Abstract
BACKGROUND AND PURPOSE:
Vertebroplasty and kyphoplasty are 2 minimally invasive spine augmentation procedures currently used in the management of vertebral compression fractures. Our aim was to examine the NIS data base to identify trends in spine augmentation procedures over time.
MATERIALS AND METHODS:
Patients were identified from the NIS data base by using primary diagnosis codes (ICD-9–pathologic vertebral fracture, 733.13) and procedures codes (ICD-9–other repair of bone, 78.49; vertebroplasty, 81.65; kyphoplasty, 81.66). Means and their corresponding standard errors were compared for statistically significant differences by using the Z-test.
RESULTS:
Between 2001 and 2008, >240 000 inpatient spine augmentations were performed in the United States. From 2001 to 2008, there was a 741% increase in the number of hospital discharges for patients who underwent a spine augmentation, but the year-to-year rate of increase has been declining since 2001. From 2004 to 2008, >50 000 inpatient verterbroplasties and >152 000 inpatient kyphoplasties were identified. Compared with vertebroplasty, kyphoplasty patients were less often admitted from the emergency department (33% versus 56%, P < .001), had shorter postaugmentation hospital stays (2.3 versus 3.1 days, P < .001), had fewer comorbidities at presentation (1.4 versus 1.6, P < .01), and were less likely to be discharged to a long-term facility (28% versus 43%, P < .001).
CONCLUSIONS:
Significant differences were noted in multiple comparisons between vertebroplasty and kyphoplasty, including length of hospital stay and discharges to long-term facilities. However, these findings may simply reflect differences in practice patterns rather than real differences in efficacy between the procedures.
Vertebral compression fractures occur in up to 19% of patients over the age of 50 and thus represent a substantial public health problem.1 Symptomatic vertebral compression fractures are a growing cause of disability and can cause acute and long-term pain as well as impair the activities of daily living and mobility.1 Vertebroplasty and kyphoplasty are 2 minimally invasive spine augmentation procedures currently used in the management of symptomatic vertebral compression fractures.2 Over the past 2 decades, these 2 procedures have become increasingly popular, especially for the treatment of vertebral compression fractures secondary to osteoporosis. The goal of this current study was to examine a large, unselected sampling of US clinical practice to identify trends in spine augmentation for patients with vertebral compression fractures between 2001 and 2008. To achieve this goal, we analyzed discharge data from the NIS data base, a public data base available in the United States containing discharge information from approximately 8 million hospital stays per year.
Materials and Methods
Data Base Characteristics
We reviewed data from the NIS from 2001 to 2008. The NIS data base is one of the Healthcare Cost and Utilization Projects sponsored by the Agency for Healthcare Research and Quality.3 The NIS is the largest all-payer inpatient care data base in the US that analyzes national trends in health care utilization, access, charges, quality, and outcomes based on data extracted from 7–8 million hospital stays representing approximately a 20% stratified sample of the US community hospitals.3 Community hospitals are defined as all nonfederal, short-term, general and other specialty hospitals, including academic medical centers. Short-term rehabilitation hospitals, long-term acute care hospitals, psychiatric hospitals, and chemical dependency treatment facilities are not included in the sample.
Five hospitals characteristics—geographic region, ownership, location (urban or rural), teaching status, and bed size—are used to create a stratified sample that is maximally representative of hospitalizations in the United States. For the years considered in our study, 1000–1056 hospitals from 33 to 42 states contributed discharges to the data base. Each year, hospitals within a stratum have an equal probability of selection for the sample, regardless of whether they appeared in a prior sample. Detailed information on the design of the NIS is available at http://www.hcup-us.ahrq.gov.
Patient Selection
We analyzed data collected from the NIS from 2001 to 2008 to determine trends in spine augmentation, specifically vertebroplasty and kyphoplasty. Before 2004, patients who underwent a spinal augmentation procedure were identified by using an ICD-9 code (ICD-9–pathologic vertebral fracture, 733.13) and then cross-referenced with the common identifying procedure code (ICD-9–other repair of bone, 78.49). In late 2004, new ICD-9 procedures codes were implemented, subdividing the previous procedure code into more specific codes for vertebroplasty (ICD-9, 81.65) and kyphoplasty (ICD-9, 81.66). To exclude patients who underwent spine augmentation for a vertebral compression fracture secondary to a malignancy, patients with a diagnosis of cancer (ICD-9, 1400–1991, 2000–2089) were excluded from our analysis.
Outcomes
For spine augmentations performed from 2001 to 2008, we analyzed variables including age, sex, race, hospital charges, length of hospital stay, admissions from the ED, and discharges to long-term facilities. In addition, the incidence of various complications associated with spine augmentations were examined by cross-referencing ICD-9 diagnosis codes with the patient data. Complication rates were obtained for pulmonary embolus (ICD-9, 415.11 and 415.19), postoperative surgical complications (ICD-9, 997.20–75, 998.00, 998.20, 998.59), postoperative neurologic complications (ICD-9, 997.00–997.09), and postoperative cardiovascular complications (ICD-9, 997.1).
For spine augmentations from 2004 to 2008, our analysis was adjusted to include information on the type of procedure performed, including vertebroplasty or kyphoplasty. In addition, the incidences of several comorbidities were examined by using ICD-9 diagnosis codes. Comorbidity incidence rates were obtained for obesity (ICD-9, 278.00–278.01), diabetes (ICD-9, 250.00–250.93), pulmonary disease (ICD-9, 491.10–519.90), hypertension (ICD-9, 401.00–405.99), peripheral vascular disease (ICD-9, 440.00–447.90), congestive heart failure (ICD-9, 428.00–428.90), chronic ischemic heart disease (ICD-9, 414.00–414.90), and valve disease (ICD-9, 394.00–397.90). Appropriate weights from the NIS data base were applied for national estimates. Means and their corresponding SEs were compared for statistically significant differences by using the Z-test (P < .05).
Results
Spine Augmentations from 2001 to 2008
Using the NIS data base, 247 278 spine augmentation discharges in total were identified between 2001 and 2008. During this 8-year period, there was an overall increase of >741% in the number of hospital discharges for patients who underwent a spine augmentation, from 6197 in 2001 to 52 119 in 2008 (Fig 1A). The demographic characteristics for spine augmentation patients are summarized in Table 1.
Fig 1.
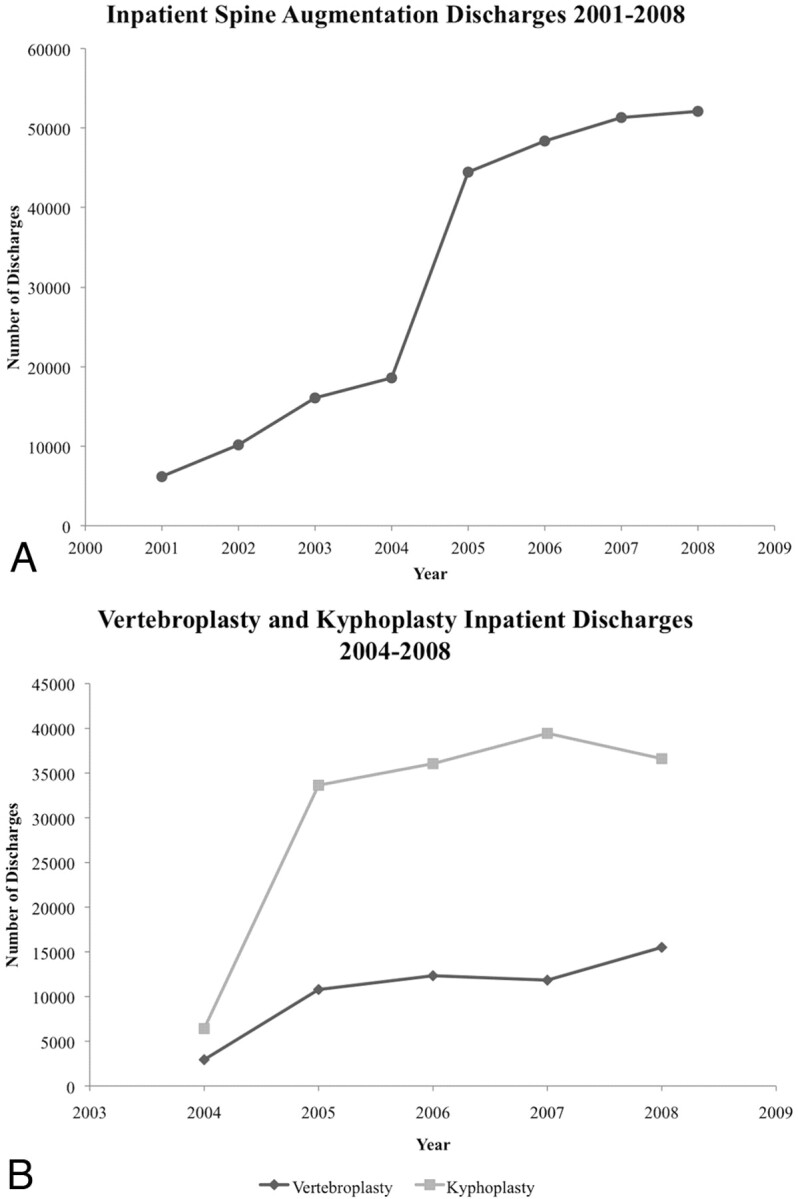
A, Graph shows trend over time for spine augmentation discharges. It demonstrates a steady increase (741%) in the number of discharges from 2001 to 2008 (P < .001). B, Graph shows trend over time for vertebroplasty and kyphoplasty discharges from 2004 to 2008. It demonstrates a 427% increase in vertebroplasty discharges and a 470% increase in kyphoplasty discharges over the 4-year period.
Table 1:
Summary of patient demographics and complications for inpatient spine augmentations performed from 2001 to 2008
| Spine Augmentations 2001–2008 | Patient Demographics and Complications | Total No. of Discharges | % |
|---|---|---|---|
| All discharges | 247 278 | 100.00 | |
| Sex | Male | 60 311 | 24.39 |
| Female | 186 967 | 75.61 | |
| Age (yr) | 18–44 | 3066 | 1.24 |
| 45–64 | 25 143 | 10.17 | |
| 65–84 | 155 674 | 62.96 | |
| ≥85 | 63 395 | 25.64 | |
| Complications | Pulmonary embolus | 841 | 0.34 |
| Cardiovascular | 1162 | 0.47 | |
| Postoperative surgical | 3264 | 1.32 | |
| Postoperative neurologic | 297 | 0.12 | |
| Mortality | Died | 1244 | 0.50 |
| Avg. age (yr) | 77.2 |
Vertebroplasty and Kyphoplasty Procedures from 2004 to 2008
From 2004 to 2008, 53 417 vertebroplasty discharges and 152 183 kyphoplasty discharges were identified (Table 2). During this 4-year period, vertebroplasty discharges increased by 427%, whereas kyphoplasty discharges increased by 470% (P < .01) (Fig 1B). The demographic characteristics for vertebroplasty and kyphoplasty patients for this time period are summarized in Table 3.
Table 2:
Comparison of inpatient spine augmentations performed from 2004 to 2008
| Inpatient Vertebroplasty | Inpatient Kyphoplasty | Comparison P Value | |
|---|---|---|---|
| No. of discharges, 2004–2008 | 53 417 | 152 183 | <.001 |
| Mean hospital stay, 2004–2008 | 6.4 | 4.4 | <.001 |
| Mean no. of days from admission to procedure, 2004–2008 | 3.3 | 2.1 | <.001 |
| Mean no. of days from procedure to discharge, 2004–2008 | 3.1 | 2.3 | <.001 |
| Mean hospital charges (US$) | 37 177 | 39 305 | <.001 |
Table 3:
Summary of patient demographics, comorbidities, and complications for vertebroplasty and kyphoplasty procedures performed from 2004 to 2008
| Patient Demographics, Comorbidities, and Complications | Total No. of Vertebroplasty Discharges | % | Total No. of Kyphoplasty Discharges | % | Comparison P Value | |
|---|---|---|---|---|---|---|
| All discharges | 53 417 | 100.00 | 152 183 | 100.00 | <.001 | |
| Sex | Male | 12 791 | 23.95 | 38 040 | 25.00 | <.001 |
| Female | 40 626 | 76.05 | 114 143 | 75.00 | <.001 | |
| Age (yr) | 18–44 | 691 | 1.29 | 1983 | 1.30 | .861 |
| 45–64 | 5182 | 9.70 | 16 277 | 10.70 | <.001 | |
| 65–84 | 30 870 | 57.79 | 96 792 | 63.60 | <.001 | |
| 85+ | 16 674 | 31.21 | 37 131 | 24.40 | <.001 | |
| Complications | Pulmonary embolus | 308 | 0.58 | 410 | 0.27 | <.001 |
| Cardiovascular | 195 | 0.37 | 763 | 0.50 | <.001 | |
| Post-op surgical | 696 | 1.30 | 1958 | 1.29 | .821 | |
| Post-op neurologic | 64 | 0.12 | 188 | 0.12 | .831 | |
| Comorbidities | Obesity | 1955 | 3.66 | 4928 | 3.24 | <.001 |
| Diabetes | 10 219 | 19.13 | 28 124 | 18.48 | <.01 | |
| Pulmonary disease | 16 789 | 31.43 | 43 654 | 28.69 | <.001 | |
| Peripheral vascular disease | 3735 | 6.99 | 8710 | 5.72 | <.001 | |
| Hypertension | 31 633 | 59.22 | 89 445 | 58.77 | <.074 | |
| Congestive heart failure | 7805 | 14.61 | 16 871 | 11.09 | <.001 | |
| Chronic ischemic heart disease | 11 209 | 20.98 | 30 803 | 20.24 | <.001 | |
| Valve disease | 1041 | 1.95 | 2346 | 1.54 | <.001 | |
| Mortality | Died | 384 | 0.72 | 618 | 0.41 | <.001 |
| Avg. age (yr) | 78.2 | 76.9 | <.001 |
The number of patients who underwent kyphoplasty outnumbered those patients who underwent vertebroplasty by a factor of 2.85 (Tables 2 and 3). For both vertebroplasty and kyphoplasty, approximately 75% of the patients were female and approximately 90% of the patients were white. The average kyphoplasty patient was 76.9 years old, whereas the average vertebroplasty patient was slightly older at 78.2 years (P < .001).
Vertebroplasty and Kyphoplasty 2004–2008: Hospital Characteristics and Outcomes
Approximately one-half of patients who underwent inpatient vertebroplasty and one-third of patients who underwent inpatient kyphoplasty were admitted from the ED (P < .001). In addition, the total hospital stay for vertebroplasty patients was, on average, 2 days longer than kyphoplasty patients, with vertebroplasty patients staying an average of 6.4 days compared with 4.4 days for kyphoplasty patients (P < .001). The postaugmentation duration of stay was also statistically longer for vertebroplasty patients, with vertebroplasty patients staying an average of 3.1 days compared with 2.3 days for kyphoplasty patients (P < .001; Table 2).
A review of the clinical comorbidities for both vertebroplasty and kyphoplasty is presented and summarized in Table 3. Both kyphoplasty and vertebroplasty patients had a similar incidence of hypertension at approximately 59% (P = .074). Besides hypertension, vertebroplasty patients had a statistically higher incidence of obesity (3.66% versus 3.24%, P < .001), diabetes (19.13% versus 18.48%, P < .01), pulmonary disease (31.43% versus 28.69%, P < .001), peripheral vascular disease (6.99% versus 5.72%, P < .001), congestive heart failure (14.61% versus 11.09%, P < .001), chronic ischemic heart disease (20.98% versus 20.24%, P < .001), and valve disease (1.95% versus 1.54%, P < .001) compared with kyphoplasty patients. In 2004, the average vertebroplasty patient presented with 1.6 of the 8 comorbidities that were analyzed and this remained steady through 2008. In contrast, the incidence of presenting comorbidities in kyphoplasty patients has risen from an average of 1.3 comorbidities in 2004 to 1.5 comorbidities in 2008.
The rates for several operative/postoperative complications were analyzed for both procedures and are summarized in Table 3. Both vertebroplasty and kyphoplasty had similar rates of 1.30% and 1.29% for postoperative surgical complications (P = .821) and an identical rate of 0.12% for postoperative neurologic complications (P = .831). The rate of pulmonary embolus was statistically higher at 0.58% for vertebroplasty compared with 0.27% for kyphoplasty (P < .001). In contrast, the rate of postoperative cardiovascular complications was statistically higher at 0.50% for kyphoplasty compared with 0.37% for vertebroplasty (P < .001). The mortality rate for both procedures remained fairly low with vertebroplasty having a statistically higher rate at 0.7% and kyphoplasty having a mortality rate of 0.4% (P < .001).
Discharge Disposition and Cost
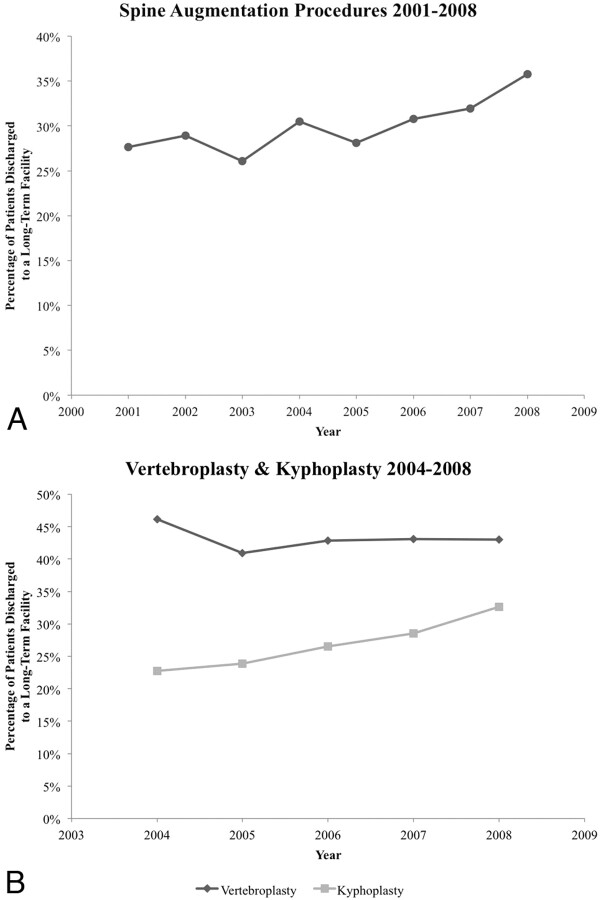
The discharge disposition for all spine augmentations from 2001 to 2008 has shown a statistically significant increase in discharges to long-term facilities over time, with 36% of patients being discharged to long-term facilities in 2008 compared with 27% in 2001 (P < .02) (Fig 2A). Kyphoplasty procedures showed a statistically significant increase in discharges to long-term facilities (P < .02), whereas vertebroplasty did not (Fig 2B). The discharge disposition for vertebroplasty has maintained relatively constant since 2006 at approximately 43% to long-term facilities (Fig 2B).
Fig 2.
A, Graph shows trend over time for discharges to long-term facilities for spine augmentations from 2001 to 2008. It demonstrates a steady increase in discharges to long-term facilities from 2003 to 2008 (P < .02). B, Graph shows trend over time for discharges to long-term facilities for vertebroplasty and kyphoplasty from 2004 to 2008. It demonstrates the increase in discharges to long-term facilities for kyphoplasty procedures (P < .02) and the relatively constant level of discharges to long-term facilities for vertebroplasty.
Mean hospital charges for all spine augmentations since 2001 were US$36 923. The mean hospital charges for vertebroplasty from 2004 to 2008 averaged US$37 177, whereas charges for kyphoplasty averaged US$39 305 (P < .001; Table 2).
Discussion
This current analysis of the NIS demonstrates a marked increase in the number of inpatient spine augmentations performed over time. However, the rate of increase has diminished in recent years. Surprisingly, the proportion of patients discharged to long-term facilities has increased over time, which may represent changes in practice patterns to include patients with greater comorbidities.
Numerous, significant differences between vertebroplasty and kyphoplasty were found in our analysis, including the proportion of patients admitted from the ED, the length of hospital stay, the number of presenting comorbidities, the proportion of patients discharged to long-term facilities, and the overall number of procedures performed. However, these differences may simply reflect differences in practice patterns rather than essential differences in the procedure.
It has been suggested that as vertebral augmentation has developed over the past 10 years, greater experience has been gained with the procedure, especially the older vertebroplasty procedure, and thus practitioners have become more willing to perform treatment on severely ill patients. Compared with kyphoplasty patients, vertebroplasty patients had a statistically higher number of presenting comorbidities; however, this difference has steadily decreased over the past 4 years with kyphoplasty being used increasingly on patients with a higher number of comorbidities. Thus, it may be the case that though vertebroplasty was initially used to treat sicker patients, due to more experience with the procedure, it is less so the case today.
It is of particular interest that the increase in presenting comorbidities observed in kyphoplasty patients from 2004 to 2008 seems to mirror a similar increase in the percentage of kyphoplasty patients discharged to a long-term facility. Similarly, presenting comorbidities in vertebroplasty patients have remained steady from 2004 to 2008, mirroring the relatively constant percentage of vertebroplasty patients discharged to long-term facilities. These results seem to suggest that the increasing percentage of kyphoplasty patients being discharged to long-term facilities may be, at least in part, due to the increasing number of comorbidities in patients undergoing treatment.
It has been reported previously that kyphoplasty costs anywhere between 2 and 20 times more than vertebroplasty.4,5 Our results continue to support this and showed that total hospital charges were higher in kyphoplasty patients than in vertebroplasty patients. It is interesting, however, that total charges were higher for kyphoplasty patients despite the fact that vertebroplasty patients had longer hospital stays and had a higher number of comorbidities. Thus, it may be that the cost of kyphoplasty is substantially higher than the observed difference of US$250 and the higher number of comorbidities and longer hospital stays observed in the vertebroplasty group reduced the cost difference between the 2 procedures.
Practitioners have previously been encouraged to admit outpatients after kyphoplasty procedures to the hospital, whereas outpatients treated with vertebroplasty usually have been discharged directly after recovery, without hospital admission. Because only inpatients are included in the NIS data base, these practice patterns would have resulted in relatively shorter lengths of stay for the kyphoplasty cohort, because many of these patients would have been admitted solely for the kyphoplasty procedure. Furthermore, it is not surprising that a smaller proportion of kyphoplasty patients than vertebroplasty patients were discharged to long-term facilities, because many of these kyphoplasty patients may have been admitted solely for the augmentation procedure.
The fact that a significantly greater proportion of vertebroplasty patients had been admitted from the ED supports our conjecture regarding the influence of practice patterns on observed outcomes, because these patients admitted from the ED probably were admitted for pain control and not simply for postaugmentation care.
The rapid rise of spine augmentations over the past 2 decades has been established by several studies. Lad et al demonstrated a substantial increase (12 900%) in the number of spine augmentations performed from 1993 to 2004, and a recent study that examined aggregate fee-for-service data from US Medicare enrollees from 2001 to 2005 showed that the number of vertebroplasties performed during this time period almost doubled.6,7 Our study confirmed these results and showed that there continues to be a steady but gradually plateauing rise in the number of spine augmentations performed each year through 2008.
The limitations of the data used in the present study must be acknowledged. The NIS data base lacks disease severity scales as well as specific procedural information. Thus, information such as the severity of vertebral fractures and the number of vertebral levels treated during each spine augmentation procedure was not available for analysis. In addition, the NIS data base does not include detailed procedure-related cost information and only reports total hospital charges. Unfortunately, this makes specific cost analysis and comparison between procedures difficult due to the numerous factors that can influence cost such as type of anesthesia administered, procedure room charges, equipment costs, and postop/recovery charges. Another limitation is that the outcomes available for analyses in this study (discharge disposition, length of stay, and hospitalization costs) are not necessarily related directly to functional outcomes, they also could be influenced by factors such as payer status and social factors.
The accuracy of the NIS data base is also largely dependent on the selection of the appropriate diagnosis codes and the proper sequencing of the codes.8 The differences between kyphoplasty and vertebroplasty procedures demonstrated in this study also may reflect a coding artifact. For example, the large increase in the number of spine augmentations seen in 2005 may be due to the implementation and rapid adoption of new ICD-9 codes for vertebroplasty and kyphoplasty in late 2004. We also acknowledge that our results may reflect practice predisposition artifacts such as the recent claims of Medicare fraud that allege that numerous hospitals unnecessarily performed kyphoplasty on an inpatient basis to increase Medicare billings.9,10
Conclusions
Kyphoplasty and vertebroplasty are 2 spine augmentation procedures that have gained widespread acceptance in clinical practice over the past 2 decades.11–13 Using the NIS data base, this current study showed that the frequency of all spine augmentations increased >740% between 2001 and 2008, but the year-to-year rate increases are beginning to plateau. In addition, the incidence of both vertebroplasty and kyphoplasty increased >400% from 2004 to 2008. Most patients undergoing both vertebroplasty and kyphoplasty were women (76% and 75%, respectively). Also of note, compared with vertebroplasty, kyphoplasty patients had shorter postaugmentation hospital stays (2.3 versus 3.1 days, P < .001), were less often admitted from the ED (33% versus 56%, P < .001), had fewer comorbidities at presentation (1.4 versus 1.6, P < .01), and were less likely to be discharged to a long-term facility (28% versus 43%, P < .001). These results seem to indicate that the number of elective cases and the referral patterns for each procedure differ substantially.
Abbreviations
- ED
emergency department
- ICD-9
International Classification of Diseases, Ninth Revision
- NIS
National Inpatient Sample
Footnotes
Disclosures: Harry Cloft, Consultant: Medtronic/Kyphon, Details: Serve on Data Safety Monitoring Board for KAVIAR study.
References
- 1. Melton LJ, 3rd, Kallmes DF. Epidemiology of vertebral fractures: implications for vertebral augmentation. Acad Radiol 2006;13:538–45 [DOI] [PubMed] [Google Scholar]
- 2. Garfin SR, Yuan HA, Reiley MA. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine (Phila Pa 1976) 2001;26:1511–15 [DOI] [PubMed] [Google Scholar]
- 3. AHRQ. HCUP Nationwide Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). Rockville, MD; 2001–2008 [Google Scholar]
- 4. Mathis JM, Ortiz AO, Zoarski GH. Vertebroplasty versus kyphoplasty: a comparison and contrast. AJNR Am J Neuroradiol 2004;25:840–45 [PMC free article] [PubMed] [Google Scholar]
- 5. Gray DT, Hollingworth W, Onwudiwe N, et al. Costs and state-specific rates of thoracic and lumbar vertebroplasty, 2001–2005. Spine (Phila Pa 1976) 2008;33:1905–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lad SP, Patil CG, Lad EM, et al. National trends in vertebral augmentation procedures for the treatment of vertebral compression fractures. Surg Neurol 2009;71:580–84; discussion 584–85 [DOI] [PubMed] [Google Scholar]
- 7. Gray DT, Hollingworth W, Onwudiwe N, et al. Thoracic and lumbar vertebroplasties performed in US Medicare enrollees, 2001–2005. JAMA 2007;298:1760–62 [DOI] [PubMed] [Google Scholar]
- 8. Berthelsen CL. Evaluation of coding data quality of the HCUP National Inpatient Sample. Top Health Inf Manage 2000;21:10–23 [PubMed] [Google Scholar]
- 9. Blesch G. Kyphoplasty cacophony. Six more hospitals settle false claims allegations. Mod Healthc 2009;39:10. [PubMed] [Google Scholar]
- 10. Werling K, Carnell H, McCormick D. Nine hospitals to pay $9.4M for false claims allegations involving kyphoplasty. Health Care Law Mon 2010;2010:8–9 [Google Scholar]
- 11. Alvarez L, Alcaraz M, Perez-Higueras A, et al. Percutaneous vertebroplasty: functional improvement in patients with osteoporotic compression fractures. Spine (Phila Pa 1976) 2006;31:1113–18 [DOI] [PubMed] [Google Scholar]
- 12. Diamond TH, Bryant C, Browne L, et al. Clinical outcomes after acute osteoporotic vertebral fractures: a 2-year non-randomised trial comparing percutaneous vertebroplasty with conservative therapy. Med J Aust 2006;184:113–17 [DOI] [PubMed] [Google Scholar]
- 13. Yan D, Duan L, Li J, et al. Comparative study of percutaneous vertebroplasty and kyphoplasty in the treatment of osteoporotic vertebral compression fractures. Arch Orthop Trauma Surg 2010 [DOI] [PubMed] [Google Scholar]