Abstract
BACKGROUND AND PURPOSE:
Flow diversion with the Pipeline Embolization Device has emerged as an attractive treatment for cerebral aneurysms. Processes involved in aneurysm occlusion include changes in intra-aneurysmal hemodynamics and endothelialization of the device. Here, we call attention to a radiographic sign not previously reported that is detected in incompletely occluded aneurysms after treatment with the Pipeline Embolization Device at angiographic follow-up and referred to as the “collar sign.”
MATERIALS AND METHODS:
A retrospective review of all patients who underwent placement of a Pipeline Embolization Device for cerebral aneurysms between January 2014 and May 2016 was performed. All aneurysms found to show the collar sign at follow-up were included. Optical coherence tomography was performed in 1 case.
RESULTS:
One hundred thirty-five aneurysms were treated in 115 patients. At angiographic follow-up, 17 (10.7%) aneurysms were found to be incompletely occluded. Ten (58.8%) of these aneurysms (average diameter, 7.9 ± 5.0 mm) were found to have the collar sign at angiographic follow-up (average, 5.5 ± 1.0 months). Four (40.0%) of the aneurysms underwent a second angiographic follow-up (average, 11.0 ± 0.9 months) after treatment, and again were incompletely occluded and showing the collar sign. Two patients underwent retreatment with a second Pipeline Embolization Device. Optical coherence tomography showed great variability of endothelialization at the proximal end of the Pipeline Embolization Device.
CONCLUSIONS:
The collar sign appears to be indicative of endothelialization, but continued blood flow into the aneurysm. This is unusual given the processes involved in aneurysm occlusion after placement of the Pipeline Embolization Device and has not been previously reported.
Flow diversion with the Pipeline Embolization Device (PED; Covidien, Irvine, California) has emerged as an attractive treatment option for cerebral aneurysms, resulting in 6-month occlusion rates higher than 90%.1–3 Serving as a scaffold for endothelialization, the PED is believed to divert blood flow away from the aneurysm, inducing thrombosis and collagenization within its sac.4 The relative contribution of the 2 processes, namely endothelialization and blood stasis followed by clot formation, in leading to aneurysm occlusion and shrinkage remains poorly understood. However, visualization of complete obliteration of the lesion via DSA is believed to coincide with endothelialization across the neck of the lesion. Here, we report on a series of incompletely occluded aneurysms after PED placement where a gap in contrast opacification between parent vessel and aneurysm dome, or “collar sign,” was observed upon angiographic follow-up. Optical coherence tomography (OCT) was performed in 1 case.
Materials and Methods
After obtaining institutional review board approval, a retrospective review of all patients who underwent flow-diversion treatment for intracranial aneurysms with the PED at our institution between January 2014 and May 2016 was performed. All aneurysms were followed up with DSA, generally at 6 months after PED placement, by using standard anteroposterior and lateral projections and high-magnification views. Injections were performed from the ICA in all cases. All aneurysms found to show the collar sign at angiographic follow-up were included. Follow-up images were reviewed by at least 2 physicians with subspecialty training in neuroendovascular surgery.
Optical Coherence Tomography Procedure
OCT was performed in 1 case (case 10). A 6F guide catheter was placed in the right ICA. Baseline intracranial angiograms were obtained and 5000 U of IV heparin were administered. A Navien intracranial support catheter (Covidien) was positioned in the cavernous ICA. A 0.014-inch Synchro Standard microwire (Stryker Neurovascular, Kalamazoo, Michigan) was advanced through the Navien, past the aneurysm, and positioned in the MCA. Next, a 2.7F Dragonfly OCT imaging catheter (St. Jude Medical, St. Paul, Minnesota) was advanced over the microwire. Attempts to negotiate the carotid siphon past the aneurysm with the Dragonfly OCT catheter failed. These attempts included alternative distal access catheters and stiffer microwires, such as the 0.014-inch Transend (Stryker Neurovascular). After several attempts, there was profound spasm in the ICA, and the decision was made to only perform OCT of the proximal end of the PED in the horizontal segment of the cavernous ICA. The guide catheter was connected to a power injector. An OCT acquisition over 2.7 seconds was done during power injection of contrast to trigger the internalized automated “pull-back” method that renders catheter manipulation unnecessary during image acquisition and to transiently clear red blood cells from the imaging area.5,6 Image processing and data analysis were done using a commercially available OCT system (Ilumien System; St. Jude Medical).
Results
A total of 135 aneurysms were treated at our institution with PEDs in 115 patients between January 2014 and May 2016. Ninety of these aneurysms (66.7%) underwent angiographic follow-up, at which point 73 (81.1%) were found to be completely occluded and 5 (5.6%) were >90% occluded. Of 17 aneurysms that were incompletely occluded, 10 (58.8%) aneurysms (average diameter, 7.9 ± 5.0 mm) in 9 patients (average age, 54.2 ± 14.5 years) were found to have a collar sign with variable thickness at first angiographic follow-up (average, 5.5 ± 1.0 months). Two aneurysms underwent retreatment with a second PED device. Seven (70.0%) aneurysms were paraophthalmic ICA aneurysms, but the collar sign was also observed in MCA, ICA bifurcation, and posterior communicating artery aneurysms (1 aneurysm each). No procedural complications occurred. Satisfactory wall apposition as demonstrated on fluoroscopy was achieved in all cases. Four (40.0%) of the aneurysms underwent a second angiographic follow-up (average, 11.0 ± 0.9 months) after treatment, and again were incompletely occluded showing the collar sign (Fig 1). Opacification of parent vessel and aneurysm occurred simultaneously with injection of the ICA, reducing the possibility for retrograde aneurysm filling via external carotid artery or other collaterals. The collar sign was observed were in both clopidogrel responders and nonresponders treated with ticagrelor (On-line Table).
Fig 1.
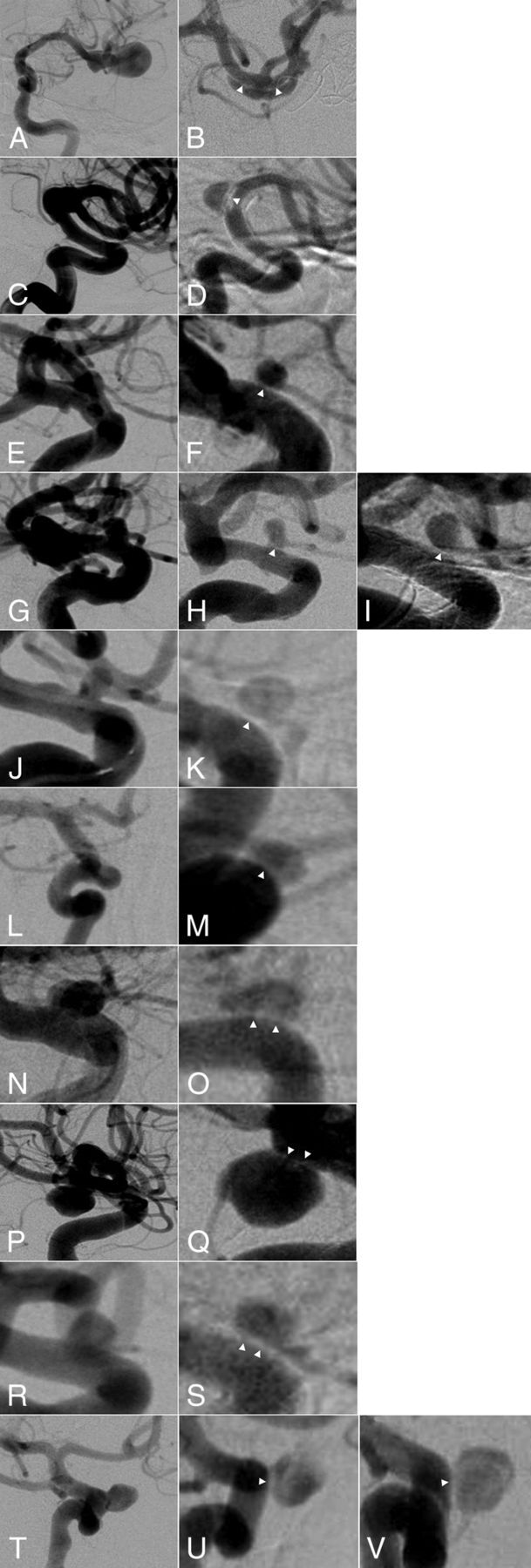
DSA showing collar sign in incompletely occluded aneurysms after Pipeline embolization. Each line represents 1 aneurysm corresponding to the On-line Table. The left column shows the aneurysm before Pipeline embolization. The right column shows the residual aneurysm with the collar sign (white arrowheads) after Pipeline placement at last follow-up. For aneurysms 4 and 10, both first and second angiographic follow-up are shown.
Optical Coherence Tomography Findings
Because of inability to negotiate the carotid siphon with the OCT catheter past the aneurysm, only the proximal end of the PED in the horizontal segment of the cavernous ICA could be imaged with OCT (Fig 2). Interestingly, there was great variability of endothelialization of the PED. There were portions where the PED struts laid bare or were covered by thin endothelium or robust neointima. The degree of endothelialization was even variable on the same cross-section.
Fig 2.
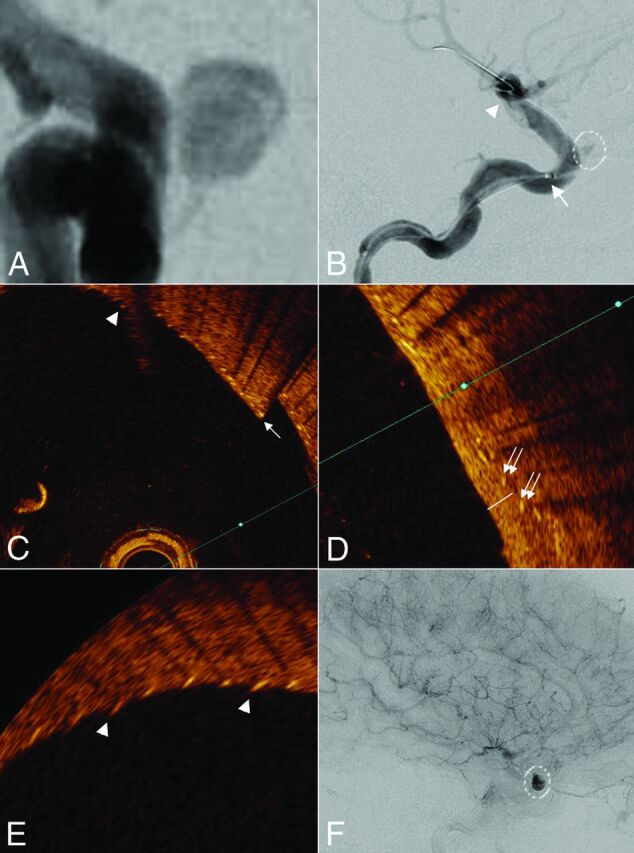
Case 10. DSA showing collar sign in incompletely occluded paraophthalmic ICA aneurysm after Pipeline embolization (A). Lateral DSA of the ICA showing the aneurysm (white dashed line) and position of the tip (arrowhead) and the beginning of the scanning portion (arrow) of the OCT catheter (B). OCT images showing variable degree of endothelialization (C–E). There are portions where the PED struts lay bare (arrowheads) or are covered with thin endothelium (arrow) or robust neointima (double arrow and white line showing the distance from lumen to PED struts). After treatment with a second PED, there is stasis of contrast within the aneurysm (F).
Discussion
Here, we report on a series of patients with incompletely occluded cerebral aneurysms after PED placement where the parent vessel appeared to be separate from the aneurysm on angiographic follow-up. We decided to use the term “collar sign” to describe this observation. The main purpose of this article was to report this interesting observation and spark discussion among neurointerventionalists about its significance.
Potential Mechanisms Underlying the Collar Sign
Given the contiguous nature of this sign with the endothelial lining of the parent vessel, it appears to represent endothelialization on the surface of the stent adjacent to the neck of the aneurysm. Why there is continued blood flow into the aneurysm, however, is unclear. Small channels, not readily apparent on DSA, must remain, connecting the parent vessel with the aneurysm. It has been postulated that endothelialization, rather than intra-aneurysmal hemodynamic changes, are primarily responsible for aneurysm obliteration after PED placement. After performing immunohistochemical analysis in rabbit models, Kadirvel et al7 found that endothelial cells derived from the parent vessel rather than from progenitor cells from the bone marrow are responsible for neointimal growth after flow-diverter placement, supporting previous results in mice models. They further found that smooth muscle cells derived from the parent vessel and the aneurysm itself also served as the scaffold for neointimal formation. The presence of inflammatory cells, including macrophages and monocytes, within the portion of the device covering the aneurysm neck was observed in cases of incomplete obliteration and was associated with disorganized thrombus formation at 8 weeks after flow-diverter placement. The macrophages and monocytes formed islands at the neck of the aneurysms without associated endothelial, smooth muscle, and progenitor cells. Similar processes may, in part, be responsible for the collar sign observed on follow-up DSA in humans, and it may represent an angiographic correlate for inflammatory-driven aberrant endothelialization. Along the same lines, Dai et al8 reported a case of a patient who underwent PED placement for a basilar tip aneurysm. At 4 months, the aneurysm was occluded, but at 1 year, it had recanalized, and the patient died from brain stem compression. Microscopic analysis of the aneurysm revealed channels extending through thick, newly formed islands of intima from the parent vessel to the sac of the aneurysm containing fresh blood clot. The aneurysm was filled with disorganized thrombus. The collar sign on the DSAs obtained in the present series of patients were mostly homogeneous in appearance with variable thickness, even though they contained rare regions speckled with contrast, indicative of blood flow through this layer. OCT performed in 1 case showed variable degrees of endothelialization at the proximal end of the PED, ranging from no coverage of the PED struts to thick neointima. Unfortunately, the area of the collar sign could not be imaged because of inability to negotiate the carotid siphon with the OCT catheter. In animal models, OCT has been used to assess PED wall apposition9 and side branches covered by the PED.10,11 We are not aware of any prior use of OCT after PED placement in humans.
Clinical Implications of the Collar Sign
The implications of the collar sign are unclear. Initially, we assumed that incompletely occluded aneurysms with this associated sign at 6 months would likely be occluded at subsequent follow-up. However, all patients who had additional angiographic follow-up past the 6-month mark continued to have aneurysm filling, with no notable change in the collar sign appearance. Given that flow diversion is associated with high rates of complete occlusion at 6-month follow-up,2,12–14 these aneurysms only represent a small fraction of all aneurysms treated with the PED. Nevertheless, it is important to consider. If the collar sign at 6 months is not predictive of occlusion in the future, early treatment with a second PED may be warranted. In the current series, this approach was pursued in 2 aneurysms, with close follow-up on the others.
Conclusions
Pipeline embolization is associated with high rates of occlusion of cerebral aneurysms. Two mechanisms underlying occlusion have been proposed for the device: 1) diversion of blood flow away from the fundus of the lesion, resulting in subsequent thrombus formation and aneurysm shrinkage; and 2) endothelialization of the neck of the aneurysm over time. Here, we report on a series of patients who underwent PED placement and were found to have incomplete occlusion of their aneurysms at angiographic follow-up, with a characteristic collar sign visible on angiography. They appear to represent endothelialization along the neck of the aneurysm with continued filling of the lesions. Subsequent follow-ups in a subset of these patients demonstrated residual blood flow into these aneurysms and continued incomplete endothelialization across the neck, warranting retreatment.
Supplementary Material
ABBREVIATIONS:
- OCT
optical coherence tomography
- PED
Pipeline Embolization Device
Footnotes
Disclosures: Ajith Thomas—UNRELATED: Consultancy: Stryker, Comments: data safety monitoring board of SCENT trial*; Expert Testimony: testimony related to aneurysm treatment. *Money paid to the institution.
References
- 1. Alderazi YJ, Shastri D, Kass-Hout T, et al. Flow diverters for intracranial aneurysms. Stroke Res Treat 2014;2014:415653 10.1155/2014/415653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Szikora I, Berentei Z, Kulcsar Z, et al. Treatment of intracranial aneurysms by functional reconstruction of the parent artery: the Budapest experience with the Pipeline embolization device. AJNR Am J Neuroradiol 2010;31:1139–47 10.3174/ajnr.A2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Griessenauer CJ, Ogilvy CS, Foreman PM, et al. Pipeline Embolization Device for small paraophthalmic artery aneurysms with an emphasis on the anatomical relationship of ophthalmic artery origin and aneurysm. J Neurosurg 2016. March 4:1–8. [Epub ahead of print] 10.3171/2015.12.JNS152499 [DOI] [PubMed] [Google Scholar]
- 4. D'Urso PI, Lanzino G, Cloft HJ, et al. Flow diversion for intracranial aneurysms: a review. Stroke 2011;42:2363–68 10.1161/STROKEAHA.111.620328 [DOI] [PubMed] [Google Scholar]
- 5. Attizzani GF, Jones MR, Given CA 2nd, et al. Frequency-domain optical coherence tomography assessment of very late vascular response after carotid stent implantation. J Vasc Surg 2013;58:201–04 10.1016/j.jvs.2012.11.038 [DOI] [PubMed] [Google Scholar]
- 6. Griessenauer CJ, Foreman PM, Deveikis JP, et al. Optical coherence tomography of traumatic aneurysms of the internal carotid artery: report of 2 cases. J Neurosurg 2016;124:305–09 10.3171/2015.1.JNS142840 [DOI] [PubMed] [Google Scholar]
- 7. Kadirvel R, Ding YH, Dai D, et al. Cellular mechanisms of aneurysm occlusion after treatment with a flow diverter. Radiology 2014;270:394–99 10.1148/radiol.13130796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dai D, Ding YH, Kelly M, et al. Histopathological findings following Pipeline embolization in a human cerebral aneurysm at the basilar tip. Interv Neuroradiol 2016;22:153–57 10.1177/1591019915622165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. van der Marel K, Gounis MJ, Weaver JP, et al. Grading of Regional Apposition after Flow-Diverter Treatment (GRAFT): a comparative evaluation of VasoCT and intravascular OCT. J Neurointerv Surg 2016;8:847–52 10.1136/neurintsurg-2015-011843 [DOI] [PubMed] [Google Scholar]
- 10. Iosif C, Saleme S, Ponsonnard S, et al. Intravascular optical coherence tomography for the evaluation of arterial bifurcations covered by flow diverters. J Neurointerv Surg 2016. January 27. [Epub ahead of print] 10.1136/neurintsurg-2015-012084 [DOI] [PubMed] [Google Scholar]
- 11. Lopes DK, Johnson AK. Evaluation of cerebral artery perforators and the Pipeline embolization device using optical coherence tomography. J Neurointerv Surg 2012;4:291–94 10.1136/neurintsurg-2011-010102 [DOI] [PubMed] [Google Scholar]
- 12. Kan P, Siddiqui AH, Veznedaroglu E, et al. Early postmarket results after treatment of intracranial aneurysms with the Pipeline embolization device: a U.S. multicenter experience. Neurosurgery 2012;71:1080–87, discussion 1087–88 10.1227/NEU.0b013e31827060d9 [DOI] [PubMed] [Google Scholar]
- 13. O'Kelly CJ, Spears J, Chow M, et al. Canadian experience with the Pipeline embolization device for repair of unruptured intracranial aneurysms. AJNR Am J Neuroradiol 2013;34:381–87 10.3174/ajnr.A3224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yu SC, Kwok CK, Cheng PW, et al. Intracranial aneurysms: midterm outcome of Pipeline embolization device–a prospective study in 143 patients with 178 aneurysms. Radiology 2012;265:893–901 10.1148/radiol.12120422 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


