functioning normally with no nonunions and similar refracture rates. The mean age for patients treated operatively was 2.5 years older than for patients treated nonoperatively. Patients treated operatively were more likely to have translation of ≥100%. In a subanalysis of patients with greater shortening and translation and in older patients at or near skeletal maturity, scores remained similar. Of the operatively treated patients, 19% underwent subsequent implant removal. The majority of patients treated nonoperatively were treated by pediatric orthopaedic surgeons, and the majority of patients treated operatively were treated by adult orthopaedic (sports, trauma, and upper extremity) surgeons.
Two recent meta-analyses studied operative management compared with nonoperative management of midshaft clavicle fractures in children and adolescents. In their meta-analysis, Gao et al. included 12 studies and concluded that operative management yields faster return to activity, superior Constant scores, and equal QuickDASH scores7. Although Constant scores were significantly higher in operatively treated patients, all patients demonstrated favorable scores compared with the general, uninjured population. In their meta-analysis of 7 studies, Nawar et al. reported no difference in time to union, return to activity, or complications between operative and nonoperative management, concluding that there is no significant difference between operative and nonoperative management in the skeletally immature population8. The lack of nonunions in this cohort is consistent with the low rate reported in these meta-analyses (nonunion rates of <1% to 2% for nonoperative management and <1% to 3% for operative management7,8). The refracture rates of 5% in the operatively treated group and 3% in the nonoperatively treated group are in keeping with previously reported rates of 0% to 8.7%7,8. Our implant removal rate of 19% is in keeping with the previously reported rate of 15%7. The findings of the current study concur with both meta-analyses’ conclusions with regard to no difference in QuickDASH scores. Of note, meta-analyses can only be as good as the pooled studies that make them, and in these meta-analyses, many of the original studies were limited by the lack of a comparison group, small series1,9-21, or, in larger cohorts, limited PROMs that, in turn, limited the comparison of functional outcomes13.
Range of motion, strength, and endurance have been investigated following operative and nonoperative management. In a pilot (underpowered) study of 8 operatively treated and 8 nonoperatively treated displaced clavicle fractures with >15-mm shortening, Parry et al. noted similar patient satisfaction and PROMs (QuickDASH and Constant scores). There was no difference in range of motion, strength, or endurance between operatively and nonoperatively treated patients, although operatively treated patients had 3% decreased abduction endurance compared with the uninjured side. That study was limited by the small sample size15. In their study, Schulz et al. reported on 16 nonoperatively treated pediatric fractures with a mean displacement of 133% (range, 100% to 193%) and a mean shortening of 11.8 mm (range, 5 to 21 mm)21; strength deficits were observed. They compared the operative side with the nonoperative side; there was no control group. Importantly, the nonoperative side was the dominant side for 81% (13 of 16) of patients, and the dominant side is known to be stronger without exception in male patients and female patients35. External rotation maximal strength was reduced by 8.4% (p = 0.04) and abduction endurance diminished by 12% (p = 0.04) compared with the uninjured side21. The strength differential between dominant and nondominant arms is estimated at 3% to 10%36-42. It is not possible to discern whether these identified strength differences are due to weakness after healing in a malunited state or confounding due to hand dominance. QuickDASH scores were similar to normative values21. That study was limited by the small sample size of 16 patients, the lack of a comparison group, and the lack of control for hand dominance.
In a study of 16 children and adolescents with malunion following an initial fracture with displacement of >2 cm, Bae et al. noted no clinically important pain, loss of strength, loss of motion, or difference in patient satisfaction and aesthetic appearance43. They concluded that motion and strength concerns in displaced nonsegmental fractures should not dictate the need for surgical fixation.
In adults, the COTS published the first randomized trial of operative compared with nonoperative management of displaced midshaft clavicle fractures. The time to radiographic union was shorter for operative treatment (16 weeks) compared with nonoperative treatment (28 weeks). The nonunion rates were 3% (2 of 62 patients) for operative treatment and 14% (7 of 49 patients) for nonoperative treatment. Satisfaction was superior in the operatively treated group at 1 year (84% compared with 53% satisfied) (p < 0.05). Constant and QuickDASH scores were superior across all time points in the operative group (p ≤ 0.05 for all comparisons)5. Importantly, this study included only a few adolescents, all of whom were likely at or near skeletal maturity, which differs from the population of the present study. Since 2007, many additional high-quality studies have been performed in adults. A recent meta-analysis pooling results showed that operative treatment of midshaft clavicle fractures results in a nonunion rate of 1.4% compared with 10.5% for nonoperative treatment (p < 0.01). The malunion rates were 6.4% for operatively managed fractures and 13.6% for nonoperatively managed fractures44. Constant and DASH scores favored operative treatment (p < 0.01). A faster return to work or daily activities was also seen for operative treatment44. Findings from the original COTS trial5 have been replicated over time, yet, with their focus on adults, the results still have limited relevance to guiding treatment for children and adolescents.
The results of this study should be interpreted in the context of its limitations. First, this was a retrospective study, and, although inclusion criteria were relatively tight, the operatively and nonoperatively treated groups were not the same at baseline, with the operatively treated group, on average, 2.5 years older, with a greater proportion of ≥100% translation (78% operative compared with 47% nonoperative; p = 0.005). However, in a subanalysis of patients with ≥100% translation and in patients at or near skeletal maturity, outcomes remained similar.
Second, there were no defined criteria for surgical treatment in this study; treatment was by surgeon preference. Patients <21 years of age presenting to the NYP/Weill Cornell Medical Center emergency department are typically treated by the pediatric orthopaedic surgeon on call, although skeletally mature patients in this age range may alternatively be treated by the on-call adult orthopaedic trauma surgeon on a case-by-case basis. Depending on patient and surgeon preference, some patients are discharged home from the emergency department in a sling and follow-up is arranged on an outpatient basis with their surgeon of choice, who then determines management. Some families of adolescents will seek treatment from a pediatric orthopaedic surgeon, and others will seek treatment from an adult sports, upper-extremity, or trauma surgeon. Forty-one (95%) of 43 operatively treated patients were treated by adult sports, trauma, and upper-extremity orthopaedic surgeons, and 30 (83%) of 36 nonoperatively treated patients were treated by pediatric orthopaedic surgeons. It is possible that adult sports, trauma, and upper-extremity surgeons, accustomed to treating many of their adult patients with clavicle fractures with a surgical procedure, may favor treating pediatric and adolescent patients in this same manner.
Third, this study did not investigate the effect of other factors such as fixation method, although all patients were treated with a single precontoured plate or the double-plating technique popular at our institutions. Similarly, postoperatively protocols were not evaluated, but are known to be fairly consistent within the institutions.
Fourth, only 26% (79 of 302) of potentially eligible patients responded, provided consent themselves or through their parents or guardians, and completed the study. A thorough attempt was made to include all patients, with 5 contact attempts made to each family before considering them lost to follow-up. Tracking down children and adolescents years after the injury is fraught with challenges; families move, children leave home, and telephone numbers and last names change. Nonresponse sampling error is possible; patients who responded may not have been representative of the entire cohort. Although subsequent refracture and implant removal appeared similar between responders and nonresponders, it is possible that the implant was removed or a refracture occurred following their last contact at our hospitals. Many characteristics were similar, but we did note that a higher proportion of participating patients were female and were managed operatively when compared with the nonresponders.
Fifth, function and activity were self-reported, and physical examination data were not collected at the time of the telephone follow-up. Sixth, the PROMs used were not validated for the age of every participant (for instance, the HSS Pedi-FABS is validated for 10 to 18 years, and some patients at the time of follow-up were 22 years of age), although they have been used previously in similar, slightly out-of-range age groups27. Seventh, the limited sample size was likely not sufficient to draw definitive conclusions from the analyses of the secondary outcomes, but the results presented here should provide preliminary data for powering future studies for these outcomes. Finally, the minimally clinical important difference (MCID), substantial clinical benefit, and patient acceptable symptomatic state (PASS) are unknown for many patient-reported outcome scores after pediatric orthopaedic procedures45-47, and the value of 10 points for the QuickDASH score used for sample-size calculation was based on adult literature5.
In this subset of the cohort who responded to questionnaires and PROMs, the outcomes of midshaft clavicle fractures in children and adolescents were similar at the intermediate-term follow-up when treated operatively compared with nonoperatively, even for notably shortened and translated fractures and patients at or near skeletal maturity. Outcomes were excellent regardless of treatment method. There was no measurable benefit to operative management in primarily older adolescents compared with nonoperative management in slightly younger patients. Nonoperative management should be considered as first-line treatment for most pediatric displaced clavicle fractures, and operative management should potentially be reserved for atypical cases such as floating shoulder, multitrauma, open fractures, nonunions, and symptomatic malunions, given similar pain and functional outcomes, increased cost of operative fixation, and potential need for a secondary surgical procedure or plate removal. A definitive, prospective comparative study focusing on the most controversial age groups (14 to 18 years of age in female patients and 16 to 20 years of age in male patients) is warranted.
Footnotes
Investigation performed at the Hospital for Special Surgery and New York Presbyterian–Weill Cornell Medical Center, New York, NY
Disclosure: The authors indicated that no external funding was received for any aspect of this work. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A244).
References
- 1.Randsborg PH, Fuglesang HFS, Røtterud JH, Hammer OL, Sivertsen EA. Long-term patient-reported outcome after fractures of the clavicle in patients aged 10 to 18 years. J Pediatr Orthop. 2014June;34(4):393-9. [DOI] [PubMed] [Google Scholar]
- 2.Landin LA. Fracture patterns in children. Analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950-1979. Acta Orthop Scand Suppl. 1983;202:1-109. [PubMed] [Google Scholar]
- 3.Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994March;300:127-32. [PubMed] [Google Scholar]
- 4.Wick M, Müller EJ, Kollig E, Muhr G. Midshaft fractures of the clavicle with a shortening of more than 2 cm predispose to nonunion. Arch Orthop Trauma Surg. 2001;121(4):207-11. [DOI] [PubMed] [Google Scholar]
- 5.Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007January;89(1):1-10. [DOI] [PubMed] [Google Scholar]
- 6.Carry PM, Koonce R, Pan Z, Polousky JD. A survey of physician opinion: adolescent midshaft clavicle fracture treatment preferences among POSNA members. J Pediatr Orthop. 2011Jan-Feb;31(1):44-9. [DOI] [PubMed] [Google Scholar]
- 7.Gao B, Dwivedi S, Patel SA, Nwizu C, Cruz AI, Jr. Operative versus nonoperative management of displaced midshaft clavicle fractures in pediatric and adolescent patients: a systematic review and meta-analysis. J Orthop Trauma. 2019November;33(11):e439-46. [DOI] [PubMed] [Google Scholar]
- 8.Nawar K, Eliya Y, Burrow S, Peterson D, Ayeni O, de Sa D. Operative versus non-operative management of mid-diaphyseal clavicle fractures in the skeletally immature population: a systematic review and meta-analysis. Curr Rev Musculoskelet Med. 2020February;13(1):38-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vander Have KL, Perdue AM, Caird MS, Farley FA. Operative versus nonoperative treatment of midshaft clavicle fractures in adolescents. J Pediatr Orthop. 2010June;30(4):307-12. [DOI] [PubMed] [Google Scholar]
- 10.Hagstrom LS, Ferrick M, Galpin R. Outcomes of operative versus nonoperative treatment of displaced pediatric clavicle fractures. Orthopedics. 2015February;38(2):e135-8. [DOI] [PubMed] [Google Scholar]
- 11.Luo TD, Ashraf A, Larson AN, Stans AA, Shaughnessy WJ, McIntosh AL. Complications in the treatment of adolescent clavicle fractures. Orthopedics. 2015April;38(4):e287-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herzog MM, Whitesell RC, Mac LM, Jackson ML, Culotta BA, Axelrod JR, Busch MT, Willimon SC. Functional outcomes following non-operative versus operative treatment of clavicle fractures in adolescents. J Child Orthop. 2017August1;11(4):310-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mukhtar IA, Yaghmour KM, Ahmed AF, Ibrahim T. Flexible intramedullary nailing versus nonoperative treatment for paediatric displaced midshaft clavicle fractures. J Child Orthop. 2018April1;12(2):104-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Song MH, Yun YH, Kang K, Hyun MJ, Choi S. Nonoperative versus operative treatment for displaced midshaft clavicle fractures in adolescents: a comparative study. J Pediatr Orthop B. 2019January;28(1):45-50. [DOI] [PubMed] [Google Scholar]
- 15.Parry JA, Van Straaten M, Luo TD, Simon AL, Ashraf A, Kaufman K, Larson AN, Shaughnessy WJ. Is there a deficit after nonoperative versus operative treatment of shortened midshaft clavicular fractures in adolescents? J Pediatr Orthop. 2017June;37(4):227-33. [DOI] [PubMed] [Google Scholar]
- 16.Li Y, Helvie P, Farley FA, Abbott MD, Caird MS. Complications after plate fixation of displaced pediatric midshaft clavicle fractures. J Pediatr Orthop. 2018August;38(7):350-3. [DOI] [PubMed] [Google Scholar]
- 17.Robinson L, Gargoum R, Auer R, Nyland J, Chan G. Sports participation and radiographic findings of adolescents treated nonoperatively for displaced clavicle fractures. Injury. 2015July;46(7):1372-6. Epub 2015 Apr 23. [DOI] [PubMed] [Google Scholar]
- 18.Namdari S, Ganley TJ, Baldwin K, Rendon Sampson N, Hosalkar H, Nikci V, Wells L. Fixation of displaced midshaft clavicle fractures in skeletally immature patients. J Pediatr Orthop. 2011Jul-Aug;31(5):507-11. [DOI] [PubMed] [Google Scholar]
- 19.Frye BM, Rye S, McDonough EB, Bal GK. Operative treatment of adolescent clavicle fractures with an intramedullary clavicle pin. J Pediatr Orthop. 2012June;32(4):334-9. [DOI] [PubMed] [Google Scholar]
- 20.Rapp M, Prinz K, Kaiser MM. Elastic stable intramedullary nailing for displaced pediatric clavicle midshaft fractures: a prospective study of the results and patient satisfaction in 24 children and adolescents aged 10 to 15 years. J Pediatr Orthop. 2013September;33(6):608-13. [DOI] [PubMed] [Google Scholar]
- 21.Schulz J, Moor M, Roocroft J, Bastrom TP, Pennock AT. Functional and radiographic outcomes of nonoperative treatment of displaced adolescent clavicle fractures. J Bone Joint Surg Am. 2013July3;95(13):1159-65. [DOI] [PubMed] [Google Scholar]
- 22.Li Y, Donohue KS, Robbins CB, Pennock AT, Ellis HB, Jr, Nepple JJ, Pandya N, Spence DD, Willimon SC, Heyworth BE; Function After Adolescent Clavicle Trauma and Surgery (FACTS) Multicenter Study Group. Reliability of radiographic assessments of adolescent midshaft clavicle fractures by the FACTS Multicenter Study Group. J Orthop Trauma. 2017September;31(9):479-84. [DOI] [PubMed] [Google Scholar]
- 23.Beaton DE, Wright JG, Katz JN; Upper Extremity Collaborative Group. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005May;87(5):1038-46. [DOI] [PubMed] [Google Scholar]
- 24.Aasheim T, Finsen V. The DASH and the QuickDASH instruments. Normative values in the general population in Norway. J Hand Surg Eur Vol. 2014. February;39(2):140-4. Epub 2013 Mar 20. [DOI] [PubMed] [Google Scholar]
- 25.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998December;13(8):890-5. [DOI] [PubMed] [Google Scholar]
- 26.Fabricant PD, Robles A, Downey-Zayas T, Do HT, Marx RG, Widmann RF, Green DW. Development and validation of a pediatric sports activity rating scale: the Hospital for Special Surgery Pediatric Functional Activity Brief Scale (HSS Pedi-FABS). Am J Sports Med. 2013October;41(10):2421-9. Epub 2013 Jul 26. [DOI] [PubMed] [Google Scholar]
- 27.Fabricant PD, Suryavanshi JR, Calcei JG, Marx RG, Widmann RF, Green DW. The Hospital for Special Surgery Pediatric Functional Activity Brief Scale (HSS Pedi-FABS): normative data. Am J Sports Med. 2018April;46(5):1228-34. Epub 2018 Mar 7. [DOI] [PubMed] [Google Scholar]
- 28.Amtmann D, Cook KF, Jensen MP, Chen WH, Choi S, Revicki D, Cella D, Rothrock N, Keefe F, Callahan L, Lai JS. Development of a PROMIS item bank to measure pain interference. Pain. 2010July;150(1):173-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gausden EB, Levack AE, Sin DN, Nwachukwu BU, Fabricant PD, Nellestein AM, Wellman DS, Lorich DG. Validating the Patient Reported Outcomes Measurement Information System (PROMIS) computerized adaptive tests for upper extremity fracture care. J Shoulder Elbow Surg. 2018July;27(7):1191-7. Epub 2018 Mar 19. [DOI] [PubMed] [Google Scholar]
- 30.Döring AC, Nota SPFT, Hageman MGJS, Ring DC. Measurement of upper extremity disability using the Patient-Reported Outcomes Measurement Information System. J Hand Surg Am. 2014June;39(6):1160-5. Epub 2014 May 3. [DOI] [PubMed] [Google Scholar]
- 31.Kaat AJ, Rothrock NE, Vrahas MS, OʼToole RV, Buono SK, Zerhusen T, Jr, Gershon RC. Longitudinal validation of the PROMIS physical function item bank in upper extremity trauma. J Orthop Trauma. 2017October;31(10):e321-6. [DOI] [PubMed] [Google Scholar]
- 32.Price DD, Bush FM, Long S, Harkins SW. A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain. 1994February;56(2):217-26. [DOI] [PubMed] [Google Scholar]
- 33.Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978August;37(4):378-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Altamimi SA, McKee MD; Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. Surgical technique. J Bone Joint Surg Am. 2008March;90(Suppl 2 Pt 1):1-8. [DOI] [PubMed] [Google Scholar]
- 35.Van Harlinger W, Blalock L, Merritt JL. Upper limb strength: study providing normative data for a clinical handheld dynamometer. PM R. 2015February;7(2):135-40. Epub 2014 Sep 20. [DOI] [PubMed] [Google Scholar]
- 36.Crosby CA, Wehbé MA, Mawr B. Hand strength: normative values. J Hand Surg Am. 1994July;19(4):665-70. [DOI] [PubMed] [Google Scholar]
- 37.Petersen P, Petrick M, Connor H, Conklin D. Grip strength and hand dominance: challenging the 10% rule. Am J Occup Ther. 1989July;43(7):444-7. [DOI] [PubMed] [Google Scholar]
- 38.Reikerås O. Bilateral differences of normal hand strength. Arch Orthop Trauma Surg. 1983;101(3):223-4. [DOI] [PubMed] [Google Scholar]
- 39.Schmidt RT, Toews JV. Grip strength as measured by the Jamar dynamometer. Arch Phys Med Rehabil. 1970June;51(6):321-7. [PubMed] [Google Scholar]
- 40.Swanson AB, Matev IB, de Groot G. The strength of the hand. Bull Prosthet Res. 1970;10(14):145-53. [PubMed] [Google Scholar]
- 41.Thorngren KG, Werner CO. Normal grip strength. Acta Orthop Scand. 1979June;50(3):255-9. [DOI] [PubMed] [Google Scholar]
- 42.Armstrong CA, Oldham JA. A comparison of dominant and non-dominant hand strengths. J Hand Surg Br. 1999August;24(4):421-5. [DOI] [PubMed] [Google Scholar]
- 43.Bae DS, Shah AS, Kalish LA, Kwon JY, Waters PM. Shoulder motion, strength, and functional outcomes in children with established malunion of the clavicle. J Pediatr Orthop. 2013Jul-Aug;33(5):544-50. [DOI] [PubMed] [Google Scholar]
- 44.DPJ Smeeing, van der Ven DJC, Hietbrink F, Timmers TK, van Heijl M, Kruyt MC, Groenwold RHH, van der Meijden OAJ, Houwert RM. Surgical versus nonsurgical treatment for midshaft clavicle fractures in patients aged 16 years and older: a systematic review, meta-analysis, and comparison of randomized controlled trials and observational studies. Am J Sports Med. 2017July;45(8):1937-45. Epub 2016 Nov 18. [DOI] [PubMed] [Google Scholar]
- 45.Cvetanovich GL, Gowd AK, Liu JN, Nwachukwu BU, Cabarcas BC, Cole BJ, Forsythe B, Romeo AA, Verma NN. Establishing clinically significant outcome after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2019May;28(5):939-48. Epub 2019 Jan 24. [DOI] [PubMed] [Google Scholar]
- 46.Nwachukwu BU, Chang B, Fields K, Rebolledo BJ, Nawabi DH, Kelly BT, Ranawat AS. Defining the “substantial clinical benefit” after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med. 2017May;45(6):1297-303. Epub 2017 Feb 1. [DOI] [PubMed] [Google Scholar]
- 47.Gowd AK, Lalehzarian SP, Liu JN, Agarwalla A, Christian DR, Forsythe B, Cole BJ, Verma NN. Factors associated with clinically significant patient-reported outcomes after primary arthroscopic partial meniscectomy. Arthroscopy. 2019May;35(5):1567-1575.e3. Epub 2019 Apr 15. [DOI] [PubMed] [Google Scholar]