SUMMARY:
Antiplatelet agents are an important component of the preventive strategies currently used in clinical practice to minimize the risk of thromboembolic events during and after endovascular procedures. Because of the variability in the response to antiplatelet agents, measuring the degree of platelet inhibition may help identify and properly treat poor responders. POC testing is defined as diagnostic testing at or near the site of patient care. Knowledge of the specifics of these devices among practicing neurointerventionalists is relatively limited. In this article, the different POC devices available are presented, and their clinical utility in relation to endovascular procedures is discussed.
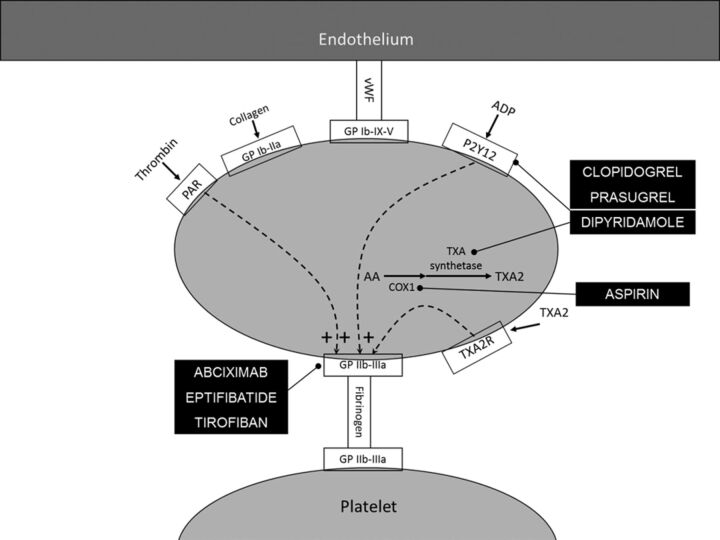
The introduction of foreign bodies into the blood stream, injury to the vessel wall, and plaque disruption are factors that lead to platelet activation during endovascular procedures,1,2 as has been shown in multiple studies performed in patients undergoing coronary or cerebral angioplasty.3,4 Angioplasty and stent placement are associated with an increased risk of thromboembolism.5 Antiplatelet agents are used in conjunction with anticoagulants to reduce the rate of thrombotic complications. Figure 1 offers a simplified overview of the mechanism of action of different antiplatelet agents.
Fig. 1.
The process of platelet activation and targets for antiplatelet agents. Platelet activators are shown with their corresponding receptors on the platelet surface. Antiplatelet agents are indicated at the point of their mechanism of action. Note the positive feedback provided by ADP and thrombin released by activated platelets.
The response to antiplatelet agents is variable. This can be identified by testing platelet function. Several POC devices are commercially available, which can be used in the angiographic suite to measure platelet function and possibly modify the antiplatelet dose. These devices differ in the platelet function/property they test, the end point, the method of end point detection, and their ability to predict outcome. In this article, we review the most commonly used POC devices for measuring platelet function, explaining mechanism of action and potential utility in the neuroendovascular practice. The Table summarizes the main features of the devices discussed in this article.
POC Platelet Function Measuring Devices
Rapid Platelet Function Assay: VerifyNow
VerifyNow (Accumetrics, San Diego, California) (formerly known as the Ultegra RPFA) is a whole-blood POC device. It is based on the phenomenon of platelet aggregation as measured by light transmittance, similar to the LTA test. When a light beam shines through platelets containing fluid (whole blood or plasma in the case of VerifyNow and LTA, respectively), it is scattered by platelets. When there are fewer platelets, light transmittance increases. In the case of VerifyNow, platelets aggregate around fibrinogen-coated polystyrene beads, leading to increased light transmittance. The instrument measures this change in optical signal intensity caused by aggregation.6 Different platelet agonists are used depending on which assay is being performed. If platelets are not inhibited, the activation process will ensue with subsequent platelet aggregation. This method was initially designed to measure the effects of GP IIb/IIIa inhibitors,7 but now modified assays are available to measure the effect of aspirin, clopidogrel, and prasugrel.8
In the VerifyNow aspirin assay, arachidonic acid is the platelet agonist used. If aspirin has produced the expected antiplatelet effect, inhibiting cyclo-oxygenase, arachidonic acid will not be converted to thromboxane A2 and platelets will exhibit minimal aggregation around beads. Results are interpreted on the basis of the extent of platelet aggregation reported in ARUs. A preclinical trial conducted by the manufacturer suggested that in patients who are on aspirin, a value of <550 ARU demonstrates an aspirin effect, while a value of ≥550 ARU indicates no platelet dysfunction (ie, cyclo-oxygenase resistance) with 91% sensitivity and 100% specificity.6 However, this cutoff has been challenged by other studies.9
VerifyNow P2Y12 assay is used to measure the effect of P2Y12 ADP-receptor inhibitors clopidogrel and prasugrel.10 ADP is used to maximally activate the platelets by binding to the P2Y1 and P2Y12 platelet receptors. Prostaglandin E1 is used to suppress the ADP-induced P2Y1-mediated platelet activation and, therefore, increase assay sensitivity.11 A second channel of the device, referred to as baseline channel, assesses the baseline platelet function by measuring P2Y12-independent platelet activation. This is measured by using iso-thrombin-receptor-activating peptide with PAR4-activating peptide and fibrinogen-coated beads. The device reports 2 results for each assay: 1) P2Y12 PRU, indicating the amount of P2Y12 receptor-mediated aggregation specific to the platelet, calculated as a function of the rate and extent of platelet aggregation in the ADP channel; and 2) the percentage change from baseline aggregation, which is calculated from the PRU result and the BASE result as follows: Percentage Inhibition = (BASE − PRU/BASE) × 100.11
Low PRU (or higher percentage inhibition) indicates high P2Y12-receptor inhibition and good response to clopidogrel or prasugrel. Results may be affected by GP IIb/IIIa inhibitor drugs and cilostazol, but aspirin and other nonsteroidal anti-inflammatory drugs have no effect. There are no data on patients with platelet counts of <100,000/mL or inherited platelet disorders.12 In a prospective study (n = 147), the reference range for baseline platelet function by using P2Y12 assay 194–418 PRU (mean, 307 PRU), which dropped to 17–100 PRU (mean, 110 PRU) 24 hours after administration of 450 mg of clopidogrel and to 23–100 PRU (mean, 37 PRU) after administration of 75 mg of clopidogrel for at least 7 days. Overall, clopidogrel therapy resulted in a mean 64 ± 25% PRU reduction.11
VerifyNow GP IIb/IIIa assay uses iso-thrombin-receptor-activating peptide as an activator. The assay reports patient results in PAU, which indicate the amount of iso-thrombin-receptor-activating peptide-mediated activation of GP IIb/IIIa receptors involved in platelet aggregation. Expected values are in the range of 0–330 PAU. In a study, there were no differences in baseline PAU values between patients with and without the following medications: aspirin, ticlopidine, clopidogrel, heparin, warfarin, acetaminophen, nonsteroidal anti-inflammatory drugs, beta blockers, calcium channel blockers, statins, and nitrates. Assay performance was not affected by platelet count values between 98,000 and 376,000 platelets per microliter or hematocrit values between 23% and 45%.13 The GOLD (from the chemical symbol of gold, AU: ‘Assessing Ultegra’) study was a prospective observational single-arm study that enrolled 485 patients undergoing PCI with the planned use of a GP IIb/IIIa inhibitor. Most patients (84%) received abciximab. Platelet inhibition was measured serially after GP IIb/IIIa-inhibitor initiation by using VerifyNow (then known as Ultegra RPFA). Major adverse cardiac events (composite of death, myocardial infarction, and urgent target vessel revascularization) were prospectively monitored, and the incidence was correlated with the measured level of platelet function inhibition. Patients who did not achieve ≥95% inhibition 10 minutes after the bolus experienced a significantly higher incidence of the composite outcome (14% versus 6%, P = .006). Patients whose platelet function was <70% inhibited at 8 hours after the start of therapy had a higher rate of adverse events compared with those ≥70% (25% versus 8%, P = .009). By multivariate analysis, platelet function inhibition ≥95% at 10 minutes after the start of therapy was associated with a significant decrease in the incidence of a major adverse cardiac event (odds ratio, 0.46; 95% CI, 0.22–0.96; P = .04).13
Plateletworks
Plateletworks (Helena Laboratories, Beaumont, Texas; previously known as ICHOR Plateletworks) is a simple assay that uses standard cell-counting principles. The ICHOR Hematology Analyzer (Helena Laboratories) is the device used to perform the assay. The platelet count is performed with a fresh whole-blood sample that passes through an aperture, thereby interrupting a constant electrical current and resulting in an electrical pulse that is amplified and sorted to provide the final platelet count. Two values are obtained, baseline count and another count after adding a platelet agonist. In the presence of an agonist, platelets aggregate; therefore, they exceed the threshold limitations for platelet size and are no longer counted as platelets. The difference in the platelet count between the 2 samples provides a measurement of platelet aggregation and is reported as percentage aggregation per the following equation: Baseline Platelet Count − Agonist Platelet Count/Baseline Platelet Count × 100.14–16 Currently, 3 assays are commercially available using 3 different agonists: collagen, ADP, and arachidonic acid. The arachidonic acid assay is specifically designed to measure the antiplatelet activity of aspirin, while both the collagen and ADP assays can be used to measure the antiplatelet effects of GP IIb/IIIa inhibitors, clopidogrel, prasugrel, and ticlopidine.16
On the basis of data collected from healthy volunteers and patients undergoing PCI and cardiopulmonary bypass, the package insert of the ADP/collagen Plateletworks assay states that the correlation with LTA was found to be 0.83 (Pearson correlation).16 In a recent report, data from 160 patients on dual antiplatelet therapy undergoing PCI showed that the results of Plateletworks were strongly correlated with both “peak” (r = 0.71, P = .0001) and “late” aggregation (r = 0.74, P = .0001) as measured by LTA. However, the absolute degree of platelet aggregation was consistently higher when measured with Plateletworks compared with LTA (71 ± 25% versus 61 ± 12%, P = .0001). This discrepancy was explained by the fact that single platelet counting is sensitive to microaggregation, whereas LTA measures macroaggregation only. The same study showed that Plateletworks is highly time-dependent. The absolute percentage of aggregation was not significantly different at 5 and 10 minutes, but between 10 and 15 minutes, the absolute percentage of aggregation decreased significantly from 64 ± 6% to 35 ± 8%, (P = .0001) in the patients on dual antiplatelet therapy and from 96% ± 1% to 71% ± 7% (P = .005) in the healthy volunteers. The overestimation at 15 minutes is because of disaggregation of the formed aggregates.17
Characteristics of main POC devices used to measure platelet functions tests
| Test/Device | Manufacturer | Technique | Unit | Remarks |
|---|---|---|---|---|
| PFA-100 | Siemens Diagnostic Deerfield, Illinois | Measures time to complete occlusion an aperture in a capillary-like membrane under sheer force | Closure time (for all 3 assays) | Three assays vary in platelet agonist: CEPI assay, CADP assay, and Innovance. Simulates physiologic conditions, significantly affected von Willebrand factor |
| Platelet Works | Helena Laboratories Beaumont, Texas | Measures platelet count before and after addition of platelet activating factor | % Aggregation | Time dependent |
| Impact and Impact-R | DiaMed, Cressier, Switzerland | Measures platelet inhibition induced by shear stress | Surface coverage, average size | Simulates physiologic conditions, significantly affected von Willebrand factor, Impact-R more suitable for testing antiplatelet effect |
| VerifyNow | Accumetrics, San Diego, California | Measures optical signal of light transmitted through whole blood which depends on the degree of platelet aggregation around fibrinogen coated beads | Aspirin Reaction Units (Aspirin assay), P2Y12 Reaction Units (P2Y12 assay), Platelet Aggregation Units (GP IIb/IIIa assay) | Three assays vary in platelet agonist: Aspirin assay, P2Y12 assay, and Gp IIb/IIIa assay. Based on the same concept of light transmittance as, and correlates well with LTA |
| P2Y12 assay: PRUs, GP IIb/IIIa assay: PAUs | ||||
| Clot Signature Analyzer | Xylum Corporation Scarsdale, New York | Measures the time for platelets to occlude holes “punched” in a blood conduit and collagen-induced thrombus formation as blood flows in a channel containing a collagen fiber | Platelet Hemostasis Time (bleeding time equivalent), Clot Time (ACT equivalent), Collagen Induced Thrombus Formation | Assess multiple aspects of hemostasis under near-physiologic conditions |
PFA-100
The PFA-100 System (Siemens Healthcare Diagnostics, Deerfield, Illinois) is designed to simulate hemostasis in a blood vessel. In disposable test cartridges, anticoagulated whole blood is aspirated from the sample reservoir through a capillary and an aperture in a platelet agonist−coated membrane, thereby exposing platelets to high-shear-flow and biochemical activation simultaneously. The agonists at the membrane trigger platelet adhesion, activation, and aggregate formation at the aperture. Closure time is the time required to occlude the central aperture (diameter, 100 μm), resulting in cessation of blood flow. Closure time depends on different variables, such as von Willebrand factor levels, platelet count, and hematocrit.18–20 The role of von Willebrand factor, in particular, is important because it is essential for platelet plug formation under shear stress. In fact, the PFA-100 has been more useful in screening for von Willebrand disease20,21 and verifying the effect of desmopressin acetate in presurgical patients22 than it has been in predicting outcome following PCI or blood loss after open heart surgery.23
Two test cartridges were developed initially with a membrane coated either with collagen and epinephrine (CEPI) or collagen and ADP (CADP). Aspirin prolongs the CEPI-closure time, more than the CADP-closure time.21,24 Initially, the CADP cartridge was thought to be suitable for measuring P2Y12-receptor inhibition. However, studies have shown the CADP to be unsuitable for assessing the efficacy of clopidogrel therapy,25 especially among patients with stroke.26 This finding is because collagen-mediated platelet activation and the residual activation potential of ADP via the P2Y1 receptor are sufficient to overcome the effect of P2Y12-receptor blockade.27 Pidcock and Harrison27 showed that a secondary addition of MRS 2179, a P2Y1-receptor antagonist, to a blood sample, already treated with the P2Y12-receptor antagonist, cangrelor, resulted in significant prolongation of the CADP-closure-time. This prompted the development of a third cartridge, the Innovance PFA P2Y (Siemens Healthcare Diagnostics, Deerfield, Illinois), which was specifically designed for the purpose of clopidogrel monitoring.18 This device was found to have a high sensitivity for the detection of P2Y12 receptor blockade but only a limited specificity for a good response to clopidogrel compared with flow cytometry analysis of intracellular vasodilator-stimulated phosphoprotein phosphorylation.28
Impact and Impact-R
The cone and plate instruments have been used in studying physical properties (mainly to measure viscosity) of fluids since the 1930s. The idea is to trap fluid between a cone with a very shallow angle and a flat plate. When the cone rotates, shear is created. The initial cone and plate(let) analyzer device Impact (DiaMed, Cressier, Switzerland) used the same idea.29 A whole-blood sample is trapped between a Teflon (Dupont, Wilmington, Delaware) cone and a plate covered with extracellular matrix, known to have thrombogenic properties. The cone rotation at a speed of 1300/s creates a high shear stress similar to the arterial environment. The sample is then washed with phosphate buffered saline, stained, and air-dried. Platelet adhesion and aggregation on the extracellular matrix are evaluated by using an image analyzer. Data are expressed as a percentage of surface coverage and average size. Surface coverage is a reflection of platelet adhesion while average size reflects platelet aggregation. Both of these parameters reach maximal values after 2 minutes and are affected by hematocrit and platelet count. Under low- or high-shear conditions, comparable adhesion occurs but the higher shear creates an additional progressive platelet aggregation.29 In vitro studies demonstrated a dose-dependent inhibition of platelet deposition with blocking of the GP IIb/IIIa receptor by abciximab or tirofiban and of GP IIb by a recombinant of the von Willebrand factor fragment, which correlated to the inhibitory effect as tested by LTA.30 The cone and plate(let) analyer has been used to assess platelet function in different clinical situations, such as in patients with diabetes,31 thrombocytopenia,32 von Willebrand disease,30 and thrombotic thrombocytopenic purpura.33
Samples subjected to a second run after being transferred to a new extracellular matrix–coated well demonstrate a decrease in the adhesion properties of platelets with associated microaggregate formation in the suspension. This phenomenon, called transient adhesion refractoriness, is dependent on platelet activation during the first run and is prevented by addition of apyrase (ADP scavenger) or ADP-receptor inhibitor, suggesting a role for ADP in mediating this response.34 Exposure to platelet stimulants such as ADP and thrombin-receptor-activating peptide results in a similar transient adhesion refractoriness; after the second run.34 Transient adhesion refractoriness was used to modify the cone and plate(let) analyzer test (Impact-R device, DiaMed) and to evaluate the effect of the antagonists on platelet function.35 This modification entailed the incubation of the whole-blood sample with ADP or arachidonic acid (both of which are platelet agonists shown to cause transient adhesion refractoriness; for 1 minute before performing the cone and plate(let) analyzer test. The effect of arachidonic acid was prevented by aspirin and that of ADP was reduced by 2-methylthio-AMP, a P2Y12 ADP receptor inhibitor. There was a modest correlation observed between the modified cone and plate(let) analyzer and aggregometry (R2 = 0.55). Of note, in the absence of platelet agonists, aspirin did not cause significant change in surface coverage, while 2-methylthio-AMP reduced platelet deposition.35 However, the Impact-R ADP test has shown significant variability in healthy subjects. After administration of a high clopidogrel loading dose (600 mg), 62% of the patients were identified as clopidogrel nonresponders as opposed to 24% and 34% by using LTA and vasodilator-stimulated phosphoprotein phosphorylation analysis, respectively. Head-to-head comparison with optical aggregometry in 451 patients showed only a modest correlation between both methods (r = 0.20, P = .0001).17
Clot Signature Analyzer
CSA (Xylum, Scarsdale, New York) is a global hemostasis screen for assessing both platelet function and fibrin clot formation under shear stress. The device is composed of a closed pressurized tubing system in which whole nonanticoagulated blood is perfused under physiologic flow conditions. Two holes are punched in the tube, and the resulting drop in pressure is recorded. The PHT (bleeding time equivalent) is the time required for the holes to be plugged by a platelet and fibrin clot and is measured by recovery of the pressure. As the platelet plug propagates and a fibrin clot is formed, the tube becomes occluded and pressure at the distal end of the tube falls and is measured as the closure time (activated-clotting-time equivalent). Whole blood is also passed through another tube containing collagen fibrils. Platelets adhere to collagen with subsequent aggregation, release, and fibrin clot formation. The CITF is the time required for a collagen-induced thrombus to occlude completely a tube of flowing blood. CITF is defined as the time to a 50% decrease in pressure.36,37
The effect of GP IIb/IIIa inhibitors was evaluated and compared with LTA in 36 patients undergoing PCI.38 Platelet function was assessed at baseline and 10 minutes following a clinically recommended dose of 1 of the 3 GP IIb/IIIa inhibitors. All agents profoundly inhibited shear-induced platelet function. Prolongation of PHT and CITF was independent of the agent. Neither PHT nor CITF correlated with LTA measurements. PHT and CITF were prolonged greater than the assay (ie, >30 minutes, which is the maximum time displayed by the Clot Signature Analyzer) in all except 7 patients, indicating that Clot Signature Analyzer lacked sensitivity to discriminate platelet function under conditions of profound inhibition by these agents.38
Comparison of Various Platelet Function Tests
There is a definite correlation between 1 platelet function test and another. However, these results are not identical and are not interchangeable. A patient who is categorized as having adequate platelet inhibition by 1 test may not be categorized the same using another test. It is difficult to compare different platelet function tests because of their variance and unique attributes. Agonists of different concentrations, risk of damaging and activating platelets before the test during phlebotomy and collection, and temperature variations need to be standardized before results of platelet inhibition from different assays can be compared.39 The commonly used POC platelet function tests such as Plateletworks, VerifyNow, and PFA-100 are affected by the variability of platelet count, platelet response, and platelet-receptor concentration.40 Some of the tests do not have assays that can measure platelet inhibition by all antiplatelet agents. The PFA-100 is also not very sensitive to the antiplatelet effects of clopidogrel.41
In 1 study, 4 assays measuring clopidogrel-mediated platelet inhibition (VerifyNow P2Y12, vasodilator-stimulated phosphoprotein phosphorylation assay, multiple electrode aggregometry, and Impact-R) were compared with LTA in 80 patients with peripheral, coronary, carotid, or visceral artery disease treated with stent placement followed by aspirin and clopidogrel. The cutoff values were a maximal aggregation of ≥62% for LTA, PRUs of ≥273 for VerifyNow, platelet reactivity index ≥69% for the phophorylation assay, Assessing Ultegra ≥68 for multiple electrode aggregometry, and a surface coverage of ≤2% for Impact-R. Twenty patients (25%) had residual ADP-inducible platelet aggregation by LTA criteria despite pretreatment with clopidogrel. All 4 assays correlated significantly with LTA but with a variable degree of correlation strength. VerifyNow revealed the strongest correlation (r = 0.61), while Impact-R had the weakest correlation (r = 0.33). The rate of discordance (patients meeting the cutoff value in 1 test but not the other) ranged from 22.5% (between LTA and VerifyNow) to 32.5% (between LTA and multiple electrode aggregometry). This study demonstrated the considerable variability among these 5 tests.42
The study called Do Platelet Function Assays Predict Clinical Outcomes in Clopidogrel-Pretreated Patients Undergoing Elective PCI (known as POPULAR study), was a prospective observational single-center study of 1069 consecutive clopidogrel-pretreated patients who underwent elective coronary stent placement. The primary end point (defined as a composite of all-cause death, nonfatal acute myocardial infarction, stent thrombosis, and ischemic stroke) was correlated with platelet reactivity as measured by LTA and at least 1 of the following POC devices: VerifyNow, Plateletworks, Impact-R, and PFA-100. The study found that after 1 year, the primary end point occurred more frequently in patients with high on-treatment platelet reactivity as tested by LTA, (11.7% versus 6.0%, P < .001), VerifyNow (13.3% versus 5.7%, P < .001), and Plateletworks (12.6% versus 6.1%, P = .005).43 Impact-R and PFA-100 results were not significantly associated with the primary end point. None of the assay measurements were able to predict patients with high bleeding risks following PCI.43
Utility of Platelet Function Tests in Patients Undergoing PCI
Antiplatelet regimens are always used in patients who are undergoing PCI. Typically, the procedure is done under dual-antiplatelet coverage. GP IIb/IIIa inhibitors are commonly used as well. However, the most appropriate dosing, treatment duration, and choice of antiplatelet agents are still a subject of debate.44,45 Some data support the finding that a poor response to antiplatelet treatment detected by POC testing predicts ischemic complications in patients undergoing PCI. A study that measured platelet hyper-reactivity by using a PFA-100 device (a CEPI-closure time test) among 256 patients who underwent PCI found that the in-stent thrombosis-free survival for patients with CEPI-closure time < 190 seconds was lower than that in those who had CEPI > 190 seconds both at 1 month (95.4% versus 99.3%) and at 9 months (83.6% versus 96.4%), suggesting that patients with platelet hyper-reactivity after PCI are at higher risk for in-stent thrombosis.46
POC devices can help identify patients who are aspirin-resistant. The VerifyNow device was used to determine aspirin responsiveness in patients with aspirin use of 80–325 mg daily for ≥1 week scheduled for nonurgent PCI. All patients received a 300-mg loading dose of clopidogrel >12 hours before and a 75-mg maintenance dose in the morning of the PCI. Of 151 patients, 19% were noted to be aspirin-resistant (defined as ARU ≥ 550). Multivariate analysis revealed aspirin resistance to be an independent predictor of myonecrosis identified by creatine kinase myocardial band elevation (odds ratio, 2.9; 95% CI, 1.2–6.9; P = .015).47
However, other studies did not find a correlation between aspirin resistance and cardiac complications post-PCI.48,49
Clopidogrel resistance as measured by POC devices has been associated with complications post-PCI in some studies. In 1 study, 804 patients underwent drug-eluting stent placement after receiving 600 mg of clopidogrel followed by dual antiplatelet therapy with aspirin and clopidogrel. The 6-month incidence of in-stent thrombosis was higher among clopidogrel nonresponders (8.6% versus 2.3%, P < .001).50 Another study compared 26 patients who had angiographically determined in-stent thrombosis with 21 patients who did not have in-stent thrombosis. The rate of clopidogrel resistance in those with in-stent thrombosis was 40% versus 14% (P = .02), while the rate of aspirin resistance was not different between the 2 groups (23% versus 5%, P value nonsignificant) as assessed by VerifyNow.51 In an attempt to utilize POC devices to individualize antiplatelet therapy following PCI, the Gauging Responsiveness With a VerifyNow P2Y12 Assay: Impact on Thrombolysis and Safety (GRAVITAS) trial randomized patients with high on-treatment platelet reactivity (defined as ≥230 PRU) to a regimen of high-dose (600 mg loading dose; 150 mg/d maintenance dose) or standard-dose (300 mg loading dose; 75 mg/d maintenance dose) of clopidogrel. There was no difference in the rate of occurrence of the primary end point (6-month incidence of death from cardiovascular causes, nonfatal myocardial infarction, or stent thrombosis) between the 2 groups (hazard ratio, 1.01; 95% CI, 0.58–1.76; P = .97).52 However, in a subsequent analysis, when a more stringent cutoff of ≥208 PRU was selected to define adequate platelet inhibition, there was a significant association with lower cardiovascular events at 60 days (hazard ratio, 0.23; 95% CI, 0.05 to 0.98; P = .047) and tended to be associated at 6 months (hazard ratio, 0.54; 95% CI, 0.28 to 1.04; P = .065).53
Recent studies support the concept of global antiplatelet resistance. A study of 219 patients treated with aspirin and clopidogrel before PCI found that the rate of low response to aspirin was 16%; to clopidogrel, 15%; and to both, 9% by using multiple electrode aggregometry. The highest rate of myocardial infarction and composite ischemic events at 30 days was seen among patients with low response to both medications.54
Another study assessed the response to a clopidogrel loading dose among 150 patients undergoing PCI who were categorized as either aspirin-resistant or aspirin-sensitive. Forty-seven percent of patients with aspirin resistance were also clopidogrel-resistant diagnosed using multiple platelet function tests. The incidence of dual antiplatelet low response was estimated at 6% in 746 patients with PCI. Patients with dual-antiplatelet low response were at significantly higher risk of in-stent thrombosis (hazard ratio, 3.18; P = .027) and the composite end point of cardiac mortality and in-stent thrombosis (hazard ratio, 2.94; P = .022).55
Several approaches have been proposed to manage dual antiplatelet resistance, including increasing the clopidogrel dose from 75 to 150 mg daily56 and adding a third antiplatelet agent. However, there is no consensus on these approaches.57,58
The magnitude of platelet inhibition may also predict the risk of PCI-associated bleeding complications. Measurement of platelet inhibition with multiple electrode aggregometry in 2533 patients who received 600 mg of clopidogrel before undergoing PCI demonstrated that the risk of major bleeding was significantly higher in patients with enhanced response to clopidogrel (n = 975) compared with the other patients (2.2% versus 0.8%; adjusted odds ratio, 3.5).59
Utility of Platelet Function Tests in Patients Undergoing Neuroendovascular Procedures
Few studies addressed the issue of monitoring platelet function in relation to neuroendovascular procedures. A study identified inadequate platelet inhibition (defined as <550 ARU for aspirin and >50% inhibition of the P2Y12/ADP receptor unit for clopidogrel by using the VerifyNow assay) in 13% of patients who took aspirin versus 66% of patients who took clopidogrel (P < .0001) among 216 patients who took aspirin or clopidogrel before their procedures. Inadequate platelet inhibition by POC testing was more common among patients who were administered 600 mg of clopidogrel within 6 hours of the procedure than in patients who had taken 300 mg within 24 hours or 75 mg daily for at least 7 days before the procedure.60
Another study that defined ideal platelet inhibition as <550 ARU for aspirin and >40% inhibition for clopidogrel by using VerifyNow included 98 patients. Those patients were given a 300-mg loading dose of clopidogrel followed by 325 mg of aspirin and 75 mg of clopidogrel daily for 5–10 days before their procedure. Among them, 2.1% were found to be poor aspirin responders and 42.9% were poor clopidogrel responders.61 In this study, all 3 patients who had procedure-related thrombosis had <20% platelet inhibition.
The use of POC testing has been evaluated in patients treated with GP IIb/IIIa inhibitors. The Ultegra device was used to measure platelet activity during intravenous eptifibatide infusion during internal carotid artery stent placement. The mean value of platelet-aggregation inhibition after a first 180-mcg/kg bolus was 91 ± 6% (range, 80%–100%), and after a second 180-mcg/kg bolus, was 96 ± 4% (range, 86%–100%). Although a high degree of inhibition was obtained initially, the mean inhibition at 1 hour was reduced to 80% despite ongoing intravenous maintenance administration of 2 mcg/kg/min, suggesting an early loss of inhibition and a need for monitoring to titrate dosing to individual responses.62
Conclusions
Recognition of the individual variability in inhibition of platelet aggregation and the ability to measure such variability with POC testing may lead to the development of more effective strategies to reduce thromboembolic events associated with neuroendovascular procedures. However, a detailed understanding of the differences in design, function, and interpretation of the results of those POC tests is essential to ensure improvement in the care of patients.
ABBREVIATIONS:
- ADP
adenosine diphosphate
- AMP
adenosine monophosphate
- ARU
aspirin reaction unit
- BASE
baseline
- CADP
collagen/ADP test cartridge
- CEPI
collagen/epinephrine test cartridge
- CI
confidence interval
- CITF
collagen-induced thrombus formation
- GP IIb/IIIa
glycoprotein IIb/IIIa
- LTA
light-transmission aggregometry
- PAR
protease-activated receptors
- PAU
platelet aggregation units
- PCI
percutaneous coronary intervention
- PHT
platelet hemostasis time
- POC
point-of-care
- PRU
P2Y12 reaction units
References
- 1. Qureshi AI, Luft AR, Sharma M, et al. Prevention and treatment of thromboembolic and ischemic complications associated with endovascular procedures. Part II. Clinical aspects and recommendations. Neurosurgery 2000;46:1360–75, discussion 1375–76 [DOI] [PubMed] [Google Scholar]
- 2. Krpski WC, Bass A, Kelly AB, et al. Heparin-resistant thrombus formation by endovascular stents in baboons: interruption by a synthetic antithrombin. Circulation 1990;82:570–77 [DOI] [PubMed] [Google Scholar]
- 3. Ries T, Buhk J-H, Kucinski T, et al. Intravenous administration of acetylsalicylic acid during endovascular treatment of cerebral aneurysms reduces the rate of thromboembolic events. Stroke 2006;37:1816–21 [DOI] [PubMed] [Google Scholar]
- 4. Riedel C, Tietke M, Alfke K, et al. Subacute stent thrombosis in intracranial stenting. Stroke 2009;40:1310–14 [DOI] [PubMed] [Google Scholar]
- 5. Sutton JM, Ellis SG, Roubin GS, et al. Major clinical events after coronary stenting: the multicenter registry of acute and elective Gianturco-Roubin stent placement—the Gianturco-Roubin Intracoronary Stent Investigator Group. Circulation 1994;89:1126–37 [DOI] [PubMed] [Google Scholar]
- 6. VerifyNow aspirin assay [package insert]. San Diego, California: Accumetrics. [Google Scholar]
- 7. Smith JW, Steinhubl SR, Lincoff AM, et al. Rapid platelet-function assay: an automated and quantitative cartridge-based method. Circulation 1999;99:620–25 [DOI] [PubMed] [Google Scholar]
- 8. Ang L, Mahmud E. Monitoring oral antiplatelet therapy: is it justified? Ther Adv Cardiovasc Dis 2008;2:485–96 [DOI] [PubMed] [Google Scholar]
- 9. Nielsen HL, Kristensen SD, Thygesen SS, et al. Aspirin response evaluated by the VerifyNow Aspirin System and light transmission aggregometry. Thromb Res 2008;123:267–73 [DOI] [PubMed] [Google Scholar]
- 10. Antman EM, Wiviott SD, Murphy SA, et al. Early and late benefits of prasugrel in patients with acute coronary syndromes undergoing percutaneous coronary intervention: a TRITON-TIMI 38 (TRial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet InhibitioN with Prasugrel-Thrombolysis In Myocardial Infarction) analysis. J Am Coll Cardiol 2008;51:2028–33 [DOI] [PubMed] [Google Scholar]
- 11. Malinin A, Pokov A, Spergling M, et al. Monitoring platelet inhibition after clopidogrel with the VerifyNow-P2Y12(R) rapid analyzer: the VERIfy Thrombosis risk ASsessment (VERITAS) study. Thromb Res 2007;119:277–84 [DOI] [PubMed] [Google Scholar]
- 12. VerifyNow P2Y12 Assay [Package Insert]. San Diego, California: Accumetrics. [Google Scholar]
- 13. Steinhubl SR, Talley JD, Braden GA, et al. Point-of-care measured platelet inhibition correlates with a reduced risk of an adverse cardiac event after percutaneous coronary intervention: results of the GOLD (AU-Assessing Ultegra) multicenter study. Circulation 2001;103:2572–78 [DOI] [PubMed] [Google Scholar]
- 14. Lakkis NM, George S, Thomas E, et al. Use of ICHOR-platelet works to assess platelet function in patients treated with GP IIb/IIIa inhibitors. Catheter Cardiovasc Interv 2001;53:346–51 [DOI] [PubMed] [Google Scholar]
- 15. Carville DG, Schleckser PA, Guyer KE, et al. Whole blood platelet function assay on the ICHOR point-of-care hematology analyzer. J Extra Corpor Technol 1998;30:171–77 [PubMed] [Google Scholar]
- 16. Helena Laboratories. Plateletworks: Platelet Function Kits. http://www.helena.com/plateletworks.html. Accessed January 2011
- 17. van Werkum JW, Kleibeuker M, Postma S, et al. A comparison between the Plateletworks-assay and light transmittance aggregometry for monitoring the inhibitory effects of clopidogrel. Int J Cardiol 2010;140:123–26 [DOI] [PubMed] [Google Scholar]
- 18. Linnemann B, Schwonberg J, Rechner AR, et al. Assessment of clopidogrel non-response by the PFA-100 system using the new test cartridge INNOVANCE PFA P2Y. Ann Hematol 2010;89:597–605 [DOI] [PubMed] [Google Scholar]
- 19. Kundu SK, Heilmann EJ, Sio R, et al. Description of an in vitro platelet function analyzer–PFA-100. Semin Thromb Hemost 1995;21(suppl 2):106–12 [DOI] [PubMed] [Google Scholar]
- 20. Fressinaud E, Veyradier A, Truchaud F, et al. Screening for von Willebrand disease with a new analyzer using high shear stress: a study of 60 cases. Blood 1998;91:1325–31 [PubMed] [Google Scholar]
- 21. Homoncik M, Jilma B, Hergovich N, et al. Monitoring of aspirin (ASPIRIN) pharmacodynamics with the platelet function analyzer PFA-100. Thromb Haemost 2000;83:316–21 [PubMed] [Google Scholar]
- 22. Koscielny J, von Tempelhoff GF, Ziemer S, et al. A practical concept for preoperative management of patients with impaired primary hemostasis. Clin Appl Thromb Hemost 2004;10:155–66 [DOI] [PubMed] [Google Scholar]
- 23. Fattorutto M, Pradier O, Schmartz D, et al. Does the platelet function analyser (PFA-100) predict blood loss after cardiopulmonary bypass? Br J Anaesth 2003;90:692–93 [DOI] [PubMed] [Google Scholar]
- 24. Marshall PW, Williams AJ, Dixon RM, et al. A comparison of the effects of aspirin on bleeding time measured using the Simplate method and closure time measured using the PFA-100, in healthy volunteers. Br J Clin Pharmacol 1997;44:151–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Golanski J, Pluta J, Baraniak J, et al. Limited usefulness of the PFA-100 for the monitoring of ADP receptor antagonists–in vitro experience. Clin Chem Lab Med 2004;42:25–29 [DOI] [PubMed] [Google Scholar]
- 26. Kotzailias N, Elwischger K, Sycha T, et al. Clopidogrel-induced platelet inhibition cannot be detected by the platelet function analyzer-100 system in stroke patients. J Stroke Cerebrovasc Dis 2007;16:199–202 [DOI] [PubMed] [Google Scholar]
- 27. Pidcock M, Harrison P. Can the PFA-100 be modified to detect P2Y12 inhibition? J Thromb Haemost 2006;4:1424–26 [DOI] [PubMed] [Google Scholar]
- 28. Koessler J, Kobsar AL, Rajkovic MS, et al. The new INNOVANCE(R) PFA P2Y cartridge is sensitive to the detection of the P2Y receptor inhibition. Platelets 22:19–25 [DOI] [PubMed] [Google Scholar]
- 29. Varon D, Dardik R, Shenkman B, et al. A new method for quantitative analysis of whole blood platelet interaction with extracellular matrix under flow conditions. Thromb Res 1997;85:283–94 [DOI] [PubMed] [Google Scholar]
- 30. Varon D, Lashevski I, Brenner B, et al. Cone and plate(let) analyzer: monitoring glycoprotein IIb/IIIa antagonists and von Willebrand disease replacement therapy by testing platelet deposition under flow conditions. Am Heart J 1998;135:S187–93 [DOI] [PubMed] [Google Scholar]
- 31. Knobler H, Savion N, Shenkman B, et al. Shear-induced platelet adhesion and aggregation on subendothelium are increased in diabetic patients. Thromb Res 1998;90:181–90 [DOI] [PubMed] [Google Scholar]
- 32. Kenet G, Lubetsky A, Shenkman B, et al. Cone and platelet analyser (CPA): a new test for the prediction of bleeding among thrombocytopenic patients. Br J Haematol 1998;101:255–59 [DOI] [PubMed] [Google Scholar]
- 33. Shenkman B, Inbal A, Tamarin I, et al. Diagnosis of thrombotic thrombocytopenic purpura based on modulation by patient plasma of normal platelet adhesion under flow condition. Br J Haematol 2003;120:597–604 [DOI] [PubMed] [Google Scholar]
- 34. Savion N, Shenkman B, Tamarin I, et al. Transient adhesion refractoriness of circulating platelets under shear stress: the role of partial activation and microaggregate formation by suboptimal ADP concentration. Br J Haematol 2001;112:1055–61 [DOI] [PubMed] [Google Scholar]
- 35. Spectre G, Brill A, Gural A, et al. A new point-of-care method for monitoring anti-platelet therapy: application of the cone and plate(let) analyzer. Platelets 2005;16:293–99 [DOI] [PubMed] [Google Scholar]
- 36. Li CK, Hoffmann TJ, Hsieh PY, et al. The Xylum Clot Signature Analyzer: a dynamic flow system that simulates vascular injury. Thromb Res 1998;92:S67–77 [DOI] [PubMed] [Google Scholar]
- 37. Fricke W, Kouides P, Kessler C, et al. A multicenter clinical evaluation of the Clot Signature Analyzer. J Thromb Haemost 2004;2:763–68 [DOI] [PubMed] [Google Scholar]
- 38. Simon DI, Liu CB, Ganz P, et al. A comparative study of light transmission aggregometry and automated bedside platelet function assays in patients undergoing percutaneous coronary intervention and receiving abciximab, eptifibatide, or tirofiban. Catheter Cardiovasc Interv 2001;52:425–32 [DOI] [PubMed] [Google Scholar]
- 39. Harrison P. Platelet function analysis. Blood Rev 2005;19:111–23 [DOI] [PubMed] [Google Scholar]
- 40. Campbell J, Ridgway H, Carville D. Plateletworks: a novel point of care platelet function screen. Mol Diagn Ther 2008;12:253–58 [DOI] [PubMed] [Google Scholar]
- 41. Harle CC. Point-of-care platelet function testing. Semin Cardiothorac Vasc Anesth 2007;11:247–51 [DOI] [PubMed] [Google Scholar]
- 42. Gremmel T, Steiner S, Seidinger D, et al. Comparison of methods to evaluate clopidogrel-mediated platelet inhibition after percutaneous intervention with stent implantation. Thromb Haemost 2009;101:333–39 [PubMed] [Google Scholar]
- 43. Breet NJ, van Werkum JW, Bouman HJ, et al. Comparison of platelet function tests in predicting clinical outcome in patients undergoing coronary stent implantation. JAMA 2010;303:754–62 [DOI] [PubMed] [Google Scholar]
- 44. Braunwald E, Angiolillo D, Bates E, et al. Antiplatelet therapy and platelet function testing: introduction. Clin Cardiol 2008;31(3 supple 1):I1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Mukherjee D, Chew DP, Robbins M, et al. Clinical application of procedural platelet monitoring during percutaneous coronary intervention among patients at increased bleeding risk. J Thromb Thrombolysis 2001;11:151–54 [DOI] [PubMed] [Google Scholar]
- 46. Jacopo G, Elisabetta V, Silverio S, et al. Identification of platelet hyper-reactivity measured with a portable device immediately after percutaneous coronary intervention predicts in stent thrombosis. Thromb Res 2007;121:407–12 [DOI] [PubMed] [Google Scholar]
- 47. Chen WH, Lee PY, Ng W, et al. Aspirin resistance is associated with a high incidence of myonecrosis after non-urgent percutaneous coronary intervention despite clopidogrel pretreatment. J Am Coll Cardiol 2004;43:1122–26 [DOI] [PubMed] [Google Scholar]
- 48. Buch AN, Singh S, Roy P, et al. Measuring aspirin resistance, clopidogrel responsiveness, and postprocedural markers of myonecrosis in patients undergoing percutaneous coronary intervention. J Am Coll Cardiol 2007;99:1518–22 [DOI] [PubMed] [Google Scholar]
- 49. Gulmez O, Yildirir A, Kaynar G, et al. Effects of persistent platelet reactivity despite aspirin therapy on cardiac troponin I and creatine kinase-MB levels after elective percutaneous coronary interventions. J Thromb Thrombolysis 2008;25:239–46 [DOI] [PubMed] [Google Scholar]
- 50. Buonamici P, Marcucci R, Migliorini A, et al. Impact of platelet reactivity after clopidogrel administration on drug-eluting stent thrombosis. J Am Coll Cardiol 2007;49:2312–17 [DOI] [PubMed] [Google Scholar]
- 51. Pinto Slottow TL, Bonello L, Gavini R, et al. Prevalence of aspirin and clopidogrel resistance among patients with and without drug-eluting stent thrombosis. Am J Cardiol 2009;104:525–30 [DOI] [PubMed] [Google Scholar]
- 52. Price MJ, Berger PB, Teirstein PS, et al. Standard- vs high-dose clopidogrel based on platelet function testing after percutaneous coronary intervention: the GRAVITAS randomized trial. JAMA 2011;305:1097–105 [DOI] [PubMed] [Google Scholar]
- 53. Price MJ, Angiolillo DJ, Teirstein PS, et al. Platelet reactivity and cardiovascular outcomes after percutaneous coronary intervention. A time-dependent analysis of the gauging responsiveness with a VerifyNow P2Y12 assay: impact on thrombosis and safety (GRAVITAS) trial. Circulation 2011:124:1132–7 [DOI] [PubMed] [Google Scholar]
- 54. Eshtehardi P, Windecker S, Cook S, et al. Dual low response to acetylsalicylic acid and clopidogrel is associated with myonecrosis and stent thrombosis after coronary stent implantation. Am Heart J 2010;159:891–98 e1 [DOI] [PubMed] [Google Scholar]
- 55. Gori AM, Marcucci R, Migliorini A, et al. Incidence and clinical impact of dual nonresponsiveness to aspirin and clopidogrel in patients with drug-eluting stents. J Am Coll Cardiol 2008;52:734–39 [DOI] [PubMed] [Google Scholar]
- 56. Tavassoli N, Voisin S, Carrie D, et al. High maintenance dosage of clopidogrel is associated with a reduced risk of stent thrombosis in clopidogrel-resistant patients. Am J Cardiovasc Drugs 2010;10:29–35 [DOI] [PubMed] [Google Scholar]
- 57. Han Y, Li Y, Wang S, et al. Cilostazol in addition to aspirin and clopidogrel improves long-term outcomes after percutaneous coronary intervention in patients with acute coronary syndromes: a randomized, controlled study. Am Heart J 2009;157:733–39 [DOI] [PubMed] [Google Scholar]
- 58. Chen KY, Rha SW, Li YJ, et al. Triple versus dual antiplatelet therapy in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Circulation 2009;119:3207–14 [DOI] [PubMed] [Google Scholar]
- 59. Sibbing D, Schulz S, Braun S, et al. Antiplatelet effects of clopidogrel and bleeding in patients undergoing coronary stent placement. J Thromb Haemost 2010;8:250–56 [DOI] [PubMed] [Google Scholar]
- 60. Pandya DJ, Fitzsimmons BF, Wolfe TJ, et al. Measurement of antiplatelet inhibition during neurointerventional procedures: the effect of antithrombotic duration and loading dose. J Neuroimaging 2010;20:64–69 [DOI] [PubMed] [Google Scholar]
- 61. Lee DH, Arat A, Morsi H, et al. Dual antiplatelet therapy monitoring for neurointerventional procedures using a point-of-care platelet function test: a single-center experience. AJNR Am J Neuroradiol 2008;29:1389–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Qureshi AI, Siddiqui AM, Hanel RA, et al. Safety of high-dose intravenous eptifibatide as an adjunct to internal carotid artery angioplasty and stent placement: a prospective registry. Neurosurgery 2004;54:307–16, discussion 316–17 [DOI] [PubMed] [Google Scholar]