Supplemental Digital Content is available in the text.
Abstract
Background:
Lower lip depression was historically regarded a neglected area of facial paralysis, but, with refinement of techniques, has gained increasing attention. We present the first detailed description and evaluation of a 2-stage technique, using first cross facial nerve graft and then the anterior belly of digastric muscle (ABDM), innervated by the cross facial nerve graft, to restore dynamic and spontaneous lower lip depression.
Methods:
Retrospective analysis of 2-stage lower lip reanimations between 2010 and 2018 was performed. Demographics, etiology, and operative details were recorded. Videos were graded pre/postoperatively using a 5-point Likert scale by 21 independent observers. Objective changes of symmetry were analyzed using Photogrammetry (Emotrics).
Results:
Twenty-seven patients were identified (median age 34.9 years, range 6–64). The mean duration between the 2 stages was 15.1 months. Follow-up ranged from 18–72 months. There were minor complications in 4 patients, and 1 case was abandoned due to insufficient length of anterior belly of digastric muscle. Average peer-reviewed scores improved from 2.1 to 3.2 (P < 0.05). Emotrics did not show improvement in static symmetry (P > 0.05). However, during open-lip smiling, lower lip height improved significantly (P < 0.05) whilst dental show improvements approached significance (P < 0.08). Lower lip symmetry was also improved during lower lip depression, as shown by improvements in lower lip height (P < 0.05), smile angle, and dental show (both P < 0.05).
Conclusions:
These results show the safety and efficacy of 2-stage lower lip reanimation using anterior belly of digastric muscle transposition. This procedure is our choice for longstanding lower lip paralysis and provides coordinated spontaneous lower lip depression, thus enhancing the overall perioral animation and smile.
Introduction
Society places a high value on symmetrical facial movements. As such, many techniques have evolved to treat facial paralysis.1 These strive for symmetry in repose, voluntary movement, and spontaneous expression, but focus predominantly on upper lip and smile restoration.2,3 Functioning lower lip depressors are also important, not just for a full denture smile, but for subtle movement of lower lip and phonetics in everyday conversation. Even after successful restoration of upper lip movement, lack of lower lip retraction remains an obvious stigma of facial paralysis.
Palsy of the marginal mandibular branch (MMB) of the facial nerve, the primary innervator of lower lip movement, can be isolated or part of a global facial paralysis. Arising from the facial nerve cervicofacial trunk, the MMB runs from 2 cm above, to just below the inferior margin of the mandible. It courses usually superficially across the facial vessels, then runs superiorly. It gives branches to platysma, depressor anguli oris, orbicularis oris, depressor labii inferioris, and mentalis.4 MMB paralysis can be part of a developmental condition or secondary to trauma, iatrogenic injury, tumors, infection, or higher facial nerve insult. The resulting asymmetric smile and inability to depress or lateralize the lower lip impacts upon social function, oral continence, and eating.4,5
Treatments for lower lip paralysis aim to either:
1) Make the paralysis less noticeable by weakening the contralateral side, or
2) Restore lower lip depression.
Botulinum toxin, neurectomy, and myomectomy achieve the former, and slings and neurotization of the MMB or depressor muscles the latter.5–8 In cases with no potential for reinnervation (longstanding paralysis; no residual depressor muscle function), muscle transfers are necessary to restore dynamic symmetry.4 Transposition of the anterior belly of digastric muscle (ABDM) works well owing to its location and innervation (mylohyoid branch of the mandibular division of trigeminal nerve), as it remains functional in most cases of facial paralysis (Fig. 1). Originally transposed in combination with fascia lata strips,9 the use as single-stage muscle transfer to the lower lip has been adopted and modified.2,6,7,10,11 This technique, however, does not provide spontaneous reanimation as it relies upon trigeminal motor innervation. Dynamism can be achieved following rehabilitation and training by clenching the teeth, but a true symmetrical, emotionally responsive contraction of the muscle is only possible with innervation via a cross facial nerve graft (CFNG) from the contralateral facial nerve. A 2-stage method where a CFNG is placed, and the muscle transferred at least 6 months later offers potential to achieve a more natural dynamic result.4
Fig. 1.
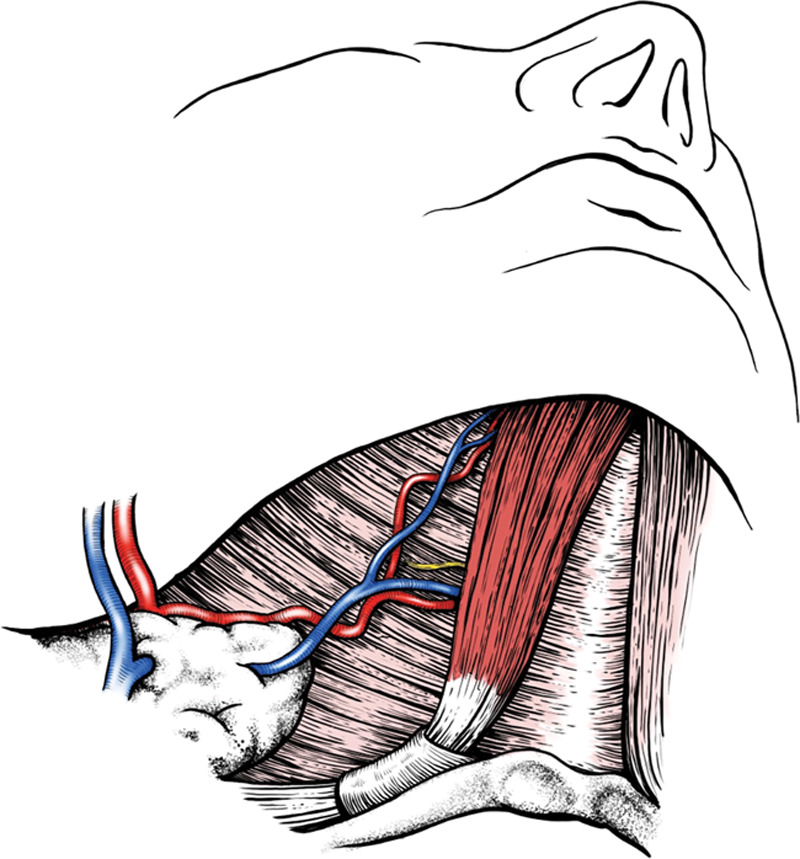
Anatomy of the ABDM, with its nerve (branch from the nerve to mylohyoid) and the vascular pedicle (submental branches of the facial artery and vein).
The senior author (KT) employs a holistic approach to managing facial paralysis and has performed 2-stage ABDM transfer for many years. Having modified and refined the technique, the authors detail it below, to facilitate replication in other centers.
Methods
Patient Selection
Management of facial paralysis depends largely on time since injury. Our decision algorithm is depicted in Figure 2. Muscle transfer for lower lip reanimation was offered to all patients with longstanding paralysis and no residual depressor muscle function (confirmed with electromyography (EMG) studies). Patients were assessed in a tailored facial palsy clinic by the operating surgeon and specialized facial therapists. The stages were planned in conjunction with other necessary procedures; in those with more extensive paralysis, all CFNG were performed at the same time (eg, to upper lip or eyelids). Such patients then underwent other procedures such as free-gracilis transfer for smile, or adjustments to slings and weights. The second stage of lower lip reanimation, the ABDM transposition, was intended as the final facial symmetrization procedure.
Fig. 2.
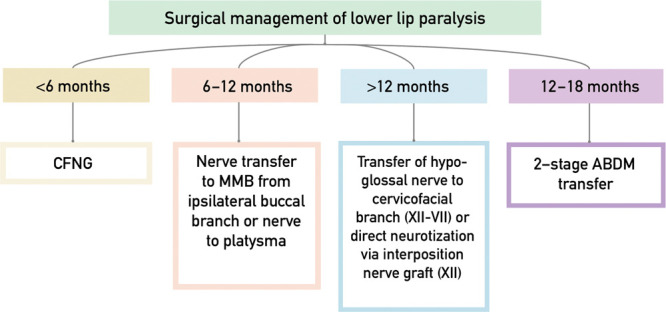
St. Andrew’s algorithm for management of lower lip paralysis.
Procedural Technique
All operations were performed by the senior author (KT), each approximately 2–3 hours.
First Stage: CFNG
Patients were anesthetized with the nasal endotracheal tube facing cephalad. Sural nerve grafts were harvested via stab incisions. Functioning, contralateral facial nerves (CNVII) were accessed via a modified facelift incision. A nerve stimulator (VARI-STIM III Medtronic Xomed Inc. USA, setting 2 mA) is used to carefully identify the various branches and ensure the donors were not the sole innervator of the lower lip. Based on anatomical studies,12,13 the MMB has 3–4 distal branches; so it is safe to use 1 or 2 of these, as well as a lower buccal branch that retracts the lower lip or stimulates risorius, without imparting donor weakness.
Sural nerve grafts were reversed and tunneled subcutaneously through the cheek to a submental pocket on the affected side. Proximally, it was splayed to coapt (end-to-end with 9/0 non-absorbable Ethilon) to the 2 or 3 identified terminal facial nerve branches. Via 2 small incisions (1 at the submental crease and 1 halfway along the ABDM), the CFNG end was draped at full length, and the distal end was tagged with a ligaclip (Fig. 3).
Fig. 3.
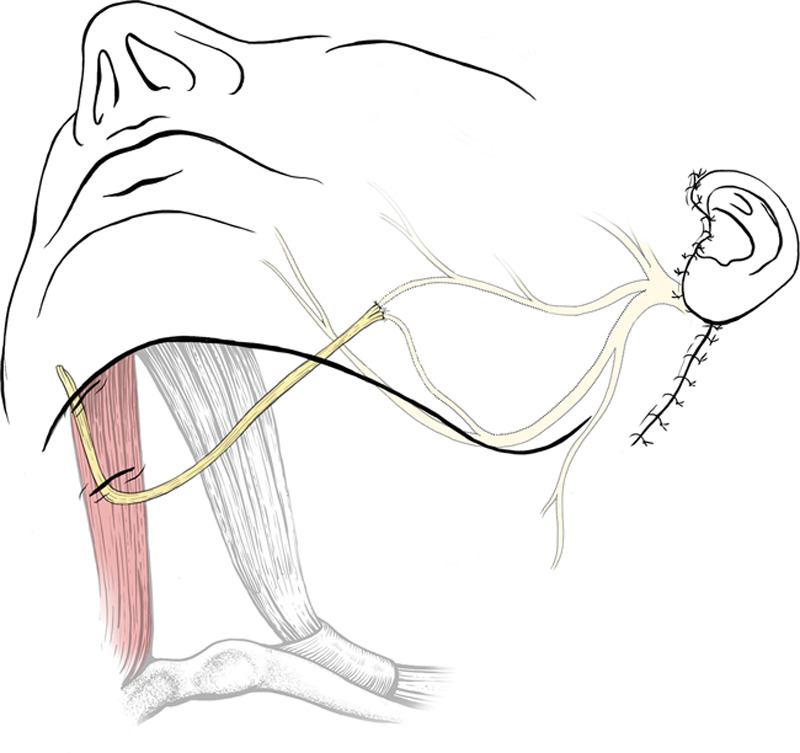
Stage 1: CFNG coapted to 2–3 terminal lower buccal and MMBs of functional facial nerve, then banked subcutaneously in submandibular region of the affected side of the face.
Second Stage: ABDM Transfer
Patients were reviewed at 3–4-monthly intervals until evidence of axonal regeneration was evident at the submental site (the Tinel test). At the second stage, ABDM surface anatomy was marked, the incision over ABDM was re-opened to 3 cm, (through skin and fat only), and the CFNG was found and protected (See Video 1 [online], which demonstrates the operative technique (second stage).). The platysma was incised by 4 cm to access ABDM, arising from the lower mandibular border close to the midline.
Video 1. Video 1 from “Reanimation of the lower lip: experience using the anterior belly of digastric muscle as a two-stage procedure”.
The vascular pedicle was preserved (submental branch of the facial artery/vein, which enters the muscle on the lateral and deep aspect, in the middle third). The innervating branch of the mylohyoid nerve was identified with the nerve stimulator, deeper and slightly superior to the vascular pedicle. The ABDM conjoint tendon at the hyoid was divided as posteriorly as possible for maximal length, and the tendon split into 2 (Fig. 4A). Two 1-cm incisions were made in the ipsilateral lower lip (dividing into thirds from midline to commissure), in the red line between the wet and dry mucosa.
Fig. 4.
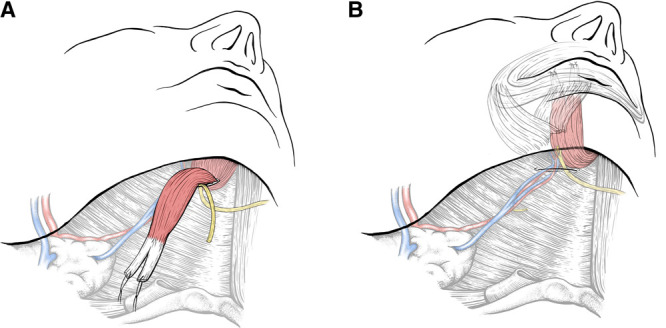
Key parts of the operation during Stage 2: A, CFNG identified and released; ABDM divided at the conjoint tendon and the tendon divided into 2 slips. B, ABDM with coaptation of CFNG, tunneled to the lower lip in a submuscular plane. Vascular pedicle preserved.
The ABDM was transposed cephalad to the lower lip, with minimal dissection of the pedicle, and preserving a small vessel entering ABDM at the mandibular insertion. Sub-mentalis tunneling of ABDM avoided bulging, while staying supraperiosteal avoided mental nerve injury (although the nerve is more lateral). Tendinous slips were anchored into the central part of orbicularis oris using 3/0 polydiaxonone (Ethicon PDSII), with 4/0 polyglactin 910 (Ethicon Vicryl) to close the mucosa (Fig. 4B). The slips were tensioned so that the medial part was overcorrected slightly, but not laterally to avoid notching. The nerve to ABDM was divided close to the hilum and coapted end-to-end to the CFNG, using 9/0 sutures. Due to size mismatch with the small mylohyoid branch (1–2 fascicles), the remaining CFNG fascicles were splayed to directly neurotize the ABDM.
Absorbable sutures closed the incisions and a thermoplastic splint was applied to secure lip depression. Patients were encouraged to wear this for 1 week, and to consciously exercise/retract the lower lip in front of a mirror for 4 months.
Study Design
All patients who underwent the 2-stage lower lip reanimation, and with ≥18-month follow-up were identified. Information gathered included demographics, etiology, extent and duration of paralysis, number of facial palsy procedures, complications, and revisions.
Independent Observer Ratings
All patients were invited to undergo standardized pre- and postoperative video- and photography. At the clinical photography department, attempts are made for each patient with facial palsy to elicit a spontaneous smile, and all patients are also asked to give a short narrative to assess lower lip movement on normal talking.
Independent observers graded the videos using a 5-point Likert scale based on Terzis’ lower lip aesthetic grading scale.4,14 The original scale was from 0 to 2 in 0.5 increments. This was changed to 1–5 in whole number increments to simplify data handling (Table 1). Images were randomly ordered to eliminate bias. The observers were unpaid, with no affiliation to our unit, and were instructed to grade only the lower lip ignoring other features of the facial paralysis. Observers included 4 medical artists, 8 junior doctors or postgraduate MSc students, and 9 plastic surgery registrars/consultants. Videos were shown in a random order to avoid bias from knowing whether images were pre- or post-surgery.
Table 1.
Modified Terzis’ Lower Lip Grading Scale4
| Original Terzis’ Scale | Modified Scale | Designation | Description |
|---|---|---|---|
| 0 | 1 | Poor | Total paralysis |
| 0.5 | 2 | Fair | Trace contraction with no movement |
| 1 | 3 | Moderate | Observable movement but inadequate excursion and without symmetry |
| 1.5 | 4 | Good | Almost complete excursion of lower lip with depression and full denture smile |
| 2 | 5 | Excellent | Normal symmetric movement of lower lip |
Photogrammetry
The following pre- and postoperative photograph sets were downloaded for each patient: repose, maximal open-lip smile, and lower lip depression (as in saying “eeee”). Patients were excluded for a particular smile analysis if they did not have both pre- and postoperative photographs for that pose (complete set).
Complete sets were analyzed using Emotrics.15 Emotrics compares landmark position differences between the pre- and postoperative photographs, providing readings for both affected and unaffected sides, thereby computing excursion of facial landmarks and changes in symmetry.
The following measurements were computed for each pose:
repose: commissure height, lower lip height and upper lip height.
maximal open-lip smile and lower lip depression: commissure height, commissure excursion, dental show, smile angle, and lower lip height.
Statistics
The Shapiro-Wilk test assessed for normality of data distribution. Kendall W was used for interrater variability. Gaussian data were reported as means (SD), whereas skewed data were reported as medians (range). The significance of the differences in mean pre- and postoperative landmark position and excursion was tested using paired t-tests (Gaussian) and Wilcoxon signed rank test (skewed). Paired t-tests (normal distribution) and Mann-Whitney tests (skewed distribution) were used to test the significance of the differences in landmark symmetry. Statistical significance was set at P < 0.5.
Results
Cohort and Operative Data
Table 2 summarizes the results. Twenty-seven patients were eligible (13 men, 14 women). Mean age at ABDM transfer was 34.9 years (range 6–64). All had complete paralysis of the lower lip (16 right-sided and 11 left-sided). Seven patients (25.9%) had isolated lower lip paralysis, eight (29.6%) had more extensive but still partial paralysis, 12 (44.4%) had global/complete facial palsy. Nine patients (33.3%) had developmental paralysis and 11 (40.7%) had post-tumor resection paralysis, mostly acoustic neuroma (n = 8). Five patients (18.5%) had longstanding Bell’s palsy, 1 was secondary to neurofibromatosis and 1 iatrogenic, following cyst excision and MMB damage.
Table 2.
Summary of Patients Undergoing 2-stage Lower Lip Reanimation with ABDM
| ID | Sex | Age at ABDM Transfer (y) | Laterality of FP | Etiology | Comorbidities | Extent of Paralysis | Total FP Operations | ABDM Transfer Operation Number | Time between CFNG & ABDM (Mo) | Complications Post-ABDM Transfer | ABDM Revision Operations | Preoperative Score | Postoperative Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 12 | R | Developmental | Velocardiofacial syndrome, cleft palate, velopharyngeal dysfunction | Isolated lower lip | 2 | 2 | 8 | Minor infection | 0 | 2 | 2.5 |
| 2 | M | 6 | R | Developmental | Nil else | Isolated lower lip | 2 | 2 | 10 | Mild dermatitis | 0 | 2.3 | 3.8 |
| 3 | M | 32 | L | Developmental | Nil else | Isolated lower lip | 2 | 2 | 6 | N | 0 | 1.6 | 3.4 |
| 4 | F | 6 | R | Developmental | Asthma | Global | 4 | 3 | 11 | N | 0 | 3 | 4 |
| 5 | F | 64 | R | Tumor | Asthma | Partial | 3 | 3 | 8 | N | 0 | 2 | 2.4 |
| 6 | F | 55 | R | Tumor | HTN, CKD | Global | 6 | 5 | 12 | ABDM length insufficient for transfer | 0 | excluded | excluded |
| 7 | M | 47 | L | Tumor | Nil else | Global | 8 | 6 | 41 | Minor infection | 2 (Correction of notch & lipofilling x2) | 2.2 | 2.8 |
| 8 | M | 7 | R | Developmental | Amniotic band syndrome, syndactyly | Partial | 2 | 2 | 10 | N | 0 | 2.6 | 2.7 |
| 9 | F | 33 | L | Bell’s | Nil else | Partial | 4 | 3 | 27 | N | 1 (Lipofilling) | 1.9 | 3.2 |
| 10 | M | 49 | R | Bell’s | Nil else | Global | 5 | 3 | 34 | N | 2 (Correction of notch & lipofilling x2) | 1.8 | 2.8 |
| 11 | M | 39 | L | Tumor | Nil else | Global | 5 | 4 | 12 | Stitch abscess | 0 | 1.8 | 3.3 |
| 12 | F | 49 | R | Tumor | Hypertension, gastro- esophageal reflux, obesity | Partial | 2 | 2 | 10 | N | 0 | 1.9 | 2.5 |
| 13 | M | 24 | L | Tumor | Neurofibromatosis type II | Global | 4 | 4 | 3 | N | 0 | 1.7 | 3 |
| 14 | F | 22 | R | Tumor | Nil else | Global | 5 | 3 | 11 | N | 2 (Lipofilling) | 1.7 | 3.2 |
| 15 | M | 25 | R | Developmental | Nil else | Global | 3 | 3 | 11 | N | 0 | 2 | 3.4 |
| 16 | F | 57 | R | Tumor | Pernicious anemia | Partial | 2 | 2 | 5 | N | 0 | 1.5 | 2.2 |
| 17 | M | 26 | L | Developmental | Gastro- oesophageal reflux | Isolated lower lip | 2 | 2 | 6 | N | 0 | 2.3 | 4.6 |
| 18 | F | 14 | L | Developmental | Nil else | Isolated lower lip | 2 | 2 | 12 | N | 0 | 2.5 | 4.5 |
| 19 | F | 51 | R | Bell’s | Nil else | Partial | 2 | 2 | 6 | N | 0 | 1.9 | 3.1 |
| 20 | F | 16 | R | Bell’s | Asthma | Global | 4 | 3 | 11 | N | 0 | 2.1 | 3.1 |
| 21 | F | 48 | R | Tumor | Hypertension, type 2 diabetes | Global | 5 | 4 | 29 | N | 0 | 2.1 | 2.3 |
| 22 | M | 38 | L | Tumor | Nil else | Global | 3 | 3 | 26 | N | 0 | 1.4 | 2 |
| 23 | M | 60 | L | Tumor | Nil else | Global | 5 | 4 | 40 | N | 0 | 1.4 | 3.1 |
| 24 | F | 37 | L | Bell’s | Nil else | Partial | 3 | 3 | 39 | N | 0 | 2.1 | 2.6 |
| 25 | M | 36 | L | Developmental | Nil else | Isolated lower lip | 2 | 2 | 9 | N | 0 | 2.5 | 3.1 |
| 26 | F | 48 | R | Tumor | Nil else | Partial | 3 | 2 | 4 | N | 1 (Correction of lip notch) | 3.5 | 4.2 |
| 27 | M | 41 | R | Iatrogenic | Nil else | Isolated lower lip | 2 | 2 | 7 | N | 0 | 2.1 | 4.1 |
| 13 | M | 24 | L | Tumor | Neurofibromatosis type II | Global | 4 | 4 | 3 | N | 0 | 1.7 | 3 |
| 14 | F | 22 | R | Tumor | Nil else | Global | 5 | 3 | 11 | N | 2 (Lipofilling) | 1.7 | 3.2 |
| 15 | M | 25 | R | Developmental | Nil else | Global | 3 | 3 | 11 | N | 0 | 2 | 3.4 |
| 16 | F | 57 | R | Tumor | Pernicious anemia | Partial | 2 | 2 | 5 | N | 0 | 1.5 | 2.2 |
| 17 | M | 26 | L | Developmental | Gastro- oesophageal reflux | Isolated lower lip | 2 | 2 | 6 | N | 0 | 2.3 | 4.6 |
| 18 | F | 14 | L | Developmental | Nil else | Isolated lower lip | 2 | 2 | 12 | N | 0 | 2.5 | 4.5 |
| 19 | F | 51 | R | Bell’s | Nil else | Partial | 2 | 2 | 6 | N | 0 | 1.9 | 3.1 |
| 20 | F | 16 | R | Bell’s | Asthma | Global | 4 | 3 | 11 | N | 0 | 2.1 | 3.1 |
| 21 | F | 48 | R | Tumor | Hypertension, type 2 diabetes | Global | 5 | 4 | 29 | N | 0 | 2.1 | 2.3 |
| 22 | M | 38 | L | Tumor | Nil else | Global | 3 | 3 | 26 | N | 0 | 1.4 | 2 |
| 23 | M | 60 | L | Tumor | Nil else | Global | 5 | 4 | 40 | N | 0 | 1.4 | 3.1 |
| 24 | F | 37 | L | Bell’s | Nil else | Partial | 3 | 3 | 39 | N | 0 | 2.1 | 2.6 |
| 25 | M | 36 | L | Developmental | Nil else | Isolated lower lip | 2 | 2 | 9 | N | 0 | 2.5 | 3.1 |
| 26 | F | 48 | R | Tumor | Nil else | Partial | 3 | 2 | 4 | N | 1 (Correction of lip notch) | 3.5 | 4.2 |
| 27 | M | 41 | R | Iatrogenic | Nil else | Isolated lower lip | 2 | 2 | 7 | N | 0 | 2.1 | 4.1 |
Patients with isolated lower lip paralysis underwent 2 consecutive stages procedures. Those with complete palsy had free-gracilis muscle transfer (n = 8), or adjunctive procedures (eg, for the periorbital area) before ABDM transfer. The mean number of operations for all the patients was 3.4 (median 3, range 2–8). There was a mean 15.1 months (median 11) duration between the CFNG and the ABDM transfer.
Complications and Revisions
There were neither major complications nor donor weaknesses. There were 2 antibiotic-treated superficial infections, one each for splint dermatitis and stitch abscess. One patient in whom transposition was abandoned intraoperatively due to insufficient ABDM length was excluded from analysis. Follow-up ranged from 18–72 months (median 49) by the discharge date or analysis for this study. Five patients underwent lipofilling to correct minor lip notches.
Peer-reviewed Results
Twenty-one observers analyzed 26 patients’ results. Terzis scores improved from 2.1 to 3.2 (P < 0.001). Kendall’s W for interrater variability showed fair to average agreement amongst all raters. The difference between scores from medical artists, junior and senior surgeons, is seen in Table 3. Those perceived to have the greatest amount of improvement are shown in Figure 5. Those with least improvement were a 7-year-old boy with developmental paralysis (+0.1) and a 48-year-old woman (+0.2) with global paralysis. (See figure, Supplemental Digital Content 1, which displays the patients with the least improvement, as perceived by the raters. A, B, Demonstration of pre- and postoperative appearance of 7-year-old boy with developmental marginal mandibular palsy. C, D, Demonstration of pre- and postoperative appearance of 48-year-old woman with global facial paralysis (House-Brackmann VI) post acoustic neuroma resection, and history of hypertension and type 2 diabetes mellitus. http://links.lww.com/PRSGO/B593.)
Table 3.
Mean Facial Grading Scores of the Videos and Photographs of 26 Patients, Stratified by Observer Group
| Medical Artists (4) | SHO/MSc Students (8) | Registrar/Consultant (9) | All Observers (21) | |
|---|---|---|---|---|
| Mean preoperative score | 2.2 | 2.0 | 2.1 | 2.1 |
| Mean postoperative score | 3.3 | 3.0 | 3.3 | 3.2 |
| Mean improvement | 1.1 | 1.0 | 1.2 | 1.1 |
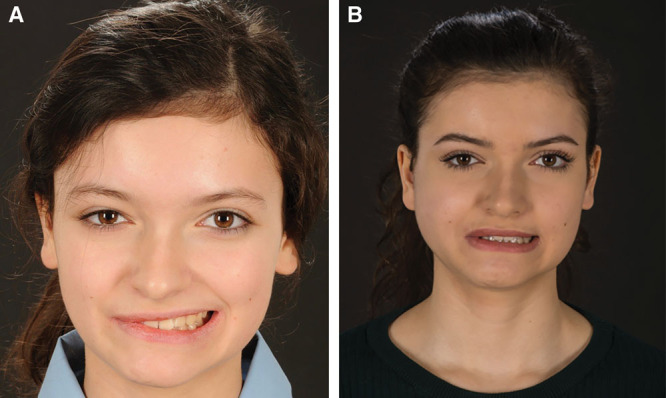
Fig. 5.

Patients with high levels of perceived improvement (each with pre- and postoperative appearance). Each patient had an isolated MMB paralysis and a 2-stage ABDM transfer. A, B, 41-year-old man, iatrogenic MMB injury following a subcutaneous mass removal along the right mandibular border 4 years before his presentation. C, D, 26-year-old man, developmental lower lip paralysis. E, F 14-year-old woman, developmental lower lip paralysis. G, H, 32-year-old man, developmental lower lip paralysis.
There was a greater mean improvement in appearance in the isolated MMB palsy group (+1.5) compared with those with more extensive paralysis (partial +0.7, global +1.1) (Fig. 6). A number of cases are shown in Video 2. (See Video 2 [online], which displays pre- and postoperative smiles demonstrated side-by-side for comparison, and spontaneous smile of the patient shown in Fig. 7.)
Fig. 6.
Patient with global facial paralysis (House-Brackmann V) due to Bell’s palsy. A, Preoperative image, aged 12. B, postoperative image, aged 16, following 3-stage procedure: (1) Placement of 2 CFNGs, to buccal and MMB nerves; (2) free-gracilis transfer; (3) ABDM transfer.
Fig. 7.

Lip notching requiring lipofilling.
Video 2. Video 2 from “Reanimation of the lower lip: experience using the anterior belly of digastric muscle as a two-stage procedure”.
Photogrammetry
Table 4 summarizes photogrammetric (Emotrics) results. The number of patients with complete sets for repose, open-lip smile, and lower lip eversion were 24, 22, and 11 respectively. There was no change in resting symmetry, as shown by nonsignificant changes (P > 0.05). However, during open-lip smiling, lower lip height improved significantly (P < 0.05), whilst dental show improvements approached significance (P < 0.08), whereas other measures did not change significantly (P > 0.05). Lower lip symmetry was also improved during lower lip depression as shown by improvements in lower lip height (P < 0.05), smile angle, and dental show (both P < 0.05).
Table 4.
EMOTRICS15 Photogrammetric Outcomes
| Pose | Measurement | Overall (n = 25) | ||
|---|---|---|---|---|
| Preoperative Difference (mm or ° for Smile Angle) | Postoperative Difference (mm or ° for Smile Angle) | P | ||
| Repose (n = 24) | Commissure height | 4.2 ± 3.9 | 3.6 ± 3.4 | 0.48* |
| Upper lip height | 4.3 ± 3.3 | 4.0 ± 3.2 | 0.39* | |
| Lower lip height | 2.2 ± 1.0 | 2.5 ± 1.8 | 0.29* | |
| Open-lip smile (n = 22) | Commissure height | 2.4 ± 0.9 | 2.6 ± 1.6 | 0.59* |
| Smile angle | 3.3 ± 2.0 | 4.5 ± 3.3 | 0.19* | |
| Lower lip height | 3.9 ± 3.1 | 2.5 ± 2.3 | <0.05* | |
| Dental show | 6.0 ± 4.7 | 4.5 ± 3.5 | 0.08* | |
| Lower lip depression (n =11) | Smile angle | 8.6 ± 5.9 | 4.9 ± 4.3 | 0.16* |
| Lower lip height | 5.3 ± 3.5 | 2.4 ± 1.9 | <0.05* | |
| Dental show | 2.5 ± 2.3 | 2.0 ± 3.0 | 0.29* | |
*Wilcoxon signed rank test.
Discussion
Lower Lip Reanimation
Lower lip depression was a neglected target in facial palsy surgery but several surgical options now exist.4,9 As smile restoration improves, attention is turning toward the lower lip to optimize results. Semi-dynamic reanimation can be restored with bidirectional fascia grafting16 and dynamic reanimation with nerve transfers from the hypoglossal nerve to the cervicofacial branch, or neurotization of viable depressors directly or via CFNG.4,8,14
If paralysis is longstanding, with no residual depressor function, muscle transfers are indicated. These can be local (ABDM, platysma) or microsurgical free muscle transfers (platysma, extensor digitorum brevis, serratus anterior, rectus femoris).4,6,17 These procedures, with minimal donor cost,18 can be effective ways to enhance oral movements following smile reanimation surgery. Two-stage extensor digitorum brevis transfer was found to be problematic by Tulley et al6 due to the duration of procedure (requires microsurgical anastomosis as it is a free muscle transfer) and unreliable results; they preferred the local ABDM option, which was performed as a single-stage procedure.6
The one-stage ABDM transfer has been utilized for some time and Conley found it “effective” in all of their 36 cases, with 3 minor complications.2 Tan gained satisfactory results in 14 single-stage ABDM transfers and noted dynamic improvement despite no physiotherapy regime, inferring the trigeminal nerve functioned well following transfer.10 Butler et al found similarly high satisfaction comparing ABDM transfer with botulinum toxin; ABDM having the advantage of longevity.7 The only other series of 2-stage reanimations was by Terzis and Kalantarian4 (discussed below).
Outcomes
These data present the largest series of 2-stage lower lip reanimation cases to date. Both nonmedical and medical raters felt the procedures improved patients’ appearance as shown by improvements in Terzis scores. This is in keeping with Terzis’ results,4 in which 16 of 22 ABDM reanimations were 2-stage. Interestingly, although raters in Terzis’ series scored patients undergoing platysma transfer higher than ABDM ones, the platysma group had a higher preoperative score and so the degree of improvement was actually similar for both groups (mean scores 0.18–1.45 of 2 (+1.27) for ABDM and 0.44–1.61 (+1.17) for platysma.
The senior author’s technique is similar to Terzis’ with some personalizations. Differences include using 2 rather than 4 tendon slips as 3 or more became flimsy and risked avulsion. Also, the mandibular attachment of the ABDM was left intact, rather than divided and lateralized for averting potential risk of avulsing the vascular pedicle.
These results were corroborated by objective data from Emotrics15 also showing some improvements in lower lip symmetry. Both lower lip measures (height and dental show) improved during animation but not at rest. This is to be expected as lower lip asymmetry becomes apparent during animation. Although, some of the improvements did not reach statistical significance, the Terzis scale data show that these improvements were clinically apparent. Due to the small excursions of the lower lip, statistical significance requires larger sample sizes. The authors believe that the peer-reviewed and objective results should be analyzed together as they assess subtly different aspects. This is important since although people notice asymmetry, they do not compute it in numbers as per Emotrics15 but may form a view like the independent raters.
Complications and Revisions
The complication and revision profile was acceptable. Five patients required minor aesthetic revisions like lipofilling to correct lip notching (Fig. 7). The senior author now prevents this by overcorrecting the medial tendon attachment to the lower lip and suturing the tendon to the orbicularis substance away from the lip mucosa. Excessive vermillion border bulk, as reported by Lindsay et al in their four ABDM transfers,5 was not found. Patients are counseled about the possibility of inadequate ABDM length and fascia lata extensions. Ultrasound may be advisable especially in hemifacial microsomia whose ABDM may be absent or hypoplastic.6,19,20
Limitations and Remediations
Limitations include retrospectivity of the analysis and a low number of complete sets for the eversion pose for the photogrammetry. This was fed back to the medical photographers to improve the fidelity of our records, as it affected significance calculations. Further, there were insufficient numbers of single-stage reanimations, which KT reserves for the comorbid or physiologically aged, to compare the 2 approaches.
However, several features improve the quality of this study. Using 21 observers, more than all other studies, reduced the impact of interobserver variability. Since there are no perfect facial palsy outcome assessment tools,21 the authors used the unambiguous, lower lip-specific, and validated Terzis’ scale, which can also be used by nonmedical observers.
Observers were specifically briefed to grade only lower lip movement and to ignore any other features of facial paralysis or surgery. That those with isolated MMB palsy improved more than those with more extensive paralysis may be due to better results, or maybe raters had a subconscious tendency to downgrade the patients with more extensive facial palsy, even if lower lip results were good.
Conclusions
These results show the safety and efficacy of 2-stage lower lip reanimation using ABDM transposition. Depressor reanimation is both desirable and achievable following MMB paralysis. Two-stage ABDM transfer was preferred in patients with longstanding MMB paralysis to reconstruct spontaneous, symmetrical, and emotional movement. The authors hope these results encourage other surgeons to learn and offer this effective lower lip reanimation method.
Supplementary Material
Footnotes
Published online 15 March 2021.
Drs. Tzafetta and Ruston contributed equally to this work.
Presented at 13th International Facial Nerve Symposium, August 2017, Los Angeles; 14th Congress of European Federation of Societies for Microsurgery, May 2018, Belgrade; ESPRAS, October 2018, Cyprus; BAPRAS Winter Meeting, November 2018, London; ASRM, February 2019, Palm Desert, Calif.; WSRM, June 2019, Bologna; BAPRAS Winter Meeting, December 2020, London.
Disclosure: The authors have no financial interests to declare in relation to the content of this article. No funding was received for this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
The study had Departmental approval (CA17 067) and conforms to principles stated in the Helsinki Declaration.
References
- 1.Su P, Ishii LE, Joseph A, et al. Societal value of surgery for facial reanimation. JAMA Facial Plast Surg. 2017; 19:139–146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Conley J, Baker DC, Selfe RW. Paralysis of the mandibular branch of the facial nerve. Plast Reconstr Surg. 1982; 70:569–577 [DOI] [PubMed] [Google Scholar]
- 3.Lin JT, Lu JC, Chang TN, et al. Simultaneous reconstruction of the lower lip with gracilis functioning free muscle transplantation for facial reanimation: comparison of different techniques. Plast Reconstr Surg. 2018; 142:1307–1317 [DOI] [PubMed] [Google Scholar]
- 4.Terzis JK, Kalantarian B. Microsurgical strategies in 74 patients for restoration of dynamic depressor muscle mechanism: a neglected target in facial reanimation. Plast Reconstr Surg. 2000; 105:1917–1931 [DOI] [PubMed] [Google Scholar]
- 5.Lindsay RW, Edwards C, Smitson C, et al. A systematic algorithm for the management of lower lip asymmetry. Am J Otolaryngol. 2011; 32:1–7 [DOI] [PubMed] [Google Scholar]
- 6.Tulley P, Webb A, Chana JS, et al. Paralysis of the marginal mandibular branch of the facial nerve: treatment options. Br J Plast Surg. 2000; 53:378–385 [DOI] [PubMed] [Google Scholar]
- 7.Butler DP, Leckenby JI, Miranda BH, et al. Botulinum toxin therapy versus anterior belly of digastric transfer in the management of marginal mandibular branch of the facial nerve palsy: a patient satisfaction survey. Arch Plast Surg. 2015; 42:735–740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Terzis JK, Tzafetta K. The “babysitter” procedure: minihypoglossal to facial nerve transfer and cross-facial nerve grafting. Plast Reconstr Surg. 2009; 123:865–876 [DOI] [PubMed] [Google Scholar]
- 9.Edgerton MT. Surgical correction of facial paralysis: a plea for better reconstructions. Ann Surg. 1967; 165:985–998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tan ST. Anterior belly of digastric muscle transfer: a useful technique in head and neck surgery. Head Neck. 2002; 24:947–954 [DOI] [PubMed] [Google Scholar]
- 11.Aszmann OC, Ebmer JM, Dellon AL. The anatomic basis for the innervated mylohyoid/digastric flap in facial reanimation. Plast Reconstr Surg. 1998; 102:369–372 [DOI] [PubMed] [Google Scholar]
- 12.Terzis JK, Tzafetta K. Essays on the facial nerve: part I. microanatomy. Plast Reconst Surg. 2010; 125:879–889 [DOI] [PubMed] [Google Scholar]
- 13.Touré G, Tran de Fremicourt MK, Randriamanantena T, et al. Vascular and nerve relations of the marginal mandibular nerve of the face: anatomy and clinical relevance. Plast Reconstr Surg. 2019; 143:888–899 [DOI] [PubMed] [Google Scholar]
- 14.Terzis JK, Tzafetta K. Outcomes of mini-hypoglossal nerve transfer and direct muscle neurotization for restoration of lower lip function in facial palsy. Plast Reconstr Surg. 2009; 124:1891–1904 [DOI] [PubMed] [Google Scholar]
- 15.Guarin DL, Dusseldorp J, Hadlock TA, et al. A machine learning approach for automated facial measurements in facial palsy. JAMA Facial Plast Surg. 2018; 20:335–337 [DOI] [PubMed] [Google Scholar]
- 16.Watanabe Y, Sasaki R, Agawa K, et al. Bidirectional/double fascia grafting for simple and semi-dynamic reconstruction of lower lip deformity in facial palsy. J Plast Reconst Aesthet Surg. 2015; 68:321–328 [DOI] [PubMed] [Google Scholar]
- 17.Terzis JK, Tzafetta K. “Babysitter” procedure with concomitant muscle transfer in facial paralysis. Plast Reconstr Surg. 2009; 124:1142–1156 [DOI] [PubMed] [Google Scholar]
- 18.Rainer C, Schoeller T, Bauer T, et al. The anatomic basis for the innervated mylohyoid/digastric flap in facial reanimation. Plast Reconstr Surg. 1999; 103:1798. [DOI] [PubMed] [Google Scholar]
- 19.MacQuillan A, Biarda FU, Grobbelaar A. The incidence of anterior belly of digastric agenesis in patients with hemifacial microsomia. Plast Reconstr Surg. 2010; 126:1285–1290 [DOI] [PubMed] [Google Scholar]
- 20.Liquidate BM, Barros MD, Alves AL, et al. Anatomical study of the digastric muscle: variation in the anterior belly. Intern J Morphol. 2007; 25:797–800 [Google Scholar]
- 21.Niziol R, Henry FP, Leckenby JI, et al. Is there an ideal outcome scoring system for facial reanimation surgery? A review of current methods and suggestions for future publications. J Plast Reconstr Aesthet Surg. 2015; 68:447–456 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


