SUMMARY:
LSTVs are common within the spine, and their association with low back pain has been debated in the literature for nearly a century. LSTVs include sacralization of the lowest lumbar vertebral body and lumbarization of the uppermost sacral segment. These vertebral bodies demonstrate varying morphology, ranging from broadened transverse processes to complete fusion. Low back pain associated with an LSTV may arise from the level above the transition, the contralateral facet when unilateral, and/or the anomalous articulation when present. Although this association is still somewhat controversial, beyond dispute is the importance of identifying an LSTV in patients in whom a surgical or interventional procedure is planned. This is essential to avoid an intervention or surgery at an incorrect level. In this article, each of these issues will be addressed with attention to identifying and correctly numbering LSTVs as well as detecting imaging findings related to the genesis of low back pain.
LSTVs are congenital spinal anomalies defined as either sacralization of the lowest lumbar segment or lumbarization of the most superior sacral segment of the spine. LSTVs are common in the general population, with a reported prevalence of 4%–30%.1–15 The degree of morphologic variation of these segments ranges from L5 vertebrae with broadened elongated transverse processes to complete fusion to the sacrum. Conversely, the S1 vertebral segment can show varying degrees of lumbarization, such as the formation of an anomalous articulation rather than fusion to the remainder of the sacrum, well-formed lumbar-type facet joints, a more squared appearance in the sagittal plane, as well as a well-formed fully-sized disk, rather than the smaller-sized disk typically seen between S1 and S2.
While LSTVs can be identified on all imaging modalities, they have been classically described as being best imaged on Ferguson radiographs (AP radiographs angled cranially at 30°). Currently, given its superior spatial resolution, CT is the best imaging technique for characterization of LSTVs. These anomalies are usually identified incidentally because CT is not typically indicated solely to identify LSTVs, due to radiation concerns, nor is it the preferred imaging technique used to evaluate patients with nontraumatic low back pain. In these clinical cases, MR imaging is more often indicated, given its superior tissue differentiation within and around the spine. With this said, the classification and numbering of LSTVs are most problematic on MR imaging due to factors including limited imaging of the thoracolumbar junction, identification of the lowest rib-bearing vertebral body, and differentiation between thoracic hypoplastic ribs and enlarged lumbar transverse processes. These factors present a dilemma for radiologists because they may have to read a lumbar spine MR imaging examination in isolation without the benefit of other imaging such as spine radiographs to help correctly identify and enumerate LSTVs.
Correct identification of an LSTV is essential because there are important clinical implications. Inaccurate identification may lead to surgical and procedural errors and poor correlation with clinical symptoms. Additionally, although the relationship of low back pain and LSTV, termed “Bertolotti Syndrome,” has been debated in the literature since its initial description in 1917, many support this association.2–4,8,9,12,13,15–28 Symptoms can originate from the anomalous articulation itself, the contralateral facet joint (when unilateral), instability and early degeneration of the level cephalad to the transitional vertebrae, and nerve root compression from hypertrophy of the transverse process.2,3,5,8,9,12,20,24,29–31 The symptoms associated with each of the above processes are treated differently, requiring reliable techniques to not only identify LSTVs but also determine the type and site of the pathology generated by the transitional segment.
Identification and Morphology
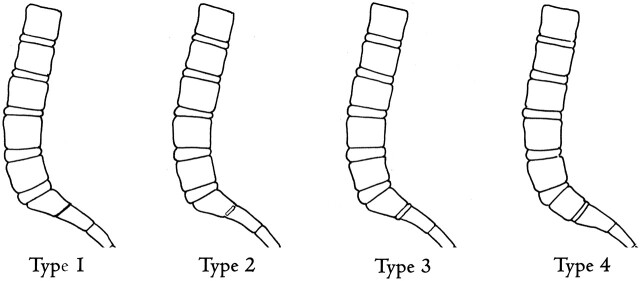
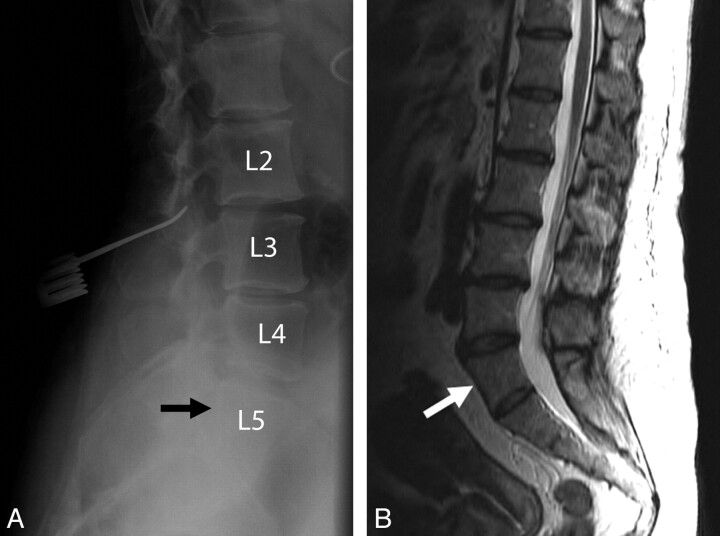
Lumbosacral transitional vertebrae have been classically identified by using lateral and Ferguson radiographs (Fig 1). In 1984, Castellvi et al2 described a radiographic classification system identifying 4 types of LSTVs on the basis of morphologic characteristics (Fig 2). Type I includes unilateral (Ia) or bilateral (Ib) dysplastic transverse processes, measuring at least 19 mm in width (craniocaudad dimension) (Fig 3). Type II exhibits incomplete unilateral (IIa) or bilateral (IIb) lumbarization/sacralization with an enlarged transverse process that has a diarthrodial joint between itself and the sacrum (Fig 4). Type III LSTV describes unilateral (IIIa) or bilateral (IIIb) lumbarization/sacralization with complete osseous fusion of the transverse process(es) to the sacrum (Fig 5). Type IV involves a unilateral type II transition with a type III on the contralateral side (Fig 6). Although useful for characterizing the relationship between the transitional segment and the level above or below, this classification system does not provide information relevant to accurate enumeration of the involved segment.
Fig 1.
Ferguson radiograph in a 35-year-old man. AP radiograph angled cranially at 30° allows better characterization of the transverse processes of L5. LSTVs have been classically described as best imaged by using Ferguson radiographs.
Fig 2.
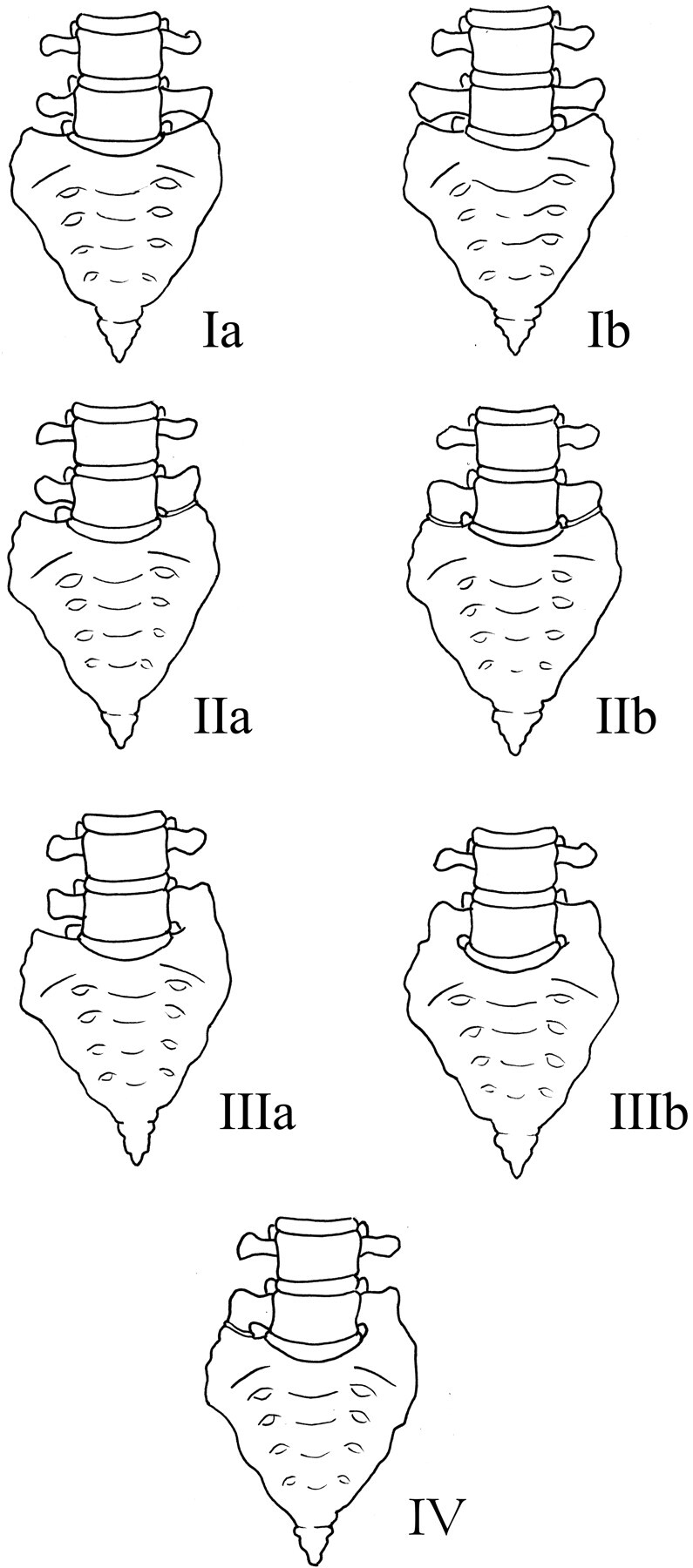
Illustration demonstrating the Castellvi classification of LSTVs.
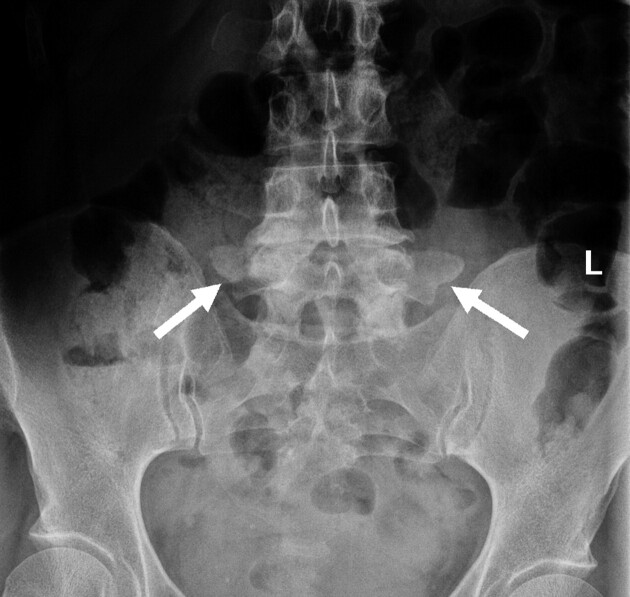
Fig 3.
Castellvi type Ib LSTV in a 53-year-old woman. AP radiograph demonstrates an LSTV with bilaterally enlarged L5 transverse processes (white arrows). There is no articulation with the sacrum.
Fig 4.
Castellvi type IIa and IIb LSTVs. A, AP radiograph demonstrates an LSTV with a unilateral anomalous articulation of the right L5 transverse process with the sacrum (white arrow) in a 42-year-old man. B, T2-weighted coronal MR image demonstrates a unilateral anomalous articulation with the sacrum (white arrow) on the left in a 64-year-old man. C, Coronal reconstructed CT image demonstrates bilateral anomalous articulations of broadened transverse processes with the sacrum and the iliac bone on the left (white arrow) in a 52-year-old woman.
Fig 5.
Castellvi type IIIa and IIIb LSTVs. A, Axial CT image demonstrates osseous fusion of the left L5 transverse process with the sacrum in a 36-year-old woman. B, Coronal reconstructed CT image demonstrates bilateral osseous fusion of L5 to the sacrum in a 31-year-old man. C, Volume-rendered CT image shows a Castellvi type IIIb LSTV with complete osseous fusion of the transverse processes to the sacrum in the same patient as seen in B.
Fig 6.
Castellvi type IV LSTV in a 61-year-old woman. Coronal T2-weighted MR image demonstrates osseous fusion of the L5 transverse process to the sacrum on the left with an anomalous articulation on the right (white arrow).
Other morphologic characteristics of transitional vertebrae include squaring of the upper sacral segment when it is lumbarized and wedging of the lowest lumbar segment when it is sacralized (Figs 7 and 8).15 These morphologic changes represent cranial and caudal shifts of the spine, respectively, resulting in either a greater or lesser number of motion segments. Wigh and Anthony15 describe the “squared” appearance of transitional vertebrae on lateral radiographs as the ratio of the AP diameter of the superior vertebral endplate to that of the inferior vertebral endplate as ≤1.37. This relative “squaring” and “wedging” represent a spectrum of vertebral body morphologic change and cannot be reliably used to definitively identify an LSTV.
Fig 7.
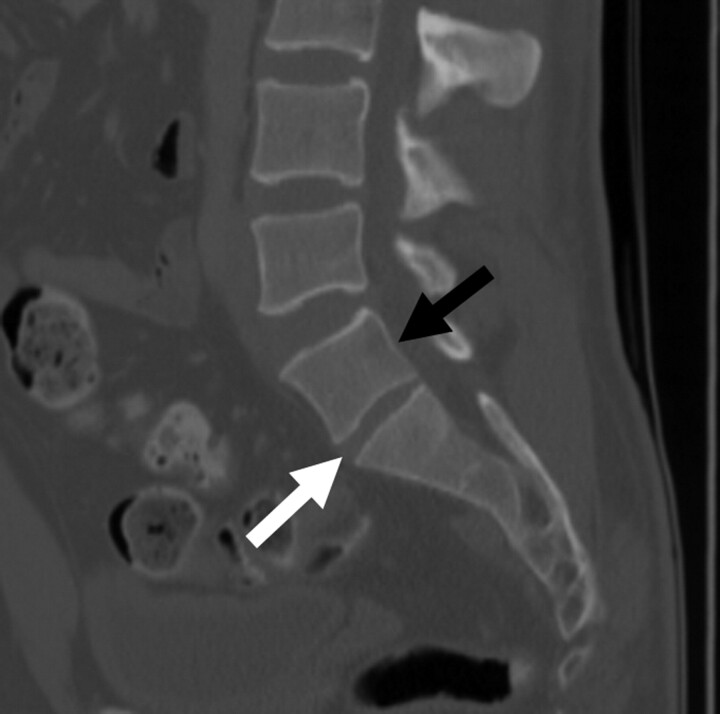
Transitional S1 vertebral body in a 52-year-old woman. Sagittal CT image demonstrates “squaring” of a lumbarized S1 vertebral body (black arrow). Additionally, there is a fully-sized lumbar type disk between S1 and S2 (white arrow), compared with the characteristic vestigial disk typically seen at this level.
Fig 8.
Transitional L5 vertebral body in a 52-year-old man. Sagittal CT image demonstrates “wedging” of a sacralized L5 transitional vertebral body (white arrow). A, Note the decreased height between the sacralized L5 vertebral body and S1 (black arrow) compared with the normal height typically seen at this level. B, Coronal CT image shows bilateral osseous fusion of the transverse processes of L5 with the sacrum (Castellvi type IIIb).
Nicholson et al32 described a decreased height on radiographs of the disk between a lumbar transitional segment and the sacrum compared with the normal disk height between L5 and S1. Similarly, it has been observed that when a lumbarized S1 is present, the disk space between S1 and S2 is larger than the rudimentary disk that is most often seen in spines without transitions. O'Driscoll et al11 developed a 4-type classification system of S1–2 disk morphology by using sagittal MR images, depending on the presence or absence of disk material and the AP length of the disk (Fig 9). Type 1 exhibits no disk material and is seen in patients without transitional segments. Type 2 consists of a small residual disk with an AP length less than that of the sacrum. This type is also most often seen in patients without transitional segments. Type 3 is a well-formed disk extending the entire AP length of the sacrum and can be seen in normal spines as well as in those with LSTVs. Type 4 is similar to type 3 but with the addition of squaring of the presumed upper sacral segment. Good correlation was found between a type 4 S1–2 disk and an S1 LSTV (Castellvi type III or IV).
Fig 9.
Illustration depicting the O'Driscoll classification system of S1–2 disk morphology.
LSTVs with anomalous diarthrodial articulations of the transverse processes with the sacrum (Castellvi type II) and some Castellvi type III vertebrae are not reliably identified by using this sagittally disk-based classification system and should be evaluated with axial or coronal MR images. Furthermore, without using other techniques or additional imaging, one can have difficulty determining what is actually S1 and, therefore, reliably identifying the S1–2 disk.
A final morphologic observation is that the facet joints between a transitional L5 and the sacrum are typically hypoplastic or even nonexistent in cases of complete osseous fusion of L5 to S1 (Fig 10 ). Conversely, with a lumbarized S1, facet joints are often identified between S1 and S2, where there is typically osseous fusion (Fig 11).
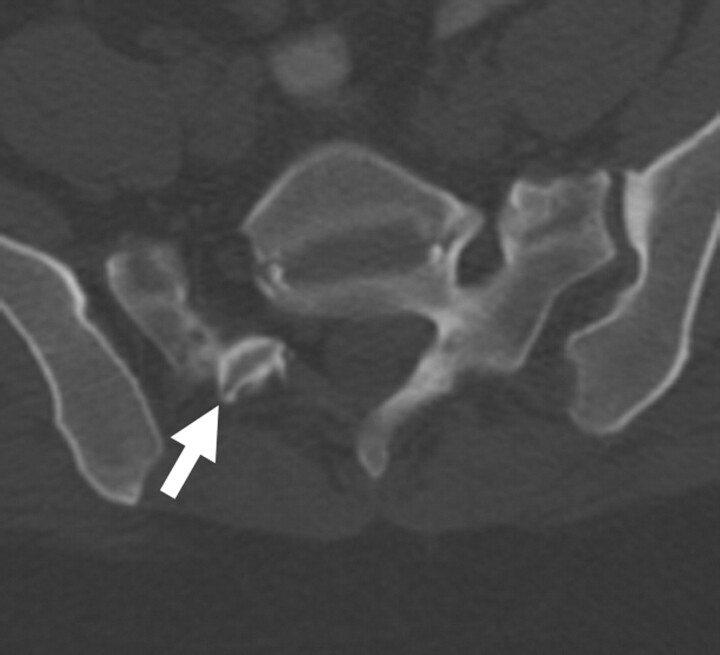
Fig 10.
Axial CT scan in a 52-year-old-woman with a Castellvi type IIa LSTV demonstrates fusion of the ipsilateral facet joint as well as a hypoplastic contralateral facet joint (white arrow) at L5-SI.
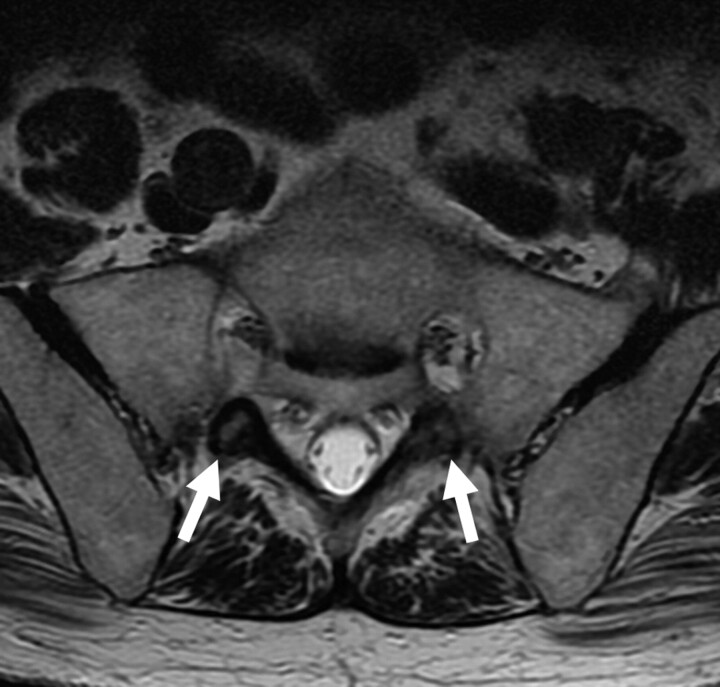
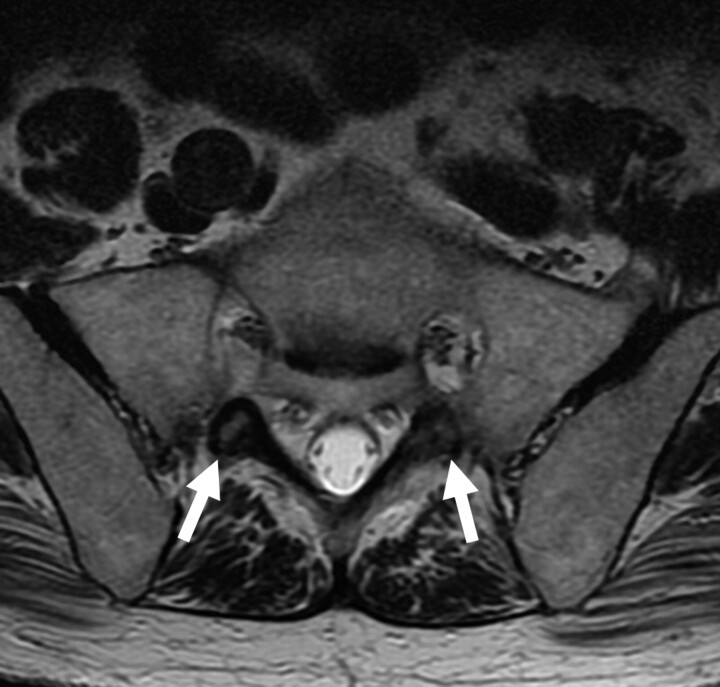
Fig 11.
Axial T2-weighted MR image demonstrates rudimentary facet joints bilaterally (white arrows) at the S1-S2 level in this 79-year-old man with a lumbarized S1.
Numbering Technique
Not only is identification of an LSTV important, accurate numeric identification of the vertebral segments on MR imaging is essential before surgery. Inaccurate numbering may lead to an interventional procedure or surgery at an unintended level. Establishing whether an LSTV is a lumbarized S1 or a sacralized L5 on MR imaging alone can often be problematic. Conventional spine radiographs are often unavailable at the time of imaging, and cervicothoracic localizers may not be routinely obtained. Radiographs of the entire spine allow the radiologist not only to count from C2 inferiorly but also to differentiate hypoplastic ribs from lumbar transverse processes, therefore enabling counting of the number of thoracic segments and correct identification of the L1 vertebral body. After this vertebral body is correctly identified, determining the correct numeric assignment of the LSTV is possible. In our experience, it is rare to have radiographs of the entire spine. More commonly, lumbar spine radiographs alone are available. In these cases, correct enumeration can often be achieved, but there remain cases in which it is difficult to differentiate hypoplastic ribs from transverse processes at the thoracolumbar junction. The presence of thoracolumbar transitions as well as segmentation anomalies further complicates evaluation of these patients.
Hahn et al6 first described the use of a sagittal cervicothoracic MR localizer to better evaluate transitional vertebrae. With a sagittal MR localizer, the vertebrae may be counted in a caudad direction from C2 rather than cephalad from L5. Using a sagittal cervicothoracic MR localizer alone assumes 7 cervical and 12 thoracic vertebrae and does not account for thoracolumbar transitions or allow differentiation of dysplastic ribs from lumbar transverse processes. The addition of a coronal MR cervicothoracic localizer increases the accuracy of enumerating lumbosacral transitional vertebrae13 because it allows better differentiation at the thoracolumbar junction. However, given the large field of view and increased section thickness of these localizers, they still commonly do not provide enough reliable anatomic information to consistently number the segments of the lumbar spine correctly. In addition, many radiologists do not routinely obtain an MR localizer inclusive of the cervical and thoracic spine when imaging patients with low back pain.
Another technique used to correctly number an LSTV is locating the iliolumbar ligaments, because they reliably arise from the L5 transverse processes.33 The iliolumbar ligament functions to restrain flexion, extension, axial rotation, and lateral bending of L5 on S1. It is seen as a low-signal-intensity structure on both axial T1- and T2-weighted MR images as a single or double band extending from the transverse process of L5 to the posteromedial iliac crest (Fig 12 ).33–35 Hughes and Saifuddin33 labeled an LSTV as L5 when no iliolumbar ligament was identified at the level above. When an iliolumbar ligament was seen to arise above the LSTV, then the vertebral body with the iliolumbar ligament was labeled L5 and the LSTV, as S1. This technique has limitations because it assumes that there are always 7 cervical, 12 thoracic, and 5 lumbar vertebrae. Various segmentation anomalies may occur along with thoracolumbar transitional vertebrae, and in these cases, identification of the iliolumbar ligament is not sufficient to accurately identify the L5 vertebral body.36
Fig 12.
Iliolumbar ligaments in a 64-year-old woman. Axial T2-weighted MR image shows low-signal-intensity iliolumbar ligaments extending from the L5 transverse processes to the posteromedial iliac crests (arrows).
The use of anatomic markers, including the aortic bifurcation, right renal artery, and conus medullaris has been reported to be least reliable. Although Lee et al37 report the position of the aortic bifurcation and right renal artery to be reliable landmarks for determining the lumbar vertebral segments on MR imaging and CT, these anatomic markers are widely believed to be less than satisfactory.33 Although the right renal artery is usually located at the L1–2 disk space, 25% of the time it is either not imaged or is present at another location.33 Variability may be seen in the position of the aortic bifurcation as it has been found at L4 in 83% of patients.37 Lee et al have also shown that the conus medullaris should not be used as a landmark because its position is quite variable.
Essentially without high-quality imaging of the entirety of the spine, there is no foolproof method for accurately numbering a transitional segment; therefore, identification, communication with the referring clinician, and correlation of intraoperative and preoperative imaging become of paramount importance as discussed later in this article.
Clinical Significance
Bertolotti Syndrome
Bertolotti syndrome, the association between an LSTV and low back pain, is controversial and has been both supported and disputed since Bertolotti first described it in 1917.2–4,8,9,12,13,15–28 Although not initially described, the low back pain of this syndrome is currently thought to be of varying etiologies, subsequently arising from different locations: 1) disk, spinal canal, and posterior element pathology at the level above a transition5,8,9,12,20,24,31; 2) degeneration of the anomalous articulation between an LSTV and the sacrum; 3) facet joint arthrosis contralateral to a unilateral fused or articulating LSTV30,32); and 4) extraforaminal stenosis secondary to the presence of a broadened transverse process (Figs 13–16).12,29–31,38 In most of the literature that supports Bertolotti syndrome, the implicated transitional segments are Castellvi types II-IV. Castellvi2 states that type I LSTVs are of no clinical significance and are a “forme fruste” and therefore have no relation to what was initially described as Bertolotti syndrome. However, Aihara et al39,40 determined that short and broad iliolumbar ligaments lend a protective effect to the L5-S1 disk space and potentially destabilize the L4-L5 level. There may be an association of such iliolumbar ligament morphology with broadened long transverse processes (Castellvi type I) (Fig 16). This could potentially lend some credence to an association of low back pain with a type I LSTV but requires further investigation.
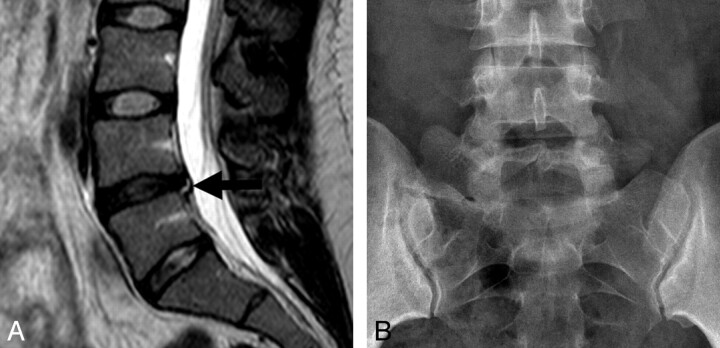
Fig 13.
Adjacent-level disease. Sagittal T2-weighted MR image (A) demonstrates disk desiccation with a small central protrusion and associated annular tear (black arrow) in a 25-year-old female patient with a Castellvi type IIa LSTV as seen on this AP radiograph (B).
Fig 14.
Adjacent-level disease in a 24-year-old woman. Sagittal T2-weighted MR image in a patient with a Castellvi type IIa LSTV demonstrates grade 1 anterolisthesis, disk desiccation, and disk bulging at the level above the transitional level.
Fig 15.
Contralateral facet arthrosis in a 45-year-old man. Coronal T1-weighted MR image in a patient with a Castellvi type IIa LSTV demonstrates severe facet arthropathy (white arrow) contralateral to the anomalous articulation.
Fig 16.
Degeneration of an anomalous articulation in an 84-year-old woman. Axial T1-weighted image demonstrates marked degeneration of the anomalous articulation on the right (white arrow) in a patient with a Castellvi type IIb LSTV.
In a series of 4000 patients, Tini et al10 reported no correlation between low back pain and transitional vertebrae. Elster5 found that the incidence of structural pathology (disk pathology, spinal and foraminal stenosis) did not differ in patients with LSTV compared with those without transitional vertebrae. However, the distribution of pathology was markedly different in that lesions occurred at the intervertebral disk space above the level of the transitional vertebra almost exclusively and never between the LSTV and the sacrum. Although Taskaynatan et al9 did not find an increased incidence of pathology in patients with LSTV, they reported increased severity of low back pain in patients with LSTV and an associated increase in nerve root symptoms.
Other studies of patients being imaged for low back pain or surgery for disk pathology demonstrated a greater than expected number of transitional vertebrae.2–4,8,15 Multiple studies have shown an increased incidence of disk pathology above LSTVs.2,5,31,40 Luoma et al8 reported an increased risk of early degeneration in the upper disk in young patients, but this change was obscured by age-related changes in the middle-aged population. Epstein et al41 described increased disk herniation in adolescents with spinal anomalies, including LSTV.
Transitional vertebrae likely affect the normal biomechanics of the lumbar spine. The lack of mobility at a fused transitional level or the decreased mobility at a partially fused or anomalously articulating vertebra lends stabilization to this level. A decreased prevalence of disk pathology was found in the disk below the transitional vertebral body.5,8,15 This may be explained by the altered biomechanics from the aberrant joints between the LSTV and sacrum. First, there is restricted motion between the transitional vertebra and sacrum due to the anomalous articulation and/or bony fusion.5 The load can, therefore, be effectively absorbed by the fused transverse process or the aberrant joint decreasing motion and relieving stress on the intervertebral disk. This results in preservation of disk integrity seen on MR imaging as normal bright signal intensity within the nucleus on T2-weighted sequences.11,42
The increased stability between an LSTV and the sacrum can potentially lead to hypermobility above the transitional segment, at the ipsilateral anomalous articulation5,38,40,43,44 and/or at the contralateral facet joint.30 Elster5 likened the hypermobility at the disk level above the LSTV to adjacent-level disease seen at spinal segments above and below postsurgical fusion masses or a block vertebra. Hypermobility and abnormal torque moments at the intervertebral disk are believed to place the disk and facet joints at increased risk of accelerated degeneration.5,31,40,45 Additionally, Aihara et al40 found that the iliolumbar ligaments above an LSTV were thinner and weaker, potentially further predisposing this level to hypermobility and premature degeneration. No difference has been reported in the incidence of spondylolysis or spondylolisthesis between patients with LSTVs and controls.2,5,10,46 It has been observed that in patients with lytic spondylolisthesis, there is a greater degree of slip seen at the L4–5 level above an L5 transition compared with the L5-S1 level above an S1 transition.47
Connolly et al,17 in a series of 48 patients with low back pain and an LSTV, showed increased uptake at the anomalous articulation between the transverse process of the LSTV and the sacrum in 81% of patients. All of these symptomatic patients had diarthrodial joints (Castellvi type II LSTV). This increased uptake was not demonstrated in patients with osseous fusion of the transverse process to the sacral ala. It can, therefore, be assumed that when fused, this stress is transferred superiorly or to the contralateral facet joint if the fusion is unilateral.
Contralateral facetogenic pain may be seen in patients with unilateral anomalous articulations or osseous fusion (Castellvi type IIa or IIIa). Analogous to cases in which the stress is dissipated to the level above, in these unilateral cases, torque forces are distributed across to the contralateral facet joint. Facet arthrosis can be seen on CT or radiographs as a degenerated-appearing joint with the typical findings of osteoarthrosis: joint space narrowing, cartilage loss, and osteophyte formation. MR imaging and nuclear medicine can more reliably identify the facet as a discrete source of pain when bone marrow edema signal intensity or increased tracer uptake is identified respectively.48
Extraforaminal stenosis leading to nerve root entrapment and radiculopathy has been reported in patients with an LSTV.29,49 Best imaged on coronal MR imaging, the nerve root may be seen compressed between the hyperplastic transverse process of the LSTV and the adjacent sacral ala.29 Furthermore, patients with nerve root symptoms and an LSTV are more likely to have disk prolapse at the level above the LSTV than those without an LSTV.29 Additionally, in the absence of spondylolisthesis, spinal stenosis is more likely to occur at the disk level above the LSTV.12 Assessing nerve root symptoms in patients with an LSTV is also complicated by the fact that there is associated variation of lumbosacral myotomes.44 When a sacralized L5 vertebral body is present, the L4 nerve root serves the usual function of the L5 nerve root; and similarly when a lumbarized S1 is present, the S1 nerve root functions as the L5 nerve root.3,50 McCulloch and Waddell51 demonstrated that the functional L5 nerve root always originates at the lowest mobile level of the lumbosacral spine. Knowledge of these variations by both the radiologist and referring clinician can help to explain confounding radicular symptoms.
Wrong-Level Spine Surgery
The accurate assessment of spinal segmentation is crucial in eliminating surgical and procedural errors because most wrong-level spine surgery occurs in patients with variant spine anatomy, including LSTVs.52 Often, surgical errors occur when MR imaging of the lumbar spine is reported without accompanying conventional radiographs11 or cervicothoracic MR localizers. Because intraoperative radiographs are used during spinal surgery for confirmation of disk level, it is important to correlate prior MR imaging with these radiographs. As important is obtaining high-quality intraoperative lateral radiographs. Lack of correlation by the operating surgeon of the intraoperative radiograph with the preoperative sagittal MR imaging can lead to the dreaded consequence of wrong-level spine surgery (Fig 17 ). To prevent this complication, it is imperative that there is communication between the radiologist and the surgeon regarding numbering of vertebral segments before surgery.
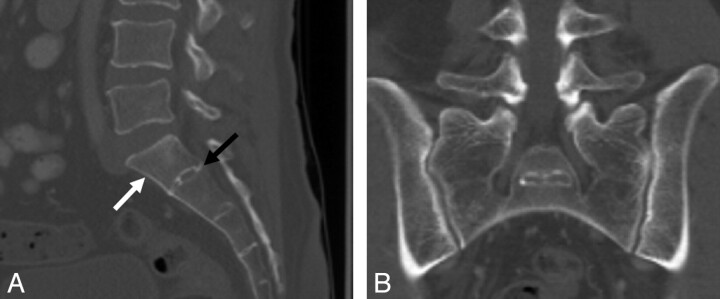
Fig 17.
Wrong-level spine surgery in a 55-year-old woman. A, Intraoperative radiograph demonstrates a localization device at what was believed to be the L3-L4 level based on misinterpretation of a sacralized L5 vertebral body (black arrow) as S1. B, Correlation with preoperative sagittal T2-weighted MR image better reveals the presence of the LSTV (white arrow) and, if used in combination with the intraoperative films, would have helped to avoid this surgical complication.
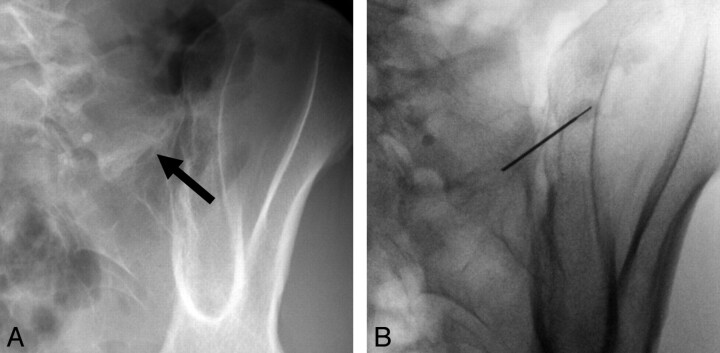
Treatment
Although there is no consensus on the clinical significance of LSTVs, several treatment strategies have been advocated. These include conservative nonsurgical management with local injection of anesthetic and corticosteroids within the pseudoarticulation or contralateral facet joint (Fig 18), radio-frequency ablation and surgical management with partial transverse process resection, and/or posterior spinal fusion. It is suggested that local anesthetic injection be part of the diagnostic work-up in patients with Bertolotti syndrome for whom surgery is being considered.44 Direct local anesthetic and steroid injection or surgical resection of the anomalous or contralateral facet joint has produced successful relief of pain and can yield valuable diagnostic information.30,38,44,53–55
Fig 18.
Injection of an anomalous articulation in a 48-year-old woman with right-sided low back pain and a Castellvi type IIa LSTV. A and B, Fluoroscopic spot images demonstrate degeneration of the anomalous articulation (arrow, A) and needle placement within the anomalous articulation for injection of anesthetic and corticosteroid (B).
Operative treatment is suggested in select patients. For example, resection of the transverse process may be beneficial for those who demonstrate pain truly emanating from a transitional joint and fail conservative treatment. If the pain source is from a degenerated disk above a transitional level, posterior fusion is an option as well.44 In a case report, Brault et el30 described successful treatment of contralateral facetogenic pain by resection of the ipsilateral anomalous articulation. Jonsson et al38 reported relief of pain in 9 of 11 patients following surgical resection of a unilateral LSTV pseudoarticulation. Ugokwe et al54 and Almeida et al55 similarly describe successful treatment after surgical resection. In a case series of 8 patients who underwent surgical resection of the unilateral anomalous articulation and 8 patients who underwent posterolateral fusion of the LSTV, Santavirta et al44 reported improvement in pain in 10 of 16 patients at 9-year follow-up without a difference between the fusion or resection groups. Finally, radio-frequency denervation is another possible treatment option and provided temporary relief of pain due to an anomalous articulation in a case report by Almeida et al.55
Conclusions
LSTVs are common anomalies of the spine necessitating the ability to accurately identify and number the affected segment. Although it has been long contested, there is fairly convincing evidence of an association of low back pain with LSTV. Knowledge of the biomechanical alterations within the spine caused by LSTVs will aid the radiologist in understanding and recognizing the imaging findings seen in patients with low back pain and a transitional segment. Additionally, a thorough understanding of the importance for both accurate enumeration of LSTV and communication to the referring clinician will help to avoid such dreaded complications as wrong-level spine surgery.
Acknowledgments
We thank Alissa Burge, MD, for her medical illustrations and Damon J. Spitz, MD, and Tal Rencus, MD, for their contributions to this article.
Abbreviations
- AP
anteroposterior
- LSTV
lumbosacral transitional vertebra
References
- 1. Bron JL, van Royen BJ, Wuisman PI. The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg 2007;73:687–95 [PubMed] [Google Scholar]
- 2. Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine 1984;9:493–95 [DOI] [PubMed] [Google Scholar]
- 3. Chang HS, Nakagawa H. Altered function of lumbar nerve roots in patients with transitional lumbosacral vertebrae. Spine 2004;29:1632–35 [DOI] [PubMed] [Google Scholar]
- 4. Delport EG, Cucuzzella TR, Kim N, et al. Lumbosacral transitional vertebrae: incidence in a consecutive patient series. Pain Physician 2006;9:53–56 [PubMed] [Google Scholar]
- 5. Elster AD. Bertolotti's syndrome revisited: transitional vertebrae of the lumbar spine. Spine 1989;14:1373–77 [PubMed] [Google Scholar]
- 6. Hahn PY, Strobel JJ, Hahn FJ. Verification of lumbosacral segments on MR images: identification of transitional vertebrae. Radiology 1992;182:580–81 [DOI] [PubMed] [Google Scholar]
- 7. Hughes RJ, Saifuddin A. Imaging of lumbosacral transitional vertebrae. Clin Radiol 2004;59:984–91 [DOI] [PubMed] [Google Scholar]
- 8. Luoma K, Vehmas T, Raininko R, et al. Lumbosacral transitional vertebra: relation to disc degeneration and low back pain. Spine 2004;29:200–05 [DOI] [PubMed] [Google Scholar]
- 9. Taskaynatan MA, Izci Y, Ozgul A, et al. Clinical significance of congenital lumbosacral malformations in young male population with prolonged low back pain. Spine 2005;30:E210–13 [DOI] [PubMed] [Google Scholar]
- 10. Tini PG, Wieser C, Zinn WM. The transitional vertebra of the lumbosacral spine: its radiological classification, incidence, prevalence, and clinical significance. Rheumatol Rehabil 1977;16:180–85 [DOI] [PubMed] [Google Scholar]
- 11. O'Driscoll CM, Irwin A, Saifuddin A. Variations in morphology of the lumbosacral junction on sagittal MRI: correlation with plain radiography. Skeletal Radiol 1996;25:225–30 [DOI] [PubMed] [Google Scholar]
- 12. Otani K, Konno S, Kikuchi S. Lumbosacral transitional vertebrae and nerve-root symptoms. J Bone Joint Surg Br 2001;83-B:1137–40 [DOI] [PubMed] [Google Scholar]
- 13. Peh WC, Siu TH, Chan JH. Determining the lumbar vertebral segments on magnetic resonance imaging. Spine 1999;24:1852–55 [DOI] [PubMed] [Google Scholar]
- 14. Seçer M, Muradov JM, Dalgiç A. Evaluation of congenital lumbosacral malformations and neurological findings in patients with low back pain. Turk Neurosurg 2009;19:145–48 [PubMed] [Google Scholar]
- 15. Wigh RE, Anthony HF, Jr. Transitional lumbosacral discs: probability of herniation. Spine 1981;6:168–71 [DOI] [PubMed] [Google Scholar]
- 16. Bertolotti M. Contribute alla conoscenza dei vizi di differenzazione del rachide con speciale reguardo all assimilazione sacrale della v lombare. La Radiologia Medica 1917;4:113–44 [Google Scholar]
- 17. Connolly LP, d'Hemecourt PA, Connolly SA, et al. Skeletal scintigraphy of young patients with low-back pain and a lumbosacral transitional vertebra. J Nucl Med 2003;44:909–14 [PubMed] [Google Scholar]
- 18. Dai L. Lumbosacral transitional vertebrae and low back pain. Bull Hos Jt Dis 1999;58:191–93 [PubMed] [Google Scholar]
- 19. Frymoyer JW, Newburg A, Pope MH, et al. Spine radiographs in patients with low-back pain: an epidemiological study in men. J Bone Joint Surg Am 1984;66:1048–55 [PubMed] [Google Scholar]
- 20. Hsieh CY, et al. Lumbosacral transitional segments: classification, prevalence, and effect on disk height. J Manipulative Physiol Ther 2000;23:483–89 [DOI] [PubMed] [Google Scholar]
- 21. Mann DC, Keene JS, Drummond DS. Unusual causes of back pain in athletes. J Spinal Disord 1991;4:337–43 [DOI] [PubMed] [Google Scholar]
- 22. Nachemson A. Towards a better understanding of low-back pain. Rheumatol Rehabil 1975;14:129–43 [DOI] [PubMed] [Google Scholar]
- 23. Peterson CK, Bolton J, Hsu W, et al. A cross-sectional study comparing pain and disability levels in patients with low back pain with and without transitional lumbosacral vertebrae. J Manipulative Physiol Ther 2005;28:570–74 [DOI] [PubMed] [Google Scholar]
- 24. Quinlan JF, Duke D, Eustace S. Bertolotti's syndrome: a cause of back pain in young people. J Bone Joint Surg Br 2006;88:1183–86 [DOI] [PubMed] [Google Scholar]
- 25. Santiago FR, Milena GL, Herrera RO, et al. Morphometry of the lower lumbar vertebrae in patients with and without low back pain. Eur Spine J 2001;10:228–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Schuller . Die Sakralisation des 5. Lendenwirnels mit besonderer Berucksichtigung ihrer klinischen Bewertung. Beitr Klin chir 1924;131:281–300 [Google Scholar]
- 27. Steinberg EL, Luger E, Arbel R, et al. A comparative roentgenographic analysis of the lumbar spine in male army recruits with and without lower back pain. Clin Radiol 2003;58:985–89 [DOI] [PubMed] [Google Scholar]
- 28. Tabor ML. Statistical study of anomalies of the lumbar and lumbosacral vertebrae: radiologic findings from 7,500 orthopedic patients [in French]. J Radiol Electrol Med Nucl 1968;49:713–18 [PubMed] [Google Scholar]
- 29. Hashimoto M, Watanabe O, Hirano H. Extraforaminal stenosis in the lumbosacral spine: efficacy of MR imaging in the coronal plane. Acta Radiol 1996;37:610–13 [DOI] [PubMed] [Google Scholar]
- 30. Brault JS, Smith J, Currier BL. Partial lumbosacral transitional vertebra resection for contralateral facetogenic pain. Spine (Phila Pa 1976). 2001;26:226–29 [DOI] [PubMed] [Google Scholar]
- 31. Vergauwen S, Parizel PM, van Breusegem L, et al. Distribution and incidence of degenerative spine changes in patients with a lumbo-sacral transitional vertebra. Eur Spine J 1997;6:168–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nicholson AA, Roberts GM, Williams LA. The measured height of the lumbosacral disc in patients with and without transitional vertebrae. Br J Radiol 1988;61:454–55 [DOI] [PubMed] [Google Scholar]
- 33. Hughes RJ, Saifuddin A. Numbering of lumbosacral transitional vertebrae on MRI: role of the iliolumbar ligaments. AJR Am J Roentgenol 2006;187:W59–W65 [DOI] [PubMed] [Google Scholar]
- 34. Basadonna PT, Gasparini D, Rucco V. Iliolumbar ligament insertions: in vivo anatomic study. Spine 1996;21:2313–16 [DOI] [PubMed] [Google Scholar]
- 35. Rucco V, Basadonna PT, Gasparini D. Anatomy of the iliolumbar ligament: a review of its anatomy and a magnetic resonance study. Am J Phys Med Rehabil 1996;75:451–55 [DOI] [PubMed] [Google Scholar]
- 36. Bressler EL. Numbering of lumbosacral transitional vertebrae on MRI. AJR Am J Roentgenol 2007;188:W210, author reply W211 [DOI] [PubMed] [Google Scholar]
- 37. Lee CH, Seo BK, Choi CY, et al. Using MRI to evaluate anatomic significance of aortic bifurcation, right renal artery, and conus medullaris when locating lumbar vertebral segments. AJR Am J Roentgenol 2004;182:1295–300 [DOI] [PubMed] [Google Scholar]
- 38. Jonsson B, Stromqvist B, Egund N. Anomalous lumbosacral articulations and low back pain: evaluation and treatment. Spine (Phila Pa 1976) 1989;14:831–34 [DOI] [PubMed] [Google Scholar]
- 39. Aihara T, Takahashi K, Ono Y, et al. Does the morphology of the iliolumbar ligament affect lumbosacral disc degeneration? Spine 2002;27:1499–503 [DOI] [PubMed] [Google Scholar]
- 40. Aihara T, Takahashi K, Ogasawara A, et al. Intervertebral disc degeneration associated with lumbosacral transitional vertebrae: a clinical and anatomical study. J Bone Joint Surg Br 2005;87:687–91 [DOI] [PubMed] [Google Scholar]
- 41. Epstein JA, Epstein NE, Marc J, et al. Lumbar intervertebral disk herniation in teenage children: recognition and management of associated anomalies. Spine 1984;9:427–32 [DOI] [PubMed] [Google Scholar]
- 42. Desmond RM, Buirski G. Magnetic resonance appearances of developmental disc anomalies in the lumbar spine. Australas Radiol 1993;37:21–29 [DOI] [PubMed] [Google Scholar]
- 43. Avimadje M, Goupille P, Jeannou J, et al. Can an anomalous lumbo-sacral or lumbo-iliac articulation cause low back pain? A retrospective study of 12 cases. Rev Rheum Engl Ed 1999;66:35–39 [PubMed] [Google Scholar]
- 44. Santavirta S, Tallroth K, Ylinen P, et al. Surgical treatment of Bertolotti's syndrome: follow-up of 16 patients. Arch Orthop Trauma Surg 1993;112:82–87 [DOI] [PubMed] [Google Scholar]
- 45. Keim HA. Transitional vertebrae and Bertolloti's syndrome. In: Proceedings of the 15th Annual Meeting of the Scoliosis Research Society, Chicago, Illinois. September 17–19, 1980 [Google Scholar]
- 46. Cinotti G, Postacchini F, Fassari F, et al. Predisposing factors in degenerative spondylolisthesis: a radiographic and CT study. Int Orthop 1997;21:337–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kim NH, Suk KS. The role of transitional vertebrae in spondylolysis and spondylolytic spondylolisthesis. Bull Hosp Jt Dis 1997;56:161–66 [PubMed] [Google Scholar]
- 48. Friedrich KM, Nemec S, Philipp P, et al. The prevalence of lumbar facet joint edema in patients with low back pain. Skeletal Radiol 2007;36:755–60 [DOI] [PubMed] [Google Scholar]
- 49. Abe E, Sato K, Shimada Y, et al. Anterior decompression of foraminal stenosis below a lumbosacral transitional vertebra: a case report. Spine (Phila Pa 1976) 1997;22:823–26 [DOI] [PubMed] [Google Scholar]
- 50. Kim YH, Lee PB, Lee CJ, et al. Dermatome variation of lumbosacral nerve roots in patients with transitional lumbosacral vertebrae. Anesth Anelg 2008;106:1279–83 [DOI] [PubMed] [Google Scholar]
- 51. McCulloch JA, Waddell G. Variation of the lumbosacral myotomes with bony segmental anomalies. J Bone Joint Surg Br 1962;62:475–80 [DOI] [PubMed] [Google Scholar]
- 52. Wigh RE. The thoracolumbar and lumbosacral transitional junctions. Spine 1980;5:215–22 [DOI] [PubMed] [Google Scholar]
- 53. Marks RC, Thulbourne T. Infiltration of anomalous lumbosacral articulations: steroid and anesthetic injections in 10 back pain patients. Acta Orthop Scand 1991;62:139–41 [DOI] [PubMed] [Google Scholar]
- 54. Ugokwe KT, Chen TL, Klineberg E. Minimally invasive surgical treatment of Bertolotti's syndrome: case report. Neurosurgery 2008;62:454–55 [DOI] [PubMed] [Google Scholar]
- 55. Almeida DB, Mattei TA, Sória MG, et al. Transitional lumbosacral vertebrae and low back pain: diagnostic pitfalls and management of Bertolotti's syndrome. Arq Neuropsiquiatr 2009;67:268–72 [DOI] [PubMed] [Google Scholar]