Abstract
BACKGROUND AND PURPOSE:
Our research focuses on interventional neuroradiology (stroke treatment including imaging methods) and general neuroimaging with an emphasis on functional MR imaging. Our aim was to determine the efficacy of revascularization (TIMI) of middle cerebral and/or carotid artery occlusion by means of mechanical recanalization techniques and to evaluate the impact of collateralization, mismatch in perfusion CT, time to revascularization, grade of revascularization on tissue, and clinical outcome in patients with acute ischemic stroke.
MATERIALS AND METHODS:
Thirty-one patients with MCA and/or ICA occlusion were included. Ischemic stroke was diagnosed by NECT, CTA, and volume PCT for grading collateralization and mismatch. Time to recanalization was measured from the onset of stroke to the time point of DSA-proved mechanical recanalization. Tissue outcome was calculated by segmentation of infarct size between pre- and postinterventional CT and percentage mismatch lost. Clinical outcome was determined by the mRS.
RESULTS:
Twenty-one of 31 patients (61.8%) presented with MCA and 10/31 patients (38.2%), with distal ICA occlusions. Sufficient recanalization (TIMI 2 and 3) was achieved in 23/31 (75%). Clinical evaluation revealed an mRS score of ≤2 in 25.5%. Age (r = 0.439, P = .038) and TIMI (r = 0.544, P = .002) showed the strongest correlation with clinical outcome. Time to recanalization, TIMI score, and mismatch were associated with a good tissue outcome in ANOVA.
CONCLUSIONS:
Favorable outcome after mechanical recanalization of acute MCA and ICA occlusion depends on time to and grade of recanalization, mismatch, and collateralization. These results indicate that multimodal stroke imaging is helpful to guide therapy decisions and to indicate patients amenable for mechanical recanalization.
Effective stroke therapy remains one of the most important tasks for neurologic and neuroradiologic patient care, because stroke represents one of the most frequent causes of mortality in the Western countries.
Recently, mechanical devices have been developed and implemented and play an increasing role in endovascular stroke therapy. Mechanical thrombectomy can improve the outcome of patients with stroke. Recanalization time and TIMI grade may be superior to approaches based on systemic thrombolysis alone, especially in the case of large-vessel occlusion.1 First results of the MERCI trial (Concentric Medical, Mountain View, California) and trials using the Penumbra system (Penumbra, Alameda, California) and Phenox clot retriever (Phenox, Bochum, Germany) reported recanalization rates (TIMI 2 or 3) ranging from 53% (MERCI) to 92.2%–100% (Penumbra).2–4 A newly published study showed a recanalization rate of 90% by using a retrievable stent device (Solitaire; ev3, Irvine, California).5
In addition, improved neuroimaging technologies in acute stroke care have been implemented with the development of diffusion-weighted MR imaging and CECT in combination with PCT. Whole-brain analysis can be performed providing imaging parameters on perfusion and mismatch, which could be used for the selection of advanced therapeutic procedures based on mechanical recanalization.6,7
Besides the presence of mismatch and collateralization, the time from onset of symptoms to recanalization is regarded as one of the key factors for good clinical outcome, with an increasing time span (several hours) to recanalization decreasing the chances of success for the rescue of tissue at risk.8,9 In a multivariate analysis to identify patients with high risk for a poor outcome, Hallevi et al10 found no significant influence of the duration between symptom onset and recanalization, but there was an influence for recanalization grade, extent of mismatch, and duration of the interventional procedure. Thus CT- or MR imaging−based concepts with defined thresholds may help to identify salvageable tissue independently from the duration of symptoms and to establish a physiology-based image-guided approach to performing modern stroke therapy.11–13
The aim of our study was to evaluate the impact of mechanical recanalization on clinical and tissue outcome of patients with acute stroke. We assessed initial image-based parameters for decision-making in patients who are suitable for mechanical recanalization, by evaluating the extent of final infarction and clinical outcome as measured by the mRS in relation to time from symptom onset to recanalization, recanalization grade, presence of mismatch and collateralization, and patient age.
Materials and Methods
Patients with acute ischemic stroke admitted to the Stroke Unit of the University Hospital Münster (certified by the German Stroke Society) within a 6-hour time window after onset of symptoms were investigated between April 2008 and July 2009. In this time period, 899 patients were treated with symptoms of acute stroke, and 90 patients received intravenous application of rtPA. Seventy-five patients were not included in interventional treatment due to time delay to admission, patient consent, comorbidities. and size of demarcated infarction. Thirty-one patients with proximal cerebral artery occlusions were considered for interventional treatment, with 21/31 occlusions of the MCA and 10/31 of the ICA (17 [54.8%] men, 14 [45.2%] women; age range, 18–83 years; mean age, 68.8 years). mRS was documented at the time of admission. All patients presented with the typical clinical signs of an ischemic infarct in the right (n = 24) or left (n = 7) MCA territory with contralateral hemiparesis. The present study can be regarded as a retrospective analysis of a case series, in which the procedures have been defined in a prospective manner (prospective clinical observational study since April 2008).
Inclusion and Exclusion Criteria
Inclusion criteria of the study were the following: 1) admission to the stroke unit within 6 hours after symptom onset, 2) initial NIHSS score of 6 or worse, 3) CT-proved proximal cerebral artery occlusion in the anterior circulation with persisting occlusion on DSA (all patients), and 4) no or limited (less than one-third of the MCA territory) infarct demarcation on initial CT. All patients meeting these criteria were taken to the DSA unit and received immediate general anesthesia and mechanical recanalization.
Exclusion criteria were the following: 1) admission to the stroke unit later than 6 hours, 2) demarcation of infarct in NECT of more than one-third of the territory of the MCA, 3) contraindications against general anesthesia, 4) an M2 occlusion on CTA, 5) an NIHSS score below 6, and 6) a vanished thrombotic occlusion on later DSA (not observed).
CT Protocol
NECT.
NECT was performed by using a standard protocol (120 kV; 340 mAs; collimation, 2 × 20 × 0.6 mm). Images were reconstructed with a section thickness of 5.0 mm and no overlap by using a medium-sharp convolution kernel (H30f). This scan was performed immediately after admission and within 24 hours after treatment. Timing and scanning parameters of the follow-up scan were similar to those of the first one.
Perfusion CECT.
For perfusion CT, the neurocranium was scanned repetitively after the injection of 30 mL of contrast medium with a flow of 6 mL/s by using a 128-section scanner (Definition AS+; Siemens Healthcare, Forchheim, Germany) with the following parameters: 80 kV; 200 mAs; collimation, 2 × 64 × 0.6 mm. A range of 96 mm from the skull base to the top of the calvaria was covered with a temporal increment of 1.25 seconds for 50 seconds. From these data, the cerebral volume perfusion was calculated. Perfusion datasets were reconstructed with section thicknesses of 1.5, 5.0, and 10 mm by using a soft convolution kernel (H20f).
After the perfusion CT, a CTA from the aortic arch to the superior sagittal sinus was obtained after the injection of 80 mL of contrast at a flow rate of 4 mL/s. Scan parameters were the following: 120 kV; 175 mAs; collimation, 2 × 64 × 0.6 mm. Images were reconstructed with a section thickness of 1.0 and an increment of 0.7 mm by using a soft convolution kernel (H20f).
Multimodal stroke CT, including NECT, CTA, and PCT, was performed immediately. All 31 patients were subjected to general anesthesia to undergo mechanical recanalization therapy. Twenty milligrams of rtPA was administered intravenously immediately after CT imaging according to the bridging concept. The DSA was used to confirm the CT diagnosis in advance immediately before intervention.
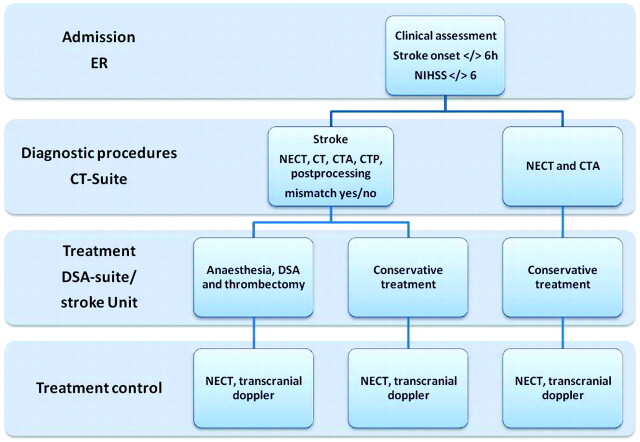
The perfusion data were calculated by using the VPCT-Neuro program on a separate workstation (Siemens Healthcare). rCBV, relative cerebral blood flow, and time-to-peak maps were calculated after semiautomatically estimating the arterial (anterior cerebral artery) and venous input functions (superior sagittal sinus). The evaluation of tissue outcome included the calculation of the volume of tissue loss (infarct growth) and the percentage mismatch lost. The infarct growth was measured as the difference of volume of the demarcated infarct on pre- and postinterventional NECT images. Volumes were determined by segmenting ischemic lesions on a section-by-section basis (Analyze 9.0; AnalyzeDirect, Overland Park, Kansas). The volume of tissue at risk of infarct was defined as the difference of the volume of total ischemia (elevated MTT) and the initial infarct core (significantly low CBV) on PCT maps by using published thresholds (Fig 1A, -B).14 Lesion volume of the infarct core on the CBV maps and total volume of ischemia on the MTT maps were segmented semiautomatically on a section-by-section basis with a window level set at the corresponding threshold and manual adjustment of window width (Fig 1C) (Analyze 9.0). The relative volume of postinterventional final infarct size was determined by using the NECT lesion map coregistered to the PCT images within a 24-hour time window (Fig 1D). The percentage of mismatch lost (percentage of tissue at risk loss) after the intervention was calculated as follows: 100 × [volume (final infarct) − volume (initial infarct core)] / volume (tissue at risk).
Fig 1.
A and B, MTT and rCBV maps for estimating the extent of penumbra and the infarct core. C, The difference in size of the infarct core and penumbra. D, The final infarct as shown with NECT and the mismatch lost in percentages are calculated by Analyze software.
Twenty patients were treated with the Penumbra system; 6 patients, with the Phenox clot retriever, and in 5 patients, additional recanalization methods were used (stent angioplasty, n = 4; balloon angioplasty, n = 1). The outcome of intervention was documented by angiography as well as duplex sonography at follow-up. For evaluation of clinical outcome, mRS was documented after 3 months.
All patients were examined by experienced neurologists being responsible for admission and surveillance of patients with stroke on a certified stroke unit. All patients were investigated with regard to initial NIHSS and mRS scores. The time window of symptom onset was below 3 hours in 19 patients and 6 hours in 11 patients. Patients with an NIHSS score of ≤6 and a time window of ≤6 hours from symptom onset were included in the study.
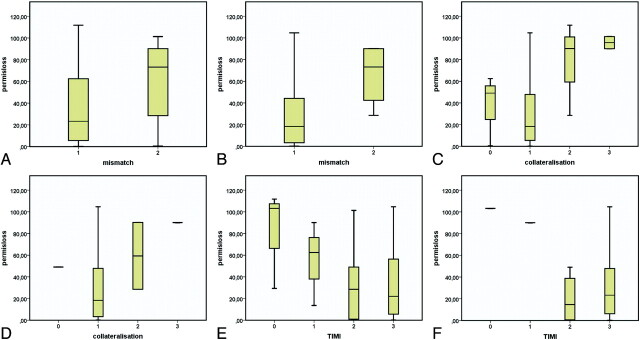
After DSA-proved recanalization of the proximal vessel with remaining distal thrombi, rtPA was given to a maximum dose as stated above. The grade of recanalization was determined following the TIMI classification.15,16 Here, a TIMI score of 2 and 3 was regarded as sufficient, and a TIMI score of 0 and 1 was regarded as insufficient. The procedural time from onset of neurologic symptoms to the TTR was defined as the time from the beginning of symptoms to the end of the endovascular recanalization procedure. Figure 2 shows the sequence in the work-up of patients with acute stroke.
Fig 2.
Work-up of patients with acute ischemic stroke. The flow chart of the work-up procedures was determined in cooperation with the Departments of Neurology and Anesthesiology.
A 3-grade score has been adapted to the score introduced by Knauth et al17,18 and was further developed by using CTA postprocessing techniques19 to visualize the time-resolved CTA-based DSA series and later DSA, which was used in our study, as references for the evaluation of collaterals. The scale was defined as follows: 1) contrast filling being visible from pial collaterals to the M1 segment on CTA and DSA; 2) contrast filling being visible from the periphery to M2 branches in CTA and DSA; and 3) only peripheral vascular structures showing contrast filling.
Interventional Technique
Angiography and Thrombectomy.
All patients were prepared for angiography under general anesthesia after the diagnosis of MCA or distal ICA occlusion and after informed consent for an interventional treatment was obtained from either the patient (if possible) or his or her relatives. Anesthesia was induced in the angiography suite by using a standardized protocol with a timeframe of <60 minutes between admission and start of the angiography. After a diagnostic series of the right and left ICAs to detect collateralization, a 6F guiding catheter was inserted into the proximal ICA and a microcatheter was used to pass the thrombus in the occluded vessel. Due to time considerations, there was no additional catheterization of the vertebral artery to evaluate collaterals from the posterior circulation. In the next step, a Phenox clot retriever or a Penumbra system was inserted, and the fragmentation of the thrombotic material was started. For fragmentation of thrombi in the MCA, the usual diameter selected for the Penumbra system in use was 32 inches. Thrombotic occlusions of the ICA were treated with a 41-inch Penumbra system. All patients underwent mechanical recanalization in combination with medical intravenous bridging during the preparatory phase of anesthesia. All patients received rtPA as a bolus of 10 mg (“bridging dose”) and 10 mg/h intravenously until subsequent intra-arterial application. After local intra-arterial catheter placement, rtPA was injected directly into the guiding catheter with a flow velocity of 40 mg/h to a maximum dose of 0.9 mg/kg body weight. rtPA application was stopped after recanalization of the vessel. The total applied intra-arterial rtPA dose ranged from 20 to 80 mg. Heparin was given at a dose of 15,000 IU/24 hours starting at 24 hours after intervention.
After DSA-proved recanalization of the proximal vessel with remaining distal thrombi, rtPA was given to a maximum dose as stated above. Patients were monitored under general anesthesia, and CECT was performed within 24 hours after the DSA. Grade of recanalization was determined following the TIMI classification.15
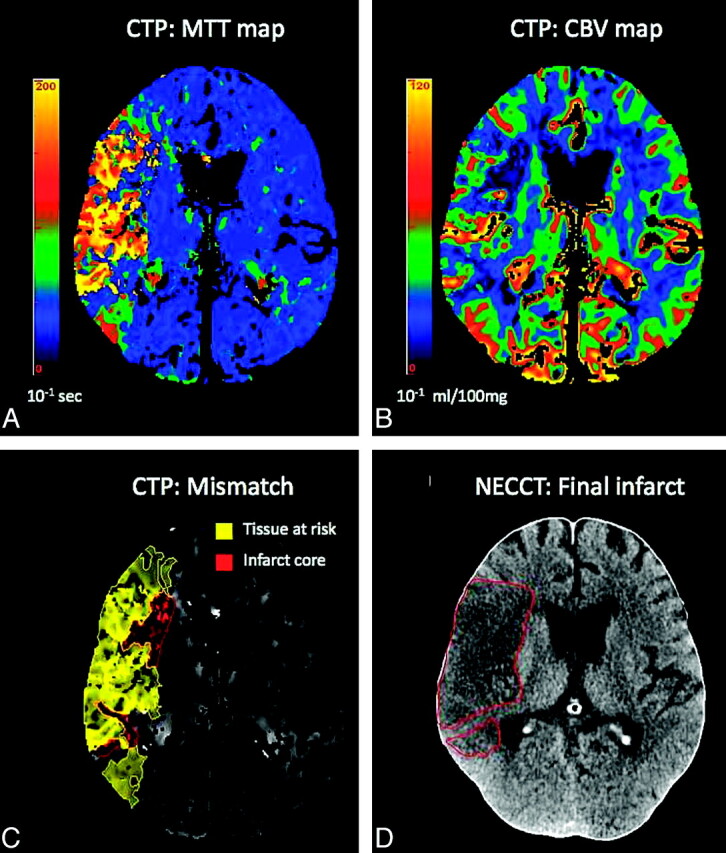
Statistic evaluation was performed with PASW 18 (http://support.spss.com/productsext/statistics/documentation/18/clientindex.html). Statistics included estimation of recanalization rate, Spearman correlation coefficients for infarct volume, percentage mismatch lost and mRS score, recanalization score, collateralization score and procedural time, and multivariate analysis of these parameters to exclude the influence of age. The effect of mismatch, degree of collateralization, and recanalization on the percentage mismatch lost are demonstrated by boxplot analysis (Fig 3).
Fig 3.
Boxplot analyses of the predictive factors for infarct growth. A, Boxplot analysis for the factor “mismatch” for the whole group (1, mismatch; 2, no mismatch) demonstrates a higher percentage mismatch lost (permisloss) for patients without mismatch (2) in preinterventional stroke CT. B, Boxplot analysis for mismatch for the Penumbra subgroup (1, mismatch; 2, no mismatch) shows a greater difference of permisloss between patients with mismatch (1) in comparison with patients without mismatch (2) in preinterventional stroke CT. C, Boxplot analysis for the factor “collateralization” shows a higher permisloss for poor collateralization (3) with the most pronounced difference between good (1) and moderate (2) collateralization in preinterventional CT. Zero indicates missing values (n = 3). D, Boxplot analysis for the factor collateralization for the Penumbra subgroup shows a comparable relation (as in C) between an increasing percentage mismatch lost and a decreasing extent of collaterals (1, good collaterals; 2, moderate collaterals; 3, no collaterals; 0, missing values). E, Boxplot analysis for the factor TIMI for the whole group (TIMI 0, poor; 1, moderate; 2, good; 3, complete) shows a reduction of percentage mismatch lost with increasing recanalization grades. F, Boxplot analysis for the factor “TIMI” for the Penumbra subgroup (TIMI 1, poor; 2, moderate; 3, good; 4, complete) shows a reduction of percentage mismatch lost with higher recanalization grades.
Results
On admission, the mean NIHSS score was 14.4 ± 4.4 for all patients. Twenty-one of 31 patients presented with MCA occlusion. These patients had a mean NIHSS score of 13.8 ± 3.8. Ten of 31 patients presented with ICA occlusion with a mean NIHSS score on admission of 15.5 ± 5.3.
At 3 months, the mRS score revealed a good outcome (mRS, 0–2) in 8 (25.8%) patients and a fair or poor outcome in 23 (73.3%) patients. Thirty-five percent of patients showing a mismatch on the initial CT presented with a good clinical outcome (mRS, 0–2) at follow-up. For estimating the mismatch by CTA and PCT, 28/31 patients could be evaluated. Twenty-one of 28 patients (67.7%) presented with and 7/28 (22.6%) presented without mismatch on the initial stroke CT. Three of 31 patients did not receive the full CECT examination needed for calculation of mismatch. During the preinterventional angiography, a good collateralization (grade 1) was depicted in 19/31 patients (61%), a medium collateralization (grade 2) was depicted in 5 patients (16%), and 7 patients presented without the presence of collaterals (23%). In none of the patients was spontaneous reopening observed. There was an overall recanalization rate of 80.9% for patients with MCA occlusions, which was 88.7% for the Penumbra subgroup. Sixty percent of ICA occlusions could be treated satisfactorily (TIMI 2 and 3). The overall recanalization rate irrespective of the recanalized vessel was 75% (for details see Table 2). For 6 patients being treated with the Phenox clot retriever, 3 patients presented without (TIMI 0 and 1) and 3 patients presented with sufficient recanalization (TIMI 2–3). In 5 patients being treated with alternative methods (stents), recanalization was not achieved in 1 and was satisfactory in 4 patients (80%).
Table 2:
Recanalization rates according to TIMI classification for all patients and the Penumbra subgroup with ICA or MCA occlusion
| Recanalization Grade | All Patients | Penumbra Subgroup | ||||||
|---|---|---|---|---|---|---|---|---|
| TIMI | 0 | 1 | 2 | 3 | 0 | 1 | 2 | 3 |
| ICA | 1 | 3 | 3 | 3 | 0 | 0 | 1 | 2 |
| % | 10 | 30 | 30 | 30 | 0 | 0 | 33.3 | 66.7 |
| MCA | 3 | 1 | 4 | 13 | 1 | 1 | 4 | 11 |
| % | 14.3 | 4.8 | 19 | 61.9 | 5.9 | 5.9 | 23.5 | 64.7 |
Table 1:
Distribution of vessel occlusions of all interventionally treated patients
| Type of Occluded Artery | Total No. of Occluded Arteries | Percentage | No. of Patients Treated with Penumbra | Percentage of All Patients |
|---|---|---|---|---|
| ICA | 10 | 29.4 | 3 | 13.6 |
| MCA | 21 | 61.8 | 17 | 77.3 |
Spearman correlation (On-line Table 1) showed a significant inverse correlation between mRS and recanalization grade (TIMI score; r = −0.544, P = .002). The detection of mismatch before intervention was associated with a smaller infarct growth (r = −0.476, P = .007 for all patients; r = −0.511, P = .018 for the Penumbra subgroup). In the Penumbra subgroup, the extent of collateralization was inversely related to infarct growth (r = −0.456, P = .033) and to mRS (r = −0.522, P = .018). The mRS score was significantly correlated to the age of patients. On-line Table 2 summarizes the interdependencies analyzed by ANOVA after excluding age as a covariate. The extent of mismatch was associated with the extent of infarct growth and percentage mismatch loss for both groups. The extent of recanalization (TIMI) was related to infarct growth and to percentage mismatch loss for the whole group (but not for the Penumbra subgroup). The time to recanalization had an influence on infarct growth, showing that the factor of procedural time and time from onset of symptoms to reopening of the vessel is an important component for tissue outcome. Collateralization had a significant impact on infarct growth but not for percentage mismatch lost. There were interactions between time to recanalization, mismatch, and TIMI score, indicating that mismatch may positively influence successful recanalization (On-line Table 2).
In Fig 3A-F, the relation of percentage mismatch lost with the preinterventional CT-proved mismatch, collateralization, and TIMI score is depicted. In Fig 3A and B, the percentage mismatch loss is inversely related to the extent of mismatch. In Fig 3C and D, the percentage mismatch lost is inversely related to the grade of collateralization. In Fig 3E and F, the percentage mismatch lost is inversely related to the grade of recanalization (TIMI). Thus, the boxplot analyses underscore the importance of CT-based tissue parameters and recanalization grade for tissue outcome.
Discussion
This study demonstrates, in an image-guided approach, a significant impact of the extent of collateralization, the extent of mismatch, and the recanalization grade with the final tissue outcome (infarct volume) in patients with acute stroke from MCA or ICA occlusion. Our findings also demonstrate the influence of age on clinical and tissue outcome as has been described before.19
Current techniques for interventional stroke therapy using mechanical devices are evolving fast with various devices such as the Merci retriever (Concentric Medical, Mountain View, California), Phenox, Penumbra system, and microstents for temporal stent placement like the Solitaire stent.5 Some single-center studies demonstrated the efficacy of the Penumbra system and described recanalization rates between 81% and 100%.1,2,20–22 Findings in these studies are similar to our results with a recanalization rate of 88.2%. The Phenox clot retriever revealed a recanalization rate of 50% in a comparably small number of cases in our study (n = 6). Ongoing new developments indicate that retrievable stent systems will have great impact on interventional stroke therapy.5
Despite the excellent recanalization data, good clinical outcome (mRS scores, ≤2) was reached in 25% of the entire patient population and in 35% of patients with CT-proved mismatch. Comparable to the findings in the Penumbra PIVOTAL study with a 25% rate of patients presenting with an mRS score of 2 or less in the 3 month outcome, the outcome in our study is lower than that in the intra-arterial tissue plasminogen activator therapy group of PROACT II.20 We believe that this is mostly due to a selection bias because in PROACT II, M1 and M2 occlusions were both included into the study, whereas M2 occlusions are mostly treated by systemic thrombolysis in our institution, which is facilitated by immediate CT and a preselection of patients. Moreover, we included patients with carotid artery occlusion in our evaluation who were clinically often severely affected and in whom there is a high demand for interventional effort to reopen the vessel. When we excluded carotid artery occlusions and patients without mismatch (37.5%), 16 patients showed an mRS score of ≤2, which most likely equals the inclusion criteria of PROACT II (NECT without bleeding or infarction of more than one-third of the media territory). This cohort of patients includes patients with M2 occlusions in eloquent cerebral regions, which is regarded as the best subgroup in a CT-based prospective observational study of intra-arterial lysis or mechanical recanalization. Excluding this patient population may be responsible for the better outcome data in PROACT II in relation to the PIVOTAL trial and our study. In our opinion, the results of the PROACT trial are comparable with the results of our study with regard to clinical outcome and time to revascularization. A larger multicenter trial with a larger cohort of patients with CT-proved artery occlusions is probably needed to evaluate the effect of improved recanalization grades with interventional devices.
Multimodal stroke CT, combining NECT, CTA, and PCT, demonstrated its feasibility to assess patients with acute stroke.23 The next step toward a more individualized therapy of stroke was to use an intra-arterial application of rtPA, which was recommended as an alternative therapy beyond the 3-hour time window.24
Most publications use the recanalization success and the clinical outcome as a treatment control and do not correlate their data to tissue outcome. Volume perfusion CECT, as in our study, combined with an off-line analysis of infarct volume, is a highly valuable parameter for therapy control. The presence of mismatch and the TIMI score correlate strongly with a better tissue outcome. Our data are supported by the findings of Tan et al,19 who found a significantly smaller infarct size in patients with higher TIMI scores.
The recanalization grade was not strongly correlated with tissue outcome, which is most obviously a consequence of the high number of recanalized vessels, so the group of unsuccessful interventional results is small. However, after correcting for age, there is a substantial effect of recanalization grade on tissue outcome. Consequently, as soon as recanalization failed (TIMI 0), a remarkable growth of the visible infarct size on NECT and a higher percentage mismatch lost was observed. These results parallel the findings by Jansen et al,9 who showed a significantly smaller infarct size in patients with early recanalization.
An important finding of our study is that the time interval of 1–3.5 hours between onset of symptoms and recanalization showed an effect on tissue outcome after correction for age. However, mismatch and degree of collateralization seem to be more important. This finding fits the data of a comparative study on systemic and local thrombolysis showing a more favorable outcome in patients with intra-arterial thrombolysis despite the longer procedural time, so the time delay caused by the interventional approach may be justified.25 However, in accordance with the findings of Hallevi et al,10 our data show that the duration from symptom onset to recanalization alone is not as critical as the expression “time window” may suggest. Our data indicate that a modern prestroke imaging-based assessment of flow maintenance by collaterals either directly or by calculation of infarct core and mismatch adds important prognostic information.
Similar to our strategy, Struffert et al2 showed that application of a thrombolytic agent in addition to thrombus aspiration is safe. In their study, recanalization was performed without general anesthesia, showing similar results. The indication of general anesthesia has to be discussed for several reasons. Our data suggest that the delay in treatment from anesthesia can be accepted as long as collaterals are present, but to prove the effect of time delay of general anesthesia on the outcome parameters, one must take into account the pre- and postinterventional collaterals (eg, by 4D-CTA).
Age seems to play a critical role. Younger patients with stroke benefit even more from interventional stroke therapy.19 This may change with the further technical developments of interventional devices. Moreover, one has to assume that therapy at a certified stroke unit is more effective in treating the young.26,27 The fact that intracranial bleeding caused 1 death also demonstrates the risk of fatal failure of this treatment.
Conclusions
In a multimodal ischemic stroke concept, diagnosis and treatment rely on improved imaging, with calculation of mismatch and collateralization demonstrating their impact on decision-making. In our study, 60%–80% recanalization rates in patients with ICA and MCA occlusions are related to improved clinical outcome (mRS score, ≤ 2) in 25.8% of all patients and 35% of patients with CT-proved mismatch. Thus, mechanical recanalization on the basis of multimodal stroke CT is a reasonable approach for patients with large-vessel occlusions without flow and a high amount of thrombotic material and when systemic lysis has to be escalated. The comparison with PROACT II showed that there is a need for a larger study to prove the therapeutic benefit of mechanical recanalization procedures.
Supplementary Material
ABBREVIATIONS
- CECT
contrast-enhanced CT
- mRS
modified Rankin scale
- NECT
nonenhanced CT
- PCT
perfusion CT
- PIVOTAL
phase III clinical “pivotal” key study
- PROACT
prolysis in acute cerebral thromboembolism
- rCBV
relative cerebral blood volume
- TIMI
thrombolysis in myocardial infarction
- TTR
time to recanalization
Footnotes
Disclosures: Harald Seifarth, Research Support (including provision of equipment or materials: Siemens, Details: research support for CT; Consultant: Siemens, Details: consultant for CT applications.
References
- 1. Kulcsar Z, Bonvin C, Pereira VM, et al. Penumbra system: a novel mechanical thrombectomy device for large-vessel occlusions in acute stroke. AJNR Am J Neuroradiol 31: 628– 33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Struffert T, Kohrmann M, Engelhorn T, et al. Penumbra stroke system as an “add-on” for the treatment of large vessel occlusive disease following thrombolysis: first results. Eur Radiol 2009; 19: 2286– 93 [DOI] [PubMed] [Google Scholar]
- 3. Liebig T LJ, Reinartz J, Roth C, et al. Early clinical experiences with new thrombectomy device for the treatment of ischemic stroke. In: Proceedings of the International Stroke Conference, New Orleans, Louisiana. February 20–22, 2008 [Google Scholar]
- 4. Flint AC, Duckwiler GR, Budzik RF, et al. Mechanical thrombectomy of intracranial internal carotid occlusion: pooled results of the MERCI and Multi MERCI Part I trials. Stroke 2007; 38: 1274– 80. Epub 2007 Mar 1 [DOI] [PubMed] [Google Scholar]
- 5. Castano C, Dorado L, Guerrero C, et al. Comment on: Mechanical thrombectomy with the Solitaire AB device in large artery occlusions of the anterior circulation: Castaño C, Dorado L, Guerrero C, et al. Stroke 2010;41:1836–40. Clin Neuroradiol 2010; 20: 267– 68. Epub 2010 Dec 3 [DOI] [PubMed] [Google Scholar]
- 6. Kloska SP, Fischer T, Nabavi DG, et al. Color-coded perfused blood volume imaging using multidetector CT: initial results of whole-brain perfusion analysis in acute cerebral ischemia. Eur Radiol 2007; 17: 2352– 58 [DOI] [PubMed] [Google Scholar]
- 7. Heiss WD, Sobesky J, Hesselmann V. Identifying thresholds for penumbra and irreversible tissue damage. Stroke 2004; 35: 2671– 74 [DOI] [PubMed] [Google Scholar]
- 8. Nichols C, Khatri P, Tomsick T, et al. Advantages of a combined approach to recanalization therapy. Stroke 2008; 39: e71, author reply e72 [DOI] [PubMed] [Google Scholar]
- 9. Jansen O, Schellinger P, Fiebach J, et al. Early recanalisation in acute ischaemic stroke saves tissue at risk defined by MRI. Lancet 1999; 353: 2036– 37 [DOI] [PubMed] [Google Scholar]
- 10. Hallevi H, Barreto AD, Liebeskind DS, et al. Identifying patients at high risk for poor outcome after intra-arterial therapy for acute ischemic stroke. Stroke 2009; 40: 1780– 85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schaefer PW, Roccatagliata L, Ledezma C, et al. First-pass quantitative CT perfusion identifies thresholds for salvageable penumbra in acute stroke patients treated with intra-arterial therapy. AJNR Am J Neuroradiol 2006; 27: 20– 25 [PMC free article] [PubMed] [Google Scholar]
- 12. Wechsler LR. Imaging evaluation of acute ischemic stroke. Stroke 42: S12– 15 [DOI] [PubMed] [Google Scholar]
- 13. Gonzalez RG. Imaging-guided acute ischemic stroke therapy: from “time is brain” to “physiology is brain”. AJNR Am J Neuroradiol 2006; 27: 728– 35 [PMC free article] [PubMed] [Google Scholar]
- 14. Wintermark M. Brain perfusion-CT in acute stroke patients. Eur Radiol 2005; 15(suppl 4): D28– 31 [DOI] [PubMed] [Google Scholar]
- 15. Tomsick T. TIMI, TIBI, TICI: I came, I saw, I got confused. AJNR Am J Neuroradiol 2007; 28: 382– 84 [PMC free article] [PubMed] [Google Scholar]
- 16. Khatri P, Neff J, Broderick JP, et al. Revascularization end points in stroke interventional trials: recanalization versus reperfusion in IMS-I. Stroke 2005; 36: 2400– 03. Epub 2005 Oct 13 [DOI] [PubMed] [Google Scholar]
- 17. Knauth M, von Kummer R, Jansen O, et al. Potential of CT angiography in acute ischemic stroke. AJNR Am J Neuroradiol 1997; 18: 1001– 10 [PMC free article] [PubMed] [Google Scholar]
- 18. Hesselmann V, Seifarth H, Dziewas R, et al. Darstellung der kollateralisation zerebraler gefäßverschlüsse durch zeitlich aufgelöste cta zur einschätzung der lyse- und rekanalisationsfähigkeit. Jahrestagung der deutschen Gesellschaft 7–9 Oktober 2009 [Google Scholar]
- 19. Tan IY, Demchuk AM, Hopyan J, et al. CT angiography clot burden score and collateral score: correlation with clinical and radiologic outcomes in acute middle cerebral artery infarct. AJNR Am J Neuroradiol 2009; 30: 525– 31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Penumbra Pivotal Stroke Trial Investigators. The Penumbra pivotal stroke trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke 2009; 40: 2761– 68. Epub 2009 Jul 9 [DOI] [PubMed] [Google Scholar]
- 21. Grunwald IQ, Walter S, Papanagiotou P, et al. Revascularization in acute ischaemic stroke using the Penumbra system: the first single center experience. Eur J Neurol 2009; 16: 1210– 16. Epub 2009 Jul 29 [DOI] [PubMed] [Google Scholar]
- 22. Bose A, Henkes H, Alfke K, et al. The Penumbra system: a mechanical device for the treatment of acute stroke due to thromboembolism. AJNR Am J Neuroradiol 2008; 29: 1409– 13. Epub 2008 May 22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kloska SP, Nabavi DG, Gaus C, et al. Acute stroke assessment with CT: do we need multimodal evaluation? Radiology 2004; 233: 79– 86 [DOI] [PubMed] [Google Scholar]
- 24. Schellinger PD, Orberk E, Hacke W. Antithrombotic therapy after cerebral ischemia [in German]. Fortschr Neurol Psychiatr 1997; 65: 425– 34 [DOI] [PubMed] [Google Scholar]
- 25. Mattle HP, Arnold M, Georgiadis D, et al. Comparison of intraarterial and intravenous thrombolysis for ischemic stroke with hyperdense middle cerebral artery sign. Stroke 2008; 39: 379– 83 [DOI] [PubMed] [Google Scholar]
- 26. Turaj W, Slowik A, Wnuk M, et al. Gender-related differences in diagnostic evaluation and outcome of ischemic stroke in Poland. Stroke 2009; 40: 980– 82 [DOI] [PubMed] [Google Scholar]
- 27. Saposnik G, Hill MD, O'Donnell M, et al. Variables associated with 7-day, 30-day, and 1-year fatality after ischemic stroke. Stroke 2008; 39: 2318– 24 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.