Abstract
BACKGROUND AND PURPOSE:
TS analysis has been suggested as a useful method to evaluate the fiber integrity of white matter tracts. This study investigated the intrarater and interrater reliability and validity of a TS analysis for the CST and compared the results with those of a ROI-based analysis.
MATERIALS AND METHODS:
Diffusion spectrum imaging was performed on 7 patients with subcortical ischemic stroke on a 3T MR imaging system. For the TS analysis, seed regions were placed at the cerebral peduncle and the medial portion of the primary motor cortex to reconstruct the tracts of the CST for motor control of the lower extremity. The mean GFA was measured at the PLIC by calculating the weighted sum of the GFAs sampled by the CST tracts at this segment. For the ROI-based analysis, the posterior two-thirds of the PLIC were enclosed on the GFA maps, and the mean GFA in this ROI was calculated.
RESULTS:
The results showed good-to-excellent intrarater and interrater reliability on the seed region/ROI placement (mean κ values >0.80) and mean GFA values (ICCs >0.90) for both the TS and ROI-based analyses. Both the GFAPLIC-TS and GFAPLIC-ROI values were highly correlated with the motor function of the affected lower extremity (r = 0.76 and 0.80, respectively; P < .05).
CONCLUSIONS:
We demonstrated good reliability and validity of the TS and ROI-based analyses of the CST corresponding to lower extremity motor control in patients with subcortical ischemic stroke.
Using MR DTI to assess the integrity of white matter tracts in patients with stroke is potentially valuable to correlate the motor impairments and to predict functional outcomes.1,2 It has been reported that FA, which is a quantitative index of the directional anisotropy of water molecular diffusion derived from the diffusion tensor, is an effective measure of fiber integrity.3 Decreases in FA have been found in the affected tracts at infarct regions and regions with wallerian degeneration.1,4,5 Knowledge about tract integrity after stroke may allow for both the accurate stratification of functional recovery and the planning of effective customized rehabilitation programs for individual patients.
Most studies have used ROI-based analysis of FA maps to detect white matter changes in patients with stroke.2,6,7 Using ROI-based analysis, researchers manually select certain white matter regions with the aid of anatomic landmarks. This approach depends on raters' familiarity with the brain anatomy and is thus subject to poor interrater and intrarater reproducibility.8 Recently, several studies have suggested that TS analysis may be more objective, specific,9–11 and reliable11,12 than ROI-based analysis to evaluate the integrity of white matter fibers. The TS analysis method uses diffusion tractography as a guide to quantify the FA of a specific fiber tract bundle.9,11,13–16 Compared with ROI-based analysis, TS analysis has the advantage of exploring the fiber integrity anywhere along a tract of interest, and thus, it is not limited to regions identifiable by anatomic landmarks.
Performing tractography of a long tract bundle such as the CST often encounters interruption of the tracts in patients with stroke.17–19 This is because the FA values tend to decrease, and the tensor orientations become disorganized in the infarct location and its surroundings. The tracking procedure of the tractography algorithm would come to a halt when the FA value or proceeding angle does not pass a default threshold. Even if the tractography is not interrupted, it is still difficult to obtain a minor branch of a tract bundle from the tractography because the tensor orientation is predominantly pointing toward the orientation of the major branches. Analysis of our unpublished laboratory data supported that these difficulties pose a great challenge to TS analysis of the CST if a minor branch, such as that corresponding to the lower extremity motor control originated from M1, is to be assessed. In this study, we used DSI to address these problems.20,21 DSI entails the acquisition of >200 diffusion-weighted images over the whole brain, where each diffusion weighting corresponds to a specific encoding point in the q-space. DSI tractography has been demonstrated to differentiate the CST from other crossing fiber tracts, including the corpus callosum, superior longitudinal fasciculus, and middle cerebellar peduncle, and it has been shown to separate the branches arising from different cortical areas responsible for the movement of different body parts.22,23
Previous studies have investigated the reproducibility of TS analysis in patients with amyotrophic lateral sclerosis and in premature infants.9,11 The same studies in patients with stroke are still lacking. Although there have been many studies by using ROI-based analysis to reveal the correlation between the FA and motor function in patients with stroke,1,2,4,24,25 such functional correlation studies by using the TS quantitative analysis have not yet been established. As for diffusion tensor tractography, only a qualitative analysis of the CST has been performed to relate the degrees of tract interruption and functional outcomes.17–19,26,27
Therefore, the goal of this study was to establish the reliability and validity of the TS analysis method. We acquired DSI data from patients with subcortical ischemic stroke, reconstructed the whole CST originating from the M1 region corresponding to the lower extremity motor control, and quantified the GFA at the segments covering the PLIC. The purpose of this study was 2-fold. First, we investigated the reliability of TS analysis of the CST or, more specifically, the intrarater and interrater reliability of the GFA values. Second, we tested the validity of the TS analysis by correlating the GFA values with the clinical motor function scores of the affected lower limbs. In this study, the performance of the ROI-based analysis was also evaluated and compared with the TS analysis.
Materials and Methods
Subjects
Patients with stroke were recruited from the stroke registry of the Neurology Department at the National Taiwan University Hospital. The inclusion criteria of the patients to participate in this research were the following: 1) having first-ever ischemic stroke based on clinical imaging reports and physician diagnosis; 2) presenting subcortical stroke with unilateral hemiplegia or hemiparesis; 3) showing mild-to-moderate severity of stroke, corresponding to the NIHSS ≤1528; 4) being between 40 and 80 years old; and 5) having no contraindications for MR scanning, such as an electrical device implanted in the body or claustrophobia. Patients were excluded if they had cortical stroke, unstable medical conditions, impaired cognitive function, or were unable to communicate. All participants signed an informed consent form approved by the institutional review board.
We evaluated the function of cognition with the MMSE.29 Impairment in sensation, range of motion, and motor function of the affected lower extremity were evaluated by using the FMA-LE.30 We used Manual Muscle Testing31 to check whether there was any muscle weakness of the unaffected lower extremity. The reliability and validity of these clinical assessments have been established.32–34
Seven patients with subcortical ischemic stroke participated in this study (4 men and 3 women; mean age, 59.2 ± 7.9 years; 5 with right subcortical lesions and 2 with left subcortical lesions). The 7 subjects were all right-handed and right-footed before their stroke episode. All of them showed early (within 3 days of onset) NIHSS scores ranging from 2 to 8, indicating mild to moderate stroke in the acute stage (Table 1). All patients had normal cognitive function (MMSE >24, out of a total of 30) and intact sensory function of the affected lower extremities (FMA-LE sensory score of 24, out of a total of 24). One participant had moderate range of motion limitation at the hip and ankle joints of the affected lower extremity. The FMA-LE motor score of the affected lower extremities of the subjects ranged from 12 to 34 (out of a total of 34), indicating mild-to-moderate residual motor impairment (Table 1). All of the patients underwent MR imaging scanning ∼90 days (93.6 ± 5.9 days) after stroke onset.
Table 1:
Demographics of stroke subjects
| Subject | Sex | Age | Handedness | Footedness | Lesion Location | NIHSS (42) | Post-Onset Days | FMA-LE Sensation (24) | FMA-LE Range of Motion (22) | FMA-LE Motor (34) | MMSE (30) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 59.2 | R | R | R corona radiata | 7 | 89 | 24 | 15 | 12 | 29 |
| 2 | F | 66.1 | R | R | R BG, PLIC | 5 | 99 | 24 | 22 | 34 | 28 |
| 3 | M | 49.3 | R | R | L thalamus | 8 | 102 | 24 | 22 | 28 | 29 |
| 4 | F | 65.4 | R | R | R corona radiata | 4 | 87 | 24 | 22 | 34 | 25 |
| 5 | F | 69.0 | R | R | R corona radiata | 5 | 89 | 24 | 22 | 34 | 26 |
| 6 | M | 54.6 | R | R | L thalamus, PLIC | 7 | 98 | 24 | 22 | 28 | 30 |
| 7 | M | 50.7 | R | R | R corona radiata | 2 | 91 | 24 | 22 | 34 | 30 |
| Mean | 59.2 | 93.6 | 24.0 | 21.0 | 29.1 | 28.1 | |||||
| SD | 7.9 | 5.9 | 0.0 | 2.7 | 8.1 | 1.9 |
Note:—Numbers in parentheses indicate the highest possible score of the assessments.
MR Data Acquisition
Patients were scanned on a 3T MR imaging system (Magnetom Trio; Siemens, Erlangen, Germany) with an 8-channel phased-array head coil. Head movement was restricted with expandable foam cushions. An axial plane parallel to the anterior/posterior commissure line was determined for the section orientation of both the subsequent structural MR imaging and the DSI scans. To provide an anatomic reference, a T2-weighted fast spin-echo sequence was performed with 35 contiguous axial sections covering the whole brain (TR/TE = 5290/102 ms, flip angle = 150°, FOV = 250 × 250 mm2, matrix = 256 × 256, section thickness = 3.9 mm). The DSI data were acquired by using a pulsed gradient twice-refocused spin-echo echo-planar imaging sequence.35 In this study, 203 diffusion gradient vectors were applied, each corresponding to one of the isotropic 3D grid points in the q-space.36 The maximum diffusion gradient was equivalent to the maximum diffusion sensitivity (bmax) of 6000 s/mm2. The DSI data were obtained at 2.9 × 2.9 × 2.9 mm3 isotropic resolution (TR/TE = 9100/142 ms, flip angle = 90°, FOV = 370 × 370 mm2, matrix = 128 × 128, section thickness = 2.9 mm). As a result, a total of 203 diffusion-weighted brain volumes were acquired, where each volume consisted of 45 transaxial sections encompassing the whole brain. We used a standard procedure to stabilize the head and body of the participants during the scanning to minimize the problem of head motion. The total scan time was ∼45 minutes for each participant. All participants were able to tolerate the whole scanning section.
MR Data Analysis
Two raters (Z.-A.L. and Y.-H.K.), who are licensed physical therapists specialized in neurologic physical therapy and had had 2 years of intensive training on MR data acquisition and analysis, were first trained by the set of analysis guidelines described below. The relatively fair spatial resolution of the GFA maps on which the seed region/ROI areas were selected may also affect the reliability of the seed region/ROI placement. To ameliorate this potential problem, the raters used the subjects' T2-weighted structure images to guide the identification of anatomic landmarks on the GFA maps.
TS Quantitative Analysis
Having acquired the DSI data, the probability attenuation function at each pixel was reconstructed by performing a Fourier transform of the signal intensity in the q-space. The orientation distribution function was then calculated by using the second moments of the probability attenuation function in different radial directions.20 The GFA,37 a quantitative index derived from the orientation distribution function to indicate diffusion anisotropy, was calculated at each pixel. The fiber vectors at each pixel were also defined by selecting the peak orientations of the orientation distribution function.23
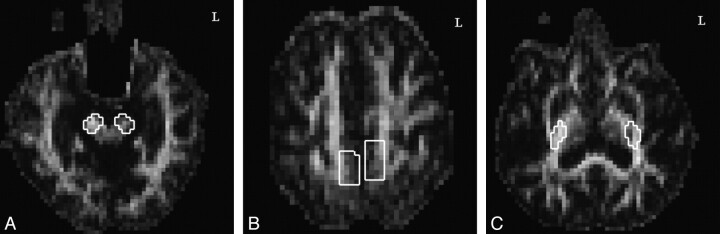
The reconstruction of the CST tractography was performed by a modified streamline method22 by using the in-house software DSI Studio (http://sites.google.com/a/labsolver.org/dsi-studio/). The seed points for initiating the fiber tracking were placed at 2 seed regions: the CP at the midbrain level (Fig 1A) and the M1 (Fig 1B). The CST corresponding to motor control of the lower extremity was obtained by tracking through the 2 seed regions. The selection of the seed region at the CP was outlined by choosing the 2 sections containing the CP at the midbrain and then enclosing the pixels containing the CP area. The seed region at the lower extremity region of the precentral gyrus was defined as follows. First, from the vertex downward, we selected the first 4 sections that allowed clear identification of the precentral sulcus, precentral gyrus, central sulcus, and postcentral gyrus. Second, we encompassed the region corresponding to motor control of the lower extremity in the precentral gyrus. The seed region that was thereby defined usually spanned 4 columns of pixels on each bank of the medial longitudinal fissure, and the seed region was typically located between the precentral sulcus and central sulcus. To determine the propagating direction of a fiber vector in the seed region, trilinear interpolation was applied on the fiber orientations of neighboring voxels at the 8 corners. If voxels contained multiple fiber orientations, the orientation closest to the previous propagating direction was selected for interpolation. The next point of the fiber tract was determined by the propagating direction. The procedures were performed recursively and terminated when the turning angle exceeded a specific threshold, 32°, or when the tract reached a voxel without fibers. Using this method, the fiber tracts passing through both seed regions were retained to represent the CST originating from the lower extremity motor control of the M1 (Fig 2). The sections showing the PLIC were determined on the GFA map, and the weighted-average of the GFA at the PLIC segment, denoted GFAPLIC-TS, was calculated by multiplying the GFA of each pixel with a weighting factor proportional to the number of CST tracts passing through the same pixel. The measurement was performed in both the unaffected and affected hemispheres. We grouped the data according to affected and unaffected hemisphere in this study because previous research has suggested that handedness does not directly affect CST fiber characteristics38 and that analysis of our own unpublished data of 10 healthy adults shows that neither handedness nor footedness has an effect on GFA values of the CSTs of the 2 hemispheres.
Fig 1.
Seed region and ROI placement on GFA maps at the (A) CP and (B) M1 in the TS analysis and at the (C) PLIC in the ROI-based analysis of bilateral CSTs corresponding to the lower extremity motor control in a patient with moderate stroke.
Fig 2.
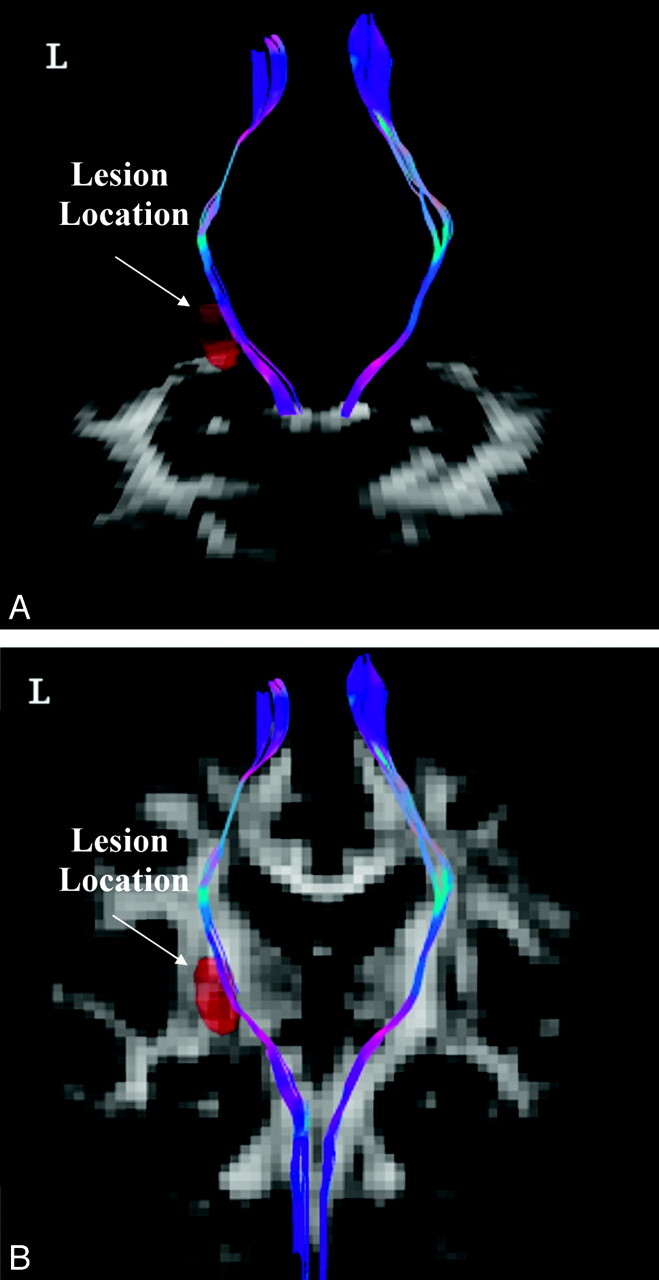
Tractography of bilateral CSTs corresponding to lower extremity motor control in a patient with ischemic stroke at the left PLIC (red area). A, The axial view of the bilateral CSTs passing through the CP; (B) the coronal view of the bilateral CSTs. For fiber direction, red indicates the left-right direction, green indicates the anteroposterior direction, and blue indicates the inferior-superior direction. The background images are GFA maps.
ROI-Based Analysis
The mean GFA values at the PLIC segments were also calculated by using the ROI-based analysis. On all sections containing the PLIC on the GFA map, the posterior two-thirds of the PLIC were selected as the ROI to represent the lower extremity motor control area (Fig 1C). We obtained the GFA values of all selected pixels and calculated the mean GFA of the ROI at the PLIC, denoted GFAPLIC-ROI. The measurement was also performed in both the unaffected hemisphere and affected hemisphere.
Statistical Analysis
To establish the intrarater and interrater reliabilities of the TS and ROI-based analyses, 2 raters (Y.-H.K. and Z.-A.L.) analyzed the data twice with a 1-week interanalysis interval. The intrarater and interrater reliabilities were investigated on the seed region placement for the TS analysis and ROI placement for the ROI-based analysis. The κ statistics were used to evaluate the agreement of pixel coordinates for both the seeds at the CP and the motor control of the lower extremity at the M1 for the TS analysis, as well as at the PLIC for the ROI-based analysis. A κ value >0.80 was considered excellent agreement, and κ between 0.60 and 0.80 represented substantial levels of agreement.39 The intrarater and interrater reliabilities for the mean GFAPLIC-TS and mean GFAPLIC-ROI were evaluated by ICC3,140 and the standard error of measurement.41 An ICC value >0.75 was regarded as good reliability.41 The standard error of measurement (, where Sx is the standard deviation of the set of observed values and rxx is the reliability of coefficient of the measure) is the standard deviation of the measurement errors, and thus smaller standard errors of measurement corresponds to better reliability of the GFA measures.41
By correlating the mean GFAPLIC-TS and GFAPLIC-ROI of the affected hemisphere analyzed by rater 1 (Z.-A.L.) with the FMA-LE rated by rater 2 (Y.-H.K.), by using the Pearson correlation coefficients, we measured the relationships between the fiber integrity of the CST of the affected hemisphere and the motor function of the affected lower extremity.
The comparisons between the mean GFAPLIC-TS and GFAPLIC-ROI, between their SDs, and between their CVs (= SD/mean) were performed by using a 2-tailed paired t test. Statistical significance was considered for P < .05.
Results
Reliability
For the TS analysis, the κ values of intrarater reliability for the coordinates of the seeds in both the unaffected hemisphere and affected hemisphere ranged from 0.87 to 0.97 for rater 1 and from 0.79 to 0.95 for rater 2 (Table 2). The κ values of interrater reliability ranged from 0.81 to 0.90 for the unaffected hemisphere and from 0.86 to 0.98 for the affected hemisphere (Table 2). These results indicated substantial-to-excellent intrarater and interrater agreement on the seed region placement at the CP and the motor control of the lower extremity at the M1.
Table 2:
Kappa values for agreement on the seed region and ROI placement in the TS and ROI-based analyses
| Subject | TS Analysis |
ROI-Based Analysis |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intrarater |
Interrater: Raters 1 and 2 |
Intrarater |
Interrater: Raters 1 and 2 |
|||||||||
| Rater 1 |
Rater 2 |
Rater 1 |
Rater 2 |
|||||||||
| UH | AH | UH | AH | UH | AH | UH | AH | UH | AH | UH | AH | |
| 1 | 0.93 | 0.93 | 0.95 | 0.82 | 0.85 | 0.90 | 0.95 | 0.93 | 0.91 | 0.95 | 0.87 | 0.84 |
| 2 | 0.97 | 0.97 | 0.87 | 0.82 | 0.87 | 0.90 | 0.95 | 0.95 | 0.93 | 0.99 | 0.93 | 0.93 |
| 3 | 0.94 | 0.87 | 0.93 | 0.89 | 0.82 | 0.87 | 0.93 | 0.94 | 0.91 | 0.89 | 0.86 | 0.92 |
| 4 | 0.92 | 0.88 | 0.79 | 0.83 | 0.81 | 0.98 | 0.95 | 0.95 | 0.84 | 0.89 | 0.89 | 0.93 |
| 5 | 0.96 | 0.93 | 0.93 | 0.91 | 0.90 | 0.90 | 0.95 | 0.95 | 1.00 | 0.76 | 0.92 | 0.91 |
| 6 | 0.97 | 0.94 | 0.92 | 0.92 | 0.89 | 0.86 | 0.98 | 0.94 | 0.89 | 0.82 | 0.91 | 0.90 |
| 7 | 0.93 | 0.97 | 0.89 | 0.93 | 0.84 | 0.92 | 0.95 | 0.97 | 0.91 | 1.00 | 0.89 | 0.94 |
| Mean | 0.95 | 0.93 | 0.90 | 0.87 | 0.85 | 0.90 | 0.95 | 0.95 | 0.91 | 0.90 | 0.90 | 0.91 |
| SD | 0.02 | 0.04 | 0.05 | 0.05 | 0.03 | 0.04 | 0.01 | 0.01 | 0.05 | 0.09 | 0.03 | 0.03 |
The ICCs for intrarater reliability for the mean GFAPLIC-TS in both the unaffected hemisphere and affected hemisphere ranged from 0.83 to 1.00 for rater 1 (P < .05) and from 0.96 to 1.00 for rater 2 (Table 3). The ICCs for interrater reliability for the mean GFAPLIC-TS were 0.85 for the unaffected hemisphere and 1.00 for the affected hemisphere (Table 3). The standard error of measurements of the mean GFAPLIC-TS in all intrarater and interrater analyses were ≤0.01 (Table 3). The high ICCs and small standard error of measurements indicated excellent intrarater and interrater reliability for the mean GFAPLIC-TS values.
Table 3:
ICC(3,1) and standard error of measurement of the GFAPLIC-TS and GFAPLIC-ROI for intra- and interrater reliability in stroke subjects
| GFAPLIC-TS |
GFAPLIC-ROI |
|||
|---|---|---|---|---|
| Unaffected Hemisphere | Affected Hemisphere | Unaffected Hemisphere | Affected Hemisphere | |
| ICC (95% CI) | ||||
| Intrarater reliability | ||||
| Rater 1 | 0.97* (0.83–0.99) | 1.00* (0.99–1.00) | 0.99* (0.94–1.00) | 1.00* (0.99–1.00) |
| Rater 2 | 1.00* (1.00–1.00) | 0.99* (0.96–1.00) | 1.00* (0.97–1.00) | 1.00* (0.99–1.00) |
| Interrater reliability | ||||
| Raters 1 and 2 | 0.85* (0.14–0.98) | 1.00* (0.99–1.00) | 1.00* (0.99–1.00) | 1.00* (0.99–1.00) |
| Standard error of measurement | ||||
| Intrarater reliability | ||||
| Rater 1 | 0.01 | 0.01 | 0.01 | 0.01 |
| Rater 2 | 0.00 | 0.01 | 0.01 | 0.01 |
| Interrater reliability | ||||
| Raters 1 and 2 | 0.01 | 0.01 | 0.01 | 0.01 |
P < .05 indicates significance.
For the ROI-based analysis, the κ values of intrarater reliability for the coordinates of the ROIs in both the unaffected hemisphere and affected hemisphere ranged from 0.93 to 0.98 for rater 1 and from 0.76 to 1.00 for rater 2 (Table 2). The mean κ values for interrater reliability were 0.90 for the unaffected hemisphere and 0.91 for the affected hemisphere (Table 2). The results indicated excellent intrarater and interrater agreement for the ROI placement at the PLIC.
The ICCs for intrarater reliability for the mean GFAPLIC-ROI values in both the unaffected hemisphere and affected hemisphere were 0.99 or 1.00 (P < .05) for both raters. The ICCs for interrater reliability were 1.00 for both the unaffected hemisphere and affected hemisphere (Table 3). The standard errors of measurements were 0.01 for all intrarater and interrater reliability with the ROI-based analysis (Table 3). Therefore, there was excellent intrarater and interrater reliability for the mean GFAPLIC-ROI values.
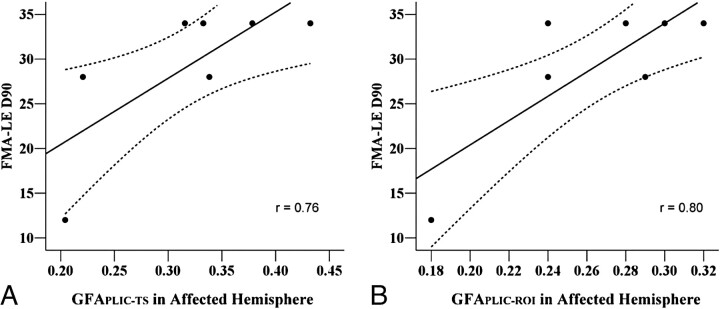
Clinical Correlation of Motor Function of the Lower Extremities
We used the data analyzed by rater 1 to calculate the correlations between the GFA values of the affected hemisphere and the FMA-LE motor scores. The results showed significantly high correlations of the FMA-LE motor score with the GFAPLIC-TS (r = 0.76, P < .05) (Fig 3A) and with the GFAPLIC-ROI (r = 0.80, P < .05) (Fig 3B).
Fig 3.
Scatterplots of the correlation between (A) the GFAPLIC-TS of the affected hemisphere and the FMA-LE motor score (r = 0.76), and (B) the GFAPLIC-ROI of the affected hemisphere and the FMA-LE motor score (r = 0.80).
Comparison of GFAPLIC-TS and GFAPLIC-ROI
We used the data analyzed by rater 1 to compare the differences between the GFAPLIC-TS and GFAPLIC-ROI (Table 4). The GFAPLIC-TS was highly correlated with the GFAPLIC-ROI for the affected hemisphere (r = 0.90, P < .05), but not for the unaffected hemisphere (r = −0.15, P > .05). The values for the mean GFAPLIC-TS of the unaffected hemisphere (0.43 ± 0.02) and affected hemisphere (0.32 ± 0.08) were significantly greater than the mean GFAPLIC-ROI of the unaffected hemisphere (0.36 ± 0.04) and affected hemisphere (0.26 ± 0.05) (P < .05). The CVs for the mean GFAPLIC-TS of the unaffected hemisphere (mean CVs = 0.08) and affected hemisphere (mean CVs = 0.17) were significantly smaller than those of the mean GFAPLIC-ROI (mean CVs = 0.23 for the unaffected hemisphere, 0.37 for the affected hemisphere) (P < .05).
Table 4:
Mean, SD, and CV of the GFA values by TS analysis and ROI-based analysis (rater 1)
| Subject | GFAPLIC-TS |
GFAPLIC-ROI |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unaffected Hemisphere |
Affected Hemisphere |
Unaffected Hemisphere |
Affected Hemisphere |
|||||||||
| Mean | SD | CV | Mean | SD | CV | Mean | SD | CV | Mean | SD | CV | |
| 1 | 0.43 | 0.03 | 0.07 | 0.20 | 0.04 | 0.21 | 0.41 | 0.07 | 0.17 | 0.18 | 0.08 | 0.44 |
| 2 | 0.44 | 0.04 | 0.09 | 0.33 | 0.05 | 0.16 | 0.40 | 0.08 | 0.20 | 0.24 | 0.13 | 0.54 |
| 3 | 0.42 | 0.02 | 0.05 | 0.34 | 0.07 | 0.22 | 0.37 | 0.07 | 0.19 | 0.29 | 0.10 | 0.34 |
| 4 | 0.40 | 0.05 | 0.13 | 0.38 | 0.02 | 0.06 | 0.33 | 0.09 | 0.27 | 0.30 | 0.08 | 0.27 |
| 5 | 0.41 | 0.03 | 0.07 | 0.43 | 0.03 | 0.07 | 0.36 | 0.09 | 0.25 | 0.32 | 0.10 | 0.31 |
| 6 | 0.45 | 0.03 | 0.07 | 0.22 | 0.08 | 0.36 | 0.34 | 0.10 | 0.29 | 0.24 | 0.10 | 0.42 |
| 7 | 0.46 | 0.03 | 0.07 | 0.32 | 0.03 | 0.10 | 0.31 | 0.08 | 0.26 | 0.28 | 0.08 | 0.29 |
| Group mean | 0.43* | 0.03* | 0.08* | 0.32* | 0.05* | 0.17* | 0.36 | 0.08 | 0.23 | 0.26 | 0.10 | 0.37 |
| Group SD | 0.02 | 0.01 | 0.03 | 0.08 | 0.02 | 0.10 | 0.04 | 0.01 | 0.05 | 0.05 | 0.02 | 0.10 |
P < .05 indicates significant differences between the TS- and ROI-based analyses.
Discussion
By analyzing the DSI data of the patients with subcortical ischemic stroke, we investigated the reliability and validity of TS analysis on the CST, and we compared the performance with that of the ROI-based analysis. We found excellent intrarater and interrater reliability for both TS- and ROI-based analyses in the seed region or ROI placement and in the mean GFA values. In the affected hemisphere, the mean GFA measured from both analyses showed high correlation with the motor function of the affected lower extremity. Although the GFA values measured by both analyses were correlated, the TS analysis yielded significantly higher mean GFA and lower variance than did the ROI-based analysis.
Several factors may affect the agreement on seed region and ROI placement. The rater's knowledge and familiarity with brain anatomy is a key factor in determining the proper selection of the seed region and ROI, which in turn influences the reliability of the seed region and ROI placement.8 In this study, using a set of guidelines and the T2-weighted template, in addition to adequate personnel training, may have helped us establish excellent reliability in both analyses.
Our excellent intrarater and interrater reliability for the seed region and ROI placement have led to the excellent reliability of the measured GFA values. Hong et al9 used both TS- and ROI-based analyses to investigate the interrater reliability of the FA values of the pyramidal tracts at the CP in patients with amyotrophic lateral sclerosis. Hong et al9 found significantly higher interrater reliability of FA values in the TS analysis (Spearman correlation coefficient rs = 0.91) compared with those in the ROI-based analysis (rs = 0.70). In contrast, our results did not show poorer reliability of the GFAPLIC-ROI as compared with that of the GFAPLIC-TS. This discrepancy may be due to the relatively clearer boundary of the CST at the PLIC region than at the CP. Furthermore, the pyramidal tracts in the brain stem are close to the space containing the CSF9 and to other crossing tracts.22 Therefore, the ROI-based analysis at the brain stem region is more subject to partial volume effects than at the PLIC region.
Ozturk et al8 investigated the intrarater and interrater reliability of the FA at the PLIC region by using ROI-based analysis in 5 healthy controls and 7 subjects with closed-head injuries. They reported a low level (κ = 0.08) of intrarater reliability and a fair level (κ = 0.31) of interrater reliability, which may be related to the long interanalysis interval (4–12 weeks) and no use of a template for ROI delineation. In summary, according to our results, both the TS quantitative analysis and the ROI-based analyses are reliable approaches for DSI data analysis and may be performed in future clinical DSI studies. The set of clear guidelines, adequate training of raters, and better ROI delineation at the PLIC region may lead to better results for reliability than the previous reports.
In this study, we found significantly good-to-excellent correlation of the GFAPLIC-TS or GFAPLIC-ROI with the FMA-LE. Previously, similar studies have been performed by using ROI-based analysis of DTI data to show a high correlation between the FA values and the overall muscle strength of the affected extremities (by using the total score of Manual Muscle Testing or Motricity Index)2,42 and the hand function 6,7 in patients with subacute or chronic ischemic stroke. Using the TS analysis, we have successfully demonstrated that the fiber integrity of the affected CST corresponding to the lower extremity motor control originating from the M1 is strongly correlated with the motor function of the affected lower extremity (r > 0.75). Our findings suggest that the integrity of the CST fibers originating from the M1 plays an important role in lower extremity motor recovery. Our approach may allow future research using the TS analysis to study the relationships between the fiber integrity of a particular fiber tract and the motor function of a particular body part.
Our findings that the correlation between the GFAPLIC-ROI and the FMA-LE of the affected lower extremity (r = 0.80) was slightly higher than that between the GFAPLIC-TS and the FMA-LE (r = 0.76) may be due to differences in the CST fibers selected by the 2 analyses. Studies by using functional MR imaging in patients with ischemic stroke have found that the brain activation areas during unilateral movement of the affected lower extremity include the ipsilesional M1, supplementary motor area, and secondary sensorimotor cortices.43,44 The descending motor fibers originating from these areas all pass through the PLIC region. Our TS quantitative analysis included only the spared CST fibers originating from the M1 area. Our ROI-based method enclosed the posterior two-thirds of the PLIC, which included not only spared CST fibers originating from the M1 but also those originating from other secondary cortical motor areas. Because all of these fibers contribute to motor recovery, this might lead to a slightly higher correlation between the GFAPLIC-ROI and the FMA-LE.
Although the GFAPLIC-TS and GFAPLIC-ROI in the affected hemisphere were highly correlated with each other and both values were correlated with the motor function of the affected lower extremity, the TS analysis yielded higher mean GFA values and less variability, as revealed by the lower standard deviation and coefficient of variance of GFA values, than did the ROI-based analysis. One reason for this discrepancy may be that the ROI-based method possibly includes pixels with evidently low GFA values, whereas the tractography preferentially passes through the relatively spared regions and samples pixels with relatively higher GFA values. Another reason may be due to the method for calculating the mean GFA values. In our TS analysis, the mean GFAPLIC-TS was calculated as the weighted sum of the GFA values of each individual pixel, with the weighting factors scaled to the number of tracts passing through the same pixel. This was to give more weighting to pixels with a greater number of fibers passing through than to those with fewer fibers passing through. In contrast, in our ROI-based analysis, the GFA values of the selected pixels were averaged with equal weights, which was consistent with conventional ROI analysis.2,6,7
Generally speaking, due to the inherent differences in the GFA sampling and calculation, the ROI analysis focuses more on functional-related regions of white matter, whereas the TS analysis allows for investigation of fiber properties of tract-specific regions and provides information about properties of particular fiber tracts of interest. The strength of the ROI-based analysis is that the obtained GFAPLIC-ROI values can be considered to represent the overall integrity of a white matter region, where both injured and spared fibers involved in lower extremity motor control are enclosed. Thus, the GFAPLIC-ROI would show a high correlation with a more general clinical outcome measure, such as the FMA-LE, of lower extremity motor control. Using ROI-based analysis, however, may potentially enclose fibers originating from different cortical motor areas, which makes it difficult to differentiate the degree of contributions from different motor areas to the recovery of lower extremity motor control. On the other hand, the TS analysis has the advantage of specifically evaluating the degree of integrity in the relatively spared tract region of the CST fibers originating from the lower extremity motor control region of the M1. This method also has the potential to allow researchers to examine other specific fibers of interest, such as those originating from secondary motor cortical areas. With this specificity of the fibers reconstructed by using the TS analysis, the GFAPLIC-TS may inevitably yield a slightly smaller correlation with the global clinical outcome measure FMA-LE than the GFAPLIC-ROI. Therefore, the decision regarding which method to be used in a study will depend on the purpose of the study.
There are a few limitations of this study. First, the sample size may be too small for the generalization of our results on rater comparison. We have performed similar rater comparison on DSI data of 10 healthy subjects by using the same analysis algorithm. The results yielded the similarly high intra- and interrater reliabilities. Second, the success of the TS analysis relies mainly on the accurate reconstruction of the tractography over the entire CST. The tractography may be interrupted in severe stroke, where low GFA values involve a large area, or in hemorrhagic stroke, where some derivatives of hemoglobin may induce severe magnetic susceptibilities. Further research on patients with greater stroke severity will be needed. Third, scan time required to acquire DSI data may potentially increase the likelihood of patient motion, which then can cause blurring of the image data and reduce the angular resolution of the orientation distribution function,45 consequently resulting in the failure of the tractography reconstruction. In this study, all participants tolerated the scan time well and presented little head motion during the scan. The tractography of the CST was successfully reconstructed from all of the participants, but difficulties may arise when it is applied to patients with a wider range of clinical problems.
In this study, the seeds/ROI placement is selected manually by following a set of guidelines. An emerging method of reconstructing white matter fibers is by using functional MR imaging-guided fiber tracking technology. This technology has been performed in healthy participants46 and in patients with brain tumors47,48 by using DTI. This methodology has potential to be used in patients with stroke for mapping the cortical representations for upper and lower extremity motor function and guiding the placement of seeds for reconstructing CST fibers associated with upper and lower extremity motor function. However, we also foresee 2 major difficulties when applying this technology in patients with stroke. First, patients with stroke may have difficulty performing isolated joint movements without any associated movements or spasticity, which then may cause larger head motion during MR imaging.44,49 Second, the BOLD signals in ipsilesional M1 may be significantly decreased or even absent while patients with stroke perform movements with the affected upper or lower extremity.50–53 Movement-related BOLD signals may shift from the primary motor cortex to secondary association motor networks or even the contralesional hemisphere in response to stroke lesions.53,54 More research will be needed to validate the usage of this new technology in patients with stroke.
Conclusions
In this study, we have demonstrated good reliability and validity of the TS analysis method and ROI-based analysis method of the CST. Both analysis methods indicate that the GFA values at the PLIC segments of the CST in the affected hemisphere are highly correlated with motor function of the affected lower extremity in patients with ischemic stroke. The different mean GFA and its variance derived from the 2 methods imply that the inherent differences in sampling and calculation of the 2 methods might provide different information about the tract integrity.
Acknowledgments
We thank Dr J.S. Jeng for helping with stroke subject recruitment. We also thank all participants of this study.
Abbreviations
- AH
affected hemisphere
- BG
basal ganglia
- BOLD
blood oxygen level–dependent
- CP
cerebral peduncle
- CST
corticospinal tract
- CV
coefficient of variance
- DSI
diffusion spectrum imaging
- DTI
diffusion tensor imaging
- FA
fractional anisotropy
- FMA-LE
Fugl-Meyer assessment of lower extremity
- GFA
generalized fractional anisotropy
- GFAPLIC-TS
GFA value of the PLIC calculated by using the tract-specific method
- GFAPLIC-ROI
GFA value of the PLIC calculated by using the ROI-based method
- ICC
intraclass correlation coefficients
- M1
primary motor cortex/precentral gyrus
- MMSE
Mini-Mental State Examination
- NIHSS
National Institutes of Health Stroke Scale
- PLIC
posterior limb of the internal capsule
- ROI
region of interest
- SD
standard deviation
- TS
tract-specific
- UH
unaffected hemisphere
Footnotes
This work was supported by grants from the National Science Council (NSC95-2314-B-002-238-MY3 to P.-F. Tang, National Taiwan University, Taipei, Taiwan, and NSC97-2752-M-002-011-PAE to W.-Y.I. Tseng, National Taiwan University Hospital, Taipei, Taiwan) and in part by the Department of Medical Imaging in the National Taiwan University Hospital and 3T MRI Laboratory in National Taiwan University Hospital, Taipei, Taiwan.
References
- 1. Liang Z, Zeng J, Liu S, et al. A prospective study of secondary degeneration following subcortical infarction using diffusion tensor imaging. J Neurol Neurosurg Psychiatry 2007;78:581–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Thomalla G, Glauche V, Koch MA, et al. Diffusion tensor imaging detects early wallerian degeneration of the pyramidal tract after ischemic stroke. Neuroimage 2004;22:1767–74 [DOI] [PubMed] [Google Scholar]
- 3. Basser PJ. Inferring microstructural features and the physiological state of tissues from diffusion-weighted images. NMR Biomed 1995;8:333–44 [DOI] [PubMed] [Google Scholar]
- 4. Liang Z, Zeng J, Zhang C, et al. Longitudinal investigations on the anterograde and retrograde degeneration in the pyramidal tract following pontine infarction with diffusion tensor imaging. Cerebrovasc Dis 2008;25:209–16 [DOI] [PubMed] [Google Scholar]
- 5. Yu C, Zhu C, Zhang Y, et al. A longitudinal diffusion tensor imaging study on wallerian degeneration of corticospinal tract after motor pathway stroke. Neuroimage 2009;47:451–58 [DOI] [PubMed] [Google Scholar]
- 6. Lindberg PG, Skejo PH, Rounis E, et al. Wallerian degeneration of the corticofugal tracts in chronic stroke: a pilot study relating diffusion tensor imaging, transcranial magnetic stimulation, and hand function. Neurorehabil Neural Repair 2007;21:551–60 [DOI] [PubMed] [Google Scholar]
- 7. Stinear CM, Barber PA, Smale PR, et al. Functional potential in chronic stroke patients depends on corticospinal tract integrity. Brain 2007;130:170–80 [DOI] [PubMed] [Google Scholar]
- 8. Ozturk A, Sasson AD, Farrell JA, et al. Regional differences in diffusion tensor imaging measurements: assessment of intrarater and interrater variability. AJNR Am J Neuroradiol 2008;29:1124–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hong YH, Sung JJ, Kim SM, et al. Diffusion tensor tractography-based analysis of the pyramidal tract in patients with amyotrophic lateral sclerosis. J Neuroimaging 2008;18:282–87 [DOI] [PubMed] [Google Scholar]
- 10. Kanaan RA, Shergill SS, Barker GJ, et al. Tract-specific anisotropy measurements in diffusion tensor imaging. Psychiatry Res 2006;146:73–82 [DOI] [PubMed] [Google Scholar]
- 11. Partridge SC, Mukherjee P, Berman JI, et al. Tractography-based quantitation of diffusion tensor imaging parameters in white matter tracts of preterm newborns. J Magn Reson Imaging 2005;22:467–74 [DOI] [PubMed] [Google Scholar]
- 12. Wang S, Melhem ER. Amyotrophic lateral sclerosis and primary lateral sclerosis: the role of diffusion tensor imaging and other advanced MR-based techniques as objective upper motor neuron markers. Ann N Y Acad Sci 2005;1064:61–77 [DOI] [PubMed] [Google Scholar]
- 13. Berman JI, Mukherjee P, Partridge SC, et al. Quantitative diffusion tensor MRI fiber tractography of sensorimotor white matter development in premature infants. Neuroimage 2005;27:862–71 [DOI] [PubMed] [Google Scholar]
- 14. Mori S, Crain BJ, Chacko VP, et al. Three-dimensional tracking of axonal projections in the brain by magnetic resonance imaging. Ann Neurol 1999;45:265–69 [DOI] [PubMed] [Google Scholar]
- 15. Mori S, van Zijl PC. Fiber tracking: principles and strategies—a technical review. NMR Biomed 2002;15:468–80 [DOI] [PubMed] [Google Scholar]
- 16. Sage CA, Peeters RR, Gorner A, et al. Quantitative diffusion tensor imaging in amyotrophic lateral sclerosis. Neuroimage 2007;34:486–99 [DOI] [PubMed] [Google Scholar]
- 17. Cho SH, Kim DG, Kim DS, et al. Motor outcome according to the integrity of the corticospinal tract determined by diffusion tensor tractography in the early stage of corona radiata infarct. Neurosci Lett 2007;426:123–27 [DOI] [PubMed] [Google Scholar]
- 18. Jang SH, Bai D, Son SM, et al. Motor outcome prediction using diffusion tensor tractography in pontine infarct. Ann Neurol 2008;64:460–65 [DOI] [PubMed] [Google Scholar]
- 19. Jang SH, Park KA, Ahn SH, et al. Transcallosal fibers from corticospinal tract in patients with cerebral infarct. NeuroRehabilitation 2009;24:159–64 [DOI] [PubMed] [Google Scholar]
- 20. Wedeen VJ, Hagmann P, Tseng WY, et al. Mapping complex tissue architecture with diffusion spectrum magnetic resonance imaging. Magn Reson Med 2005;54:1377–86 [DOI] [PubMed] [Google Scholar]
- 21. Wedeen VJ, Reese TG, Tuch DS, et al. Mapping fiber orientation spectra in cerebral white matter with Fourier-transform diffusion MRI. In: Proceedings of the Eighth Meeting of the International Society for Magnetic Resonance in Medicine. Berkeley, CA: International Society for Magnetic Resonance in Medicine, 2000:82 [Google Scholar]
- 22. Wedeen VJ, Wang RP, Schmahmann JD, et al. Diffusion spectrum magnetic resonance imaging (DSI) tractography of crossing fibers. Neuroimage 2008;41:1267–77 [DOI] [PubMed] [Google Scholar]
- 23. Yeh FC, Wedeen VJ, Tseng WYI. A recursive algorithm to decompose orientation distribution function and resolve intra-voxel fiber directions. In: International Society for Magnetic Resonance in Medicine 16th Scientific Meeting and Exhibition, Toronto, Ontario, Canada, May 3–9, 2008 [Google Scholar]
- 24. Maniega SM, Bastin ME, Armitage PA, et al. Temporal evolution of water diffusion parameters is different in grey and white matter in human ischaemic stroke. J Neurol Neurosurg Psychiatry 2004;75:1714–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pierpaoli C, Barnett A, Pajevic S, et al. Water diffusion changes in wallerian degeneration and their dependence on white matter architecture. Neuroimage 2001;13:1174–85 [DOI] [PubMed] [Google Scholar]
- 26. Lai C, Zhang SZ, Liu HM, et al. White matter tractography by diffusion tensor imaging plays an important role in prognosis estimation of acute lacunar infarctions. Br J Radiol 2007;80:782–89 [DOI] [PubMed] [Google Scholar]
- 27. Nelles M, Gieseke J, Flacke S, et al. Diffusion tensor pyramidal tractography in patients with anterior choroidal artery infarcts. AJNR Am J Neuroradiol 2008;29:488–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Brott T, Adams HP, Jr, Olinger CP, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke 1989;20:864–70 [DOI] [PubMed] [Google Scholar]
- 29. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98 [DOI] [PubMed] [Google Scholar]
- 30. Fugl-Meyer AR, Jaasko L, Leyman I, et al. The post-stroke hemiplegic patient, I: A method for evaluation of physical performance. Scand J Rehabil Med 1975;7:13–31 [PubMed] [Google Scholar]
- 31. Hislop HJ, Montgomery J. Daniels and Worthingham's Muscle Testing: Techniques of Manual Examination. Philadelphia: Saunders; 2002 [Google Scholar]
- 32. Albert M, Cohen C. The test for severe impairment: an instrument for the assessment of patients with severe cognitive dysfunction. J Am Geriatr Soc 1992;40:449–53 [DOI] [PubMed] [Google Scholar]
- 33. Duncan PW, Propst M, Nelson SG. Reliabitily of the Fugl-Meyer assessment of sensorimotor recovery following cerebrovascular accident. Phys Ther 1983;63:1606–11 [DOI] [PubMed] [Google Scholar]
- 34. Molloy DW, Standish TI. A guide to the standardized Mini-Mental State Examination. Int Psychogeriatr 1997;9 (suppl 1):87–94; discussion 143–50 [DOI] [PubMed] [Google Scholar]
- 35. Reese TG, Heid O, Weisskoff RM, et al. Reduction of eddy-current-induced distortion in diffusion MRI using a twice-refocused spin echo. Magn Reson Med 2003;49:177–82 [DOI] [PubMed] [Google Scholar]
- 36. Kuo LW, Chen JH, Wedeen VJ, et al. Optimization of diffusion spectrum imaging and q-ball imaging on clinical MRI system. Neuroimage 2008;41:7–18 [DOI] [PubMed] [Google Scholar]
- 37. Tuch DS. Q-ball imaging. Magn Reson Med 2004;52:1358–72 [DOI] [PubMed] [Google Scholar]
- 38. Westerhausen R, Huster RJ, Kreuder F, et al. Corticospinal tract asymmetries at the level of the internal capsule: is there an association with handedness? Neuroimage 2007;37:379–86 [DOI] [PubMed] [Google Scholar]
- 39. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74 [PubMed] [Google Scholar]
- 40. Shrout PE, Fleiss JL. Intraclass correlations: users in assessing rater reliability. Psychol Bull 1979;86:420–28 [DOI] [PubMed] [Google Scholar]
- 41. Portney L, Watkins M. Foundations of Clinical Research: Applications to Practice. Upper Saddle River, NJ: Pearson Education; 2009 [Google Scholar]
- 42. Kunimatsu A, Aoki S, Masutani Y, et al. Three-dimensional white matter tractography by diffusion tensor imaging in ischaemic stroke involving the corticospinal tract. Neuroradiology 2003;45:532–35 [DOI] [PubMed] [Google Scholar]
- 43. Enzinger C, Johansen-Berg H, Dawes H, et al. Functional MRI correlates of lower limb function in stroke victims with gait impairment. Stroke 2008;39:1507–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Luft AR, Forrester L, Macko RF, et al. Brain activation of lower extremity movement in chronically impaired stroke survivors. Neuroimage 2005;26:184–94 [DOI] [PubMed] [Google Scholar]
- 45. Chiang WY, Wedeen VJ, Reese TG, et al. Motion artifact for diffusion spectrum imaging. In: International Society for Magnetic Resonance in Medicine15th Scientific Meeting and Exhibition, Berlin, Germany, May 19–25, 2007 [Google Scholar]
- 46. Staempfli P, Reischauer C, Jaermann T, et al. Combining fMRI and DTI: a framework for exploring the limits of fMRI-guided DTI fiber tracking and for verifying DTI-based fiber tractography results. Neuroimage 2008;39:119–26 [DOI] [PubMed] [Google Scholar]
- 47. Kleiser R, Staempfli P, Valavanis A, et al. Impact of fMRI-guided advanced DTI fiber tracking techniques on their clinical applications in patients with brain tumors. Neuroradiology 2010;52:37–46 [DOI] [PubMed] [Google Scholar]
- 48. Smits M, Vernooij MW, Wielopolski PA, et al. Incorporating functional MR imaging into diffusion tensor tractography in the preoperative assessment of the corticospinal tract in patients with brain tumors. AJNR Am J Neuroradiol 2007;28:1354–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Luft AR, Smith GV, Forrester L, et al. Comparing brain activation associated with isolated upper and lower limb movement across corresponding joints. Hum Brain Mapp 2002;17:131–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Dobkin BH, Firestine A, West M, et al. Ankle dorsiflexion as an fMRI paradigm to assay motor control for walking during rehabilitation. Neuroimage 2004;23:370–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Jang SH, Kim YH, Cho SH, et al. Cortical reorganization associated with motor recovery in hemiparetic stroke patients. Neuroreport 2003;14:1305–10 [DOI] [PubMed] [Google Scholar]
- 52. Kim YH, You SH, Kwon YH, et al. Longitudinal fMRI study for locomotor recovery in patients with stroke. Neurology 2006;67:330–33 [DOI] [PubMed] [Google Scholar]
- 53. Ward NS, Newton JM, Swayne OB, et al. Motor system activation after subcortical stroke depends on corticospinal system integrity. Brain 2006;129:809–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ward NS, Cohen LG. Mechanisms underlying recovery of motor function after stroke. Arch Neurol 2004;61:1844–48 [DOI] [PMC free article] [PubMed] [Google Scholar]