These authors attempted to determine the time between identification of a critical finding and verbal communication with the primary caregiver. Ninety-one critical findings identified by trainees and attending physicians were analyzed. The mean time from study acquisition to critical finding discovery was 62 minutes and from then to a telephone call was 3.7 minutes (direct caregiver communication within 15 minutes for 94% of cases). During night or weekend shifts, mean notification times increased and sources of delay were inaccurate contact information, physician unavailability (shift change/office closed), patient transfer to a different service, or lack of responsiveness from caregivers.
Abstract
BACKGROUND AND PURPOSE:
Timely reporting of critical findings in radiology has been identified by The Joint Commission as one of the National Patient Safety Goals. Our aim was to determine the magnitude of delays between identifying a neuroradiologic critical finding and verbally notifying the caregiver in an effort to improve clinical outcomes.
MATERIALS AND METHODS:
We surveyed the time of critical finding discovery, attempted notification, and direct communication between neuroradiologists and caregivers for weekday, evening, overnight, and weekend shifts during an 8-week period. The data were collected by trained observers and/or trainees and included 13 neuroradiology attendings plus fellows and residents. Critical findings were based on a previously approved 17-item list. Summary and comparative t test statistics were calculated, and sources of delays were identified.
RESULTS:
Ninety-one critical findings were recorded. The mean time from study acquisition to critical finding discovery was 62.2 minutes, from critical finding discovery to call made 3.7 minutes, and from call made to direct communication, 5.2 minutes. The overall time from critical finding discovery to caregiver notification was within 10 minutes in 72.5% (66/91) and 15 minutes in 93.4% (85/91) of cases. There were no significant differences across shifts except for daytime versus overnight and weekend shifts, when means were 2.4, 5.6, and 8.7 minutes, respectively (P < .01). If >1 physician was called, the mean notification time increased from 3.5 to 10.1 minutes (P < .01). Sources of delays included inaccurate contact information, physician unavailability (shift change/office closed), patient transfer to a different service, or lack of responsiveness from caregivers.
CONCLUSIONS:
Direct communication with the responsible referring physician occurred consistently within 10–15 minutes after observation of a critical finding. These delays are less than the average interval from study acquisition to critical finding discovery (mean, 62.2 minutes).
The eradication of preventable medical errors is of paramount importance in the field of health care. In July 2011, The Joint Commission (TJC) released a National Patient Safety Goal that mandated that healthcare providers “report critical results of tests and diagnostic procedures on a timely basis.”1 There have subsequently been protocols created to reach this goal, including those for the following: 1) defining a critical finding (CF), 2) communicating the critical finding to the physician, and 3) indicating what makes a report “timely.”2–6
TJC has never defined a CF, stating only “each organization can define for itself the circumstances under which a test result is considered ‘critical.’”1 The American College of Radiology identifies findings that require nonroutine communication as those “that suggest a need for immediate or urgent intervention.”2 Likewise, TJC has never defined what “timely” means. Once again it has suggested that institutions define for themselves what is timely for a given laboratory or imaging finding. However TJC demands that institutions monitor compliance with the communication of CFs (Appendix).
At our institution, we have created, in neuroradiology, a list of critical findings that neuroradiology, neurosurgery, neurology, and otorhinolaryngology departments have agreed is acceptable to all services. It has been reviewed at 5-year intervals. As to CF notification times, the only mandate has come from our Brain Attack team for being a Stroke Center of Excellence, which requires 20 minute Team turnaround times for reports after scans. There have been no guidelines set for other CFs.
Recent studies involving the determination and communication of critical findings in neuroradiology have analyzed such compliance with the National Patient Safety Goals of the TJC by conducting surveys of academic radiology departments for the presence of a critical finding list and the method of disseminating and implementing the information.3,7 Another publication studied the existing list of critical findings in neuroradiology and revised that list to include frequent findings that were not previously identified in an effort to be more inclusive of lesions that warrant immediate communication.4 Others have suggested that careful review of performance on an ongoing basis with regard to communication of radiologic critical findings can result in significant improvement in adherence to institutional guidelines.5
Because TJC has been ambiguous about what constitutes appropriate timing for communicating CFs in radiology and no one has established baseline data with which to assess interval improvements, we sought to address this knowledge gap. The purpose of this study was to assess the extent of delays occurring between identification of a critical finding and communication to the referring physician. We focused only on this communication process (rather than delays from study ordered to study completion) to address TJC concerns about physician-physician communication delays. A broad interpretation of the mandate of TJC might suggest that radiologists must record when they see a CF, when they attempt to notify a caregiver, and when they actually communicate with the caregiver about that CF, as part of the monitoring function for critical results. For that reason, we investigated each of these intervals to assess their magnitude. We hypothesized that the time between the discovery of a critical finding and the attempt to contact the referring physician would be short and consistent across all timeframes of daily practice. However, the time between attempted notification of the referring physician and communication with the clinician would vary widely depending on the time of day the CF was discovered, the service being notified, and weekday or weekend shift. We also sought to determine the nature of such communication delays. This is the first step in improving patient care. By identifying sources of delays, addressing the sources of these delays, remediating them, and then reassessing notification times after corrections are made, we believe that patient care can be enhanced. Patients with critical health care needs can be treated earlier; hopefully, this change will positively impact outcomes.
Materials and Methods
This study of critical findings notification timing was reviewed and approved by our institutional review board. Due to the quality assurance nature of the study, informed consent by patients and providers was not required and the study was Health Insurance Portability and Accountability–compliant.
The time of completion of the critical finding discovery, the time of attempted notification of the referring physician, and the time of direct communication between the radiologist and referring physician were recorded for 4 different time periods (“shifts”) in the division of neuroradiology between June 15 and August 16, 2013. The time periods were defined as the following: weekday (8 am to 4 pm); weekday evening (4 pm to 11 pm), weekday overnight (11 pm to 8 am), and weekend (8 am to 4 pm). One of 2 trained volunteer observers independently recorded these times sitting in the radiology reading room for all critical findings during the weekday, weekday evening, and weekend periods for 20 days of the 8 weeks. These 20 days were randomly selected on the basis of the availability of the volunteers who were participating in research activities elsewhere in the institution on the other days. The volunteer observers were trained to record the times by using the stop watch function of their cell phones on 2 separate days, with verification that the methodology was accurate by the senior author (D.M.Y.). Because of the off-hours and the infrequent occurrences of neuroradiology CFs, instead of these volunteers, the neuroradiology on-call fellow and/or resident recorded the times in the same exact manner during the weekday (11 pm to 8 am) and weekend overnight shifts (4 pm to 8 am) for 4 weeks of nights. The same methodology was used. The trained observers sat in the central neuroradiology reading area, and as a reader identified a CF, that reader notified the observer and the trained observer recorded the time the CF was identified, the time a call was made to contact a referrer, and the time the referring physician responded and was told the finding. The same process was used for on-call trainees for overnight shifts, who recorded the same data points and provided the data to the trained observer the next day in the morning. The participants all were aware that the data were being collected to assess delays in notification times.
Although the first attempted call was to the responsible licensed caregiver “of record” who ordered the imaging test, we, as a policy, allow “substituted” caregivers of record, which include physicians, nurse practitioners, and physician assistants associated with the caregiver of record in our institution for a “completed” communication. All of these health care providers can write orders to address critical findings in our institution (thus secretaries or floor nurses or clerks are not legitimate substitutions for CF notifications). This directive was used for this project. Trainees are instructed at our institution to make CF calls on their own, before a faculty attending has finalized the reading, unless the trainee is unsure of the finding, at which time the trainee reviews the case with the attending beforehand. Only radiologists (trainees and attendings) made calls to clinicians. There were no surrogates. The study included all patients evaluated in our institution, including inpatients, emergency department (ED) patients, research patients, and outpatients who had CFs. All data were anonymized with respect to trainees and patients.
To put these times in perspective, the radiology information system was queried for all CF cases identified to determine the time the study was ordered and the time the study was completed. These data were not the focus of the study (which evaluated the notification cycle) but were used to provide background for the magnitude of time intervals.
An approved list of these critical findings is found in Table 1.4
Table 1:
Approved list of neuroradiologic critical findings4
| Findings |
|---|
|
Reprinted from the Journal of the American College of Radiology, Volume 10/Issue 1, Stacey A. Trotter, Lukasz S. Babiarz, Valentina G. Viertel, Paul Nagy, Jonathan S. Lewin, David M. Yousem, Determination and Communication of Critical Findings in Neuroradiology, pages 45–50, 2013, with permission from Elsevier.
The mean, median, and mode for the following time intervals were calculated for each of the 4 shifts: 1) elapsed time between the completion of the radiologic study and identification of a critical finding, 2) elapsed time between identification of a critical finding and attempted notification of referring physician, 3) elapsed time between attempted notification and direct communication with the referring physician, and 4) the total elapsed communication time from critical finding discovery to direct communication with the referring physician.
Paired t tests were performed between each of the 4 work shifts, looking at the time intervals of the following: 1) the time the study was completed to the time of notification of the referring physician; 2) the time the study was completed to the time the CF was identified by the neuroradiologist; 3) the time the CF was identified to the time of an attempt to reach the referring physician; 4) the time between an attempt to reach the referring physician; and 5) the actual time of communication between the radiologist and referring physician, and the time the CF was identified to the time the referring physician was notified. Paired t tests were also evaluated in the same manner for the services that had ≥9 CFs (Internal Medicine, Emergency Department, Neurosurgery, and Intensive Care Unit).
Results
There were 6566 neuroradiologic studies performed between June 15 and August 16, 2013. Ninety-one neuroradiology critical findings were recorded during the 8-week period (Table 2). Thirty-seven critical findings were recorded during the weekday shifts, 24 critical findings were recorded during the weekday evening (4–11 pm) shifts, 24 critical findings were identified during the overnight shifts (11 pm to 8 am), and 6 were recorded during the weekend shifts. Thirty-one of the 91 critical findings resulted from emergency department cases, 18 resulted from neurosurgery cases, 10 resulted from internal medicine cases, 9 resulted from neurology cases, and 9, from intensive care unit cases. These data are listed in Table 3. Seventy-two and one-half percent (66/91) of the critical findings were directly communicated by the radiologist to 1 health care professional, 20.9% (19/91) required calls to 2 health care professionals, and 3.3% (3/91) required calls to 3 health care professionals. Data were incomplete in 3 cases. The missing data were the times from CF discovered to the call made in all 3 cases.
Table 2:
Total time from CF discovery to referring physician notified by shift
| Shift | Total No. of CFs | Time from CF Discovery to Call Made to Physician (Notification Time) (min) | Time from CF Discovery to Referring Physician Notified (Total Communication Time) (min) | Time from Study Completed to CF Identified (min) |
|---|---|---|---|---|
| 8 am to 4 pm (weekday) | 37 | |||
| Mean/SD | 2.4/2.8 | 7.4/3.9 | 94.7/87.4 | |
| Mode | 0 | 10 | 81 | |
| Median | 1 | 7 | 72 | |
| 4 pm to 11 pm (night) | 24 | |||
| Mean/SD | 2.5/2.9 | 7.8/6.9 | 49.8/45.7 | |
| Mode | 0 | 5 | 11 | |
| Median | 2 | 5 | 44 | |
| 11 pm to 8 am (overnight) | 24 | |||
| Mean/SD | 5.6/3.6 | 10.1/7.6 | 31.6/37.8 | |
| Mode | 3 | 15 | 9 | |
| Median | 5 | 9 | 18 | |
| 8 am to 4 pm (weekend) | 6 | |||
| Mean/SD | 8.7/9.0 | 16.8/13.1 | 33.5/23.9 | |
| Mode | 3 | None | None | |
| Median | 4.5 | 11.5 | 22 | |
| All shifts | 91 | |||
| Mean/SD | 3.7/4.1 | 8.8/6.9 | 62.2/69.0 | |
| Mode | 0 | 5 | 16 | |
| Median | 3 | 8 | 43 |
Table 3:
Elapsed times for top 5 services
| Service | Total No. of CFs | Mean Response Time (min) | Range (min) | SD | Mode (min) | Median (min) | Mean Notific. Time (min) | SD | Mean Total Comm. Time (min) | SD |
|---|---|---|---|---|---|---|---|---|---|---|
| Emergency | 31 | 3.4 | 21 | 4.3 | 1 | 2 | 5.3 | 7.9 | 8.7 | 8.5 |
| Neurosurgery | 18 | 6.5 | 33 | 7.7 | 5 | 5 | 2.7 | 3.3 | 9.2 | 8.1 |
| Medicine | 10 | 5.6 | 13 | 4.7 | 1 | 4.5 | 2.8 | 3.7 | 8.4 | 4.9 |
| Neurology | 9 | 7.2 | 23 | 7.8 | 2 | 5 | 3 | 2.1 | 10.2 | 8.7 |
| Intensive care | 9 | 2.8 | 7 | 2.4 | 2 | 3 | 4.7 | 3.3 | 7.4 | 4.3 |
Note:—Notific indicates Notification; Comm., communication.
Although the denominator of the total number of cases read during the various shifts on the 20 data-collection days was not recorded, the mean percentage of cases read by neuroradiologists that were deemed critical was 9.0% (7591/84,348) for the calendar year 2013. Assuming this was consistent during the data-collection period, it would suggest that 1011 studies were reviewed during the study period.
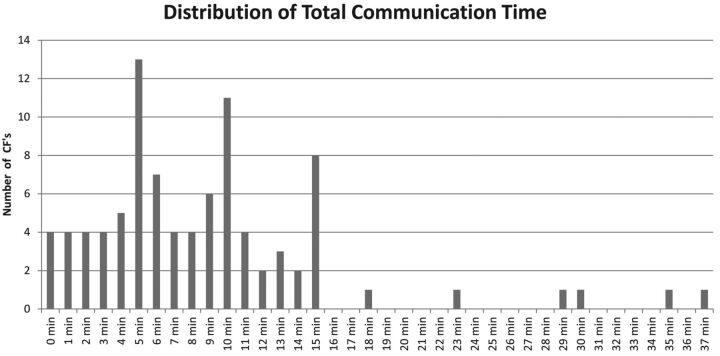
The mean time from the completion of the neuroradiologic study by the technologist to the CF discovery by the radiologist was 62.2 ± 69 minutes (median, 43 minutes; mode, 16 minutes) (Table 2). The time from CF discovery to attempted call (“attempted notification time”) was a mean of 3.7 ± 4.1 minutes (Table 2). The mean time from call/page made to actual communication with the requesting physician (“response time”) was 5.2 minutes. This meant that the mean time from CF discovery to referring physician notification (“Total Communication Time”) was 8.8 ± 6.9 minutes with 72.5% (66/91) of these CFs communicated within 10 minutes and 93.4% (85/91) communicated within 15 minutes from the time of discovery (Table 2 and Fig 1).
Fig 1.
Distribution of total notification times of all CFs.
There was little difference in the time between the discovery of a critical finding and the attempt to contact the referring physician (“attempted notification time”) between the day and evening shifts (2.4 versus 2.5 minutes), with a slight delay (5.6 minutes) noted during the overnight period and an even greater delay on the weekend (8.7 minutes). The time between attempted notification of the referring physician and communication with the referring physician (“response time”) was similar for the weekday (5.0 minutes), evening (5.3 minutes), and overnight shifts (4.5 minutes) but slightly delayed during the weekend shifts (8.2 minutes). The total communication time was similar for the weekday shift (7.4 minutes) and evening shift (7.8 minutes; P = not significant) but was moderately delayed during the overnight shift (10.1 minute; P = not significant) and was most delayed during the weekend (16.8 minutes; P = .0006 for weekday-versus-weekend shifts). The statistical tests of the intervals between CF observed and referring physician called did not detect any differences across shifts except for daytime versus overnight and weekend shifts in which the means were 2.4, 5.6, and 8.7 minutes, respectively (P < .01 for difference between daytime and overnight and daytime and weekend). Similarly, we did not detect any differences between the work shifts for physician call-back times from referring physician called to referring physician directly informed. However, if >1 physician had to be called, the mean time from referring physician called to referring physician notified increased from 3.5 minutes to 10.1 (P < .01).
The attempted notification time ranged from 0 to 6 minutes and was similar for all clinical services. Of the top 5 services in terms of CFs notified (emergency department, internal medicine, neurosurgery, intensive care unit, and neurology), the greatest variability in mean response time was between the intensive care unit and neurology, but the difference was between 2.8 and 7.2 minutes, just 4.4 minutes. With respect to the services that had the most CFs reported, the only time interval that was statistically significant for notifications was a shorter time of referring physician paged to referring physician called back for the ED service (3.4 minutes) versus the neurology service (7.2 minutes) (Table 3).
In 13 cases, the radiologists recorded the reasons for delays in communication, which included the following: 1) inaccurate contact information for the ordering physician in the information system (5.5%, 5/91), 2) the physician being unavailable (change of shift or outpatient office closed) (4.4%, 4/91), 3) the physician did not respond in a timely fashion (3.3%, 3/91), and 4) the patient was transferred to the neonatal intensive care unit (so previous floor contact information was incorrect) (1.1%, 1/91).
When multiple paired t tests were applied to the mean times between study ordered versus referring physician notified, there were statistically significantly differences between the day shift (8 am to 4 pm) and each of the other shifts, with the exception of the weekend shift, the latter likely because of the small number of CFs reported during the weekend shift, causing loss of statistical power (n = 7). These findings were also true for day shift versus other shifts for the time interval from study completed to CF observed. The mean value of the day shift for study completed to physician notified/CF observed (102.1 minutes; SD = 87.6/94.7 minutes; SD = 87.4) varied from the means of the evening (57.6 minutes; SD = 45.9/49.8 minutes; SD = 45.7), overnight (41.5 minutes; SD = 37.7/31.6 minutes; SD = 37.8), and weekend (50.3 minutes; SD = 34.1/33.5 minutes; SD = 23.9) by the widest margins of all intervals.
The mean and median time intervals from physician placing the order to the study begun were 2 hours 50 minutes (range = 1 minute to 17 hours 49 minutes ± 6 hours 53 minutes) and 44 minutes (median) for CT (eliminating 1 case with a delay of 7 days scheduled as an outpatient), respectively, and 13 hours 59 minutes (range = 20 minutes to 19 hours 6 minutes ± 21 hours 49 minutes) and 7 hours 24 minutes (median) for MR imaging (eliminating 2 cases with delays of 7 and 8 days scheduled as outpatients), respectively. For the combined CT and MR imaging studies, the mean and median values were 6 hours 43 minutes (range = 1 minute to 19 hours 51 minutes ±14 hours 54 minutes) and 1 hour 10 minutes.
The time interval for study completion averaged 4 ± 6 minutes for CT and 47 ± 24 minutes for MR imaging, with an average for both modalities of 21 ± 33 minutes (median, 7 minutes). The delays from study ordered to preliminary report generated for CT were a mean of 2 hours 54 minutes ± 6 hours 53 minutes with a median of 45 minutes. For MR imaging, the same intervals showed a mean of 14 hours 46 minutes ± 21 hours 43 minutes from order to completion and a median value of 8 hours 51 minutes. If one combined MR imaging and CT, the mean was 7 hours 3 minutes ± 14 hours 58 minutes and the median was 1 hour 41 minutes.
Discussion
The Joint Commission encourages timely recording and communication of a critical finding to facilitate accurate diagnosis and appropriate treatment of urgent medical conditions, which in turn improves patient care and reduces unfavorable outcomes. Delays in the communication of critical findings could lead to greater morbidity or even death of patients with serious illnesses. TJC requires that radiologists take measures to ensure that critical findings are communicated expeditiously and accurately.8 However they are not proscriptive about what constitutes a critical finding or what timeframe is considered “expeditious.” Expeditious may vary from one setting to another. In the treatment of acute cerebrovascular accidents, benefits may accrue with interventions that may be minutes earlier in their onset. Similarly, early communication of critical findings has been shown to result in improved clinical outcomes in areas such as the treatment of acute pulmonary embolism.9 The Brigham and Women's Radiology Department has created the red, orange, and yellow alert system, by which caregivers are supposed to be notified for critical findings in <60 minutes, <3 hours, or <15 days, respectively.5 They include tension pneumothorax, ischemic bowel, and intracerebral hemorrhage as red alerts, intra-abdominal abscess and impending pathologic hip fracture as orange alerts, and lung nodules and solid renal masses as yellow alerts. Face-to-face or telephone communication, as described herein, is required for red and orange alert items.5
Although there is universal agreement among health care providers that rapid and accurate communication of critical radiologic findings is imperative, there are few data in neuroradiology to prove that these practices are being fully implemented and that critical findings are being notified in a timely manner.
Our data reveal that the mean time from CF discovery to physician notification was 8.8 minutes with 72.5% (66/91) of these findings communicated within 10 minutes and 93% (85/91) communicated within 15 minutes. The most common notification time (ie, the mode) was 5 minutes. These data suggest that notifications are being done within a short timeframe at our institution to ensure urgent medical attention and promote positive patient outcomes. The mean time elapsed between when the study was completed and the CF was discovered (62.2 minutes) dwarfs any part of the total notification time components. Furthermore, we found that the time interval for all CFs from study ordered to study completed constituted a mean of 7 hours 3 minutes and median of 1 hour 41 minutes. Compared to the values above, the mean time from CF discovery to physician notification of 8.8 minutes is a relatively insignificant portion of time in the overall process of obtaining and reporting the CF results of a neuroradiology imaging study.
The notifications we describe include those patients evaluated as ED patients and inpatients but also those who are outpatients for whom ready access to physicians of record may be less forthcoming, especially if cases are read after hours.
The presence of outlier notification times of >10 minutes (especially those notification times at 23, 29, 30, 35, and 37 minutes) also implies that certain modifications could be made to reduce the variability in our notification protocol for patient care. The causes of delays in communication that were identified included inaccurate contact information for the ordering physician, physician unavailable (change of shift or outpatient office closed, physician did not respond in a timely fashion, or patient transferred to another floor so that previous floor contact information was incorrect). In 1 instance, the PACS system crashed, and the delay on reboot created the delay. When only the ordering physician's name appears in our radiology information system and/or PACS, not the covering physician, our service is predisposed to errors related to “change of shift” ordering doctor versus covering doctor miscommunication.
Although it was not the focus of this article, which investigated the delays between identification of the CF and speaking to a responsible caregiver, the data regarding the interval between study completed to CF discovered had some peculiarities. Daytime cases had a longer mean delay between study completed and CF discovered (94.7 minutes) compared with evenings (49.8 minutes), nights (31.6 minutes), and weekends (33.5 minutes). The reason is not clear from the data. Various factors, including the volume of cases versus the physician staffing full time equivalents (one would expect that with fewer physicians in-house over the weekend and night shifts that the delays would be longer during these shifts), inpatient and outpatient ratios in the various shifts, the ratio of ED cases to inpatient to outpatient studies among the various shifts, and the number of on-call medical personnel, could influence these values. Overnight shifts and weekend shifts have far fewer magnets (n = 1–2) operating to manage the work lists, as opposed to the full complement of clinical magnets operating during the day shifts (10 magnets for all MR imaging clinical services). We have noted that the backup of cases in the work queue is less troublesome on the “off-shifts” than on the day shifts at our institution.
Our data compare favorably with systems reported elsewhere. Using internally developed software (later sold as a PACS plug-in called RadStream; Amicas/Merge Healthcare; http://www.beverlyhospital.org/media/483167/amicasradstream.pdf) radiologists at the Cincinnati Children's Medical Center were able to achieve an average critical result reporting time of 10.8 minutes with 53% communicated in <10 minutes and approximately 75% communicated within 20 minutes.6 Using a commercially available system (PowerScribe 360/Critical Results; Nuance Health Care/Communications; http://www.nuance.com/products/powerscribe-360-critical-results/index.htm), the Virginia Commonwealth University Health System radiology department was able to achieve an average turnaround time of 18 minutes to communicate a critical finding.10 PowerScribe 360/Critical Results software is currently in use in >300 hospitals nationally, and another system from Amcom software called Critical Test Results Management (CTRM) for Radiology is also available (Amcomsoftware.com/CTRM-Radiology).11 Our results, without using purchased software programs, are in the same range as the results provided in these reports using software solutions, albeit performed by our radiologists using their own manual effort.
The medicolegal ramifications of improved communication of critical findings between radiologists and referring physicians are obvious. Malpractice cases are often filed because of poor communication between radiologists and clinicians.12,13 Improved communication (as measured by decreased communication delay times) may lead to fewer malpractice cases brought against radiologists or medical institutions. However, the absence of communication (rather than the speed of communication) often is the more hazardous misstep in medicolegal cases.
Prior publications on critical findings have focused on determination and standardization of critical findings in neuroradiology. Some studies analyzed neuroradiologists' compliance with the National Patient Safety Goals of The Joint Commission by conducting surveys asking whether each radiology department had a critical finding list.7 As part of a practice quality-improvement initiative, another study analyzed the existing lists of critical findings and revised these lists to include frequent findings that were not already included—all in an effort to increase efficiency.4
In our neuroradiology division, we do not treat every study in the same way because stat cases and emergency department cases (eg, brain attack cases) are moved to the top of the work list. Additionally, our technologists do notify our service when they see a significant finding on a study or if they have a stat case on the technique. This practice could influence the time from acquisition to observation of a CF, the single longest time interval. However, this would not influence the communication times from time observed, to the time the call was attempted, or to the time the communication was completed, which was the emphasis of this article. What starts the clock on the communication issue is the observation of a critical finding. In other words, there is no pretest probability/suspicion of a CF mentioned. Our emphasis in this article was gaps in notification times from time observed to time communicated.
The Joint Commission mandate does not specify which times must be recorded when documenting communication of a critical finding in a patient's imaging report. However, in our institution, more detail is being sought to make sure we can meet any TJC inspections. Thus, it was proposed that radiologists should record all 3 time points (CF seen, call made, caregiver spoken to). This study has shown that in our practice, there is limited value in consistently documenting the time between initial discovery to attempted notification (mean, 3.7 minutes) and the time from attempted call to communication with the referring physician (mean, 5.2 minutes) because the overall time intervals for these steps (mean, 8.8 minutes) are so small compared with the times between completion of the studies and initially looking at the studies (62.2 minutes) and from physician ordering the study and study completion (mean 7 hours 3 minutes). Reporting the time of referring physician notification alone would seem to be sufficient because from the information system, one can readily provide the times from study completion to notification; the time of notification starts the clock for any delays in treating the critical finding by the clinical service. The delays in subsequent treatment have been shown to dwarf the communication delays provided herein as well.14 Radiologists may, in limited instances in which there is a response time delay that may impact patient care, document the delay, but this should not be perceived as a means of relieving the radiologists of a responsibility for the prompt care of the patient. Calling the patient directly is an option that the American College of Radiology guidelines mention as one possibility.2 The value in noting the time of discovery and time of contact may be to investigate any systemic sources of the breakdown of communication. Efficient communication of CFs may avert a potentially poor outcome and have a positive effect on the health of our patients.
Current protocols for notifying physicians in our neuroradiology division have led to prompt notification of neuroradiologic critical findings. The outliers for notification largely revolve around shift changes that may be mitigated by universal sign out protocols or electronic solutions in which paged physicians no longer on call provide automated feedback to other physicians informing the callers that they are off service. The hospital information system ideally should provide covering-physician contact information for all patients at all times. In addition, the use of cell phones may be a more efficient mode of communication than contact via calling a medical floor or pagers. Problems with calling a floor include residents changing shifts and services and the limited hours of duty of present-day interns and residents.
How do our results compare with another subspecialty service that frequently must notify caregivers about critical findings? In 2008, Valenstein et al14 assessed the CF notification times of 3545 specimens across 121 institutions in the College of American Pathologists Q-Probes program. The authors found that the median time from identifying the critical finding to communication of that finding was 4–5 minutes, whereas the median time from specimen collection to notification was 56–57 minutes.14 These numbers are remarkably similar to our median values of 8 minutes and 43 minutes, respectively. Valenstein et al did not record the times from lab test ordered to lab test completed. They did note that the median notification times for rural/suburban facilities (median 3 minutes) was shorter than that for a city location (median, 7 minutes—our facility is in a city environment) and was shorter in smaller hospitals (ours is a 930-bed hospital). The authors stated, “Given the amount of time that typically elapsed between specimen collection and notification, in even the speediest facilities, it is doubtful that…institution variation in calling speed makes much clinical difference.”14 They noted that the time it takes for caregivers to act on critical laboratory values ranged from 2 to 5 hours, making 5-minute notification times a very tiny proportion of the patient care process.14
Although this study presents much useful data regarding the reporting of CFs, it has some obvious limitations. We recognize that this was a random sample of cases, and in some instances, each shift or service did not have large numbers of CFs. There may be a bias because physicians were aware that this was an ongoing study; therefore, they may have been more compliant and more compulsive about pursuing the communication, knowing that data were being recorded. This could have caused artificially shortened notification times. Because there was a preponderance of inpatient/ED cases, there could be additional bias in that these services are generally more easily located and the physicians are more easily notified because of “on-call” services. Three cases had incomplete data. Outpatient studies, particularly after hours and on weekends from private physician offices, usually incur greater delays because weekend/nighttime office hours are limited. Finally, because we have some services that respond to a single phone number (ie, the neurosurgical resident on call or the emergency department main number), there may be some inherent favorable bias to the system at our institution.
This was a pilot study designed to detect general trends in the sources of communication delays. We acknowledge that using ANOVA with a Bonferroni correction rather than paired t tests would have been a more rigorous approach. At this stage, we wanted to cast a wider net, and we were willing to accept a higher cumulative false-positive rate for all of our analyses taken together. In follow-up studies, however, we plan to focus on a smaller number of the most promising factors to explore the observed relationships further and to verify our preliminary results.
Conclusions
Given the results of this study with 93.4% (85/91) of notification times in <15 minutes, there may be more merit focusing on reducing the time from study completed to study interpreted (mean in this study of 62.2 minutes) and study ordered to study completed (mean, 7 hours 3 minutes) to advance patient safety and health care quality. We agree with the conclusion of Valenstein et al14 in their article on the pathology CFs: The notification interval “represents one of the least important vulnerabilities in the process that leads to timely correction of a critical…result.” However, any effort to provide caregivers more accurate and more timely data with which to diagnose and treat their patients is a worthy endeavor. This may lead to improved outcomes, and we encourage such quality improvement projects to optimize the provision of care of radiology departments.
ABBREVIATIONS:
- CF
critical finding
- ED
emergency department
- TJC
The Joint Commission
Appendix
The Joint Commission's Patient Safety Goal 02.03.01
NPSG.02.03.01: Report critical results of tests and diagnostic procedures on a timely basis. Get important test results to the right staff person on time.
Rationale for NPSG.02.03.01
Critical results of tests and diagnostic procedures fall significantly outside the normal range and may indicate a life-threatening situation. The objective is to provide the responsible licensed caregiver these results within an established timeframe so that the patient can be promptly treated.
Elements of Performance for NPSG.02.03.01
- 1) Develop written procedures for managing the critical results of tests and diagnostic procedures that address the following:
- A) The definition of critical results of tests and diagnostic procedures
- B) By whom and to whom critical results of tests and diagnostic procedures are reported
- C) The acceptable length of time between the availability and reporting of critical results of tests and diagnostic procedures
2) Implement the procedures for managing the critical results of tests and diagnostic procedures.
3) Evaluate the timeliness of reporting the critical results of tests and diagnostic procedures.
Footnotes
Disclosures: David M. Yousem—UNRELATED: Expert Testimony: Self, medicolegal, Grants/Grants Pending: Bayer Pharmaceuticals.* Payment for Lectures (including service on Speakers Bureaus): American College of Radiology Education Center,* Royalties: Elsevier (3 books), Payment for Development of Educational Presentations: CMEInfo.com.* *Money paid to the institution.
REFERENCES
- 1. The Joint Commission. National Patient Safety Goals. http://www.jointcommission.org/standards_information/npsgs.aspx. Accessed July 10, 2013
- 2. American College of Radiology. ACR practice guidelines for communication of diagnostic imaging findings 2013. http://www.acr.org/∼/media/ACR/Documents/PGTS/guidelines/Comm_Diag_Imaging.pdf. Accessed August 15, 2013
- 3. Viertel VG, Trotter SA, Babiarz LS, et al. Reporting of critical findings in neuroradiology. AJR Am J Roentgenol 2013;200:1132–37 [DOI] [PubMed] [Google Scholar]
- 4. Trotter SA, Babiarz LS, Viertel VG, et al. Determination and communication of critical findings in neuroradiology. J Am Coll Radiol 2013;10:45–50 [DOI] [PubMed] [Google Scholar]
- 5. Anthony SG, Prevedello LM, Damiano MM, et al. Impact of a 4-year quality improvement initiative to improve communication of critical imaging test results. Radiology 2011;259:802–07 [DOI] [PubMed] [Google Scholar]
- 6. Ridley EL. Critical results notification system speeds timely results. AuntMinnie.com. http://www.auntminnie.com/index.aspx?sec=ser&sub=def&pag=dis&ItemID=104083. Accessed July 31, 2013
- 7. Babiarz LS, Trotter S, Viertel VG, et al. Neuroradiology critical findings lists: survey of neuroradiology training programs. AJNR Am J Neuroradiol 2013;34:735–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yee KM. Critical test results: make every effort to communicate. AuntMinnie.com. http://www.auntminnie.com/index.aspx?sec=ser&sub=def&pag=dis&ItemID=99363. Accessed July 31, 2013
- 9. Kumamaru KK, Hunsker AR, Kumamaru H, et al. Correlation between early direct communication of positive CT pulmonary angiography findings and improved clinical outcomes. Chest 2013;144:1546–54 [DOI] [PubMed] [Google Scholar]
- 10. VCU Medical Center. Virginia Commonwealth University Health System significantly reduces CTR notification turnaround time. http://www.nuance.com/ucmprod/groups/healthcare/@web-enus/documents/collateral/nd_003048.pdf. Accessed August 2, 2013
- 11. Amcom Software. Improve communication of radiology test results. http://www.amcomsoftware.com/solutions/clinical_alerting_and_notification/critical_test_results/. Accessed August 2, 2013
- 12. Whang JS, Baker SR, Patel R, et al. The causes of medical malpractice suits against radiologists in the United States. Radiology 2013;266:548–54 [DOI] [PubMed] [Google Scholar]
- 13. Gale BD, Bissett-Siegel DP, Davidson SJ, et al. Failure to notify reportable test results: significance in medical malpractice. J Am Coll Radiol 2011;8:776–79 [DOI] [PubMed] [Google Scholar]
- 14. Valenstein PN, Wagar EA, Stankovic AK, et al. Notification of critical results: a College of American Pathologists Q-Probes study of 121 institutions. Arch Pathol Lab Med 2008;132:1862–67 [DOI] [PubMed] [Google Scholar]