SUMMARY:
Rhinocerebral mucormycosis is a rare angioinvasive fungal infection that has a strong predilection for patients with poorly controlled diabetes and immunosuppression. Initial presenting symptoms are nonspecific and frequently are attributed to more mundane sinonasal and orbital pathologies. Early diagnosis and treatment are essential for survival and minimizing neurologic sequelae. CT and MR imaging are often used in the diagnostic work-up; however, CT findings are nonspecific.
Two cases of rhinocerebral mucormycosis highlight the MR imaging findings associated with devitalization of the sinonasal mucosa caused by mycotic vascular invasion. Recognition of these unusual findings may hasten the proper diagnosis and subsequent treatment of this rare but disfiguring and deadly disease. The timeliness of definitive surgical and medical treatment is directly related to the prevention of morbidity and mortality in affected patients.1
Case Reports
Case 1
A 66-year-old man with diabetes presented to the emergency department with malaise, left-eye proptosis, and left facial numbness and weakness of approximately 2 weeks’ duration. A noncontrast CT scan of the brain obtained at admission demonstrated soft-tissue secretions within the left maxillary sinus and ethmoid sinus, with some infiltration of the adjacent orbital fat and the inferior rectus muscle.2 He was placed on IV antibiotics, and an MR imaging of the brain was performed. This demonstrated left ethmoid and maxillary sinus opacification and focal lack of enhancement of the nasal turbinate mucosa and enhancement of the inferior rectus muscle (Fig 1). There was low signal intensity of the affected turbinate on T2 weighted images (Fig 2), with increased signal on DWI (Fig 3) and corresponding decreased signal on ADC images. The patient underwent a left middle meatal antrostomy with removal of tissue from the lateral nasal wall, and maxillary and ethmoid sinus debridement. Pathologic specimens demonstrated angioinvasive hyphae with characteristics of mucormycosis (Figs 4 and 5). The patient was placed on IV amphotericin, and a left orbital exenteration was then performed. He finished a 6 weeks’ course of amphotericin during a long hospital stay complicated by bacteremia and pneumonia. At the end of his course, he was ready for discharge and was to follow up with both the ophthalmology and ENT departments.
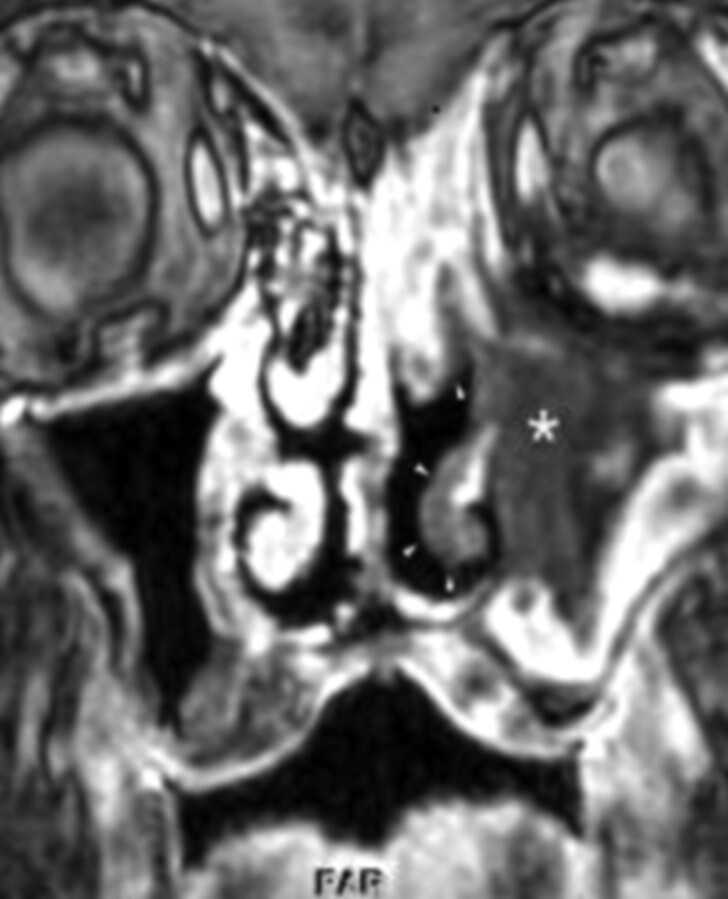
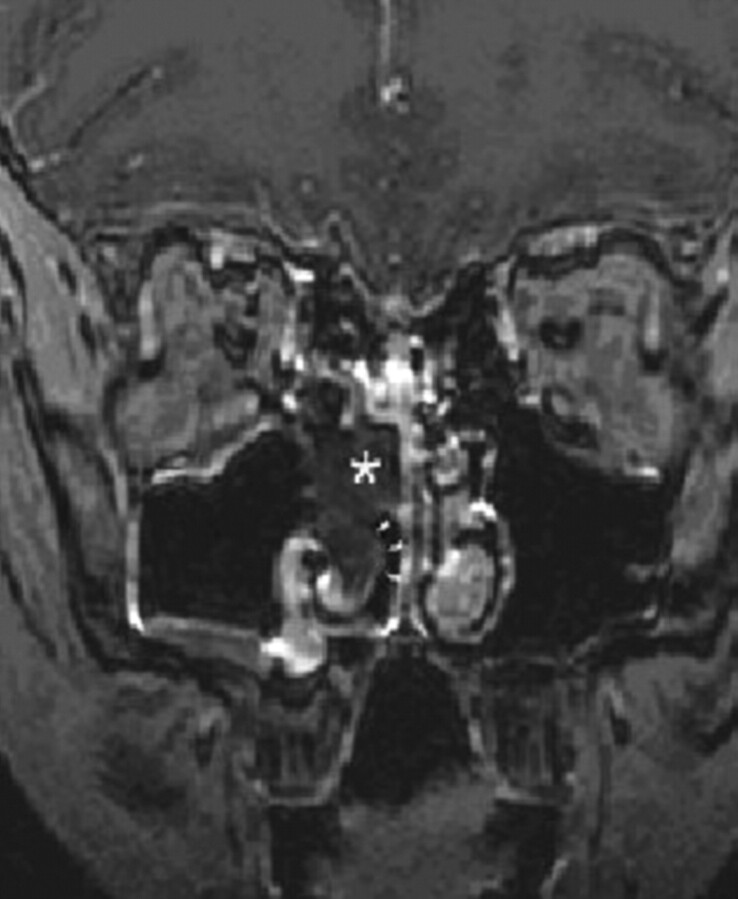
Fig 1.
Case 1: Postcontrast T1-weighted coronal MR image shows nonenhancing soft tissue, “black turbinate sign,” within the left maxillary sinus (asterisk). The mucosa of the inferior turbinate and a portion of the left middle turbinate demonstrate focal lack of the enhancement (arrowheads).
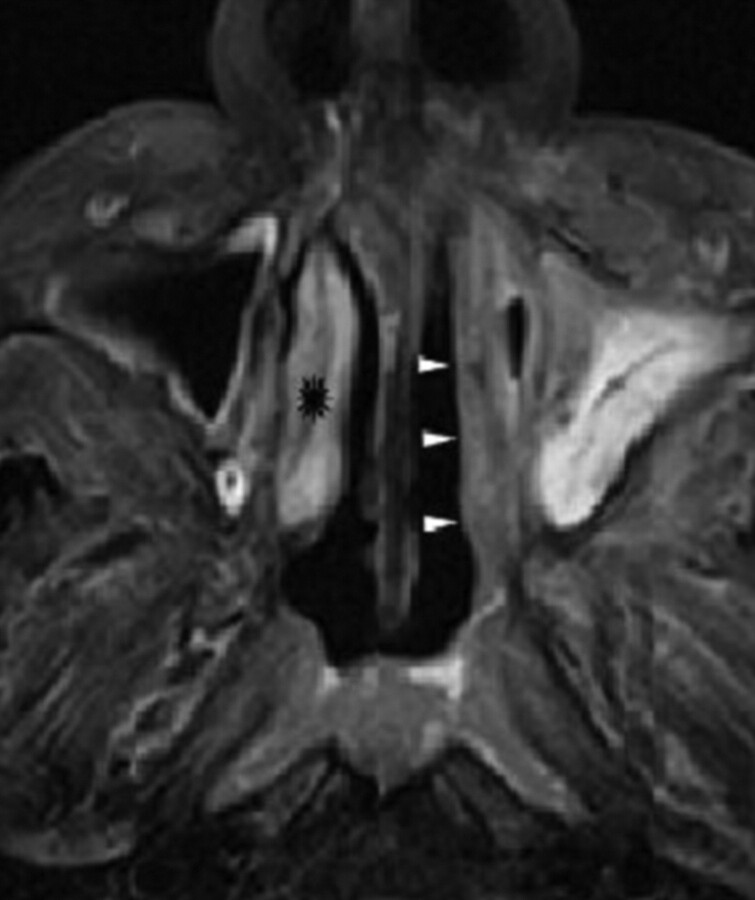
Fig 2.
Case 1: Axial T2-weighted sequence through the inferior turbinates shows low signal intensity along the left nasal turbinate (arrowheads) compared with the signal intensity on the right (starburst).
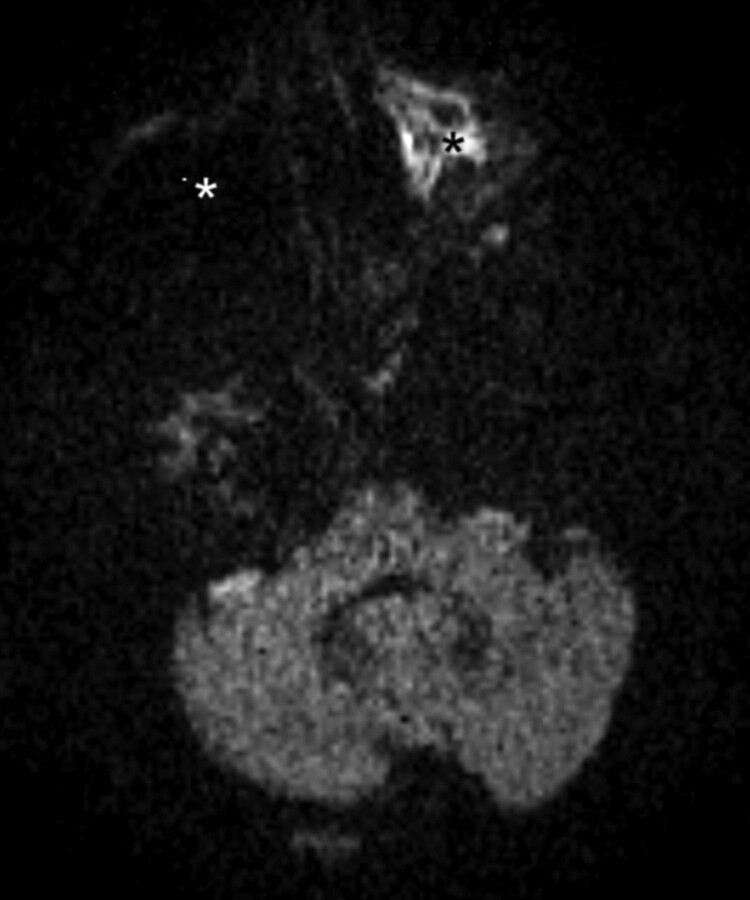
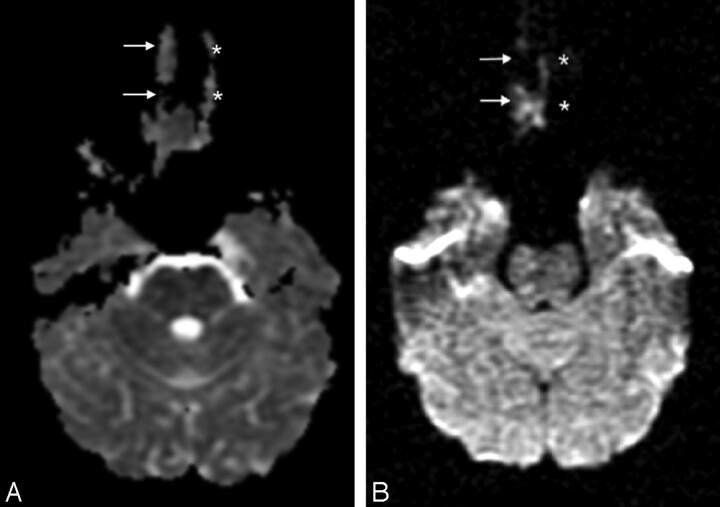
Fig 3.
Case 1: Axial DWI through the maxillary sinus level demonstrates high signal intensity within the affected left maxillary sinus (black asterisk) compared with the unaffected right maxillary sinus, which does not demonstrate any signal intensity (white asterisk). There is a corresponding reduction on the ADC sequence (not shown).
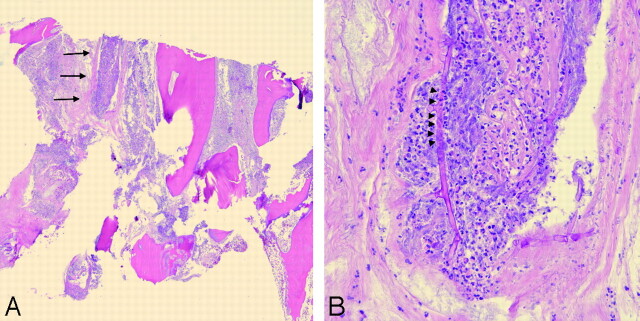
Fig 4.
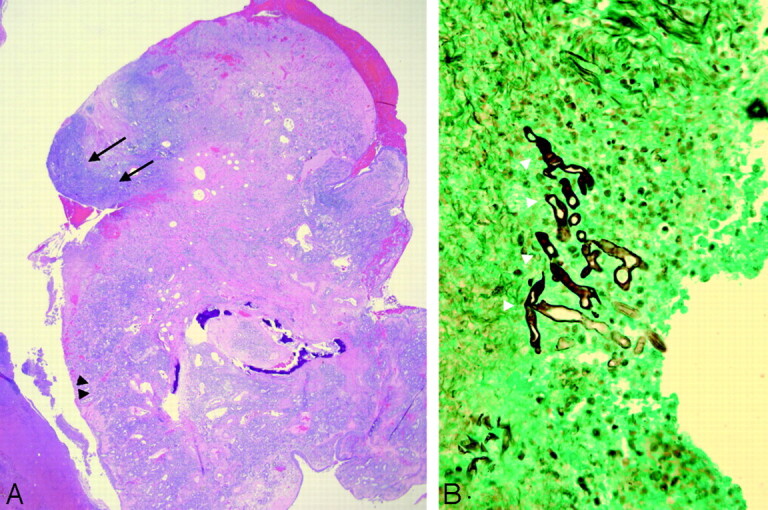
Case 1: A, Hematoxylin-eosin−stained section of the sinus mucosa of the same patient as in Fig 3 shows marked acute inflammation (black arrowheads), with adjacent areas of necrosis (black arrows) (original magnification ×20). B, Gomori methenamine silver stain shows fungal hyphae present in the mucosa. The hyphae (white arrowheads) are aseptate and broad, with irregular contours and wide-angled branching, features characteristic of mucormycosis (original magnification ×400).
Fig 5.
Case 1: A, Hematoxylin-eosin−stained section of the maxillary bone demonstrates necrosis, with marked acute inflammation and thrombosis of a blood vessel within the medullary space (black arrows) (original magnification ×20). B, On higher power, the blood vessel wall has been invaded by fungal hyphae (black arrowheads) (original magnification ×400).
Findings of nonenhancing tissue indicated devitalization that was consistent with surgical findings of extensive necrotic mucosal tissue.
Case 2
A 12-year-old girl with autoimmune hepatitis, on immunosuppressants, presented to the clinic with a 5-day history of right facial numbness, proptosis, and ear pain. An MR imaging examination of the brain was performed to assess the origin of her focal neurologic abnormalities. The MR images demonstrated focal lack of enhancement of the nasal and maxillary sinus mucosa (Fig 6), associated with mild increase in signal intensity on trace DWI images (Fig 7). Findings of images obtained through the cerebral tissues were unremarkable. Her symptoms progressed, and she developed progressive unilateral cranial neuropathies. Due to the overall clinical appearance of progressive cranial nerve palsy and nonviable tissue within the right middle and inferior turbinates, she underwent a right endoscopic middle and inferior turbinectomy with partial ethmoidectomy and nasal debridement in the ENT department. Biopsy specimens showed mucormycosis, after which IV amphotericin treatment was begun and an orbital exenteration was performed. She had an extended hospital stay, developing right cavernous sinus thrombosis and multiple right-sided cranial neuropathies during the course of her disease. The patient was discharged on day 83 with amphotericin infusions twice a day and dressing changes for her right eye exenteration and was to follow up with the neurosurgery department.
Fig 6.
Case 2: Coronal T1-weighted contrast-enhanced sequence demonstrates focal lack of enhancement of the right middle and inferior turbinates, “the black turbinate sign” (asterisk and arrowheads, respectively), in contrast to the unaffected normally enhancing left turbinates.
Fig 7.
Case 2: A and B, ADC (A) and DWI (B) images at the level of the middle turbinates demonstrate reduced signal intensity on ADC and corresponding increased signal intensity on DWI within the affected right turbinate (white arrows), indicating restricted diffusion; in comparison, the unaffected left turbinate did not show any signal intensity (white asterisk).
Discussion
Mucormycosis affects patients who are immunocompromised and is caused by fungi in the order Mucorales, including Mucor, Rhizopus, and Absidia species.2 The spores invade the nasal mucosa and are not phagocytized as in an immunocompetent individual which then germinate, forming angioinvasive hyphae that cause infarction of the involved tissue, resulting in a “dry” gangrene appearance. This devitalized mucosa appears on contrast-enhanced MR imaging as contiguous foci of nonenhancing tissue. Invasion occurs with spread to the maxillary sinuses and subsequent orbital spread through the ethmoid sinuses. Additionally, there are several routes for intracranial extension, including the ophthalmic arteries and cribriform plate into the frontal lobes, or through the cavernous sinus via the orbital apex.1–3 Extension of the disease leads to vascular thrombosis, including the cavernous sinus and other cerebral vessels due to fibrin reaction and Mucor thrombus formation. Subsequent infarctions lead to eschar formation or cerebral infarctions and, eventually in some cases, to coma or death.3
The morbidity and mortality rate of mucormycosis is high, and death can occur within as little as 2 weeks. Blindness and cranial nerve palsies are major sequelae of the disease because it is aggressively invasive.4 Thus, early detection and treatment are important factors in the resulting disposition of the patient with a substantial increase in mortality once the cranium has been penetrated. Patients treated with amphotericin B who undergo wide debridement have an overall higher survival rate.5 Diseased tissue is prone to necrosis and devitalization, which in turn leads to a lack of enhancement seen on MR imaging, “the black turbinate sign,” a feature that can aid in earlier detection of the disease.
Imaging characteristics of mucormycosis infection generally demonstrate a rim of soft-tissue thickness along the paranasal sinuses. Sinus opacification, air-fluid concentration, and obliteration of the nasopharyngeal tissue planes are features of sinonasal mucormycosis infection. On MR imaging, variable intensity within the sinuses on T1- and T2-weighted images is usually seen. Fungal elements themselves may cause a low signal intensity on T2 sequences.6 Furthermore, slightly decreased T2 signal intensity with rhinocerebral mucormycosis can be due to the involved mucosa itself (Fig 2). DWI sequences may aid in the diagnosis as demonstrated in Figs 3 and 7, showing an increased signal intensity of the affected sinus. The infarcted mucosa may lead to a restriction of diffusion. An article by Tung and Rogg7 reported that mycotic invasion and infarction of cerebral vessels could lead to cytotoxic edema and cause a restriction of diffusion. While the application to sinus mucosa is as yet unclear, the findings demonstrated in the above 2 cases may be examples of a parallel situation.
In general, the MR imaging findings of sinusitis usually demonstrate enhancement of the peripheral mucosa on T1-weighted contrast-enhanced sequences, in contrast to these 2 cases of documented sinonasal mucormycosis.8 Rhinocerebral mucormycosis should be a strong consideration when there is a lack of enhancement of the mucosa, given its angioinvasive nature, because the hyphae likely invade smaller vessels supplying the mucosa. A similar finding has been reported in an article by Horger et al,1 in which a case of rhinocerebral mucormycosis was described with areas of nonenhancement.
Of further interest concerning the case presentations of both patients are the presenting symptoms of unilateral cranial nerve involvement. The first patient had unilateral facial numbness of the affected left side while the second had right-sided facial numbness, ear pain, and proptosis. This constellation of findings is consistent with Garcin syndrome. A case report of Garcin syndrome was presented in a Japanese neurology journal in 2004. A 64-year-old patient with alcoholism and unilateral cranial nerve involvement was found to have rhinocerebral mucormycosis after presenting to the emergency department with right-sided proptosis, facial numbness, and periorbital edema.9 The disease is usually associated with infiltrating tumor; however, as in the case cited from 2004 and in the 2 case presentations discussed above, rhinocerebral mucormycosis should be considered in patients who are immunocompromised or have diabetes, presenting with multiple unilateral cranial nerve deficiencies.
Conclusions
Mucormycosis is a rare fungal disease that has a high morbidity and mortality rate. MR imaging plays an important role in aiding physicians in making a diagnosis for early treatment.10 Mucor organisms demonstrate aggressive characteristics regarding vascular and cranial nerve invasion and extension; thus, imaging and detailed descriptions of areas of involvement are key.11 In patients with predisposing factors and findings of sinus disease, mucormycosis should be a high consideration, especially in the presence of focal lack of enhancement and restricted diffusion, given the propensity of Mucor organisms for vascular invasion and thus necrosis and devitalized tissue. Furthermore, rhinocerebral mucormycosis should be considered in the appropriate patient presenting with symptoms of unilateral cranial nerve involvement suggesting Garcin syndrome. Early clinical presentations of rhinocerebral mucormycosis are often subtle and underappreciated.5 Awareness and recognition of radiologic features that may be more distinctive of mucormycosis sinusitis, such as those discussed here, can expedite management in this rapidly progressive disease.
Abbreviations
- ADC
apparent diffusion coefficient
- DWI
diffusion-weighted imaging
- ENT
ear, nose, and throat
- IV
intravenous
References
- 1. Horger M, Hebart H, Schimmel H, et al. Disseminated mucormycosis in haematological patients: CT and MRI findings with pathological correlation. Br J Radiol 2006; 79: 88–95 [DOI] [PubMed] [Google Scholar]
- 2. Hibbett DS, Binder M, Bischoff JF, et al. A higher-level phylogenetic classification of the fungi. Mycol Res 2007; 111 ( pt 5): 509–47. Epub 2007 Mar 13 [DOI] [PubMed] [Google Scholar]
- 3. Greenburg J. Rhinocerebral mucormycosis. Baylor College of Medicine. July 13, 2000. http://www.bcm.edu/oto/grand/07_13_00.htm. Accessed February 21, 2009 [Google Scholar]
- 4. Yen KG, Yen MG. Mucormycosis. Emedicine. http://search.medscape.com/emedicine-search?queryText=Mucormycosis. Accessed February 21, 2009
- 5. Spellberg B, Edwards J, Jr, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev 2005; 18: 556–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cure JK. Invasive fungal sinusitis. Amirsys. Statdx. http://www.amirsys.com/statdx/features.php. Accessed February 21, 2009
- 7. Tung G, Rogg JM. Diffusion-weighted imaging of cerebritis. AJNR Am J Neuroradiol 2003; 24: 1110–13 [PMC free article] [PubMed] [Google Scholar]
- 8. Cure JK, Michel MA. Acute rhinosinusitis. Amirsys. Statdx. http://www.amirsys.com/statdx/features.php. Accessed February 21, 2009
- 9. Mutsukura Y, Tsuboi Y, Imamura A, et al. Garcin syndrome in a patient with rhinocerebral mucormycosis [ in Japanese]. No To Shinkei 2004; 56: 231–35 [PubMed] [Google Scholar]
- 10. Mathur S, Karimi A, Mafee MF. Acute optic nerve infarction demonstrated by diffusion-weighted imaging in a case of rhinocerebral mucormycosis. AJNR Am J Neuroradiol 2007; 28: 489–90 [PMC free article] [PubMed] [Google Scholar]
- 11. Edelman RR, Hesselink JR, Zlatkin MB. Paranasal sinuses and nasal cavity. In: Edelman RR, Hesselink JR, Zlatkin MB. eds. Clinical Magnetic Resonance Imaging. Vol 4, 3rd ed. New York: WB Saunders; 2006 [Google Scholar]