Abstract
BACKGROUND AND PURPOSE:
There is no prospective study related to the sonographic differentiation of malignant PCTN from benign PCTN. This prospective study was designed to evaluate differentiation of benign from malignant PCTNs with thyroid sonography.
MATERIALS AND METHODS:
Two hundred thirteen PCTNs in 196 patients who had consecutively undergone prospective sonographic diagnosis and US-FNAB were included. The PCTNs were evaluated according to their configuration and the presence of calcification, a free margin, vascularity, spongiform appearance or daughter cysts, colloid crystal, nodule shape, and echogenicity. Each PCTN was prospectively classified into 1 of 4 diagnostic categories: benign features, probably benign, suspicious for malignancy, and malignant features. We calculated the diagnostic efficacy of a prospective sonographic diagnosis for PCTNs by comparing it with cytopathologic results.
RESULTS:
Among the 213 PCTNs, 53 underwent thyroid surgery. The sonographic classifications for 213 PCTNs included benign features (n = 182), probably benign (n = 19), suspicious for malignancy (n = 7), and malignant features (n = 5). When nonsurgical PCTNs (n = 160) with benign sonographic findings and benign cytology were considered negative, the sensitivity, specificity, PPV, NPV, and accuracy of the prospective diagnosis of PCTNs were 72.7%, 98.0%, 66.7%, 98.5%, and 96.7%, respectively. On the basis of individual analysis, eccentric configuration with an acute angle and microcalcifications were significantly associated with malignancy, but a concentric configuration, a smooth free margin, peripheral vascularity, spongiform appearance or daughter cysts, and intranodular colloid crystals showed a statistically significant association with benignity.
CONCLUSIONS:
Our prospective sonographic diagnoses of PCTNs, especially those >2 cm, were highly reliable.
Cystic thyroid nodules as detected by thyroid sonography and thyroid surgery are common.1–7 Most cystic thyroid nodules showing a mixed echogenicity develop as a result of cystic degeneration of neoplastic or non-neoplastic nodules; however, true thyroid cysts that have an epithelial lining are rare.4 Some investigators have suggested that thyroid cysts can be considered benign lesions and managed conservatively.5,6 However, more recent studies have reported that the frequency of malignancy in cystic thyroid nodules is similar to that of solid nodules.1–4
Thyroid sonography has been used as the major diagnostic technique for the evaluation of thyroid nodules. Several sonographic features such as marked hypoechogenicity, an irregular margin, microcalcifications, and a taller than wide shape have been introduced as potential predictors for the presence of a thyroid malignancy in solid thyroid nodules; however, to our knowledge, there are few studies on sonographic features as predictors of a diagnosis of cystic thyroid nodules.4,7 Recently, Lee et al7 reported that a predominantly solid component, an eccentrically placed solid component, and the presence of microcalcifications are associated with malignancy of PCTNs. However, to our knowledge, there has been no prospective study on the diagnostic efficacy of thyroid sonography for PCTN. A prospective study for sonographic diagnoses of PCTNs might be more accurate compared with a retrospective study that includes limited sonograms. Furthermore, the results of such a study could be helpful for patient care in the clinical setting by decreasing the use of US-FNAB for PCTNs on the basis of the high diagnostic efficacy of thyroid sonography for PCTN.
The aim of this prospective study was to assess the diagnostic efficacy of thyroid sonography and the sonographic classification of PCTNs for differentiating benign and malignant lesions compared with the results of US-FNAB or surgery.
Materials and Methods
Patients
Our institutional review board approved this study. From May 2008 to April 2009, 1 radiologist (D.W.K.) who had 7 years of experience in thyroid sonography (>2500 cases/year) and US-FNAB for thyroid nodules (>1000 nodules/year), sequentially performed thyroid sonography and US-FNAB of the thyroid nodules in 453 patients (378 women, 75 men; age range, 15–81 years; mean age, 48.4 years). Among them, 196 patients with 213 PCTNs (155 women, 41 men; age range, 20–75 years; mean age, 48.1 years) who had undergone ≥1 US-FNAB were enrolled in this study. The 196 patients with nodules (n = 213; size range, 0.5–7.0 cm; mean size, 2.23 ± 1.17 cm) underwent US-FNAB because of a positive prospective sonographic diagnosis (n = 12), screening (n = 150), insufficient cytology after a palpation-guided FNAB (n = 15), a positive risk factor for thyroid malignancy (n = 5), and a patient's request (n = 31).
Sonographic Examination
Thyroid sonography was performed by using a high-resolution sonographic instrument (iU22; Philips Healthcare, Bothell, Washington) equipped with a 12- to 15-MHz linear probe. During color Doppler examination, a low value of pulse repetition frequency (700 Hz) was used to evaluate the vascularity of PCTNs according to the following features: 1) configuration, 2) calcification, 3) a free margin, 4) vascularity, 5) spongiform appearance or daughter cysts, 6) the presence of intranodular colloid crystals, 7) nodule shape, and 8) echogenicity.
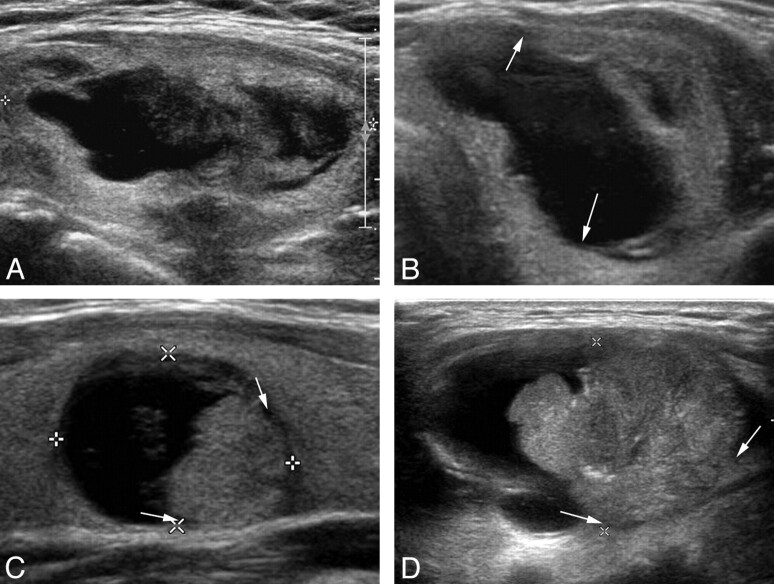
PCTNs were classified as concentric, eccentric, or multiseptate in their configuration depending on the position or composition of the main solid and cystic component, regardless of the presence of debris. A “concentric” PCTN was defined as one with a central location of the main cystic component on thyroid sonography (Fig 1 A). On the other hand, an “eccentric” PCTN was defined as one with a peripheral location of the main cystic or solid component (Figs 1 B–D and 2). The eccentric configuration was subdivided into either an acute angle or a blunt angle, depending on the angle degree between the solid component and the adjacent cyst wall on real-time sonography. “Microcalcifications” and “macrocalcifications” were defined as tiny punctuated hyperechoic foci (<1 mm) without posterior shadows or comet-tail artifacts and intensely hyperechoic abnormalities (=1 mm) with posterior shadows, respectively. The “free margin” of a PCTN was defined as the interface between the cystic component and the solid component, and it was divided into 4 categories: a smooth free margin, microlobulation, macrolobulation, and an irregular free margin. The “perinodular infiltration” of a PCTN was defined as a focal extension of the solid component beyond the outer margin of the PCTN. The “vascularity” of the PCTN was divided into 5 categories by color Doppler sonography: no vascularity, peripheral vascularity, centripetal vascularity in the pedicle, mildly increased vascularity in the entire solid component, and moderately increased vascularity in the entire solid component. A “spongiform appearance” was defined as an aggregation of multiple microcystic components in the solid components. “Daughter cysts” were defined as numerable microcystic components in the solid components. “Colloid crystal” was defined as a small hyperechoic focus with ring-down artifacts in the cystic component. The shape of the PCTN was simply classified as ovoid or flat and round.
Fig 1.
The 4 categories of thyroid sonography for the classification of PCTNs. A, Benign features in a 60-year-old woman. A longitudinal sonogram of nodular hyperplasia in the left lobe shows a concentric configuration with a centrally located cystic component, a smooth free margin, an ovoid shape, and isoechogenicity. B, Probably benign in a 50-year-old woman. A transverse sonogram of nodular hyperplasia in the left lobe shows an eccentric configuration with a blunt angle between the solid component and the wall (arrows), a smooth free margin, and isoechogenicity. C, Suspicious for malignancy in a 28-year-old woman. A longitudinal sonogram of a papillary thyroid carcinoma in the left lobe shows an eccentric configuration with an acute angle between the solid component and the wall (arrows), a microlobulation, and isoechogenicity. D, Malignant features in a 45-year-old woman. A longitudinal sonogram of a papillary thyroid carcinoma in the left lobe shows an eccentric configuration with an acute angle (arrows), macrolobulation, microcalcifications, and hypoechogenicity.
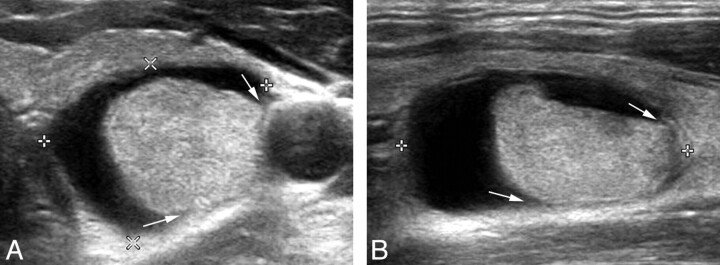
Fig 2.
A PCTN assigned to the suspicious for malignancy category on thyroid sonography in a 29-year-old man (a false-positive). A and B, Transverse and longitudinal sonograms of a PCTN in the left midlobe show an eccentric configuration with an acute angle (arrows), a smooth free margin, an ovoid shape, and isoechogenicity. The lesion was surgically confirmed as nodular hyperplasia at the patient's request despite benign cytology on the US-FNAB (1.2 × 1.6 × 1.9 cm).
The echogenicity of the solid component was classified as isoechogenicity, hypoechogenicity, marked hypoechogenicity, and hyperechogenicity by comparison of the echogenicity of the solid component with the thyroid parenchyma or strap muscles. When the echogenicity of the solid component was similar to that of the thyroid parenchyma, the echogenicity of the PCTN was classified as “isoechogenicity.” Marked “hypoechogenicity” was defined as decreased echogenicity compared with the strap muscles, and the “hypoechogenicity” was intermediate echogenicity compared with the thyroid parenchyma and the strap muscles.
According to the composition of the nodule, the PCTNs were divided into 2 groups: group 1 with a cystic component <50% and group 2 with a cystic component ≥50% (not a pure cyst). In addition, diagnostic efficacy of thyroid sonography for the PCTNs was evaluated depending on the largest diameter: ≥2 cm and <2 cm. The volume of the PCTN was calculated by the formula for a rotational ellipsoid by using 3 diameters of the nodule measured on transverse and longitudinal images.8 Therefore, thyroid nodules with a purely cystic or purely solid composition were not included in this study.
Prospective Sonographic Diagnoses for PCTNs
The sonographic features of a benign PCTN used as inclusion criteria were the following: a concentric configuration or an eccentric configuration with a blunt angle, a smooth free margin, peripheral or no vascularity, a spongiform appearance or daughter cysts in the solid component, intranodular comet-tail artifacts due to a colloid crystal, and isoechogenicity. The sonographic characteristics of a malignant PCTN included an eccentric configuration with an acute angle, microcalcifications, macrolobulation or an irregular free margin, perinodular infiltration, a centripetal vascularity in the pedicle, and hypoechogenicity.
After we performed thyroid sonography, the PCTNs were immediately classified as being in 1 of 4 categories on the basis of their sonographic features, including “benign features,” “probably benign,” “suspicious for malignancy,” and “malignant features.” The criteria for the prospective sonographic diagnosis of a PCTN included the following: If it demonstrated ≥3 sonographic characteristics of a benign nodule without sonographic features of a malignancy, it was considered benign. If a PCTN demonstrated 1 or 2 sonographic characteristics that suggested a benign lesion without sonographic features of a malignancy, it was considered probably benign. If a PCTN demonstrated 1 sonographic characteristic of a malignancy on thyroid sonography regardless of the existence of benign sonographic features, it was considered suspicious for malignancy. If a PCTN demonstrated ≥2 sonographic characteristics that suggested a malignancy on thyroid sonography regardless of the existence of benign sonographic features, it was considered malignant (Fig 1).
When a PCTN was predominantly cystic, >50%, the operator performed US-FNAB of the solid component after aspiration of the fluid from the cystic component without exchanging the needle.
Data Analysis
We retrospectively compared the prospective sonographic diagnoses and cytopathologic results of the PCTNs. A PCTN classified as having benign features or being probably benign on prospective sonographic diagnosis was categorized as negative; a PCTN classified as suspicious for malignancy and having malignant features was categorized as positive. Sensitivity, specificity, PPV, NPV, and accuracy of the prospective sonographic diagnosis for a PCTN were calculated.
The agreement between sonographic diagnosis and cytopathologic results was evaluated by means of the κ statistics as follows: The κ-values can range from 0 (no agreement) to 1.00 (perfect agreement) and can be interpreted as poor (0), slight (0.01–0.20), fair (0.21–0.40), moderate (0.41–0.60), substantial (0.61–0.80), and almost perfect (0.81–1.00). All statistical evaluations used the Statistical Package for the Social Sciences software package (SPSS, Chicago, Illinois). Individual analysis was performed to determine independent sonographic criteria for benign and malignant PCTNs, and a 2-tailed P value < 1% was statistically significant.
Results
After thyroid sonographic examination in 196 patients, 1 radiologist classified each PCTN as the following: benign features (n = 182), probably benign (n = 19), suspicious for malignancy (n = 7), and malignant features (n = 5). The frequency of the sonographic features in 213 thyroid nodules is summarized in On-line Table 1. There were solitary nodules in 32 patients and multiple nodules in 164 patients.
Thyroid surgery was performed for 53 PCTNs in 51 patients (44 women, 7 men; mean age, 45.2 ± 10.7 years) because of malignant cytology (n = 11), a positive sonographic diagnosis despite benign cytology (n = 4), indeterminate for malignancy cytology (n = 1) on consecutive US-FNAB, the presence of a large palpable mass with a benign cytology (n = 13), and patient's request (n = 24). Repeat US-FNAB on the PCTN was performed when the cytologic results in the first US-FNAB were indeterminate for malignancy (n = 3) or inadequate (n = 25). Among 28 PCTNs with indeterminate for malignancy or inadequate cytology classification on the first US-FNAB, there was no case with malignant cytology on the repeat US-FNAB. One PCTN that had a suspicious for malignancy sonographic diagnosis and indeterminate for malignancy cytology was confirmed as nodular hyperplasia after thyroid surgery. Among 201 PCTNs with benign sonographic categories, 160 PCTNs showed a benign cytology on the US-FNAB and were followed up with only thyroid sonography after at least 6 months. On thyroid sonography, 28 patients had a solitary thyroid nodule and 168 patients had ≥2 thyroid nodules. The correlation of the prospective sonographic diagnosis with cytopathologic results for PCTNs is shown in On-line Table 2.
When nonsurgical PCTNs (n = 160) with benign sonographic findings and benign cytology were considered as negative, the numbers of true-negative, true-positive, false-negative, and false-positive results for the prospective sonographic diagnosis of a PCTN were 198, 8, 3, and 4, respectively. Therefore, the sensitivity, specificity, PPV, NPV, and accuracy for a prospective sonographic diagnosis of a PCTN were 72.7% (8/11), 98.0% (198/202), 66.7% (8/12), 98.5% (198/201), and 96.7% (206/213), respectively. Statistically, there was substantial correlation between sonographic diagnosis and cytopathologic results in this study (κ= .678; 95% confidence interval, 0.564 ∼ 0.792). In addition, the correlation was substantial in group 1 (κ = 0.715; 95% confidence interval, 0.559 ∼ 0.817) and in group 2 (κ = 0.644; 95% confidence interval, 0.480 ∼ 0.808).
For 182 PCTNs assigned to the benign features category on thyroid sonography, 37 nodular hyperplasias and 1 follicular adenoma were confirmed after thyroid surgery. Among 19 PCTNs assigned to the probably benign category on thyroid sonography, 3 PTCs were surgically confirmed because of malignant cytology findings on the US-FNAB. All of the PCTNs (n = 5) assigned to the malignant features group on the thyroid sonography were confirmed as PTCs. However, 7 PCTNs assigned to the suspicious for malignancy group on thyroid sonography showed malignant cytology findings (n = 3), indeterminate for malignancy cytology findings (n = 1), and benign cytology findings (n = 3) after the US-FNAB; these were surgically removed. On the pathology result for these nodules, there were 3 PTCs and 4 cases of nodule hyperplasia (Fig 2).
Individual analysis was performed to determine independent sonographic features associated with a benign or malignant PCTN (On-line Table 3). An eccentric solid component with an acute angle, microcalcifications, macrolobulation or an irregular free margin, perinodular infiltration, centripetal vascularity in the pedicle, and hypoechogenicity of the solid component showed a statistically significant association with a malignant PCTN. However, a concentric configuration, a smooth free margin, peripheral vascularity, spongiform appearance or daughter cysts, and a colloid crystal showed a statistically significant association with a benign PCTN (P < .01).
When 4 sonographic features (eccentric configuration with an acute angle, microcalcifications, macrolobulation or irregular free margin, and centripetal vascularity in the pedicle) were combined, all combinations showed high specificity, NPVs, and accuracy (>90%). Especially, the combinations including eccentric configuration with an acute angle and microcalcifications had a high sensitivity, >90%. However, all combinations showed a low PPV (On-line Table 4).
In group 1 (a cystic component <50%), the sensitivity, specificity, PPV, NPV, and accuracy for the prospective sonographic diagnosis of a PCTN were 100% (4/4), 97.4% (113/116), 57.1% (4/7), 100% (113/113), and 97.5% (117/120), respectively. In group 2 (a cystic component ≥50%), the sensitivity, specificity, PPV, NPV, and accuracy for the prospective sonographic diagnosis of a PCTN were 57.1% (4/7), 98.8% (85/86), 80% (4/5), 96.6% (85/88), and 95.7% (89/93), respectively. There was no statistically significant difference in the diagnostic efficacy of thyroid sonography between groups 1 and 2 (κ-value in group 1, 0.715; κ-value in group 2, 0.678). However, there were 11 malignant PCTNs in group 2, and no malignancy in group 1.
When 213 PCTNs were divided into 2 groups depending on the largest diameter of the nodule being ≥2 cm (n = 112) and <2 cm (n = 101), the sensitivity, specificity, PPV, NPV, and accuracy for the prospective sonographic diagnosis of PCTNs of ≥2 cm and <2 cm were 100% and 50%, 100% and 95.8%, 100% and 42.9%, 100% and 96.8%, and 100% and 94.1%, respectively. There was a statistically significant difference in the diagnostic efficacy of thyroid sonography between the 2 groups (κ-value in ≥2 cm, 1; and κ-value in <2 cm, 0.425). Especially, the prospective sonographic diagnoses of PCTNs ≥2 cm were entirely correct.
Discussion
Most PCTNs are thought to be the result of a degenerative process; some PCTNs have true epithelium.4 In the past, thyroid cysts were considered benign lesions; however, more recently, the management of PCTNs has been debated. To date, clinical findings such as sex, nodule size, previous neck irradiation, or recurrence after repeated aspirations have not been useful to distinguish benign from malignant PCTNs.2,4,9 Recently, Lee et al7 suggested that an eccentrically placed solid component and microcalcifications were associated with malignancy in PCTNs. The results of this study showed that the sonographic characteristics of PCTNs were different from the features of purely or predominantly solid nodules showing well-known malignant features; these characteristics included marked hypoechogenicity, microcalcifications, irregular free margin, and a taller than wide shape.
The risk of malignancy in PCTNs has variably been reported from approximately 2% to 18%.1–4,10,11 In the present study, the rate of malignancy for the PCTNs was 5.2% (11/213). However, this rate of malignancy for the PCTNs was significantly lower than the frequency of malignancy for thyroid nodules (25.6%, 112/438) on the basis of thyroid sonography and consecutive US-FNAB in our hospital.12 Therefore, the findings showed that the frequency of malignant PCTNs is relatively low compared with the frequency of malignancy in solid thyroid nodules.
We classified the sonographic diagnoses of the PCTNs into 4 categories, including benign features, probably benign, suspicious for malignancy, and malignant features. Although all PCTNs assigned to the malignant features category on thyroid sonography were confirmed as papillary thyroid carcinomas and all PCTNs assigned to benign features category on thyroid sonography showed no malignancy on cytopathologic results, 4 PCTNs assigned to the suspicious for malignancy group and 3 PCTNs assigned to the probably benign group on thyroid sonography were false-positives and false-negatives, respectively. The prospective sonographic diagnosis for PCTNs showed a high specificity (98.0%, 198/202), NPV (98.5%, 198/201), and accuracy (96.7%, 206/213), while there was a relatively low sensitivity (72.7%, 8/11) and PPV (66.7%, 8/12). Therefore, the results showed that it is possible for experienced radiologists to obtain a high diagnostic accuracy on thyroid sonography for PCTNs. The sonographic classification of a PCTN described in this study can be helpful in selecting the methods for determining which patients undergo US-FNAB and have more conservative care. This approach is predicted to reduce the frequency of the unnecessary US-FNABs for benign PCTN.
The results of this study showed that the eccentric configuration with an acute angle, microcalcifications, and macrolobulation or irregular free margin significantly increased the risk of malignancy for the PCTN. Unlike in the retrospective study reported by Lee et al,7 the eccentric configuration was subdivided according to the angle between the solid component and the cyst wall (ie, the eccentric configuration with an acute angle and the eccentric configuration with a blunt angle). The eccentric configuration with a blunt angle was not significantly associated with an increase in the risk for a malignancy, while the eccentric configuration with an acute angle was significantly associated with a malignant PCTN. This result may be explained by the theory that a malignant PCTN originates from the wall of a thyroid cyst, and the real tumor tissue is frequently localized to the base of the papillomatous lesions as shown in a previous study.13 Moreover, known malignant sonographic features including marked hypoechogenicity and a taller than wide shape were not associated with an increased risk of a malignant PCTN. Most interesting, hypoechogenicity of the solid component of a PCTN was relatively correlated with a malignancy, while marked hypoechogenicity showed no increased risk for a malignancy in a PCTN. The reason for this result is unclear; however, it may be related to the easy sonic transmission through the cystic component of a PCTN compared with a solid nodule. In addition, when the solid component of a PCTN simultaneously showed marked hypoechogenicity and no vascularity, it was less likely to be malignant. We considered the pathogenesis of the marked hypoechogenicity as fibrotic regression after spontaneous collapse of the hemorrhagic component.
On the basis of the results of the present study, the PCTN showed several differences from the known malignant sonographic features of solid thyroid nodules. First, the findings of this study showed that marked hypoechogenicity was observed in 9 benign PCTNs but not in malignant PCTNs. Unlike a solid thyroid nodule, marked hypoechogenicity was highly specific for a benign PCTN despite its low frequency. Second, microlobulation was not included in the malignant criteria. A smooth free margin was used as a sonographic feature of a benign PCTN, but microlobulation was not used for the sonographic criteria. Unlike the outer margin of a benign PCTN, a free margin of a benign PCTN commonly appears to be a microlobulation on thyroid sonography; therefore, microlobulation was considered as unhelpful in the differentiation of a benign PCTN from a malignant PCTN. Third, the shape of a PCTN was not helpful in the diagnosis of malignancy. There was no malignant PCTN showing a taller than wide shape, while a taller than wide shape is well known to be a malignant sonographic feature for solid nodules.
A spongiform appearance and a colloid crystal showing comet-tail artifacts are known to be highly specific sonographic features of benign thyroid nodules.14,15 In the present study, the concentric configuration, a smooth free margin or microlobulation, peripheral or no vascularity, spongiform appearance or daughter cysts, and colloid crystals showed a significant association with the benign PCTN. In addition, an eccentric configuration with a blunt angle between the solid component and the wall, an ovoid or flat shape, or isoechogenicity of the solid component was relatively associated with benign rather than malignant PCTNs. Recently, any calcification within the thyroid nodule has been considered a feature that raises the likelihood of a malignancy.14,16 However, only 2 benign PCTNs showed macrocalcification on thyroid sonography, and there were no macrocalcifications in the malignant PCTNs.
Lee et al7 suggested that the sonographic diagnosis of PCTNs is important not only to determine the sonographic features predictive of malignancy but also to determine whether 1 of the 2 combinations just noted is present; they reported that when the combination of sonographic features, including an eccentric solid position and microcalcifications, was considered, sensitivity, specificity, PPV, NPV, and accuracy were 66.7%, 82.3%, 17.6%, 97.8%, and 81.5%, respectively. In our study, when all combinations of 4 malignant sonographic features, including eccentric configuration with an acute angle, microcalcifications, macrolobulation or irregular free margin, and centripetal vascularity in the pedicle, were considered, sensitivity, specificity, PPV, NPV, and accuracy were 90.9%, 90.1%, 33.3%, 99.5%, and 90.1%, respectively.
Unlike the retrospective study by Lee et al,7 higher values of all diagnostic indices were obtained in this study. In particular, all combinations including eccentric configuration with acute angle and microcalcifications showed a high sensitivity, specificity, NPV, and accuracy for the diagnosis of a PCTN. The low PPV was similar to the results reported by Lee et al. However, unlike the study by Lee et al, there was no malignant PCTN in group 1 (a cystic component of <50%). However, we cannot explain why the malignant PCTN had a greater incidence in predominantly cystic PCTNs (group 2) than in the predominantly solid PCTNs (group 1). Nevertheless, there was no significant difference in the diagnostic efficacy of the thyroid sonography for PCTNs between groups 1 and 2. On the other hand, when we compared the diagnostic efficacy of thyroid sonography depending on the largest diameter of the nodule, the PCTN group >2 cm showed significantly higher values than the PCTN group <2 cm. These data support the finding that a sonographic diagnosis of a PCTN of >2 cm is more reliable compared with a PCTN of <2 cm.
The limitations of this study include the following: First, not all PCTNs had thyroid surgery; they all had US-FNAB. One or more repeat US-FNABs were performed when the PCTNs had an inadequate or indeterminate cytology or an indeterminate or suspicious sonographic diagnosis. When the PCTNs that did not have thyroid surgery were excluded from the determination of the diagnostic index, the sensitivity, specificity, PPV, NPV, and accuracy for a prospective sonographic diagnosis of a PCTN were 72.7% (8/11), 91.3% (42/46), 66.7% (8/12), 93.3% (42/45), and 87.7% (50/57), respectively. Second, there were a small number of malignant PCTNs (5.2%, 11/213). Third, this study was performed by a radiologist who had experience with thyroid sonography; therefore, it does not represent general operators with less experience in thyroid sonography or trainees. Finally, only color Doppler sonography was used to evaluate the vascularity of a PCTN.
Conclusions
In summary, our prospective sonographic diagnoses of PCTNs, especially >2 cm, were highly reliable and, thus, may be used as a guide for management of PCTNs. On the basis of the present study of PCTNs, eccentric configuration with an acute angle and microcalcifications was significantly associated with the increased risk of malignancy, but a concentric configuration, a smooth free margin, peripheral vascularity, spongiform appearance or daughter cysts, and an intranodular colloid crystal showed a statistically significant association with the likelihood of benignity.
Supplementary Material
Abbreviations
- A
eccentric configuration with acute angle
- B
microcalcifications
- C
macrolobulation
- D
centripetal vascularity in pedicle
- FA
follicular adenoma
- NH
nodular hyperplasia
- NPV
negative predictive value
- PCTN
partially cystic thyroid nodule
- PPV
positive predictive value
- PTC
papillary thyroid carcinoma
- UA
unavailable
- US-FNAB
sonographically guided fine-needle aspiration biopsy
Footnotes
Indicates article with supplemental on-line tables.
This work was supported by the Busan Paik Hospital Imaging Research Institute.
References
- 1. McHenry CR, Slusarczyk SJ, Khiyami A. Recommendations for management of cystic thyroid nodule. Surgery 1999;126:1167–72 [DOI] [PubMed] [Google Scholar]
- 2. De Loss Santos ET, Keyhani-Rofagha S, Cunningham JJ, et al. Cystic thyroid nodules: the dilemma of malignant lesions. Arch Intern Med 1990;150:1422–27 [DOI] [PubMed] [Google Scholar]
- 3. Rosen IB, Provias JB, Walfish PG. Pathologic nature of cystic thyroid nodules selected for surgery by needle aspiration biopsy. Surgery 1986;100:606–12 [PubMed] [Google Scholar]
- 4. Bellantone R, Lombardi CP, Raffaelli M, et al. Management of cystic or predominantly cystic thyroid nodules: the role of ultrasound-guided fine-needle aspiration biopsy. Thyroid 2004;14:43–47 [DOI] [PubMed] [Google Scholar]
- 5. Crile G. Treatment of thyroid cysts by aspiration. Surgery 1966;59:210–12 [PubMed] [Google Scholar]
- 6. Sarda AK, Bal S, Dutta Gupta S, et al. Diagnosis and treatment of cystic disease of the thyroid by aspiration. Surgery 1988;103:593–96 [PubMed] [Google Scholar]
- 7. Lee MJ, Kim EK, Kwak JY, et al. Partially cystic thyroid nodules on ultrasound: probability of malignancy and sonographic differentiation. Thyroid 2009;19:341–46 [DOI] [PubMed] [Google Scholar]
- 8. Nygaard B, Nygaard T, Court-Payen M, et al. Thyroid volume measured by ultrasonography and CT. Acta Radiol 2002;43:269–74 [DOI] [PubMed] [Google Scholar]
- 9. Alexander EK, Hurwitz S, Heering JP, et al. Natural history of benign solid and cystic thyroid nodules. Ann Intern Med 2003;138:315–18 [DOI] [PubMed] [Google Scholar]
- 10. Nam-Goong IS, Kim HY, Gong G, et al. Ultrasonography-guided fine-needle aspiration of thyroid incidentaloma: correlation with pathological findings. Clin Endorinol (Oxf) 2004;60:21–28 [DOI] [PubMed] [Google Scholar]
- 11. Choi KU, Kim JY, Park DY, et al. Recommendations for the management of cystic thyroid nodules. ANZ J Surg 2005;75:537–41 [DOI] [PubMed] [Google Scholar]
- 12. Kim DW, Lee EJ, Kim SH, et al. Ultrasound-guided fine-needle aspiration biopsy of thyroid nodules: comparison in efficacy according to nodule size. Thyroid 2009;19:27–31 [DOI] [PubMed] [Google Scholar]
- 13. Yokozawa T, Miyauchi A, Kuma K, et al. Accurate and simple method of diagnosing thyroid nodules by the modified technique of ultrasound-guided fine-needle aspiration biopsy. Thyroid 1995;5:141–45 [DOI] [PubMed] [Google Scholar]
- 14. Moon WJ, Jung SL, Lee JH, et al. Benign and malignant thyroid nodules: US differentiation—multicenter retrospective study. Radiology 2008;247:762–70. Epub 2008 Apr 10 [DOI] [PubMed] [Google Scholar]
- 15. Ahuja A, Chick W, King W, et al. Clinical significance of the comet-tail artifact in thyroid ultrasound. J Clin Ultrasound 1996;24:129–33 [DOI] [PubMed] [Google Scholar]
- 16. Frates MC, Benson CB, Charboneau JW, et al. Management of thyroid nodules detected at US: Society of Radiologists in Ultrasound consensus conference statement. Radiology 2005;237:794–800 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.