Abstract
BACKGROUND AND PURPOSE:
The HydroCoil is an expansile hydrogel coil designed to produce a greater degree of volumetric packing within cerebral aneurysms when compared with bare platinum coils. This increased packing is, in turn, believed to decrease the risk of recurrence within aneurysms and hence the risk of their rupture in the long term. The aim of this work was to assess whether the use of HydroCoils and the proportion of HydroCoil used have any influence on the subsequent occlusion and recurrence rates of treated aneurysms.
MATERIALS AND METHODS:
A retrospective study was performed of 328 patients during 5 years at a single institution. The initial angiographic and follow-up angiographic occlusion rates were recorded as were any procedural complications. The proportion of HydroCoil used was described as the relative amount of HydroCoil length to the total coil length used during an aneurysm treatment, thus forming 4 groups: 0%–19%, 20%–49%, 50%–69%, 70%–100%, and the subgroups with 100%.
RESULTS:
Two hundred seventy patients had angiographic follow-up during an average of 13 months. The overall risk of permanent neurologic deficit and death was 3%. The rate of complete occlusion was 31% immediately postcoiling and 64.8% on follow-up. At the latest follow-up, 25.6% had residual necks and 9.6% had residual aneurysms. There was a statistically significant trend for HydroCoils to produce greater occlusion rates on follow-up when >70% HydroCoil was used (P = .025). The overall rate of recurrence for all aneurysms as a group was 15.5%. The retreatment rate was 6.6%. There has been 1 rebleed in the 328 patients.
CONCLUSIONS:
The overall results following the use of HydroCoils to occlude aneurysms compare well with those in other reported series. HydroCoils do produce a statistically significantly greater rate of occlusion when >70% of total aneurysm coil length is HydroCoil compared with coiling with <20% HydroCoil. There was no significant difference, however, in the recurrence or retreatment rate when comparing these groups.
The endovascular treatment of aneurysms is, by now, a well-established and proved alternative to surgical clipping in the treatment of aneurysms.1,2 However, its greatest limitation is the rate of aneurysm regrowth necessitating further treatment, which compares poorly with a permanent surgical solution. Quantification of this varies, but the rate of recurrence is on the order of 14%–21%,3,4 which requires further treatment in an additional 6%–10.3%.5,6
Bioactive coils are designed to provide greater occlusion of an aneurysm, with a resultant decrease in the recurrence, retreatment, and rehemorrhage. The HydroCoil (MicroVention Terumo, Aliso Viejo, California) produces this effect by means of a coating of hydrogel, which expands up to approximately 3 times its original diameter on contact with blood. Initial results on animal models7 and by the same research group in humans8 produced favorable results, with an increase in volumetric packing attenuation in the latter from 32% to 73% in 11 subjects. While the placement of these coils is not associated with any increase in periprocedural complications,9 the long-term efficacy is less well-known. This single-center study further evaluates the safety and efficiency of the use of HydroCoils in a large group of patients compared with previous experience in the literature using bare platinum coils. This study assesses the initial and follow-up occlusion rates and recurrences in HydroCoil cases within a single center for 5 years. Using internal subgroup comparisons, we evaluated the effect of the amount of HydroCoil on occlusion rates.
Materials and Methods
The study was approved by the institutional ethics review board. We performed a retrospective consecutive single-center review of all patients coiled either wholly or partially with HydroCoils at a single institution during almost a 5-year period, July 2003 to April 2008. Of our complete cohort of 328 patients, 100 had been the basis of a previously published work from this same hospital on the same subject.10 In our institution, all patients have procedural details, hospital clinical course, and clinical and angiographic follow-up outcomes recorded in an electronic data base. This data base was the principal information source, with retrieval of patient charts in certain but not all cases. All angiographic imaging was reviewed by 2 experienced attending interventional neuroradiologists (P.R.B, J.P.T). The decision to use HydroCoils in an aneurysm was determined by the neuroradiologist at the time of coiling (P.R.B, J.P.T). The primary reason for excluding the use of HydroCoils was the expectation that the coil may not be safely placed within the aneurysm. This decision was based on a number of factors, including the following: the requirement of a specific coil shape or size (not in the HydroCoil range), catheter stability, difficulty in placing the previous coil, and the anticipated difficulty in placing a coil without excessive manipulation. The HydroCoils were steamed before microcatheter entry. The total length of HydroCoil used per aneurysm was recorded. The volume of the aneurysm or packing attenuation was not measured. The proportion of HydroCoil used when coiling an aneurysm was the percentage of that HydroCoil length relative to the total coil length used in a single aneurysm. Proportions of HydroCoils were recorded as 0%–19%, 20%–49%, 50%–69%, and >70%. In addition, almost half of the last group was actually coiled with 100% HydroCoil, therefore representing a subgroup.
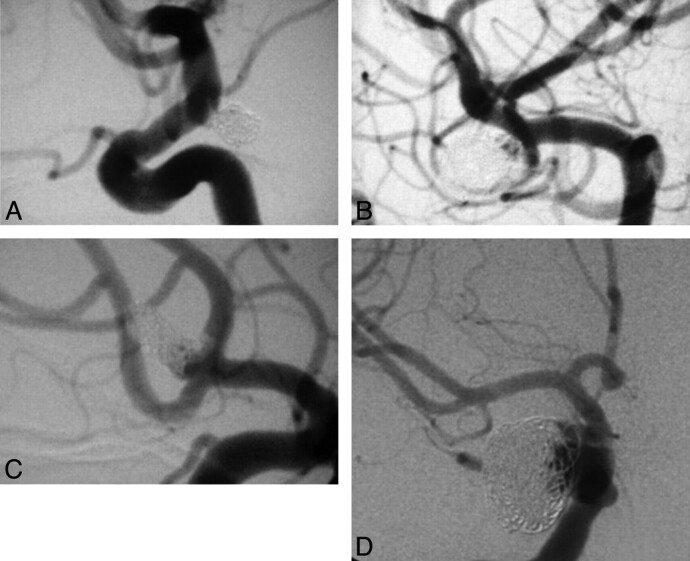
All patients were assigned a rate of occlusion on the immediate postcoiling angiogram at the time of the procedure and again at all subsequent follow-up angiography sessions. The occlusion rate assigned was based on a consensus result from the same 2 experienced interventional neuroradiologists (P.R.B, J.P.T). The occlusion scale used was a modification of the standard Raymond-Roy classification. Class 1 was complete occlusion; Class 2 was divided into 2A and 2B depending on whether the neck remnant was predominantly interstitial, A, or, without coils, B, “the dog ear.” Class 3 was incomplete or residual aneurysm (Fig 1).
Fig 1.
Angiographic classification system was a modified Raymond-Roy classification divided into the following groups: complete occlusion (A); neck remnant, interstitial (B); neck remnant with no coils (C); and residual aneurysm (D).
In addition to the actual occlusion rate scored on the angiograms, the follow-up angiogram was further categorized. This consisted of stating whether the follow-up angiogram appearance represented the following: persistent 100% occlusion, progression to 100% occlusion, progressive thrombosis but remaining <100% occluded, stable remnant, or recurrence, all relative to the initial immediate postcoiling angiography. Recurrence was described as any morphologic deterioration in the appearance and was divided into major or minor. Any aneurysm with an occlusion rate of class 3 on follow-up having previously been class 2 or 1 was labeled as a major recurrence. Similarly an aneurysm that was initially class 3 and developed anything more than the slightest change was also described as having major recurrence. Minor recurrence referred to a change from complete occlusion to a neck remnant or enlargement of a neck remnant that did not change to a residual aneurysm. The standard follow-up period was 1 year by cerebral angiography. Further follow-up beyond 1 year in a number of cases was performed by either formal angiography or MR angiography.
The size of our cohort of patients and the separate proportions of HydroCoil used afforded us the possibility of performing subgroup comparison. Therefore, those coiled with 0%–19% HydroCoil would essentially act as a surrogate control group because they contained the least amount of HydroCoil and the greatest proportion of bare platinum coil. This group would be compared with those with aneurysms containing the larger proportion of HydroCoil (>70%). Statistical analysis was performed on categoric data by using χ2 testing on statistical software (SigmaStat 3.0; SPSS, Chicago, Illinois). The P value < .05 was taken to be statistically significant. Our pretest hypotheses and, therefore, primary outcome measures were the following: 1) There would be a statistically significant difference in the number of aneurysms completely occluded on follow-up when comparing the groups containing <50% HydroCoil versus >50%, and in those coiled with 0%–19% compared with those coiled with >70% HydroCoil at follow-up angiography, and 2) we expected that there would be fewer angiographic recurrences when comparing these same groups.
Results
Demographics
In total, aneurysms in 328 patients were coiled either totally or partially with HydroCoils in Beaumont Hospital within our study period. The patient group had a mean age of 53.6 years and consisted of a mostly female-to-male ratio, 67.7%; 32.3%, respectively. Within our cohort of patients, most aneurysms were acutely ruptured (205, 62.5%), with the remainder unruptured (123, 32.5%). Of this latter group, 17 (5.4%) were recoiling procedures of previously coiled aneurysms, though 1 was coiling of a previously clipped aneurysm. Nineteen (6%) presented with symptoms related to mass effect, and the remainder were incidental (85, 26.1%). In 66 (19.9%) cases, an assist device was used, usually a balloon, with stent-assisted coiling occurring in 5 (1.5%) cases. The size of the aneurysms was divided into 3 distinct categories: 2–4.9 mm, 5–9.9 mm, and ≥10 mm. These groups contained 122, 133, and 71 patients, respectively. Most aneurysms of the cohort of patients, therefore, were between 5 and 9.9 mm. The dome-to-neck ratio was categorized as greater or less than 1.5:1. Within our cohort, 151 (46%) had a dome-to-neck ratio of <1.5:1 and 177 (54%) had a ratio of ≥1.5:1.
Complications
Adverse events were described as either procedural or disease-related. Altogether there were 53 periprocedural complications, a rate of 16.1%; 42 (80.6%) were in ruptured aneurysms and the remainder 11 (20.4%) were in unruptured ones. The most frequent complication was coil protrusion 15 (4.6%). Second, thromboembolism occurred in 13 (4%). The risk of permanent physical deficit was 1.5% (excluding deaths). Total deaths were 18, with 15 occurring early, in <30 days. Of all deaths, 5 were procedure-related (1.5%): Two patients had an on-table rupture, 2 had large thromboembolic events with significant sequelae and subsequent death, and 1 was due to an early rebleed. This was the only rebleed of our cohort and occurred in a patient in whom the initial coiling was complicated by rupture and the initial occlusion rate was class 3 with rehemorrhage within 30 days from the same aneurysm.
Follow-Up
Overall, 270 (82.3%) of our patients had angiographic follow-up. Of the 58 not followed, 16 (4.9%) died by the time of follow-up, 16 (4.9%) were followed elsewhere, 21 (6.4%) were scheduled for follow-up, and 5 (1.5%) declined follow-up. The shortest follow-up time was 1 month with the longest being 54 months. This very short 1-month period of follow-up was unintentional due to the patient's re-presentation with rehemorrhage. The mean follow-up period was 13 months, with a median of 12 months.
Coils Used
Of 1593 coils placed in all cases, HydroCoils accounted for 55% of the total number of coils but 47.7% of the total length. The mean number of HydroCoils per case was 2.7, with each aneurysm containing on average 24 cm of coil. As stated previously, the following were the 4 principal subdivisions of coil based on the proportion of HydroCoil used: 0%–19%, 20%–49%, 50%–69%, and >70%. In addition, there was the subgroup of >70% coiled in their entirety by HydroCoils. From our data, there was a clear tendency to use fewer HydroCoils during our early experience. When reviewed, it was evident that 30 of the 46 patients in group 0%–19% were treated in the first 2 years of our retrospective review. This finding reflects growing confidence in the use of HydroCoil and the fact that the first HydroCoils were available only in HydroCoil 14 and HydroCoil 18 and were more difficult to use than the subsequent HydroCoil 10.
Within the individual HydroCoil groups, 23 (43.4%) aneurysms coiled by >70% HydroCoil were between 2 and 5 mm, but this was not statistically significant when compared with the group coiled by 0%–19% HydroCoil, in which only 9 (23.7%) measured 2–5 mm (P = .86). However, the subgroup coiled by using 100% HydroCoil had actually 15 (57.7%) of its cases made up of small aneurysms of 2–4.9 mm, and this amount was statistically significant when compared with the smaller group, 0%–19% (P = .013).
Hydrocephalus
Two hundred five patients did not require any postprocedural imaging. Of the remaining 123 who did, 81 had no hydrocephalus and 42 had hydrocephalus. None of the cases of hydrocephalus were in the electively treated group. However, 1 patient developed hydrocephalus following an initial presentation of a few weeks' history of painful third nerve palsy with no evidence of subarachnoid hemorrhage on CT; this aneurysm was coiled with 19% HydroCoil. This hydrocephalus was discovered 6 months postprocedure after the patient reported persistent headache. A ventricular shunt was placed, and the patient's symptoms improved shortly thereafter.
Occlusion Rates
The initial postangiographic occlusion rates and the follow-up occlusion rates are shown in Table 1. The total rate of initial complete occlusion was 31%, which increased to 64.8% on follow-up angiography. Of the 84 patients with an initial complete occlusion, 9 (10.7%) developed recurrence on subsequent angiography. This compares with recurrence in 7 (7%) for the 2A group, 16 (24.6%) for 2B, and 10 (23.2%) for the incomplete group. This result does demonstrate a trend toward a greater rate of recurrence with a worse initial occlusion rate. Similarly, the progression to complete occlusion occurred in 77% of the 2A category and 30% of the 2B category, therefore being better than the initial occlusion rate.
Table 1:
Comparison of initial and follow-up occlusion classes of aneurysms for each HydroCoil group
| % | Initial |
Follow-Up |
||||||
|---|---|---|---|---|---|---|---|---|
| 1 (%) | 2A (%) | 2B (%) | 3 (%) | 1 (%) | 2A (%) | 2B (%) | 3 (%) | |
| 0–19 | 10 (26.3) | 10 (26.3) | 9 (23.7) | 9 (23.7) | 20 (52.6) | 11 (28.9) | 4 (10.5) | 3 (7.9) |
| 20–49 | 33 (33) | 32 (32) | 22 (22) | 13 (13) | 61 (61) | 9 (9) | 18 (18) | 12 (12) |
| 50–69 | 29 (36.7) | 27 (34.2) | 8 (10.1) | 15 (19) | 53 (67.1) | 8 (10.1) | 11 (29) | 7 (8.8) |
| >70 | 2 (22.6) | 22 (41.5) | 13 (24.5) | 6 (11.3) | 41 (77.3) | 1 (1.9) | 7 (13.2) | 4 (7.5) |
| 100 | 3 (11.5) | 11 (42.3) | 10 (38.4) | 2 (7.8) | 19 (73) | 1 (3.8) | 4 (15.4) | 2 (7.8) |
| Total | 84 (31) | 91 (33.7) | 52 (19.2) | 43 (15.9) | 175 (64.8) | 29 (10.7) | 40 (14.8) | 26 (9.6) |
The performance of the various HydroCoil categories can be seen from Table 2. The percentages quoted refer to the population that was completely followed. The rate of progression to 100% occlusion does increase with the percentage of HydroCoil used—that is, when >70% HydroCoil was used, 56.6% of cases would show progression to complete occlusion on follow-up angiography as opposed to 36.8% in the smaller 0%–19% group. However, this was not statistically significant (P = .099). The number of aneurysms completely occluded on follow-up (Table 1) was 175 of 270 (65%), so these patients had either always been 100% occluded (persistent occlusion) or they had progressive thrombus during the interim, with now 100% occlusion on follow-up. Within the 0%–19% group (n = 20), 38 (55.3%) aneurysms were completely occluded at follow-up as opposed to 41 (77.3%) of those coiled with >70% HydroCoil, a result that was statistically significant (P = .025), thus demonstrating that with the greater the amount of HydroCoil used, complete occlusion will more likely be achieved on follow-up. In the group 0%–19%, of the 20 aneurysms that were completely occluded on follow-up, 13 (65%) were from acute ruptures and 7 were from unruptured aneurysms. In the >70% group, 23 (56%) of the 41 were acute ruptures and 18 were unruptured.
Table 2:
Angiographic change according to percentage HydroCoil
| % | Persistent,a No. (%) | Progression,b No. (%), | Stable Remnant | Progressive,c No. (%) | Regrowth, No. (%) |
|---|---|---|---|---|---|
| 0–19 (n = 38) | 6 (15.8) | 14 (36.8) | 8 (21) | 3 (8.3) | 7 (18.4) |
| 20–49 (n = 100) | 31 (31) | 31 (31) | 16 (16) | 4 (4) | 18 (18) |
| 50–69 (n = 79) | 27 (34.2) | 24 (30.4) | 14 (17.7) | 5 (6.3) | 9 (11.4) |
| >70 (n = 53) | 11 (20.7) | 30 (56.6) | 2 (3.80) | 2 (3.8) | 8 (15.1) |
| 100 (n = 26) | 3 (11.5) | 16 (61.5) | 2 (7.7) | 1 (3.8) | 4 (15.4) |
Persistent 100% occlusion.
Progression to 100% occlusion.
Progressive nonocclusive thrombus.
Recurrence and Retreatment
Table 3 shows that there were 42 (15.5%) recurrences overall with the percentage of recurrences in each HydroCoil group not being very different from each other: 18.4%, 18%, 11.4% and 15.1%, respectively (no statistical significance). Of these recurrences, 20 were classified as minor and 22 were major. The proportion of major recurrences in each group was 7.9%, 9%, 6.3%, and 9.4% with no statistical significance between our groups namely <50% versus >50% and 0%–19% versus >70%. Notably the proportion of large-neck aneurysms ≤1.5 in each group was 49%, 48%, 44%, and 43%, respectively. The rate of recurrence in aneurysms ≥10 mm was 42% and 7.1% in those of <10 mm. Of all major recurrences, 13 were in unruptured and 9 were in ruptured aneurysms, whereas for minor recurrences, almost all 17 were acutely ruptured and 3 minor recurrences developed in unruptured aneurysms.
Table 3:
Recurrence rate, with rate of retreatment, and initial occlusion class
| No. | Retreated | Followed | Rehemorrhage | 1 | 2A | 2B | 3 | |
|---|---|---|---|---|---|---|---|---|
| Large regrowtha | 22 | 17 | 4 | 0 | 1 | 0 | 4 | 17 |
| Small regrowth | 20 | 1 | 18 | 1 | 8 | 4 | 6 | 4 |
One patient was too elderly.
Of these major recurrences, all were apparent on the initial follow-up angiogram, and 15 of the 18 occurred in aneurysms of >10 mm. Most major recurrences, 17 of 22 (77.3%), had a grade III occlusion rate initially on their immediate postcoiling angiography. The single large regrowth in the small aneurysm of 2–4.9 mm was confounded by the fact the procedure was stopped early due to complications, with subsequent undercoiling of the aneurysm. Of these major recurrences, 4 proved to be stable between 36 and 48 months, 13 were recoiled or due to be recoiled, 2 were clipped, 2 underwent carotid occlusion, and 1 patient was unsuitable clinically for further treatment. In comparison, those with a minor recurrence, 10 of 22, were in patients with aneurysms of >10 mm. Of the minor recurrences, 1 was retreated, therefore giving us an overall retreatment rate of 6.6% (18 of 270).
Discussion
To date, there have been at least 11 published reports in peer-reviewed journals that have addressed the efficacy of HydroCoils in endovascular coiling.9–19 These same articles were recently the subject of an evidence-based review of bioactive coils by White and Raymond,20 which revealed that on the evidence-based hierarchy, the published data were inadequate, only achieving a Cochrane level C. The downfall of many of these studies as described by the authors of this latter publication was the inaccurate and incomplete reporting of data. We have attempted to overcome some of the deficiencies highlighted by the way we have reported our data.
To our advantage, all procedures were performed in a single center by the same 2 interventional neuroradiologists. There were some similarities in our cohort to the initial procedural safety and operator-assessed efficacy results from the ongoing HELPS trial, which were published recently.21 These included the fact that aneurysm size was divided into 3 distinct categories and HydroCoil proportions were based on coil length, with angiographic outcome reported only for those with complete angiographic follow-up. The number of patients in their HydroCoil group was 249, similar to our 270 patients. Our overall procedural mortality was 1.5% with 5 procedure-related deaths. Procedure-related adverse events numbered 53 (16.1%), with a risk of permanent deficit of 1.5%. Similarly, this initial HELPS publication reported 5 procedural deaths in the hydrogel arm, with an overall complication rate of 17.4%.
HydroCoils are platinum coils with a hydrogel (hydrophilic acrylic polymer) coating. The perceived advantage of HydroCoils is the ability to increase the packing volume within an aneurysm relative to bare platinum coils. The packing attenuation has been shown to be inversely related to the overall size of coiled aneurysms.22,23 Aneurysm volumetrics and coil-packing attenuation were deliberately omitted in our study on the basis of the potential error associated with their calculation, because they rely on certain assumptions about the physical dimensions of aneurysms24 and the behavior of the hydrogel. This problem had been previously identified by the HEAL 2 authors,9 who found, like us, that the packing attenuation would have been based on observed linear measurements.
The overall recurrence risk from our study was 15.6% (42/270). There was a similar rate of total recurrence for groups using 0%–19% HydroCoil and >70% HydroCoil, 7 (18.4%) and 8 (15.1%), respectively. The data are contrary to those of HEAL, which did not see any regrowth in aneurysms coiled with >75% coil length. However in the HEAL study, only small, <10 mm, aneurysms were included in this subgroup analysis.9 If we were to examine our 42 patients with aneurysms of <10 mm coiled with >70% HydroCoil in the same fashion, the overall recurrence rate would be 3/20 for small recurrences and 0/22 for large recurrences. In the HydroCoil group of Bernstein et al,15 though only 53 patients were angiographically followed, the recurrence in aneurysms <10 mm was 0/23 and 6/22 in aneurysm of >10 mm. A more recently published reference was a large review of 121 patients coiled with HydroCoils, which showed that there was a 17.7% recurrence in aneurysms <10 mm and 28.6% in those >10 mm, irrespective of the percentage of HydroCoil used in these same studies. The overall retreatment rate was 10.7%, though the average aneurysm size was quite large, 9.3 mm.19 This increased propensity for recurrence in larger aneurysms has previously been proved in non-HydroCoil groups.25,26
This is the largest reported HydroCoil patient group followed to date, and we have demonstrated a low rate of recurrence compared with the literature on coiling to date. Using an internal surrogate control, we have shown that HydroCoils are effective in achieving an increase in the number of aneurysms with complete occlusion on follow-up. This is associated with a very low risk of rehemorrhage.27 We found that there was a statistically significant difference in the propensity of aneurysms in class 2B to be occluded on follow-up when coiled with >70% HydroCoil versus <20%, namely 77.3% and 55.3%. This was found to be independent of the fact that there were a greater proportion of aneurysms that were <5 mm in the group coiled with >70% HydroCoil. HydroCoils do offer an improved progression to occlusion of aneurysms when the percentage of HydroCoil is high, a result that is independent of the aneurysm size. Complete occlusion in itself, while certainly decreasing the risk of recurrence, certainly does not negate this risk of recurrence.
Other long-term studies report that the risk of rehemorrhage is very low, even with morphologic change.28 The primary goal of aneurysm treatment is the prevention of rebleeding. The rate of rebleeding following aneurysm coiling is low. In the International Subarachnoid Aneurysm Trial, 1005 patients had aneurysms coiled. There were 24 rebleeds in the first year and 10 more at the latest follow-up (mean, 9 years).29 We had 1 rebleed from an acutely ruptured aneurysm of 328 aneurysms in the 6 years since the first HydroCoil was used in our institution.
Recent concerns raised in relation to the “safety and efficacy” of these coils are based on heterogeneous and incomplete data from the published studies.20 HydroCoils are safe, and initial procedural results from the HELPS study showed no significant difference in the complication rate in a properly controlled study.21 This study agrees with ours in demonstrating a low risk of adverse procedure-related clinical complications. The real issue is whether HydroCoils are effective initially and long-term, and in the absence of the long-awaited complete HELPS results, no randomized controlled trial exists to assess this question. Although not a randomized trial, our study shows good long-term occlusion rates.
This work has the inherent disadvantage of being a single-center nonrandomized study with self-assessment in terms of angiographic occlusion rates. Although the results do not have the same clinical impact as would be achieved from a randomized controlled trial, we believe that there is merit in demonstrating the outcomes of following the introduction of a modified form of an existing device. The assessment of the rate of occlusion is clearly imprecise. The Raymond-Roy classification seems now to be the most widely accepted mechanism of assessment. It is, however, clearly open to interobserver variability. Although we have not used a core laboratory for evaluating our angiographic outcomes, we have attempted to be as objective as possible. There is some advantage in having the occlusion rate assessed by the person who has the best anatomic understanding of the particular aneurysm and its relation to the parent artery and overlapping branches, having studied the 3D angiograms and dynamic angiographic images. This person is most likely to be the one who performed the study.
The decision to retreat an aneurysm remnant following coiling is subjective, with differences in opinion often being found between clinicians whether they be surgeons or radiologists. This subjectivity was nicely demonstrated in a presentation by Dr Cloft at the World Federation of Interventional and Therapeutic Neuroradiology, in Montreal in 2009.30 In our institution, all cases are discussed at a multidisciplinary team meeting attended by vascular neurosurgeons and interventional neuroradiologists.
Conclusions
This large single-center experience with the use of HydroCoils in combination with other coils compares favorably with other previously published experiences of aneurysm treatment. The clinical outcome was good, and a high level of satisfactory aneurysm occlusion was obtained. There was a low rate of rebleeding, recurrence, and need for retreatment. For many, the bottom line in the efficacy of HydroCoils or any treatment is solely whether the treatment decreases the rate of recurrence and, more important, whether it decreases the rate of retreatment. However, recurrence is a multivariate phenomenon, which has many influences. To judge the efficacy of HydroCoils solely on the basis of recurrence is perhaps an oversimplification of what is undoubtedly a complex problem. The truth about HydroCoils lies in the results of a large randomized control study. For now, our opinion is that HydroCoils certainly do assist in aneurysm occlusion, potentially 1 important facet of recurrence, but on their own, they are unable to prevent it.
Acknowledgments
We thank Sinead Duff and Deirdre Daly for their continuous help throughout this study.
Abbreviations
- HEAL
HydroCoil for Endovascular Aneurysm Occlusion
- HELPS
HydroCoil Endovascular Aneurysm Occlusion and Packing Study
Footnotes
Paper previously presented at: Annual Meeting of the American Society of Radiology, May 16–19, 2009; Vancouver, British Columbia, Canada and 10th Congress of the World Federation of Interventional and Therapeutic Neuroradiology, June 22–July 3, 2009; Montreal, Quebec, Canada.
References
- 1. Molyneux AJ, Kerr RS, Yu LM, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet 2005;366:809–17 [DOI] [PubMed] [Google Scholar]
- 2. Weibers DO, Whisnant JP, Huston J, 3rd, et al. for the International Study of Unruptured Intracranial Aneurysms Investigators . Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 2003;362:103–10 [DOI] [PubMed] [Google Scholar]
- 3. Cognard C, Weill A, Spelle L, et al. Long-term angiographic follow-up of 169 intracranial berry aneurysms occluded with detachable coils. Radiology 1999;212:348–56 [DOI] [PubMed] [Google Scholar]
- 4. Raymond J, Guilbert F, Weill A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke 2003;34:1398–403 [DOI] [PubMed] [Google Scholar]
- 5. Ferns SP, Sprengers ME, van Rooij WJ, et al. Coiling of intracranial aneurysms: a systematic review on initial occlusion and reopening and retreatment rates. Stroke 2009;40:e523–29 [DOI] [PubMed] [Google Scholar]
- 6. Gallas S, Januel AC, Pasco A, et al. Long-term follow-up of 1036 cerebral aneurysms treated by bare coils: a multicentric cohort treated between 1998 and 2003. AJNR Am J Neuroradiol 2009;30:1986–92. Epub 2009 Aug 13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kallmes DF, Fujiwara NH. New expandable hydrogel-platinum coil hybrid device for aneurysm embolization. AJNR Am J Neuroradiol 2002;23:1580–88 [PMC free article] [PubMed] [Google Scholar]
- 8. Cloft HJ, Kallmes DF. Aneurysm packing with HydroCoil Embolic System versus platinum coils: initial clinical experience. AJNR Am J Neuroradiol 2004;25:60–62 [PMC free article] [PubMed] [Google Scholar]
- 9. Cloft H, for the HEAL Investigators . HydroCoil for Endovascular Aneurysm Occlusion (HEAL) study: 3–6 month angiographic follow up results. AJNR Am J Neuroradiol 2007;28:152–54 [PMC free article] [PubMed] [Google Scholar]
- 10. Fanning NF, Berentei Z, Brennan PR, et al. HydroCoil as an adjuvant to bare platinum treatment in 100 aneurysms. Neuroradiology 2007;49:139–48 [DOI] [PubMed] [Google Scholar]
- 11. Geyik S, Yauuz K, Cekirge S, et al. Endovascular treatment of basilar and ICA termination aneurysms: effects of use of HydroCoils on treatment stability in a subgroup of patients prone to a higher recurrence rate. Neuroradiology 2007;49:1015–21 [DOI] [PubMed] [Google Scholar]
- 12. Gaba RC, Ansari SA, Roy SS, et al. Embolization of intracranial aneurysms with hydrogel-coated coils versus inert platinum coils: effects on packing density, coil length and quantity, procedural performance, cost, length of hospital stay and durability of therapy. Stroke 2006;37:1443–50 [DOI] [PubMed] [Google Scholar]
- 13. Deshaies EM, Adamo MA, Boulos AS. A prospective single-center analysis of the safety and efficacy of the HydroCoil embolic system for the treatment of intracranial aneurysms. J Neurosurg 2007;106:226–33 [DOI] [PubMed] [Google Scholar]
- 14. Arthur AS, Wilson SA, Dixit S, et al. Hydrogel-coated coils for the treatment of cerebral aneurysms: preliminary results. Neurosurg Focus 2005;18:1–9 [DOI] [PubMed] [Google Scholar]
- 15. Berenstein A, Song JK, Niimi Y, et al. Treatment of cerebral aneurysms with hydrogel-coated platinum coils (HydroCoil): early single-center experience. AJNR Am J Neuroradiol 2006;27:1834–40 [PMC free article] [PubMed] [Google Scholar]
- 16. Gunnarsson T, Lurfan P, ter Brugg KG, et al. Treatment of intracranial aneurysms with hydrogel-coated expandable coils. Can J Neurol Sci 2007;34:38–46 [DOI] [PubMed] [Google Scholar]
- 17. Ya P, Jing GX, Y Y, et al. Acute ruptured intracranial aneurysm packing with HydroCoil embolic system: initial clinical experience. The Neuroradiology Journal 2007;20:61–64 [DOI] [PubMed] [Google Scholar]
- 18. Kang HS, Han MH, Lee TH, et al. Embolization of intracranial aneurysms with hydrogel-coated coils: result of a Korean multicenter trial. Neurosurgery 2007;61:51–59 [DOI] [PubMed] [Google Scholar]
- 19. Gunnarsson T, Tong FC, Klurfan P, et al. Angiographic and clinical outcomes in 200 consecutive patients with cerebral aneurysm treated with hydrogel-coated coils. AJNR Am J Neuroradiol 2009;30:1657–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. White PM, Raymond J. Endovascular coiling of cerebral aneurysms using “bioactive” or coated-coil technologies: a systematic review of the literature. AJNR Am J Neuroradiol 2009;30:219–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. White PM, Lewis SC, Nasher H, et al. HydroCoil Endovascular Aneurysm Occlusion and Packing Study (HELPS Trial): procedural safety and operator-assessed efficacy results. AJNR Am J Neuroradiol 2008;29:217–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Reul J, Weis J, Spetzger U, et al. Long-term angiographic and histopathologic findings in experimental aneurysms of the carotid bifurcation embolized with platinum and tungsten coils. AJNR Am J Neuroradiol 1997;18:35–42 [PMC free article] [PubMed] [Google Scholar]
- 23. Sluzewski M, van Rooij WJ, Slob MJ, et al. Relation between aneurysm volume, packing, and compaction in 145 cerebral aneurysms treated with coils. Radiology 2004;231:653–58 [DOI] [PubMed] [Google Scholar]
- 24. van Rooij WJ, Sluzewski M. Durability of treatment of intracranial aneurysms is not different from standard platinum coils. Stroke 2006;37:2874. [DOI] [PubMed] [Google Scholar]
- 25. Sluzewski M, van Rooij WJ, Rinkel GJ, et al. Endovascular treatment of ruptured intracranial aneurysms with detachable coils: long-term clinical and serial angiographic results. Radiology 2003;227:720–24 [DOI] [PubMed] [Google Scholar]
- 26. Schaafsma JD, Sprengers ME, van Rooij WJ, et al. Long term recurrent subarachnoid hemorrhage after adequate coiling versus clipping of ruptured intracranial aneurysms. Stroke 2009;40:1758–63. Epub 2009 Mar 12 [DOI] [PubMed] [Google Scholar]
- 27. Johnston SC, Dowd CF, Higashida RT, et al. Predictors of rehemorrhage after treatment of ruptured intracranial aneurysms: the Cerebral Aneurysm Rerupture After Treatment (CARAT) study. Stroke 2008;39:120–25 [DOI] [PubMed] [Google Scholar]
- 28. Holmin S, Krings T, Ozanne A, et al. Intradural saccular aneurysms treated by Guglielmi detachable coils at a single institution between 1993 and 2005. Stroke 2008;39:2288–97 [DOI] [PubMed] [Google Scholar]
- 29. Molyneux AJ, Kerr R, Birks J, et al. Risk of recurrent subarachnoid haemorrhage, death, or dependence and standardised mortality ratios after clipping or coiling of an intracranial aneurysm in the International Subarachnoid Aneurysm Trial (ISAT): long-term follow-up. Lancet Neurol 2009;8:427–33. Epub 2009 Mar 12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cloft H. What are we talking about? Definitions, mechanisms and risk factors. In: Proceedings of the 10th Congress of the World Federation of Interventional and Therapeutic Neuroradiology, Montreal, Quebec, Canada. June 22–July 3, 2009 [Google Scholar]