Abstract
BACKGROUND AND PURPOSE:
Wide-neck intracranial aneurysms in patients with acute SAH are often challenging lesions to treat by neurosurgical and endovascular approaches. The aim of this study was to investigate the feasibility, safety, and efficacy of the use of temporary Solitaire AB stent–assisted technique with coiling for the treatment of acutely ruptured wide-neck aneurysms without perioperative antiplatelet therapy.
MATERIALS AND METHODS:
A retrospective review of our endovascular data base identified all patients treated in the acute phase with a temporary stent–assisted technique by use of a fully resheathable Solitaire AB stent and coiling. One-year clinical and angiographic outcomes were evaluated.
RESULTS:
Eight patients (5 women and 3 men; mean age, 57.5 years) with 8 ruptured wide-neck aneurysms were treated. There were 3 complications without clinical impact. Postoperative complete occlusion was achieved in 5 aneurysms, and 3 had a neck remnant. Three patients had an mRS score of 0, and 1 an mRS score of 3. Among the 4 patients admitted with a World Federation of Neurological Societies grade of V, 1 died, 1 improved to an mRS score of 1, and the other 2 achieved mRS scores of 4 and 5. Five had a stable occlusion, and 2 of the 3 incompletely occluded aneurysms underwent recanalization.
CONCLUSIONS:
In this small series, temporary placement of the Solitaire AB stent during coiling was a feasible and effective treatment for acutely ruptured wide-neck aneurysms. This technique, avoiding the need for perioperative antiplatelet therapy, could be a valuable option for the treatment of such lesions when the balloon remodeling technique is either not an option or unsuccessful.
Endovascular treatment of ruptured intracranial aneurysms is an established technique,1 but it can be technically challenging when the neck is large. Numerous devices, including remodeling balloons2–4 and stents,5 have been developed to assist the endovascular treatment of wide-neck aneurysms. However, such techniques carry a great risk of hemorrhagic complications if they are applied in the acute phase of SAH because of the need for dual antiplatelet therapy.6,7 In the recent review of acutely ruptured aneurysms treated with stent-assisted coiling (SAC) performed by Bodily et al,7 clinically significant intracranial hemorrhagic complications occurred in 27 (8%) of 339 patients, including 9 (10%) of 90 patients known to have external ventricular drains (EVDs) who had ventricular drain–related hemorrhages.
To avoid the use of antiplatelet therapy in patients with acute SAH, the technique of temporary stent–assisted neck remodeling has been reported with the Enterprise stent (Codman & Shurtleff, Raynham, Massachusetts)8 and recently with the support of the Solitaire AB stent (Covidien, Irvine, California) in 3 cases.9 However, all patients received aspirin before the procedure, and 1 of 3 patients required antiplatelet therapy after the intervention.9 The aim of this study was to investigate the feasibility, safety, and efficacy of the use of temporary Solitaire AB SAC for the treatment of acutely ruptured wide-neck aneurysms without perioperative antiplatelet therapy.
MATERIALS AND METHODS
The institutional review board of our hospital approved this study. A retrospective review of our data base identified all patients treated in the acute phase with a temporary stent–assisted technique by use of a fully resheathable Solitaire AB stent and coiling from April 2008 to December 2008. Patients presented with a ruptured aneurysm in the acute phase (≤72 hours) of SAH; a neck size of ≤4 mm and/or a dome-to-neck ratio of ≤1.0; and unfavorable anatomy, causing the balloon remodeling technique to be unsuccessful or unfeasible as the sole technique for supporting the coil mass. Patients were included with agreement of the treating neurosurgeon.
Characteristics of the Solitaire AB Stent
The Solitaire AB stent is a fully deployable and retrievable device that self-expands when the delivery microcatheter is withdrawn.10 Its distal markers clearly show its position inside the artery at all times and in different projections. Its closed cell design and high cell deformation resistance provide flexibility and scaffolding to prevent coil herniation into the parent vessel. Moreover, it is provided with a system that allows for its retrieval.
Treatment Technique
All procedures were performed with the patient under general anesthesia and systemic heparinization (80 IU/kg). No antiplatelet therapy was given. A bilateral femoral approach by use of 6F or 8F guiding catheters was undertaken. One guiding catheter was used for the stent microcatheter (Prowler Select Plus, Codman & Shurtleff), and the other was used for the coil microcatheters (Echelon 14, Covidien and Prowler 14, Codman & Shurtleff). Coiling was achieved by a jailing technique with the use of a fully retrievable 4 × 20-mm stent, the Solitaire AB. The placement of the undetached stent was performed after microcatheter placement in the sac, and the neck was sufficiently covered in 6 patients. In the other 2 patients, a complementary balloon remodeling technique was used (HyperForm; Covidien) to prevent the coil from migrating distally into nearby arteries. In these 2 patients, the coil microcatheter and balloon were placed through the same guiding catheter. After packing of the aneurysm, the stent was retrieved by pushing the microcatheter and resheathing the stent, not by pulling the stent back.
Outcome Evaluation
Clinical outcome was assessed by means of the mRS at discharge; at 3, 6, and 12 months; and yearly thereafter (F.T.).11
Occlusion of the aneurysm was assessed angiographically at the end of the intervention, and at 3- and 12-month follow-up (F.T.). It was defined by use of the simplified 3-point Raymond classification scale: complete occlusion, neck remnant, and aneurysm remnant.12 Recanalization was defined as a worsening of classification: complete occlusion to neck remnant, neck remnant to aneurysm remnant, or complete occlusion to aneurysm remnant.
RESULTS
Eight patients (5 women, 3 men; mean age, 57.5 years) with 8 aneurysms were treated with the temporary Solitaire AB SAC technique. Initial clinical features are summarized in Table 1. Among the 8 patients, 1 patient also presented with a bilateral subdural hematoma and 1 patient bled twice before treatment. Four patients were in good clinical condition (World Federation of Neurological Societies [WFNS] grade I) and 4 were in poor clinical condition (WFNS grade V). One patient with poor grade improved to grade III soon after EVD placement before embolization.
Table 1:
Clinical and angiographic features
| Patient | Sex/Age, y | Fisher Score | WFNS Grade | Aneurysm Location | Sac Size, mm | Neck Size, mm | Complementary Technique |
|---|---|---|---|---|---|---|---|
| 1 | Male/55 | II | I | AcomA | 4 × 2.5 | 4 | RB |
| 2 | Male/51 | III | V | Medium-basilar | 21 × 13 | 8 | |
| 3 | Female/58 | IV | V | Right carotido-ophthalmic | 12 × 10 | 6 | |
| 4 | Female/77 | II | I | Vertebrobasilar junction | 9 × 10 | 10 | |
| 5 | Female/43 | IV | I | Left PcomA | 4 × 3.5 | 3.5 | |
| 6 | Female/81 | IV | I | Left PcomA | 3 × 2.5 | 3 | |
| 7 | Female/52 | III | Va | Right MCA | 10 × 5 | 5 | RB |
| 8 | Male/43 | IV | V | Left PcomA | 22 × 16 | 7 |
Note:—AcomA indicates anterior communicating artery; RB, remodeling balloon; PcomA, posterior communicating artery.
WFNS grade improved to III after EVD placement.
The mean aneurysm width was 10.6 mm (range, 3–22 mm), mean height of the sac 7.8 mm (range, 2.5–16 mm), and mean diameter of the neck was 5.8 mm (range, 3–10 mm) (Table 1).
Most aneurysms (75%) were located in the anterior circulation. Aneurysm locations are summarized in Table 1. All patients were treated successfully with the use of this technique. Placement of the undetached stent was easily performed and sufficiently covered the aneurysm neck in 6 patients, whereas concomitant balloon placement was required in 2 patients to protect a branch from distal coil migration (patients 1 and 7). The coil position was stable during and after stent retrieval in all patients.
Procedural Complications
One perforation of the aneurysm sac occurred during coil placement without clinical consequence (patient 5, mRS 0). One thromboembolic adverse event occurred during inflation of the balloon in the inferior MCA branch, which resulted in no clinical disability (patient 7, mRS 1). In another patient, premature detachment of 1 coil resulted in the placement of a portion of the coil in the basilar artery (patient 2, mRS 4). We did not retrieve the migrated coil because the free coil strand was stable in the basilar artery and did not cause distal flow reduction. Stent retrieval was uneventful.
Clinical Outcomes
Clinical outcomes are summarized in Table 2. Favorable outcome (mRS ≤2) was observed in 4 patients (50%). Among the 4 patients admitted with a WFNS grade of V, 1 died, 2 achieved mRS scores of 4 and 5 at discharge, respectively, and did not subsequently improve, and 1 improved to an mRS score of 1. Four patients required EVD placement after (and 1 before) SAC.
Table 2:
Clinical and angiographic outcomes
| Patient | mRS Score at Discharge | Aneurysmal Occlusion/Initial 1-Year Follow-Up | Further Treatment |
|---|---|---|---|
| 1 | 0 | Complete/Complete | None |
| 2 | 4 | Complete/Complete | None |
| 3 | 5 | Neck remnant/Neck remnant | None |
| 4 | 0 | Neck remnant/Recanalization | SAC (complete occlusion) |
| 5 | 0 | Complete/Complete | None |
| 6 | 3 | Neck remnant/Recanalization | SAC (complete occlusion) |
| 7 | 1 | Complete/Complete | None |
| 8 | 6 | Complete/Complete | None |
Angiographic Outcomes
Angiographic outcomes are summarized in Table 2. Postoperative angiographic results were the following: complete occlusion, 5 aneurysms (62.5%); and neck remnant, 3 aneurysms (37.5%). At 1-year follow-up, 2 of 3 patients showed recanalization and were treated electively with definitive stent placement, whereas 1 incomplete occlusion remained stable and was not treated because of the patient's persistent vegetative state.
Illustrative Cases
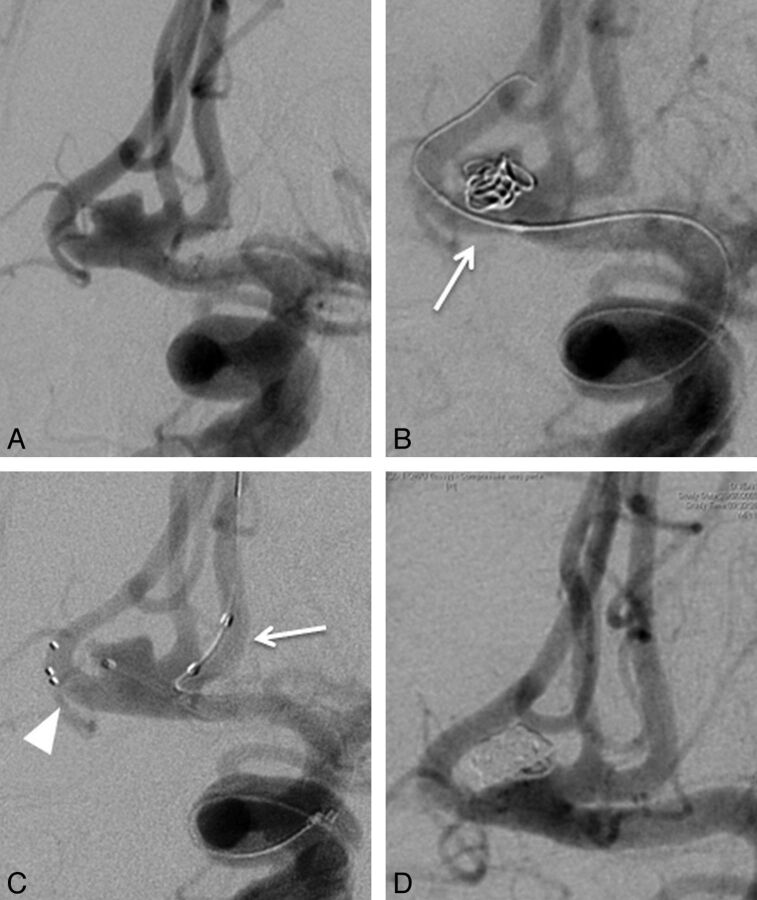
Case 1.
A 55-year-old man (patient 1) presented with severe headaches and mild confusion (WFNS grade I). CT demonstrated SAH and bilateral subdural hematomas. The angiogram revealed an aneurysm of the anterior communicating artery associated with the median artery of the corpus callosum (Fig 1A). The broad-based aneurysm (dome, 4 × 2.5 mm; neck size, 4 mm) was impossible to coil by the conventional technique because the coils did not remain within the aneurysm, even with the balloon-assisted technique (Fig 1B). In the same setting, a 4 × 20-mm self-expanding Solitaire AB stent was placed but not detached in the left A1 and right A2 segments from the left. Coil implantation again resulted in coil herniation in the left A2. Thus, the stent was retrieved, a HyperForm balloon, 4 × 7 mm, was placed in the left A2, the stent was deployed again in the left A1–right A2 (Fig 1C), and 5 detachable coils were introduced. The balloon and then the stent were retrieved. The postprocedural angiogram demonstrated complete occlusion of the aneurysm (Fig 1D). Clinical examination at discharge and at 3- and 12-month follow-up revealed no neurologic deficits and an mRS score of 0.
Fig 1.
A 55-year-old man (patient 1) with a ruptured anterior communicating artery (AcomA) aneurysm. A, Initial angiogram shows a wide-neck AcomA aneurysm associated with the median artery of the corpus callosum. B, Balloon is positioned across the aneurysm neck and the first coil is inserted into the aneurysm with the balloon inflated. The first coil prolapses into the right A2 when the balloon is deflated (arrow). C, The deployed but undetached stent is positioned in the left A1 and right A2 segments from the left (arrowhead); the balloon is placed in the left A2 (arrow) and the microcatheter into the aneurysmal sac. D, Postprocedural angiogram demonstrates complete aneurysm occlusion after stent retrieval.
Case 2.
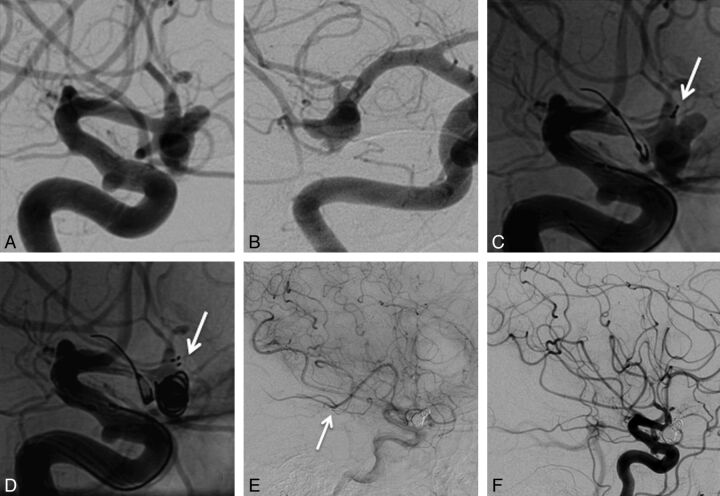
A 52-year-old woman (patient 7) was admitted with a WFNS grade V SAH from a right bilobed, broad-based (dome, 10 × 5 mm; neck size, 5 mm) MCA bifurcation aneurysm (Fig 2A, -B). The patient had an additional paraophthalmic aneurysm, considered unruptured given its small size. Her WFNS grade improved to III after EVD placement. Embolization was carried out immediately thereafter. First, a HyperForm balloon, 4 × 7 mm, was placed to protect the inferior trunk from coil migration, and the undeployed stent was positioned across the superior trunk. The coil microcatheter was then positioned in the aneurysmal sac through the same guiding catheter as that used for the remodeling balloon, and the stent was deployed (Fig 2C). A vasospasm was observed in the stented artery. Aneurysm packing was then performed (Fig 2D), and the stent and balloon were retrieved. A thromboembolic adverse event was noted at the end of the procedure in the inferior MCA branch (Fig 2E, -F), without ischemic complications on the postoperative CT scan. At the 1-year follow-up, the patient had an mRS score of 1 and had resumed all previous activities.
Fig 2.
A 52-year-old woman (patient 7) with a complex MCA aneurysm. A and B, Initial angiogram shows a broad-based, bilobed MCA bifurcation aneurysm. An additional paraophthalmic aneurysm is noted. C, The undeployed stent is positioned across the superior trunk (arrow) and the balloon placed to protect the inferior trunk from coil migration. A vasospasm in the superior division of MCA was observed. D, The stent is deployed (arrow), and aneurysm packing is performed. The distal stent markers appear to be outside the vessel wall, an appearance that is related to vasospasm. E and F, A thromboembolic adverse event occurred during inflation of the balloon in the inferior MCA branch, which resulted in no clinical disability.
DISCUSSION
Since the advent of self-expandable stents, SAC is a commonly adopted technique used in the coiling of wide-neck aneurysms.5 In these cases, the most important function of the stent is to prevent herniation of coils into the parent artery.13,14 However, perioperative antiplatelet treatment is mandatory to prevent in-stent thrombosis, which is a major concern in patients with acute SAH.6,7,15 For this reason, stent placement is generally used only as a rescue technique in acutely ruptured aneurysms. In a recent systematic review of 339 patients with ruptured aneurysms who were treated acutely with SAC, clinically significant intracranial hemorrhagic complications occurred in 8% and clinically significant thromboembolic events occurred in 6%.7
The technique of temporary stent–assisted neck remodeling has been reported with the Enterprise stent8 and recently with the Solitaire AB stent.9 Contrary to a series by Almekhlafi et al,9 we did not use antiplatelet therapy; thus theoretically reducing the risk of hemorrhagic complications linked to intraprocedural rupture of the aneurysm and to subsequent surgical interventions to treat intracranial hypertension such as EVD placement or decompressive craniectomy.16 In our series, 4 of the 8 patients underwent emergent EVD placement, and no hemorrhagic complication was noted. Moreover, 1 patient had an intraoperative aneurysm rupture that was successfully managed by coil packing. The other concern with this technique is the patency of the stented parent artery during the deployment of the stent. In 1 of our 8 cases, there was an intraprocedural thromboembolic complication. This event occurred in the inferior branch of the MCA in which the balloon was inflated with no clinical impact.
The risk of entanglement of the coils was perceived as the major risk of this technique. After placement of a coil in contact with the stent, the latter was partially resheathed to assess this possibility. If the stent moved freely, the coil detachment was decided. After completing the coiling of the aneurysm, the stent was carefully completely resheathed to reduce the risk of endothelium damage and of subsequent vasospasm.
The balloon remodeling technique is the other option applicable to treat wide-neck aneurysms2–4; it had a higher rate of adequate postoperative occlusion than did standard coiling with comparable safety17 and had the advantage to overcome antiplatelet therapy. However, in our case series, we focused on wide-neck intracranial aneurysms in which the balloon remodeling technique had failed (patients 1 and 7) or was thought technically challenging because of the difficulty of navigating the balloon across the aneurysm neck. The Solitaire AB stent is a highly flexible device that easily conforms to vessel tortuosity and caliber variations because of its flexibility, which is not reduced by the closed cell design that offers a high outward radial force. Thus, the Solitaire AB efficiently accommodates curved and tapered vessels, bridging the aneurysm neck with virtually no limits in width and supporting the vessel lumen by avoiding recoil of coils.10 There was no coil prolapse or herniation into the parent vessel during or after stent retrieval. Another advantage of this technique is the avoidance of anterograde flow arrest associated with repeated balloon inflations, which may cause ischemic stroke, given its reduced tolerance to ischemia in the setting of acute SAH.5,18 Furthermore, balloon inflation may be associated with thromboembolic complications, especially when the parent artery diameter is small as in the illustrative case 2 of our series (patient 7).
Although this study has several limitations, including its retrospective nature, a relatively small number of cases, and limited follow-up duration, temporary SAC by use of the Solitaire AB stent has acceptable rates of technical failure and appears to be safe. Except for 1 case of asymptomatic vasospasm, there were no device-related adverse events, and the clinical outcome was favorable in 4 of 8 patients, whereas it was negatively affected by the clinical course of SAH in the other 4 patients. No rebleeding occurred during the observation period.
Complete aneurysm occlusion was achieved in most cases (62.5%); this suggests that this new technique could be an effective treatment. Although all aneurysms included in this series were ruptured, the recurrence rate is in line with the results of the systematic review of 7865 aneurysms coiled as performed by Ferns et al.19
CONCLUSIONS
Our preliminary experience with temporary SAC by use of the Solitaire AB stent suggests that it is a feasible, safe, and effective treatment alternative for wide-neck aneurysms in the setting of SAH when the balloon remodeling technique is either not an option or unsuccessful.
ABBREVIATIONS:
- EVD
external ventricular drain
- SAC
stent-assisted coiling
- WFNS
World Federation of Neurological Societies
Footnotes
Disclosures: Francis Turjman—RELATED: Support for Travel to Meetings for the Study or Other Purposes: Covidien; UNRELATED: Consultancy: Codman; Payment for Lectures (including service on speakers bureaus): Codman; Payment for Development of Educational Presentations: Codman, Balt, Covidien; Travel/Accommodations/Meeting Expenses Unrelated to Activities Listed: Codman, Covidien.
REFERENCES
- 1. Li H, Pan R, Wang H, et al. Clipping versus coiling for ruptured intracranial aneurysms: a systematic review and meta-analysis. Stroke 2013;44:29–37 [DOI] [PubMed] [Google Scholar]
- 2. Moret J, Cognard C, Weill A, et al. The “remodeling technique” in the treatment of wide neck intracranial aneurysms. Intervent Neuroradiol 1997;3:21–35 [DOI] [PubMed] [Google Scholar]
- 3. Pierot L, Cognard C, Spelle L, et al. Safety and efficacy of balloon remodeling technique during endovascular treatment of intracranial aneurysms: critical review of the literature. AJNR Am J Neuroradiol 2012;33:12–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gory B, Kessler I, Seizem Nekiri G, et al. Initial experience of intracranial aneurysm embolization using the balloon remodeling technique with Scepter C, a new double-lumen balloon. Intervent Neuroradiol 2012;18:284–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Shapiro M, Becske T, Sahlein D, et al. Stent-supported aneurysm coiling: a literature survey of treatment and follow-up. AJNR Am J Neuroradiol 2012;33:159–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tahtinen OI, Vanninen RL, Manninen HI, et al. Wide-necked intracranial aneurysms: treatment with stent-assisted coil embolization during acute (<72 hours) subarachnoid hemorrhage: experience in 61 consecutive patients. Radiology 2009;253:199–208 [DOI] [PubMed] [Google Scholar]
- 7. Bodily KD, Cloft HJ, Lanzino G, et al. Stent-assisted coiling in acutely ruptured intracranial aneurysms: a qualitative, systematic review of the literature. AJNR Am J Neuroradiol 2011;32:1232–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Byun JS, Kim JK, Lee HY, et al. Temporary semi-jailing technique for coil embolization of wide-neck aneurysm with small caliber parent artery following incomplete clipping. J Korean Neurosurg Soc 2013;53:241–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Almekhlafi MA, Hockley A, Wong JH, et al. Temporary Solitaire stent neck remodeling in the coiling of ruptured aneurysms. J Neurointerv Surg 2013;5(Suppl 3):iii76–78 [DOI] [PubMed] [Google Scholar]
- 10. Henkes H, Flesser A, Brew S, et al. A novel microcatheter-delivered, highly-flexible and fully-retrievable stent, specifically designed for intracranial use. Intervent Neuroradiol 2003;9:391–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. van Swieten JC, Koudstaal PJ, Visser MC, et al. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988;19:604–07 [DOI] [PubMed] [Google Scholar]
- 12. Raymond J, Guilbert F, Weill A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke 2003;34:1398–403 [DOI] [PubMed] [Google Scholar]
- 13. Piotin M, Blanc R, Spelle L, et al. Stent-assisted coiling of intracranial aneurysms: clinical and angiographic results in 216 consecutive aneurysms. Stroke 2010;41:110–15 [DOI] [PubMed] [Google Scholar]
- 14. Maldonado IL, Machi P, Costalat V, et al. Neuroform stent-assisted coiling of unruptured intracranial aneurysms: short- and midterm results from a single-center experience with 68 patients. AJNR Am J Neuroradiol 2011;32:131–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mahaney KB, Chalouhi N, Viljoen S, et al. Risk of hemorrhagic complication associated with ventriculoperitoneal shunt placement in aneurysmal subarachnoid hemorrhage patients on dual antiplatelet therapy. J Neurosurg 2013;119:937–42 [DOI] [PubMed] [Google Scholar]
- 16. Kung DK, Policeni BA, Capuano AW, et al. Risk of ventriculostomy-related hemorrhage in patients with acutely ruptured aneurysms treated using stent-assisted coiling. J Neurosurg 2011;114:1021–27 [DOI] [PubMed] [Google Scholar]
- 17. Pierot L, Cognard C, Anxionnat R, et al. Remodeling technique for endovascular treatment of ruptured intracranial aneurysms had a higher rate of adequate postoperative occlusion than did conventional coil embolization with comparable safety. Radiology 2011;258:546–53 [DOI] [PubMed] [Google Scholar]
- 18. Sluzewski M, van Rooij WJ, Beute GN, et al. Balloon-assisted coil embolization of intracranial aneurysms: incidence, complications, and angiography results. J Neurosurg 2006;105:396–99 [DOI] [PubMed] [Google Scholar]
- 19. Ferns SP, Sprengers ME, van Rooij WJ, et al. Coiling of intracranial aneurysms: a systematic review on initial occlusion and reopening and retreatment rates. Stroke 2009;40:523–29 [DOI] [PubMed] [Google Scholar]