Abstract
BACKGROUND AND PURPOSE:
The goal of this article is to provide consensus recommendations for reporting standards, terminology, and written definitions when reporting on the radiological evaluation and endovascular treatment of intracranial, cerebral aneurysms. These criteria can be used to design clinical trials, to provide uniformity of definitions for appropriate selection and stratification of patients, and to allow analysis and meta-analysis of reported data.
METHODS:
This article was written under the auspices of the Joint Writing Group of the Technology Assessment Committee, Society of NeuroInterventional Surgery, Society of Interventional Radiology; Joint Section on Cerebrovascular Neurosurgery of the American Association of Neurological Surgeons and Congress of Neurological Surgeons; and Section of Stroke and Interventional Neurology of the American Academy of Neurology. A computerized search of the National Library of Medicine database of literature (PubMed) from January 1991 to December 2007 was conducted with the goal to identify published endovascular cerebrovascular interventional data about the assessment and endovascular treatment of cerebral aneurysms useful as benchmarks for quality assessment. We sought to identify those risk adjustment variables that affect the likelihood of success and complications. This article offers the rationale for different clinical and technical considerations that may be important during the design of clinical trials for endovascular treatment of cerebral aneurysms. Included in this guidance article are suggestions for uniform reporting standards for such trials. These definitions and standards are primarily intended for research purposes; however, they should also be helpful in clinical practice and applicable to all publications.
CONCLUSIONS:
The evaluation and treatment of brain aneurysms often involve multiple medical specialties. Recent reviews by the American Heart Association have surveyed the medical literature to develop guidelines for the clinical management of ruptured and unruptured cerebral aneurysms. Despite efforts to synthesize existing knowledge on cerebral aneurysm evaluation and treatment, significant inconsistencies remain in nomenclature and definition for research and reporting purposes. These operational definitions were selected by consensus of a multidisciplinary writing group to provide consistency for reporting on imaging in clinical trials and observational studies involving cerebral aneurysms. These definitions should help different groups to publish results that are directly comparable.
The goal of this article is to provide consensus recommendations for reporting standards, terminology, and written definitions when reporting on the radiological evaluation and endovascular treatment of intracranial cerebral aneurysms. These criteria can be used to design clinical trials, to provide uniformity of definitions for appropriate selection and stratification of patients, and to allow analysis and meta-analysis of reported data. This article must not be construed as defining the standard-of-care. These reporting standards represent an ideal and are intended primarily for use in research protocols and possibly for quality assessment in individual practice, although this is not their main intention. These definitions represent recommendations for constructing useful research data sets. These definitions do not represent the only data that are important or useful in the design of clinical trials or reporting individual case series and are not intended to represent minimally acceptable data. Much of this information may be included in operative reports but is primarily intended for research.
The intent is to facilitate production of scientifically rigorous results capable of reliable comparisons between and among similar studies. In some cases, the definitions contained here are recommended by consensus of a panel of experts for consistency in reporting and publication.
Historical Context: Aneurysm Reporting
The evaluation and treatment of brain aneurysms often involve multiple medical specialties. Recent reviews by the American Heart Association have surveyed the medical literature to develop guidelines for the clinical management of ruptured1 and unruptured2 cerebral aneurysms. Despite efforts to synthesize existing knowledge on cerebral aneurysm evaluation and treatment, significant inconsistencies remain in nomenclature and definition for research and reporting purposes.
One of the major challenges in the basic evaluation and reporting of endovascular treatment results is the interpretation of fluoroscopic and arteriographic imaging. Careful arteriographic evaluation of 3-dimensional vascular structures requires a customized approach to each patient. Cerebral arteriography must be carefully performed to prevent procedural complications while achieving the necessary diagnostic information and minimizing ionizing radiation exposure to prescribe treatment. Noninvasive methods such as volumetric MRI/MR angiography and CT angiography often offer complementary information in the evaluation of cerebral aneurysms, but catheter cerebral arteriography provides the highest spatial resolution for evaluation of the dome-to-neck ratio, neck-to-artery ratio, and exact aneurysm dimensions for treatment planning for endovascular procedures. However, appropriate planar projections must be obtained to maximize the diagnostic yield of catheter arteriography.
Whenever possible, we recommend reporting continuous data as well as categorical data. For example, aneurysm size (X) should be reported in millimeters in 3 dimensions as well as categorical taxonomy including small aneurysms (X ≤5 mm), medium aneurysms (5< X <15 mm), large aneurysms (15 ≤ X <25 mm), and giant aneurysms (X ≥25 mm). The largest diameter is used to determine the appropriate category. Furthermore, dome-to-neck ratio should be mathematically calculated and grouped according to convention by small neck (X ≤4 mm) or wide neck (X >4 mm). Some aneurysms have no definable neck with separate inflow and outflow. Terms such as “fusiform” per se have little meaning. The International Study of Unruptured Intracranial Aneurysms (ISUIA) grouped patients according to the presence or absence of prior aneurysmal subarachnoid hemorrhage and the following size categories: <7 mm, 7 to 12 mm, 13 to 24 mm, and ≥24 mm based largely on differences in the clinical propensity to rupture according to categorical size and location.3,4 Table 1 shows an overview of definitions.
Table 1.
Summary of cerebral aneurysm attributes
| General definitions |
| Clinical presentation |
| Symptomatic: hemorrhage or mass |
| Hunt and Hess Grade or World Federation of Neurological Surgeons Grading Scale |
| Glasgow Coma Scale and NIHSS |
| Modified Rankin Scale score |
| Fisher CT score |
| Date of presentation |
| Time to diagnosis (hours to days) |
| Time to arteriography (hours to days) |
| Time to treatment (hours to days) |
| Imaging source and date |
| Aneurysm shape |
| Saccular |
| Other types excluded |
| Dissecting |
| Serpentine |
| Giant, partially thrombosed |
| Dolichoectatic |
| Size and location (see Table 5) |
| Planar dimensions |
| Neck width and area |
| Parent artery diameter |
| Dome-to-neck ratio |
| Neck-to-artery ratio |
| Aneurysm volume |
| Single or multiple |
| Arteriographic comorbidities (see Table 5) |
| Procedural technique |
| Catheter type |
| Guide wire type |
| Guiding catheter type |
| Adjunctive techniques |
| Coil types, diameters, lengths, and numbers of coils |
| Technical success |
| Recanalization and recanalization rate |
| Computational results |
| Arteriographic occlusion |
| Volumetric occlusion |
| Advanced computational features |
| Computational flow dynamics |
| Clinical success |
| 30-day morbidity and mortality (assessed by independent physician) |
| Modified Rankin Scale46 |
| Barthel Index47 |
| Glasgow Outcome Scale45 |
| NIHSS48 |
NIHSS indicates National Institutes of Health Stroke Scale.
General Definitions
The definition of cerebral aneurysm is an abnormal focal dilatation of a cerebral artery with attenuation of the vessel wall. There are several different pathophysiological types of aneurysms that involve the cerebral arteries. These include saccular, dolichoectatic, dissecting, serpentine, traumatic, mycotic, and giant aneurysms with or without thrombosis. Saccular aneurysms are the most common and the primary focus; other types are beyond the scope of this article.
Aneurysms may coexist with other vascular disorders such as fibromuscular dysplasia,5 polycystic hepatorenal disease,6 brain arteriovenous malformations,7 atherosclerosis,8 arterial fenestrations or duplications,9 and persistent primitive circulations,10 to name only some of the most common conditions. Medical comorbidities, including hypertension and tobacco use, appear to predispose to aneurysm formation and rupture.11,12 There are familial predispositions to cerebral aneurysms that remain under investigation.13,14 Women are more susceptible than men.15 It is important that these features are reported.
Clinical Presentation
Clinical presentation is a component of the medical and neurological history. It is a description of the clinical event(s) that directly brought the aneurysm to medical attention. Clinical presentation includes signs, symptoms, and temporally related imaging studies. Typical symptoms might include severe headache, nausea, vomiting, photophobia, and nuchal rigidity. Commonly identified signs sometimes include altered level of consciousness, focal weakness, and cranial nerve deficits. Imaging studies using CT or MRI techniques are used to confirm the presence of the aneurysm, hemorrhage, infarct, mass effect, or hydrocephalus. It should always be clear in reporting whether radiographic hemorrhage was part of the initial presentation and whether signs and symptoms were present. Clinical grading scales such as Hunt and Hess or World Federation of Neurological Surgeons should be referenced (See Tables 2 and 3 for definitions of these grading systems.) For this reason, each of the clinical features used to determine clinical grade by either method should be reported for retrospective classification into alternative grading scales.
Table 2.
Subarachnoid hemorrhage clinical grading scales
| Grade | Hunt and Hess | World Federation of Neurological Surgeons |
|---|---|---|
| 0 | Intact aneurysm | |
| 1 | Asymptomatic or mild headache | Glasgow Coma Scale (GCS) 15 |
| 1a | Fixed neurological deficit without meningeal or brain reaction | |
| 2 | Moderate to severe headache, cranial nerve palsy, nuchal rigidity | GCS 13–14 without motor deficit |
| 3 | Lethargy, confusion, mild focal deficit | GCS 13–14 with motor deficit |
| 4 | Stupor, hemiparesis, early decerebrate posturing | GCS 7–12 without or with motor deficit |
| 5 | Coma, decerebrate posturing, moribund appearance | GCS 3–6 without or with motor deficit |
Table 3.
Glasgow Coma Scale45
| Points | Eye Opening Response | Verbal Response | Motor Response |
|---|---|---|---|
| 6 | NA | NA | Obeys |
| 5 | NA | Oriented | Localizes to pain |
| 4 | Spontaneous | Confused | Withdraws to pain |
| 3 | To speech | Inappropriate | Flexor (decorticate) |
| 2 | To pain | Incomprehensible | Extensor (decerebrate) |
| 1 | None | None | None |
NA indicates not applicable.
Presentation refers to the manner in which the aneurysm came to medical attention. If the aneurysm was incidental, this refers to a clinical presentation requiring cerebral imaging that is clearly unrelated to the aneurysm such as head trauma, spine evaluation, headaches not attributable to the aneurysm (eg, migraine, tension), seizures, or neoplasm staging. Hemorrhage means bleeding in the subarachnoid, intracerebral, intraventricular, or subdural spaces. Any intraparenchymal hemorrhage must be described including location, linear size (length, width, and height) and volume (length×width×height/2). Seizure refers to abnormal epileptiform neuronal discharge that results in focal or generalized alterations of sensation, motor function, behavior, or consciousness.16 Focal neurological deficit refers to signs including any peripheral, axial, and cranial nerve dysfunction. Hydrocephalus is a clinical entity in which a disturbance of cerebrospinal fluid circulation causes the accumulation of cerebrospinal fluid, resulting in progressive ventricular dilatation and increased intracranial pressure.17 Elevation of intracranial pressure due to obstruction of flow or malabsorption of cerebrospinal fluid can result in cerebral herniation syndromes and alterations in level of consciousness with or without associated ventricular dilatation on imaging studies. Headache is subjective head pain often thunderclap in onset and classified as secondary in type attributed to subarachnoid hemorrhage.18 Additional pain descriptors for time of onset, rapidity of onset, change in frequency, character, or location should be included. All of these symptoms should be uniformly and consistently reported and documented in reference to the aneurysm evaluation.
Hemorrhage is the most important presentation of cerebral aneurysms in terms of prevalence and morbidity. Therefore, a clear distinction between hemorrhage versus no hemorrhage must be made definitively either by imaging and/or cerebrospinal fluid confirmation. Specific dates of each hemorrhage episode with the degree of intracranial hemorrhage and associated neurological deterioration must be clearly documented for each event in chronological order. See the section on aneurysm hemorrhage for reporting recommendations.
Patient Handedness
Handedness is obtained from the neurological history and estimates hemispheric dominance potentially influencing neurological injury/disability, functional outcome, and the choice of treatment modality.
Dates of Rupture, Diagnosis, and Treatment
Date of presentation refers to the date on which patient experienced signs or symptoms leading to medical evaluation and diagnosis of the cerebral aneurysm. Date of presentation may not be the same as the date of medical evaluation or diagnosis of the aneurysm but should be temporally related. Index date is the point at which patient initially experienced symptoms referable to the aneurysm.
Example
A man developed a severe headache with nausea and vomiting at 11:00 am on January 1, which slowly subsided. At approximately 8:30 pm on January 5, the patient grasped his head, cried out, and collapsed leading to emergency transfer to the nearest hospital. The patient was medically stabilized at 9:35 pm and CT brain scan at 10:10 pm demonstrated diffuse acute subarachnoid hemorrhage >1 mm in axial thickness, intraventricular hemorrhage, and hydrocephalus. The patient was diagnosed with Hunt and Hess19 Grade IV, Fisher20 CT Grade 3/421 (Fisher CT Grade 3/4 is used to describe diffuse subarachnoid hemorrhage >1 mm layering the basilar cisterns [Fisher CT Grade 3] with intraventricular hemorrhage [Fisher CT Grade 4]) subarachnoid hemorrhage. The nomenclature recognizing the subarachnoid hemorrhage component has prognostic significance for the development of cerebral vasospasm and delayed ischemic neurological deficits21 subarachnoid hemorrhage. Because the patient was comatose, a ventricular drainage catheter was placed with an opening pressure of 34 cm water. The patient was transferred to a regional medical center. A cerebral arteriogram was performed on January 6 at 7:55 am confirming the presence of a cerebral aneurysm. After multidisciplinary evaluation of operative techniques, endovascular aneurysm treatment was performed on January 6 at 8:40 am in a procedure that required 90 minutes, 17.5 minutes of fluoroscopy with estimated dose exposure of 9972 microGray per square meter.
The index date is January 1, the date of the “sentinel” hemorrhage. The date of presentation is January 5 at which time the patient first came to medical attention. The date of diagnosis in this case is January 6, the date on which catheter arteriography confirmed the clinical suspicion of cerebral aneurysm as the proximate cause of subarachnoid hemorrhage.
Time is an important concept in aneurysm treatment. Index time is 11:00 am on January 1. Time of presentation is 9:35 pm on January 5, and the time of treatment is 8:40 am on January 6. The duration to treatment is 11 hours 5 minutes. Procedure time is 1.5 hours.
Rationale for Description of Time and Symptoms of Onset.
The index date and date of presentation are necessary to assess the natural history of aneurysmal subarachnoid hemorrhage. It is useful to calculate the duration from original hemorrhage and recurrent hemorrhage, which may be associated with natural history of the disease and treatment risk. There is often some time lag between date of the index date and date of presentation as well as some lag time between date of presentation and the date of aneurysm treatment with surgery or coiling.
After aneurysmal subarachnoid hemorrhage, the risk of recurrent hemorrhage is greatest in the hours immediately after the initial hemorrhage22,23 with reported mortality rates of 70% to 90%.24 Although data remain somewhat limited, more patients achieved satisfactory functional outcomes when aneurysm surgery was performed within 3 days than patients in whom treatment was delayed >14 days.22,25 In the International Subarachnoid Aneurysm Trial (ISAT), patients in the endovascular group underwent aneurysm treatment in 1.1 day on average, whereas patients in the surgical group underwent treatment in 1.7 days on average, a 14-hour difference (P<0.001).26 Based on historical and prospective randomized data, delays from presentation to treatment may potentially have adverse effects on patient outcomes generating external bias on treatment effect.
Baseline Imaging: Brain and Aneurysm Imaging
Imaging of Aneurysm Hemorrhage
A description of the hemorrhage location and extent must be reported. Any intraparenchymal bleeding or hematomas with mass effect must be reported. The Fisher Grading Scale20 (Table 4) is a commonly used CT-based grading system that has prognostic significance for the development of arteriographic vasospasm and delayed ischemic neurological deficits.21
Table 4.
Fisher CT Grading Scale20
| Fisher Group | Blood Pattern on Nonenhanced CT |
|---|---|
| 1 | No subarachnoid blood detected |
| 2 | Diffuse or vertical layers <1 mm thick* |
| 3 | Localized clot or vertical layers ≥1 mm thick |
| 4 | Intracerebral or intraventricular clot with diffuse or no subarachnoid hemorrhage |
“Vertical” cisterns include interhemispheric, insular, and ambient.
Evidence of new acute hemorrhage (<7 days) is present if there appears to be acute blood products on CT or MRI likely to be associated with aneurysm presentation. If no hemorrhage is apparent on imaging studies yet clinical suspicion for subarachnoid hemorrhage remains, then lumbar puncture is indicated to evaluate for blood, glucose, protein, and xanthochromia. Details of cerebrospinal fluid analysis are described separately.27
Subacute hemorrhage (1 to 6 weeks) may be apparent as layering of red blood cells in dependent locations of the brain on CT or MRI such as occipital horns of the lateral ventricles, dorsal margins of the Sylvian fissures, and sulci of the cerebral convexities. Chronic hemorrhage (>6 weeks) may be apparent as hemoglobin degradation products on MRI. The modality used for diagnosis of hemorrhage (CT, MRI, or lumbar puncture) must be recorded.
Rationale for Detailed Description of Hemorrhage
The anatomic site of bleeding is important to determine the cause and consequences of hemorrhage. In the presence of multiple aneurysms, hemorrhage location may help to determine the source of hemorrhage and the lesion requiring immediate treatment. Significant hematomas with mass effect should be quantified28 and may require surgical evacuation at the time of aneurysm clipping. The extent of hemorrhage is a significant determinant of patient outcome.20
Imaging Sources and Dates
The imaging sources and dates of each CT, CT angiography, CT–perfusion, MRI, MR angiography, MR–perfusion, and diagnostic catheter cerebral arteriography nearest in time to the date of presentation should be reviewed and reported.
Rationale for Documentation of Imaging Performed to Localize the Aneurysm.
Anatomic information may be dependent on the imaging modality used to obtain that information. The most obvious example is a cerebral aneurysm that is not apparent on nonenhanced cross-sectional CT or MRI but later becomes apparent on contrast-enhanced CT, MR angiography, or catheter arteriography. Data sources can introduce bias into the interpretation of pathological data. For example, CT angiography or MR angiography may not accurately provide dome-to-neck ratio, particularly useful for determining the relevance of endovascular coil occlusion, need for adjunctive endovascular treatment methods such as balloon neck remodeling or stenting, or the clear requirement for cranial neurosurgery with aneurysm clipping, bypass and occlusion, or vessel reconstruction.29–31
Aneurysm Location and Side
Side refers to right of midline, midline, or left of midline. If there are multiple aneurysms, then the location of each aneurysm must be described separately. Also see the section on aneurysm location.
Rationale for Lateralization of Aneurysm.
The side of the aneurysm(s) may influence treatment risk in some cases, particularly in the “dominant” hemisphere.
Aneurysm Size and Morphology
Size, measured in millimeters, is ideally recorded from 2 sources such as MRI or CT angiography and catheter arteriography (Figs 1 and 2). The size in 3 dimensions is measured using the best projections in 3 orthogonal planes. On sectional imaging studies, the height is inferred from the slice gap and thickness by “stacking” multiple levels in the standard axial projection.
Fig 1.
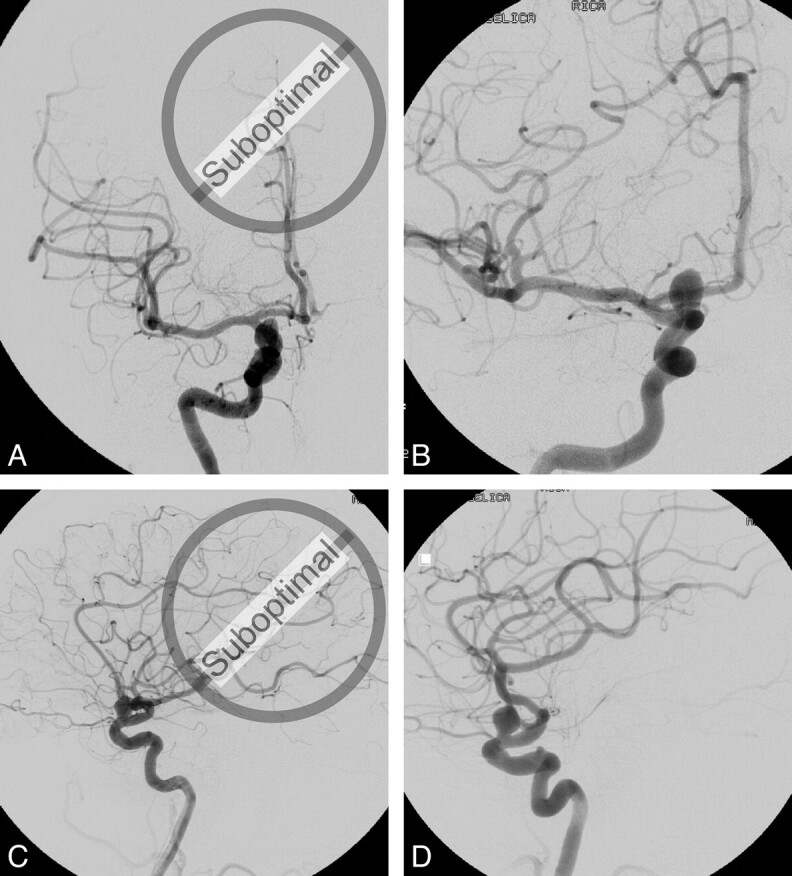
Arteriographic projections used to assess aneurysm dimensions. Posterior-anterior Townes and direct lateral projections demonstrate the presence of the right carotid–ophthalmic aneurysm, but these projections do not allow for optimal assessment of aneurysm size, dome-to-neck ratio, or artery-to-neck ratio. Magnified posterior-anterior Waters and lateral oblique projections in this particular case provide better planar imaging to assess the aneurysm for surgical or endovascular treatment.
Fig 2.
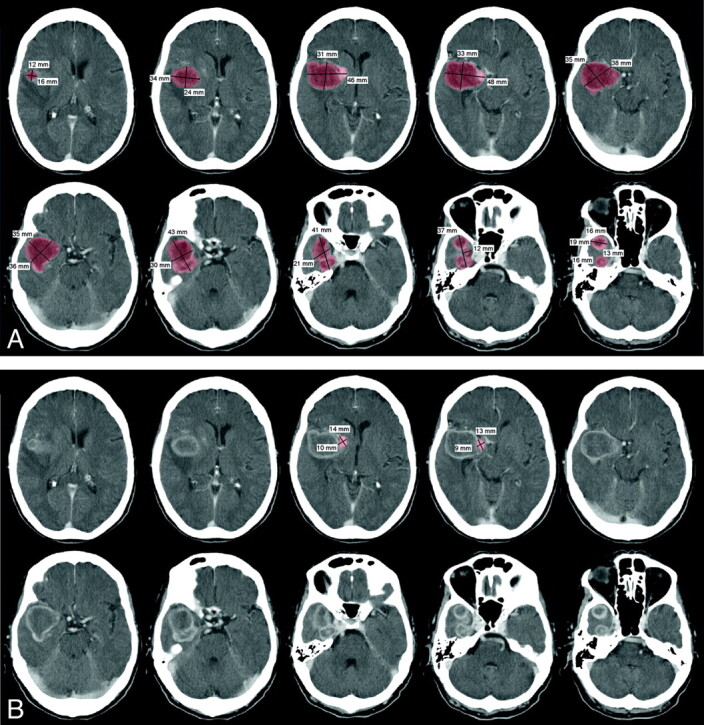
CT brain scan with intravenous iodinated contrast of a patient with a partially thrombosed, giant right middle cerebral aneurysm. A, 5-mm contiguous axial images through the aneurysm demonstrate a ring-enhancing mass with a maximal dimension of 4.8 cm and a total volume of 48 mL. B, The patent component of the aneurysm measures only 14 mm in maximal dimension with a volume of 1.33 mL. The opacified component of the aneurysm at catheter arteriography represents 2.8% of the total aneurysm volume.
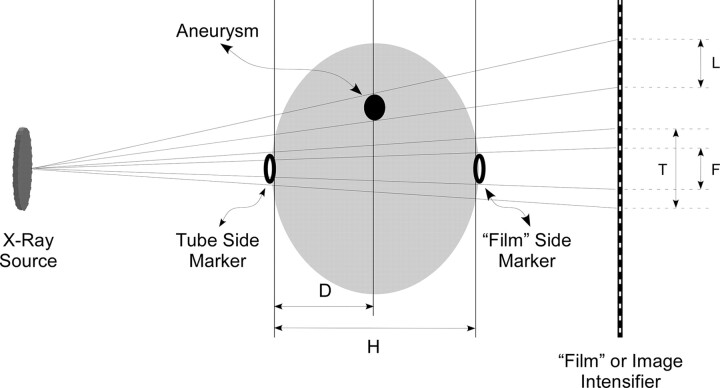
The size in 3 dimensions is measured on pretreatment catheter arteriography using best orthogonal projections profiling the aneurysm relative to the parent artery. For size calculations using planar projections, sizing markers must be placed on both sides of the head due to significant magnification that occurs (Fig 3). Computer workstations using rotational arteriography for 3-dimensional reconstructions usually include measurement features. Calibration and measurement error must be carefully assessed. Because windowing and leveling of 3-dimensional reconstructions may significantly alter aneurysm size and morphology, most accurate measurements are obtained from high-resolution planar images.
Fig 3.
Diagram of measurements to determine aneurysm dimensions without geometric magnification using 1-cm measuring rings attached to the patient's head. All measurements are made on radiographic images using x-rays. Tube side magnification factor (T), film-side magnification factor (F), and the uncorrected lesion size (L) are measured on the radiograph. The distance from the tube side of the head to the lesion (D) and the width of the head (H) are measured from radiographs in the orthogonal plane. The magnification factor (M) at the level of the lesion is derived by the following formula: . Due to inherent geometric magnification in radiographic images, the actual aneurysm size is calculated by dividing the apparent aneurysm size as follows: .
It is important to quantitatively assess aneurysm volume as closely as possible to later analyze volumetric occlusion achieved. Aneurysm volume is amenable to accurate quantitative assessment using CT/CT angiography or volumetric acquisition using MRI. On the basis of a planar catheter arteriogram or 3-dimensional reconstructions, volume must be estimated using one of several geometric formulas making best estimate of the aneurysm morphology and linear size measurements. The following formula, or variants, should be used.
Spheroid, Ellipsoid, and Cylindrical aneurysm:
Then, a calculation of coil volume can be made based on the coil type used, the number, and length of coil deployed into the aneurysm.
Arteriographic features of aneurysm morphology may be helpful in the assessment and approach to treatment of cerebral aneurysms. The aperture or orifice of an aneurysm has often been referred to as the aneurysm “neck,” whereas the body of the aneurysm has been called its “dome.” Dome-to-neck ratio, for instance, has been used to discriminate arteriographic features of aneurysms both favorable and unfavorable for durable endovascular treatment. A dome-to-neck ratio of 2:1 or greater may represent geometry conducive to endovascular coil occlusion without adjunctive methods.32 By convention, aneurysm neck size ≤4 mm has been referred to as small, whereas aneurysms with necks >4 mm have been called large neck aneurysms.33 In addition, the relationship of the parent artery diameter to the size of the aneurysm neck is an important discriminator for the requirement to use adjunctive techniques devices such as balloon neck remodeling or adjunctive devices such as stent-assisted coil occlusion of aneurysms. Although the dome-to-neck ratio may be favorable for primary endosaccular coil occlusion of an aneurysm, a 4-mm aneurysm neck relative to a 2-mm parent artery diameter may argue for the use of adjunctive devices to maintain blood flow in the parent artery. For treatment of large neck aneurysms, adjunctive use of balloon remodeling or stent-assisted aneurysm occlusion is often used.
Multilobulated or other complex shapes create difficulty in volume analysis and should be described. If 3-dimensional measurement capabilities are not present on the available imaging equipment, then volume must be mathematically estimated as accurately as possible. Irregular aneurysms may require arbitrary segmentation into more regular components for measurement and subsequent summation. If necessary, then the methodology for measurement must be described.
In summary, it is important to determine the best planar projections to evaluate aneurysm morphology based on either optimal orthogonal arteriographic projections or rotational arteriography with 3-dimensional reconstructions. The anatomic relationships of structures within the head may change during a procedure or between procedures due to brain swelling, hematoma, craniotomy/craniectomy, or other space-occupying lesion; or changes in vessel orientation due to clips, coils, stents, or other prosthetic devices. For this reason, it is incumbent on the operator to find the best angles to evaluate the aneurysm rather than relying on specific angiographic machine angles or bony landmarks on fluoroscopic images.
Rationale for Detailed Description of Aneurysm Size and Morphology.
The percentage of volumetric occlusion is infrequently reported but may be an important determinant of durable aneurysm occlusion. Both qualitative and quantitative (ie, partial, subtotal, complete, incomplete, near complete, and other such terms) occlusion (Table 6) should be reported for each procedure and in treatment series.
Table 6.
Consensus Grading Scale for Endovascular Aneurysm Occlusion
| Gradea,b | Definition |
|---|---|
| 0 | Complete aneurysm occlusion |
| 1 | 90% or greater aneurysm occlusion |
| 2 | 70–89% aneurysm occlusion |
| 3 | 50–69% aneurysm occlusion |
| 4 | 25–49% aneurysm occlusion |
| 5 | Less than 25% aneurysm occlusion |
The modifier “I” may be used to describe interstitial opacification within the confines of the coil mass.
The modifier “G” may be used to describe interval growth in the overall dimensions of the aneurysm as a separate phenomenon from coil compaction with recanalization of the aneurysm.
Digital, or electronically digitized, images with resolution of 150 to 300 dots per inch are necessary for digital analysis. The aneurysm obliteration rate can be calculated using imaging software (eg, Image, Version 1.62; National Institutes of Health, Bethesda, Md, http://rsb.info.nih.gov/nih-image/). This program, or one like it, can be used to calculate the area (number of pixels) of the aneurysm neck remnant and the area (number of pixels) of the embolic mass. This may not be the only method available to arrive at standardized measurements, but it represents a readily reproducible calculation. From these calculations, the aneurysm obliteration rate can be quantified as follows:
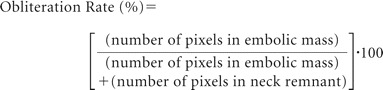 |
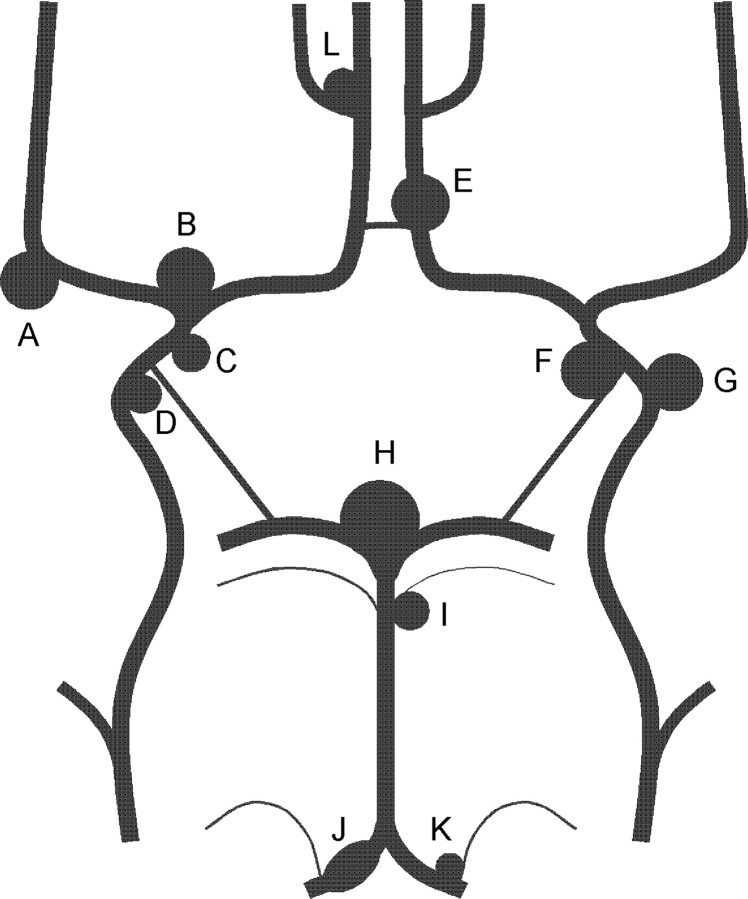
Aneurysm Location
Aneurysm locations are for grouping purposes. Location is determined by vascular distribution (Fig 4). Aneurysms are named according to the vessel of neck origin, closest branch vessel origin, or next best guess. Use of bony landmarks resulting in terms such as “supraclinoid” or nonspecific vessel locations such as “supraoptic” should be avoided. For reporting purposes, conventions of aneurysm naming are summarized in ISAT26 and ISUIA.4
Fig 4.
Common location of cerebral aneurysms surrounding the circle of Willis. (A) Middle cerebral (proximal to bifurcation, bifurcation, distal to bifurcation); (B) carotid terminus; (C) anterior choroidal; (D) superior hypophyseal; (E) anterior communicating (proximal to communicating artery, at communicating artery); (F) posterior communicating; (G) ophthalmic; (H) basilar artery (terminus, trunk); (I) superior cerebellar; (J) V4 segment, vertebral; (K) posterior inferior cerebellar; (L) pericallosal artery.
Rationale for Standardized Description of Aneurysm Location.
Epidemiological evidence indicates that aneurysm location affects risks for formation, growth, rupture, risk of treatment, and risk of recurrence. To promote accurate accumulation of these statistics, conformity to convention in naming by aneurysm location is important. Attributes of aneurysm location are listed in Table 5 combining taxonomy from ISAT and ISUIA, 2 long-range prospective studies.4,34
Table 5.
Proposed fields and ranges
| General Definitions (Choose all that apply) | |
|---|---|
| Clinical presentation | Hemorrhage |
| Incidental | Evidence of new hemorrhage |
| Hemorrhage | Age of new hemorrhage |
| Seizure | Is new hemorrhage symptomatic |
| Neurological deficit | Evidence of old hemorrhage |
| Headache | Age of old hemorrhage |
| Other | Was old hemorrhage symptomatic |
| Date of presentation | Evidence of new cerebral infarction |
| Imaging source and date | Evidence of intraparenchymal hemorrhage |
| Location and size | Size of parenchymal hemorrhage |
| Lesion side | Presence of mass effect |
| Right | Presence of hydrocephalus |
| Left | Opening pressure on insertion of ventricular catheter |
| Midline | Requirement for ongoing ventricular drainage |
| Handedness | Comorbid vascular conditions |
| Right | Fibromuscular dysplasia |
| Left | Arteriovenous malformation |
| Aneurysm size (greatest diameter in mm) | Bacterial endocarditis |
| Multiple aneurysms | Polycystic disease |
| No. of aneurysms | Familial history of aneurysms |
| Aneurysm location | Vascular occlusion |
| Internal carotid | Vascular anomalies |
| Proximal intradural or ophthalmic | Vasospasm |
| Posterior communicating | Nonatherosclerotic narrowing of the cerebral arteries |
| Bifurcation | Grading of vasospasm (mild, moderate, severe) |
| Other internal carotid | Possible clinical symptoms and signs related to vasospasm |
| Anterior cerebral | Treatment for vasospasm |
| Anterior communicating | Vasodilator, intra-arterial |
| Proximal to anterior communicating | Type and dosage of vasodilator |
| Pericallosal | Balloon angioplasty |
| Middle cerebral | Balloon type |
| Proximal to bifurcation | Vessels treated with angioplasty |
| Bifurcation | Technical success of endovascular treatment |
| Distal to main bifurcation | Unable to catheterize aneurysm |
| Posterior circulation | Unable to deploy adjunctive devices such as balloon or stent |
| Basilar bifurcation | Unable to deploy embolic materials in aneurysm |
| Basilar trunk | Embolic material herniation beyond aneurysm confines |
| Superior cerebellar | Neck remnant |
| Posterior cerebral | Interstitial opacification |
| Posterior inferior cerebellar | Near complete occlusion |
| Other posterior circulation | Complete occlusion |
Procedural Details
Therapeutic Procedural Technique
Procedural techniques vary widely and must be incorporated into every report. Arterial access procedure, anesthetic technique such as general anesthesia and agents used, the use of adjunctive medications including timing, dosages, routes of administration, assays of anticoagulation or platelet function, catheters, guide wires, contrast agents, rates and volumes with routes of administration, and fluoroscopy with measure of patient exposure should be incorporated into each report. Each embolic device must be carefully documented. The manufacturer, product type, length, diameter, and size of each coil type must be reported. Adjunctive devices such as balloon catheters for remodeling techniques and stents for blood flow remodeling or anatomic barrier formation must be detailed in their application and placement. Any liquid embolic material must be described in type, volume, and duration of administration.
Procedural Technical Success: Proposed Consensus Grading Scale for Aneurysm Occlusion
Careful assessment for complete versus incomplete aneurysm occlusion must be performed at the time of initial aneurysm treatment and at intervals after the treatment procedure to assess durability of aneurysm occlusion. The importance of planar angiographic sequences to optimally evaluate the aneurysm neck region has been previously described. If necessary, additional rotational arteriography with 3-dimensional reconstructions may be helpful. A detailed assessment of aneurysm occlusion may be important to determine the ultimate success of the endovascular treatment strategy.
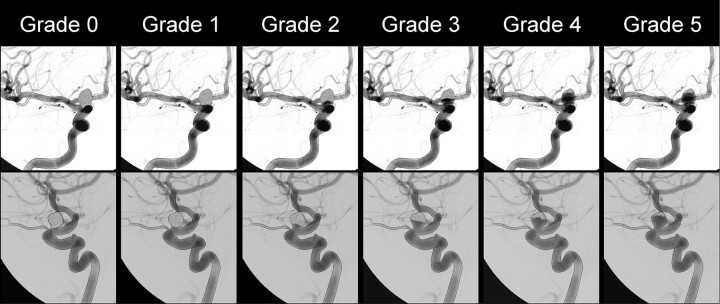
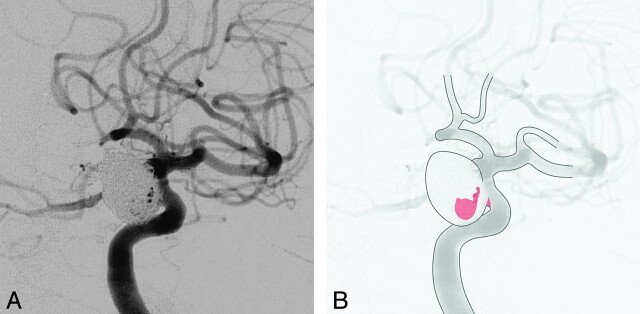
Aneurysmal remnants should be assessed for size, shape, and contrast (blood) flow patterns. Any aneurysm remnants must be described. For definition purposes, complete aneurysm occlusion can be reported only if no arteriographic opacification of any component of the aneurysm is present on multiple projections (Fig 5).
Fig 5.
Consensus grading scale for endovascular aneurysm occlusion is applied to orthogonal images obtained in optimal projections to assess aneurysm dimensions: Grade 0, complete aneurysm occlusion; Grade 1, ≥90% aneurysm occlusion; Grade 2, 70% to 89% aneurysm occlusion; Grade 3, 50% to 69% aneurysm occlusion; Grade 4, 25% to 49% aneurysm occlusion; Grade 5, <25% aneurysm occlusion.
Grading scales to assess aneurysm occlusion have been proposed,35 but none have been validated as predictive of patient outcome other than an association between residual aneurysm filling and a risk for subsequent hemorrhage in patients presenting with hemorrhage.26,36 By consensus of the participating parties, a new 6-point grading system has been proposed to account for a broader range of angiographic appearances than the most commonly used Raymond Scale. Grade 0 indicates complete and total aneurysm occlusion without remnant or interstitial filling within the aneurysm. Depending on the coil type used, complete occlusion may or may not be synonymous with complete radio-opacity of the aneurysm lumen because certain coil systems are only partially radio-opaque. Assessment must be made based on the distribution of liquid contrast material during arteriographic acquisitions in 2 optimal orthogonal projections. Grade 1 represents ≥90% volumetric occlusion of the aneurysm based on planar imaging assessment. Grade 2 includes 70% to 89% volumetric aneurysm occlusion. Grade 3 includes 50% to 69% aneurysm occlusion. Grade 4 should include 25% to 49% aneurysm occlusion, and Grade 5 represents less than 25% volumetric aneurysm occlusion. (See Table 6 and Fig 5 for a summary and pictorial explanation.)
There are 2 angiographic appearances of contrast material in an aneurysm treated with endovascular occlusion. Interstitial opacification, or interstitial recanalization, describes contrast opacification within the confines of the radio-opaque or radiolucent coil or other prosthetic mass within the aneurysm sac. The natural history of this type of aneurysm filling remains uncertain and may undergo thrombosis with involution or progressive enlargement of the patent portion of the aneurysm.37 Remnant opacification, or remnant recanalization, describes an untreated component of the aneurysm in which there is no prosthetic material. Because several aneurysm coil products now on the market may undergo degradation leading to interstitial or remnant recanalization, reporting of this anatomic configuration remains necessary. Pathologically, interstitial opacification may represent anatomic clefts within or adjacent to the coil mass predisposing to regrowth of the aneurysm (Fig 6).
Fig 6.
Modification to consensus grading scale for endovascular aneurysm occlusion describing interstitial opacification within coil mass. A, Left internal carotid arteriography in right frontal oblique projection during the arterial phase of injection shows coil occlusion of a 12×11×14 mm left posterior communicating artery aneurysm. B, Because there is a small ventral neck remnant and residual opacification within the aneurysm sac (colored areas), this represents consensus Grade 1 occlusion with “I” for persistent interstitial opacification within the coil mass.
Reassessment for aneurysm regrowth must be performed on an interval basis, at the operator's discretion, but is strongly recommended within the first year.34 In an effort to standardize the evaluation process, it is important to select a common time for re-evaluation. A survey of many operators and publications indicates that 6 months posttreatment is a common convention within the first year and is therefore recommended. Thereafter, an additional re-evaluation at 18 months from initial treatment is suggested. Catheter arteriography remains the gold standard for reassessment of previously treated aneurysms, although the role of CT angiography and MRI is under evaluation.38,39 Follow-up arteriography should include identical “best projections” used at the time of the original treatment to minimize errors in measurement for changes in morphology and the degree of aneurysm occlusion. Maximum reproducibility is of paramount importance in the assessment of treatment success. Rotational arteriography can be helpful to determine best projections, but reproducible magnification planar imaging projections are the key to proper assessment.
Using the proposed consensus grading scale for endovascular aneurysm occlusion, follow-up evaluation should include assessment of change in the status of aneurysm occlusion. If the aneurysm is unchanged in size, configuration, and volumetric occlusion, then the term, “stable” is applied. If progressive aneurysm occlusion or involution has occurred, then the term “improved” should be applied and the appropriate consensus grading scale should be stated. If the aneurysm has grown in size or changed in arteriographic configuration such that the embolic material no longer results in the same or greater volumetric occlusion of the aneurysm, then the term, “worsened” must be applied to the follow-up assessment and the appropriate proposed consensus grading scale should be stated.
Rationale for the Universal 6-Point Grading System.
The proposed consensus grading scale to assess endovascular aneurysm occlusion is meant to standardize the reporting on the degree to which volumetric occlusion has been achieved (Fig 5). To properly assess technical outcomes, new technologies, and methodologies for endovascular aneurysm treatment, standardization in reporting is critical. The degree to which endovascular aneurysm occlusion determines clinical outcome, rebleed rates, and procedural and long-term morbidity remains unclear. Reproducibility and high rates of interobserver concurrence are imperative. The Raymond scale is a commonly used outcome grading scale that divides the arteriographic outcomes of endovascularly treated saccular aneurysms into 3 categories: (1) complete occlusion; (2) residual neck; and (3) residual aneurysm.35 However, despite its simplicity, its application during industry-sponsored registries demonstrated significant interobserver variability that may limit its application and efficacy as an outcome assessment tool.40 Moreover, significant changes in aneurysm morphology and occlusion may occur within the same category using the 3-category scale. For instance, remnant opacification may increase from 2 mm to 6 mm yet still represent a Raymond Class 2 remnant. A more complete grading scale would, therefore, be desirable, one that may offer high levels of interobserver concordance. There is no literature support for the proposed consensus grading system included here, although this writing group believes it is the best available grading scale at the present time and offers a greater likelihood of reporting additional degrees of aneurysm recurrence.
After aneurysm treatment, surveillance imaging is mandatory, yet there are little data on appropriate screening intervals. For research purposes, catheter arteriography is the procedure of choice for optimal characterization of interstitial and remnant opacification. The timing of angiography needs to be standardized and is arbitrarily set at 6 months and 18 months after a treatment procedure to reflect the most common practice. The role of MRI/MR angiography in this process is under investigation currently showing 71% to 97% sensitivity and 89% to 100% specificity for overall recurrence41; however, the usefulness of MRI/MR angiography to depict interstitial and graded remnant recanalization remains unknown. Factors that favor more rapid re-evaluation include previously ruptured aneurysms, incompletely occluded aneurysms, and aneurysm locations where coil compaction is more likely such as the basilar artery terminus. Intermittent follow-up using catheter arteriography or MRI techniques should be performed even in well-occluded aneurysms to document aneurysm recurrence to potentially prevent recurrent hemorrhage42 and to evaluate for de novo and additional aneurysms that may occur in up to 8% and 20% of patients with aneurysm, respectively.43,44 Although the specific interval for this follow-up evaluation remains uncertain, these data suggest that intervals of ≤5 years may be appropriate. It is the responsibility of the treating physician and authors performing research on these topics to ensure that treated patients with aneurysm are not lost to follow-up. Patient records should be maintained in a Health Insurance Portability and Accountability Act-compliant database. Follow-up evaluation and data recording of inpatient clinical records should include both functional and angiographic assessment using standard outcome measures, including the Glasgow Outcome Scale,45 Modified Rankin Scale,46 Barthel Index,47 and the proposed consensus grading scale. Concurrent reporting of the National Institutes of Health Stroke Scale represents a well-accepted and complementary measure of any neurological deficits.48,49
In patients who have subarachnoid hemorrhage after treatment for ruptured or unruptured aneurysms, there should be an effort to determine the cause of hemorrhage in all cases, including the probable cause of recurrent hemorrhage.
Procedural Complications
A stroke is any sudden development of neurological deficits attributable to cerebral ischemia, infarction, or hemorrhage. Stroke is both a complication of cerebral arteriography and endovascular aneurysm treatment, but may also be part of the natural history of a ruptured aneurysm. Stroke is, therefore, also a major outcome measure of the effectiveness of aneurysm evaluation with arteriography and endovascular treatment. The stroke may occur in the vascular distribution of the aneurysm or in other cerebral vascular territories. Neurological deficits as a complication of the procedure may be due to embolism, hemorrhage, or flow impairment. Hemorrhage is a well-documented risk of catheter-based procedures and is detailed separately.
Neurological deficits should be listed in reference to the vascular distribution of the treated aneurysm or other cerebral vascular distribution. Patients with new neurological deficits should undergo brain imaging. New neurological deficits lasting fewer than 24 hours are transient ischemic attacks. However, some authors have shown that even very brief deficits lasting only minutes may be associated with diffusion-weighted abnormalities on MRI representing strokes. Thus, cerebral infarction on CT or MRI can be asymptomatic or symptomatic. New neurological deficits lasting at least 24 hours are defined as cerebrovascular accident or stroke. Stroke events lasting ≥24 hours may also be transient and become asymptomatic on physical examination, yet include CT or MRI evidence of infarction. Cerebrovascular accident, or stroke, may be permanent and cause minor deficits (increased National Institutes of Health Stroke Scale <4 points) or major deficits (increase in National Institutes of Health Stroke Scale ≥4 points; Table 7). Other major complications include myocardial infarction and death, which, in combination with stroke, are the major adverse events used to compare carotid stenting and endarterectomy. Complications within 30 days of the procedure are considered perioperative and procedure-related. Because deaths are frequently secondary to stroke or myocardial infarction, it is misleading to sum the individual totals of stroke, myocardial infarctions, and death. Rather, a combined rate of nonfatal stroke, nonfatal myocardial infarction, and death should also be reported with cause of death described. For other complications, the authors provide a list by consensus of potential complications, a method for their classification, and grading according to type and severity used in similar reporting documents (Tables 8 and 9).50 Postoperative assessment for complications should be performed by an independent physician, preferably an independent neurologist or other physician certified in the National Institutes of Health Stroke Scale and other outcome assessment scoring systems. MRI of the brain with diffusion-weighted imaging is the most sensitive test to the presence of acute ischemia.51 After development of acute ischemic stroke associated with aneurysm treatment, MRI with diffusion-weighted imaging is indicated for further evaluation. Diffusion-weighted imaging-positive cerebral infarction after endovascular aneurysm occlusion may be subclinical.52,53 If MRI with diffusion-weighted imaging is obtained for any reason, then the presence of diffusion-weighted imaging-positive cerebral ischemia with infarction regardless of clinical symptomatology should be reported.54
Table 7.
Definition and grading of neurological deficits
| Definition | Description |
|---|---|
| Complication | Neurological deterioration, NIHSS ≥1 |
| Transient ischemic attack | Resolution of new focal deficit within 24 hours |
| No CT or MRI evidence of infarction | |
| Cerebrovascular accident, symptomatic | Greater than 30 days duration |
| Major | NIHSS ≥4, mRS ≥3 |
| Minor | NIHSS <4, mRS ≤2 |
NIHSS indicates National Institutes of Health Stroke Scale; mRS, Modified Rankin Scale.
Table 8.
Classification of complications
| Complication | Category of Complication |
|---|---|
| Abscess | Infectious/inflammatory |
| Angina/coronary ischemia | Cardiac |
| Idiosyncratic reaction | Medication-related |
| Allergic/anaphylactoid reaction | Contrast-related |
| Arterial occlusion/thrombosis, puncture site | Vascular |
| Arterial occlusion/thrombosis, remote from puncture site | Vascular |
| Arteriovenous fistula | Vascular |
| Congestive heart failure | Cardiac |
| Device malfunction with adverse effect | Device-related |
| Death related to procedure | Death |
| Death unrelated to procedure (30-day mortality) | Death |
| Dysrhythmia, cardiac | Cardiac |
| Embolization, arterial | Vascular |
| Fluid/electrolyte imbalance | General nonvascular |
| Hematoma bleed, remote site | Vascular |
| Hematoma bleed at needle, device path: nonvascular procedure | Vascular |
| Hematoma bleed, puncture site: vascular procedure | Vascular |
| Incorrect drug | Medication-related |
| Incorrect dosage | Medication-related |
| Intimal injury/dissection | Vascular |
| Ischemia/infarction of tissue/organ | Vascular |
| Incorrect site of administration | Medication-related |
| Local infection | Infectious/inflammatory |
| Liver failure | General nonvascular |
| Migration of embolic material from target site | Device-related |
| Myocardial infarction | Cardiac |
| Malposition | Device-related |
| Nausea/vomiting | General nonvascular |
| Other (cardiac) | Cardiac |
| Other (contrast-related) | Contrast-related |
| Other (central nervous system complication) | Neurologic |
| Other dose-dependent complication | Contrast-related |
| Other (device-related) | Device-related |
| Other (gastrointestinal) | General nonvascular |
| Other (general nonvascular) | General nonvascular |
| Other (hematologic) | General nonvascular |
| Other (infectious/inflammatory) | Infectious/inflammatory |
| Other (medication-related) | Medication-related |
| Other (neurologic) | Neurologic |
| Other (respiratory/pulmonary) | Respiratory/pulmonary |
| Other (vascular) | Vascular |
| Pancreatitis | Infectious/inflammatory |
| Pulmonary embolism | Respiratory/pulmonary |
| Pulmonary embolism | Vascular |
| Peritonitis | Infectious/inflammatory |
| Hypotension | Cardiac |
| Hypoxia | Respiratory/pulmonary |
| Pulmonary edema | Respiratory/pulmonary |
| Peripheral nervous system complication | Neurologic |
| Pneumothorax | Respiratory/pulmonary |
| Pseudoaneurysm | Vascular |
| Respiratory arrest | Respiratory/pulmonary |
| Renal failure | Contrast-related |
| Septicemia/bacteremia | Infectious/inflammatory |
| Seizure | Neurologic |
| Septic shock | Infectious/inflammatory |
| Stroke, ischemic | Neurologic |
| Stroke, hemorrhagic | Neurologic |
| Tissue extravasation | Contrast-related |
| Transient ischemic attack | Neurologic |
| Unintended perforation of hollow viscus | General nonvascular |
| Vascular perforation or rupture | Vascular |
| Vagal reaction | Cardiac |
| Vasospasm | Vascular |
| Venous occlusion/thrombosis, puncture site | Vascular |
| Venous occlusion/thrombosis, remote from puncture site | Vascular |
Table 9.
Definitions of complications
| Minor complications |
| A. No therapy, no consequence |
| B. Nominal therapy, no consequence; includes overnight admission for observation only |
| Major complications |
| C. Require therapy, minor change in length of hospitalization (<48 hours) |
| D. Require major therapy, unplanned increase in level of care, prolonged hospitalization (>48 hours) |
| E. Permanent adverse sequelae |
| F. Death |
Rationale for Complication Reporting.
Medical complications remain as important to the functional outcome of patients with aneurysmal subarachnoid hemorrhage as rebleeding.55–57 Ongoing developments in stroke and intensive care neurology aim to improve overall patient outcomes by optimizing medical care in specialty treatment units.58–60
The justification for treatment of unruptured aneurysms has been more complex and has depended predominantly on an assessment of risk of future rupture (between 0.05% and 3.2% per annum for aneurysms less than 10 mm4,61,62 and up to 5.5% per annum for large aneurysms63) compared with the risks and efficacy of treatment. If the treatment-related morbidity and mortality were unknown or high, then treatment could not be justified. For craniotomy and aneurysm clipping, the risk of morbidity and mortality ranges from 0% to 7% for death and 4% to 15.3% for complications.2 Meta-analysis of surgery for unruptured aneurysm data shows similarly wide ranging risk profiles: 1% to 2.6% mortality and 4% to 10.9% morbidity.64,65 Endovascular therapy has been applied to unruptured aneurysms with comparatively low morbidity and mortality. In the ISUIA, endovascular morbidity and mortality ranged from 7.1% to 9.8%, whereas surgical morbidity and mortality ranged from 10.1% to 12.6%.4 However, the long-term efficacy of endovascular therapy in reducing or eliminating future rupture has not yet been determined. In certain surgical series, the risk of aneurysmal hemorrhage after surgical clipping ranged from 1.4% to 2.2% and 9% to 12% at 10 and 20 years after surgery, respectively.66,67 To date, there has been no randomized trial comparing methods used to treat unruptured cerebral aneurysms.
Summary
These definitions span a broad range of relevant clinical and radiographic parameters to be considered in research studies. These recommendations do not represent the only criteria for all reporting of research data related to cerebral aneurysms. For example, some architectural features described here are based on the consensus of a multidisciplinary panel. Moreover, additional technological advancements in imaging equipment will likely allow evaluation of cerebral hemodynamics but are currently not readily available.
These operational definitions were selected by consensus of this writing group to provide consistency for reporting on imaging in clinical trials and observational studies involving cerebral aneurysms. These definitions will hopefully allow different groups to publish results that are directly comparable.
Disclosures
Dr Higashida served as a consultant to Cordis Neurovascular. Dr Nesbit received honoraria from Cordis Neurovascular and Genentech, has an ownership interest in Concentric Medical, and served as a consultant to Concentric Medical. Dr Wechsler served as a consultant to Nuevelo, Inc, and Abbott Vascular. Dr Lavine received honoraria from Cordis Neurovascular. Dr Rasmussen received honoraria from the Universities of Minnesota and Pittsburgh, Microvention/Terumo, ev3, Possis Medical/Medrad, and Micrus, has an ownership interest in Chestnut Medical, and served as a consultant to Chestnut Medical.
Footnotes
Reprinted with permission from Philip M. Meyers, H. Christian Schumacher, Randall T. Higashida, Colin P. Derdeyn, Gary M. Nesbit, David Sacks, Lawrence R. Wechsler, Joshua B. Bederson, Sean D. Lavine, and Peter Rasmussen. “Reporting Standards for Endovascular Repair of Saccular Intracranial Cerebral Aneurysms” Stroke 2009;40:e366 doi: 10.1161/STROKEAHA.108.527572
References
- 1. Johnston SC, Higashida RT, Barrow DL, Caplan LR, Dion JE, Hademenos G, Hopkins LN, Molyneux A, Rosenwasser RH, Vinuela F, Wilson CB. Recommendations for the endovascular treatment of intracranial aneurysms: a statement for healthcare professionals from the Committee on Cerebrovascular Imaging of the American Heart Association Council on Cardiovascular Radiology. Stroke 2002; 33: 2536–2544 [DOI] [PubMed] [Google Scholar]
- 2. Bederson JB, Awad IA, Wiebers DO, Piepgras D, Haley EC, Jr, Brott T, Hademenos G, Chyatte D, Rosenwasser R, Caroselli C. Recommendations for the management of patients with unruptured intracranial aneurysms: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Stroke 2000; 31: 2742–2750 [DOI] [PubMed] [Google Scholar]
- 3. Unruptured intracranial aneurysms—risk of rupture and risks of surgical intervention. International Study of Unruptured Intracranial Aneurysms investigators. N Engl J Med 1998; 339: 1725–1733 [DOI] [PubMed] [Google Scholar]
- 4. Wiebers DO, Whisnant JP, Huston J, III, Meissner I, Brown RD, Jr, Piepgras DG, Forbes GS, Thielen K, Nichols D, O'Fallon WM, Peacock J, Jaeger L, Kassell NF, Kongable-Beckman GL, Torner JC. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 2003; 362: 103–110 [DOI] [PubMed] [Google Scholar]
- 5. Cloft HJ, Kallmes DF, Kallmes MH, Goldstein JH, Jensen ME, Dion JE. Prevalence of cerebral aneurysms in patients with fibromuscular dysplasia: a reassessment. J Neurosurg 1998; 88: 436–440 [DOI] [PubMed] [Google Scholar]
- 6. Fick GM, Gabow PA. Natural history of autosomal dominant polycystic kidney disease. Annu Rev Med 1994; 45: 23–29 [DOI] [PubMed] [Google Scholar]
- 7. Halim AX, Singh V, Johnston SC, Higashida RT, Dowd CF, Halbach VV, Lawton MT, Gress DR, McCulloch CE, Young WL. Characteristics of brain arteriovenous malformations with coexisting aneurysms: a comparison of two referral centers. Stroke 2002; 33: 675–679 [DOI] [PubMed] [Google Scholar]
- 8. Krex D, Rohl H, Konig IR, Ziegler A, Schackert HK, Schackert G. Tissue inhibitor of metalloproteinases-1, -2, and -3 polymorphisms in a white population with intracranial aneurysms. Stroke 2003; 34: 2817–2821 [DOI] [PubMed] [Google Scholar]
- 9. Sanders WP, Sorek PA, Mehta BA. Fenestration of intracranial arteries with special attention to associated aneurysms and other anomalies. AJNR Am J Neuroradiol 1993; 14: 675–680 [PMC free article] [PubMed] [Google Scholar]
- 10. Zink WE, Komotar RJ, Meyers PM. Internal carotid aplasia/hypoplasia and intracranial saccular aneurysms: series of three new cases and systematic review of the literature. J Neuroimaging 2007; 17: 141–147 [DOI] [PubMed] [Google Scholar]
- 11. Sacco RL, Wolf PA, Bharucha NE, Meeks SL, Kannel WB, Charette LJ, McNamara PM, Palmer EP, D'Agostino R. Subarachnoid and intracerebral hemorrhage: natural history, prognosis, and precursive factors in the Framingham study. Neurology 1984; 34: 847–854 [DOI] [PubMed] [Google Scholar]
- 12. Bonita R. Cigarette smoking, hypertension and the risk of subarachnoid hemorrhage: a population-based case–control study. Stroke 1986; 17: 831–835 [DOI] [PubMed] [Google Scholar]
- 13. Raaymakers TW, Rinkel GJ, Ramos LM. Initial and follow-up screening for aneurysms in families with familial subarachnoid hemorrhage. Neurology 1998; 51: 1125–1130 [DOI] [PubMed] [Google Scholar]
- 14. Schievink WI, Schaid DJ, Michels VV, Piepgras DG. Familial aneurysmal subarachnoid hemorrhage: a community-based study. J Neurosurg 1995; 83: 426–429 [DOI] [PubMed] [Google Scholar]
- 15. Linn FH, Rinkel GJ, Algra A, van Gijn J. Incidence of subarachnoid hemorrhage: role of region, year, and rate of computed tomography: a meta-analysis. Stroke 1996; 27: 625–629 [DOI] [PubMed] [Google Scholar]
- 16. Proposal for classification of epilepsies and epileptic syndromes. Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia 1985; 26: 268–278 [PubMed] [Google Scholar]
- 17. Mori K, Shimada J, Kurisaka M, Sato K, Watanabe K. Classification of hydrocephalus and outcome of treatment. Brain Dev 1995; 17: 338–348 [DOI] [PubMed] [Google Scholar]
- 18. Headache Classification Subcommittee of the International Headache Society . The International Classification of Headache Disorders, 2nd edition. Cephalalgia 2004; 24 (suppl 1): 9–160 [DOI] [PubMed] [Google Scholar]
- 19. Hunt WE, Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg 1968; 28: 14–20 [DOI] [PubMed] [Google Scholar]
- 20. Fisher CM, Kistler JP, Davis JM. Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery 1980; 6: 1–9 [DOI] [PubMed] [Google Scholar]
- 21. Weir B, Macdonald RL, Stoodley M. Etiology of cerebral vasospasm. Acta Neurochir Suppl 1999; 72: 27–46 [DOI] [PubMed] [Google Scholar]
- 22. Kassell NF, Torner JC, Haley EC, Jr, Jane JA, Adams HP, Kongable GL. The International Cooperative Study on the Timing of Aneurysm Surgery. Part 1: overall management results. J Neurosurg 1990; 73: 18–36 [DOI] [PubMed] [Google Scholar]
- 23. Kassell NF, Torner JC, Jane JA, Haley EC, Jr, Adams HP. The International Cooperative Study on the Timing of Aneurysm Surgery. Part 2: surgical results. J Neurosurg 1990; 73: 37–47 [DOI] [PubMed] [Google Scholar]
- 24. Rosenorn J, Eskesen V, Schmidt K, Ronde F. The risk of rebleeding from ruptured intracranial aneurysms. J Neurosurg 1987; 67: 329–332 [DOI] [PubMed] [Google Scholar]
- 25. Haley EC, Jr, Kassell NF, Torner JC. The International Cooperative Study on the Timing of Aneurysm Surgery. The North American experience. Stroke 1992; 23: 205–214 [DOI] [PubMed] [Google Scholar]
- 26. Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, Holman R. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 2002; 360: 1267–1274 [DOI] [PubMed] [Google Scholar]
- 27. Clinical policy for the initial approach to adolescents and adults presenting to the emergency department with a chief complaint of headache. American College of Emergency Physicians. Ann Emerg Med 1996; 27: 821–844 [DOI] [PubMed] [Google Scholar]
- 28. Kothari RU, Brott T, Broderick JP, Barsan WG, Sauerbeck LR, Zuccarello M, Khoury J. The ABCs of measuring intracerebral hemorrhage volumes. Stroke 1996; 27: 1304–1305 [DOI] [PubMed] [Google Scholar]
- 29. Hoh BL, Cheung AC, Rabinov JD, Pryor JC, Carter BS, Ogilvy CS. Results of a prospective protocol of computed tomographic angiography in place of catheter angiography as the only diagnostic and pretreatment planning study for cerebral aneurysms by a combined neurovascular team. Neurosurgery 2004; 54: 1329–1340; discussion 1340–134 [DOI] [PubMed] [Google Scholar]
- 30. Kallmes DF, Layton K, Marx WF, Tong F. Death by nondiagnosis: why emergent CT angiography should not be done for patients with subarachnoid hemorrhage. AJNR Am J Neuroradiol 2007; 28: 1837–1838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Karamessini MT, Kagadis GC, Petsas T, Karnabatidis D, Konstantinou D, Sakellaropoulos GC, Nikiforidis GC, Siablis D. CT angiography with three-dimensional techniques for the early diagnosis of intracranial aneurysms. Comparison with intra-arterial DSA and the surgical findings. Eur J Radiol 2004; 49: 212–223 [DOI] [PubMed] [Google Scholar]
- 32. Debrun GM, Aletich VA, Kehrli P, Misra M, Ausman JI, Charbel F, Shownkeen H. Aneurysm geometry: an important criterion in selecting patients for Guglielmi detachable coiling. Neurol Med Chir (Tokyo) 1998; 38 (suppl): 1–20 [DOI] [PubMed] [Google Scholar]
- 33. Vinuela F, Duckwiler G, Mawad M. Guglielmi detachable coil embolization of acute intracranial aneurysm: perioperative anatomical and clinical outcome in 403 patients. J Neurosurg 1997; 86: 475–482 [DOI] [PubMed] [Google Scholar]
- 34. Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, Sandercock P. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet 2005; 366: 809–817 [DOI] [PubMed] [Google Scholar]
- 35. Roy D, Milot G, Raymond J. Endovascular treatment of unruptured aneurysms. Stroke 2001; 32: 1998–2004 [DOI] [PubMed] [Google Scholar]
- 36. Sluzewski M, van Rooij WJ. Early rebleeding after coiling of ruptured cerebral aneurysms: incidence, morbidity, and risk factors. AJNR Am J Neuroradiol 2005; 26: 1739–1743 [PMC free article] [PubMed] [Google Scholar]
- 37. Raymond J, Guilbert F, Weill A, Roy D. Follow-up of treated aneurysms: the challenge of recurrences and potential solutions. Neuroimaging Clin N Am 2006; 16: 513–523, ix [DOI] [PubMed] [Google Scholar]
- 38. Majoie CB, Sprengers ME, van Rooij WJ, Lavini C, Sluzewski M, van Rijn JC, den Heeten GJ. MR angiography at 3T versus digital subtraction angiography in the follow-up of intracranial aneurysms treated with detachable coils. AJNR Am J Neuroradiol 2005; 26: 1349–1356 [PMC free article] [PubMed] [Google Scholar]
- 39. Yamada N, Hayashi K, Murao K, Higashi M, Iihara K. Time-of-flight MR angiography targeted to coiled intracranial aneurysms is more sensitive to residual flow than is digital subtraction angiography. AJNR Am J Neuroradiol 2004; 25: 1154–1157 [PMC free article] [PubMed] [Google Scholar]
- 40. Sluzewski M, van Rooij WJ. Questionable interpretation of results of active study on Matrix coils by Boston Scientific. AJNR Am J Neuroradiol 2005; 26: 1882–1883 [PMC free article] [PubMed] [Google Scholar]
- 41. Pierot L, Delcourt C, Bouquigny F, Breidt D, Feuillet B, Lanoix O, Gallas S. Follow-up of intracranial aneurysms selectively treated with coils: prospective evaluation of contrast-enhanced MR angiography. AJNR Am J Neuroradiol 2006; 27: 744–749 [PMC free article] [PubMed] [Google Scholar]
- 42. Mawad M. Subarachnoid hemorrhage due to late recurrence of a previously unruptured aneurysm after complete endovascular occlusion. AJNR Am J Neuroradiol 1998; 19: 1810–1811 [PMC free article] [PubMed] [Google Scholar]
- 43. Wirth FP. Surgical treatment of incidental intracranial aneurysms. Clin Neurosurg 1986; 33: 125–135 [PubMed] [Google Scholar]
- 44. Tsutsumi K, Ueki K, Morita A, Usui M, Kirino T. Risk of aneurysm recurrence in patients with clipped cerebral aneurysms: results of long-term follow-up angiography. Stroke 2001; 32: 1191–1194 [DOI] [PubMed] [Google Scholar]
- 45. Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet 1974; 13: 81–84 [DOI] [PubMed] [Google Scholar]
- 46. de Haan R, Limburgh M, Bossuyt P, van der MJ, Aaronson N. The clinical meaning of Rankin ‘handicap’ grades after stroke. Stroke 1995; 26: 2027–2030 [DOI] [PubMed] [Google Scholar]
- 47. Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J 1965; 14: 61–65 [PubMed] [Google Scholar]
- 48. Brott T, Adams HP, Jr, Olinger CP, Marler JR, Barsan WG, Biller J, Spilker J, Holleran R, Eberle R, Hertzberg V. Measurements of acute cerebral infarction: a clinical examination scale. Stroke 1989; 20: 864–870 [DOI] [PubMed] [Google Scholar]
- 49. Josephson SA, Hills NK, Johnston SC. NIH Stroke Scale reliability in ratings from a large sample of clinicians. Cerebrovasc Dis 2006; 22: 389–395 [DOI] [PubMed] [Google Scholar]
- 50. Higashida RT, Meyers PM, Phatouros CC, Connors JJ, III, Barr JD, Sacks D. Reporting standards for carotid artery angioplasty and stent placement. Stroke 2004; 35: e112–34 [DOI] [PubMed] [Google Scholar]
- 51. Chalela JA, Kidwell CS, Nentwich LM, Luby M, Butman JA, Demchuk AM, Hill MD, Patronas N, Latour L, Warach S. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet 2007; 369: 293–298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Biondi A, Oppenheim C, Vivas E, Casasco A, Lalam T, Sourour N, Jean LL, Dormont D, Marsault C. Cerebral aneurysms treated by Guglielmi detachable coils: evaluation with diffusion-weighted MR imaging. AJNR Am J Neuroradiol 2000; 21: 957–963 [PMC free article] [PubMed] [Google Scholar]
- 53. Rordorf G, Bellon RJ, Budzik RE, Jr, Farkas J, Reinking GF, Pergolizzi RS, Ezzeddine M, Norbash AM, Gonzalez RG, Putman CM. Silent thromboembolic events associated with the treatment of unruptured cerebral aneurysms by use of Guglielmi detachable coils: prospective study applying diffusion-weighted imaging. AJNR Am J Neuroradiol 2001; 22: 5–10 [PMC free article] [PubMed] [Google Scholar]
- 54. Oppenheim C, Lamy C, Touze E, Calvet D, Hamon M, Mas JL, Meder JF. Do transient ischemic attacks with diffusion-weighted imaging abnormalities correspond to brain infarctions? AJNR Am J Neuroradiol 2006; 27: 1782–1787 [PMC free article] [PubMed] [Google Scholar]
- 55. Solenski NJ, Haley EC, Jr, Kassell NF, Kongable G, Germanson T, Truskowski L, Torner JC. Medical complications of aneurysmal subarachnoid hemorrhage: a report of the multicenter, cooperative aneurysm study. Participants of the Multicenter Cooperative Aneurysm Study. Crit Care Med 1995; 23: 1007–1017 [DOI] [PubMed] [Google Scholar]
- 56. Hutter BO, Gilsbach JM, Kreitschmann I. Is there a difference in cognitive deficits after aneurysmal subarachnoid haemorrhage and subarachnoid haemorrhage of unknown origin? Acta Neurochir (Wien) 1994; 127: 129–135 [DOI] [PubMed] [Google Scholar]
- 57. Torner JC, Kassell NF, Wallace RB, Adams HP, Jr. Preoperative prognostic factors for rebleeding and survival in aneurysm patients receiving antifibrinolytic therapy:report of the Cooperative Aneurysm Study. Neurosurgery 1981; 9: 506–513 [PubMed] [Google Scholar]
- 58. Berman MF, Solomon RA, Mayer SA, Johnston SC, Yung PP. Impact of hospital-related factors on outcome after treatment of cerebral aneurysms. Stroke 2003; 34: 2200–2207 [DOI] [PubMed] [Google Scholar]
- 59. Cross DT, III, Tirschwell DL, Clark MA, Tuden D, Derdeyn CP, Moran CJ, Dacey RG, Jr. Mortality rates after subarachnoid hemorrhage: variations according to hospital case volume in 18 states. J Neurosurg 2003; 99: 810–817 [DOI] [PubMed] [Google Scholar]
- 60. Frontera JA, Fernandez A, Claassen J, Schmidt M, Schumacher HC, Wartenberg K, Temes R, Parra A, Ostapkovich ND, Mayer SA. Hyperglycemia after SAH: predictors, associated complications, and impact on outcome. Stroke 2006; 37: 199–203 [DOI] [PubMed] [Google Scholar]
- 61. Winn HR, Almaani WS, Berga SL, Jane JA, Richardson AE. The long-term outcome in patients with multiple aneurysms. Incidence of late hemorrhage and implications for treatment of incidental aneurysms. J Neurosurg 1983; 59: 642–651 [DOI] [PubMed] [Google Scholar]
- 62. Yasui N, Nishimura H. Surgical treatment of unruptured intracranial aneurysms over the past 22 years. Neurol Med Chir (Tokyo) 2004; 44: 155–161; discussion 162–163 [DOI] [PubMed] [Google Scholar]
- 63. Tsutsumi K, Ueki K, Morita A, Kirino T. Risk of rupture from incidental cerebral aneurysms. J Neurosurg 2000; 93: 550–553 [DOI] [PubMed] [Google Scholar]
- 64. King JT, Jr, Berlin JA, Flamm ES. Morbidity and mortality from elective surgery for asymptomatic, unruptured, intracranial aneurysms: a meta-analysis. J Neurosurg 1994; 81: 837–842 [DOI] [PubMed] [Google Scholar]
- 65. Raaymakers TW, Rinkel GJ, Limburg M, Algra A. Mortality and morbidity of surgery for unruptured intracranial aneurysms: a meta-analysis. Stroke 1998; 29: 1531–1538 [DOI] [PubMed] [Google Scholar]
- 66. Tsutsumi K, Ueki K, Usui M, Kwak S, Kirino T. Risk of recurrent subarachnoid hemorrhage after complete obliteration of cerebral aneurysms. Stroke 1998; 29: 2511–2513 [DOI] [PubMed] [Google Scholar]
- 67. Tsutsumi K, Ueki K, Usui M, Kwak S, Kirino T. Risk of subarachnoid hemorrhage after surgical treatment of unruptured cerebral aneurysms. Stroke 1999; 30: 1181–1184 [DOI] [PubMed] [Google Scholar]
- 68. Horton JA. Sizing rings: a simple technique for measuring intracranial lesions. AJNR Am J Neuroradiol 1995; 16: 1449–1451 [PMC free article] [PubMed] [Google Scholar]