SUMMARY:
We present a unique case of multiple sCADs occurring after a ruptured intracranial aneurysm embolization. We discuss the impact of head extension during embolization as the prevailing factor in multiple artery dissections in this case and point out another cause of new-onset neurologic deficit in patients with aneurysmal SAH.
Simultaneous occurrence of 3 or 4 cervical artery dissections has a reported incidence of 1–3 per 1 million in the general population and 0.1–1.6% in patients with dissection.1,2 The clinical manifestations of sCAD occur in approximately 90% of patients,3 and the most frequent are stroke, transient ischemic attack and/or brain or spinal cord ischemia,1,4,5 and SAH without ischemia in <2%3 of these patients. There are a few case reports presenting sCAD concurrent with intracranial saccular aneurysms.6,7 To our knowledge, there has not been a report of 4-vessel dissection occurring in the course of treatment of a ruptured intracranial saccular aneurysm. In this communication, we present such a case.
Case Report
A 40-year-old woman was admitted to the emergency department due to generalized seizures following the acute onset of severe headache. The head CT scan revealed a diffuse SAH due to a ruptured anterior communicating artery aneurysm. There were no other vessel abnormalities on CTA (Fig 1B). The patient underwent an embolization of the aneurysm performed through the right ICA, which was the only vessel catheterized. The working projection was an oblique view with hyperextension of the head (Fig 1A). Four days later she developed a right hemiparesis with motor aphasia and a deteriorating level of consciousness with persistent headache. Her symptoms were attributed to vasospasm. She underwent a head CTA, which revealed dissection of all 4 neck vessels (Fig 1C, –D) below the skull base. This finding was confirmed by MR imaging/MRA of the head and neck. Diffusion-weighted images also demonstrated an acute infarct of the left caudate nucleus and of the watershed area of the left-middle-to-anterior cerebral artery territories. These findings could explain the onset of her symptoms, and it was decided to start an anticoagulation treatment for the dissections without any interventional procedure. During her hospitalization, she underwent a clinical and laboratory investigation for a possible connective tissue disorder and a skin and salivary gland biopsy. None of these examinations revealed any underlying pathology. The outcome after 6 months was favorable, with a modified Rankin scale score of 2. Control MR imaging/MRA revealed a mild residual stenosis of the 4-vessel lumen and a pseudoaneurysm formation of the right ICA at the neck.
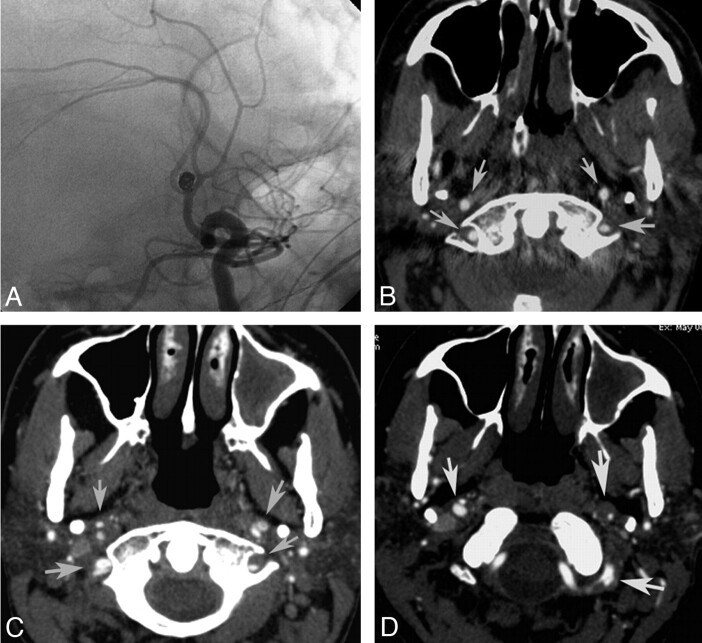
Fig 1.
A, Left ICA angiogram showing the working projection. B, Axial CTA before embolization. Note the normal aspect of both the ICA and VA (arrows). C and D, Axial CTA at symptom onset shows expansion of the outer wall with narrowing of the vessel lumen, pseudoaneurysms in both the ICA and VA (arrows), and enlargement of the outer diameter with luminal stenosis of the left VA (arrow).
Discussion
The frequency of saccular intracranial aneurysms in patients with sCAD was estimated at 5.5%,8 higher than that of the general population, supporting the evidence for an underlying vasculopathy.1,8,9 Especially in the article of Mazighi et al,9 7 cases of sCAD were reported in the course of ruptured saccular intracranial aneurysms, implying a common predisposing factor for both diseases, but more important, a higher frequency of sCAD in the course of aneurysmal SAH is supported, due to SAH-induced intense sympathetic stimulation. Female sex, migraine, and minor trauma, as in our patient, are mentioned as risk or triggering factors of sCAD.1–5 Moreover, when carotid artery dissection occurs, in 15%–29% of cases, it is bilateral or associated with VA dissection.5 Clinical vasospasm after aneurysmal SAH resulting in stroke or death occurs in 15%–20% of patients. The development of a new focal deficit in patients with SAH that cannot be explained by hydrocephalus or rebleeding is the first objective sign of vasospasm.10 Control CTA in our patient revealed another reason for neurologic deterioration in aneurysmal SAH, not previously reported.
Multiple sCADs in this patient as a periprocedural complication were ruled out because there was no intervention in any cervical vessel except the right ICA. The patient was extubated the same day without any neurologic sequelae. Her deterioration 4 days later corresponded to the median delay of the onset of neurologic deficits after sCAD. However, it is not easy to define “minor trauma” or its impact on multiple sCADs.11,12 Mild mechanical stress plays a role as a possible triggering factor in the pathogenesis of the disease.12 In our case, head extension during embolization to achieve a safe working projection for coiling appears to be the only plausible cause of multiple sCADs.
There is no standard treatment protocol or guidelines for treatment of sCAD. There are only recommendations and no evidence to support the routine use of anticoagulants or antiplatelet drugs or the superiority of each for the treatment of extracranial carotid dissection.13 Moreover, the prognosis of the disease seems to be benign,5 and spontaneous resolution is observed in >80% of patients within 3 months.1,6 Endovascular procedures are mainly reserved for traumatic dissections.14 Because stroke is the main manifestation and its recurrence rate is approximately 2%–4% in this disease,15 it is reasonable to administer anticoagulation or/and antithrombotic treatment. In our case, having secured the SAH source, we used anticoagulation therapy to prevent further ischemia, which could also progress in the course of post-SAH vasospasm.
In conclusion, we draw attention to details such as head position during embolization and propose a meticulous examination of neck vasculature in patients with SAH who deteriorate, to rule out another possible cause of deterioration frequent mostly in younger patients.
Abbreviations
- CTA
CT angiography
- ICA
internal carotid artery
- MRA
MR angiography
- SAH
subarachnoid hemorrhage
- sCAD
spontaneous cervical artery dissection
- VA
vertebral artery
References
- 1. Arnold M, DeMarchis GM, Stapf C, et al. Triple and quadruple spontaneous cervical artery dissection: presenting characteristics and long-term outcome. J Neurol Neurosurg Psychiatry 2009;80:171–74 [DOI] [PubMed] [Google Scholar]
- 2. Redekop GJ. Extracranial carotid and vertebral artery dissection: a review. Can J Neuro Sci 2008. 35:146–52 [DOI] [PubMed] [Google Scholar]
- 3. Arnold M, Bousser MG, Fahrni G, et al. Vertebral artery dissection: presenting findings and predictors of outcome. Stroke 2006;37:2499–503 [DOI] [PubMed] [Google Scholar]
- 4. Nedeltchev K, Aufder MT, Georgiadis D, et al. Ischemic stroke in young adults: predictors of outcome and recurrence. J Neurol Neurosurg Psychiatry 2005;76:2191–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dittrich R, Nassenstein I, Bachman R, et al. Polyarterial clustered recurrence of cervical artery dissection seems to be the rule. Neurology 2007;69:180–86 [DOI] [PubMed] [Google Scholar]
- 6. Marshman L, Ball L, Jadun CK. Spontaneous bilateral carotid and vertebral artery dissections associated with multiple disparate intracranial aneurysms, subarachnoid hemorrhage and spontaneous resolution: case report and literature review. Clin Neurol Neurosurg 2007;109:816–20. Epub 2007 Aug 20 [DOI] [PubMed] [Google Scholar]
- 7. Akiyama Y, Moritake K, Miyazaki T, et al. Subarachnoid hemorrhage in the presence of both intracranial dissecting and saccular aneurysms: two case reports. Neurol Med Chir (Tokyo) 2007;47:65–69 [DOI] [PubMed] [Google Scholar]
- 8. Schievink WI, Mokri B, Piepgras DG. Angiographic frequency of saccular intracranial aneurysms in patients with spontaneous cervical artery dissection. J Neurosurg 1992;76:62–66 [DOI] [PubMed] [Google Scholar]
- 9. Mazighi M, Saint Maurice JP, Rogopoulos A, et al. Extracranial vertebral and carotid dissection occurring in the course of subarachnoid hemorrhage. Neurology 2005;65:1471–73 [DOI] [PubMed] [Google Scholar]
- 10. Bederson JB, Connolly ES, Batjer HH, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: statement for healthcare professionals from a special writing group of the Stroke Council—American Heart Association. Stroke 2009;40:994–1025. Epub 2009 Jan 22 [DOI] [PubMed] [Google Scholar]
- 11. Rubinstein SM, Peederman SM, vanTulder MW, et al. A systematic review of the risk factors for cervical artery dissection. Stroke 2005;36:1575–80 [DOI] [PubMed] [Google Scholar]
- 12. Dittrich R, Rohsbach D, Heidbreder A, et al. Mild mechanical traumas are possible risk factors for cervical artery dissection. Cerebrovasc Dis 2007;23:275–81 [DOI] [PubMed] [Google Scholar]
- 13. Lyrer P, Engelter S. Antithrombotic drugs for carotid artery dissection. Cochrane Database of Systematic Reviews, 2003, Issue 3, available at: http://www.cochrane.org/reviews/en/ab000255.html. Accessed January 15, 2010 [DOI] [PMC free article] [PubMed]
- 14. Cochen JE, Ben-Hur T, Rasj G, et al. Endovascular stent assisted angioplasty in the management of traumatic internal carotid artery dissections. Stroke 2005;36:45–47 [DOI] [PubMed] [Google Scholar]
- 15. The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19,435 patients acute ischemic stroke—International Stroke Trial Collaborative Group. Lancet 1997;349:1596–81 [PubMed] [Google Scholar]