Abstract
BACKGROUND AND PURPOSE:
Many authors have reported the increase in vertebral body height after vertebroplasty; if the fractured vertebrae are mobile, we should be able to demonstrate their mobility in radiographs. The purpose of this study was to discover the diagnostic value of dynamic radiographs and the percentage of mobile vertebrae in painful VCFs.
MATERIALS AND METHODS:
From September 2005 to September 2008, 105 patients underwent surgery to treat 144 painful osteoporotic VCFs. The indications for surgery were severe pain and MR imaging−confirmed active edematous lesions. Preoperative sitting lateral radiographs of the fractured vertebrae were compared with supine cross-table (with a bolster beneath) lateral radiographs to determine the presence or absence of dynamic mobility. Kyphotic angle and anterior vertebral body height were measured.
RESULTS:
The patients' ages ranged from 62 to 90 years. There were 19 men and 86 women. The total number of mobile VCFs was 126 (87.5%). One hundred four (99%) patients had at least 1 mobile VCF. The average anterior vertebral height in sitting lateral radiographs was 13.53 ± 6.80 mm and increased to 22.01 ± 6.13 mm in supine cross-table with bolster lateral radiographs. The average vertebral body height increase was 8.48 ± 5.36 mm.
CONCLUSIONS:
Dynamic (sitting and supine with bolster) radiographs can be valuable in diagnosing painful vertebrae in VCFs. The sensitivity was 0.88 in this study.
McKiernan et al1 demonstrated dynamic mobility in 44% of 41 patients who underwent vertebroplasty. Many authors have also reported an increase in vertebral body height after vertebroplasty.2,3 Chin et al4 reported that postural reduction vertebroplasty can lead to significant restoration of vertebral body height and correction of kyphosis in osteoporotic VCFs. Lee and Chen5 showed the same results by closed reduction vertebroplasty. Orler et al6 used lordoplasty to restore the lordosis. If the vertebral body height can be increased by postural reduction or closed reduction during vertebroplasty, it must be mobile (nonunion). If it is mobile, we should be able to demonstrate its mobility in radiographs.
X-ray and MR imaging are the primary imaging modalities for evaluating suspected VCFs. However, x-ray sometimes cannot differentiate recent or unhealed fractures from those that have healed. Only MR imaging and bone scanning can be used to evaluate the edematous (symptomatic) lesion and determine which vertebra is symptomatic and requires treatment. If painful VCFs can be demonstrated to be mobile in dynamic radiographs, then we can use these radiographs to diagnose painful VCFs. The object of this study was to evaluate the percentage of mobile vertebrae in MR imaging−proved painful osteoporotic VCFs with modified dynamic radiographs and to see whether this technique is useful in diagnosing painful VCFs.
Materials and Methods
The institutional review board approved this radiographic analysis of 105 consecutive patients with 144 VCFs who underwent vertebroplasty (86 patients) or open surgery (19 patients) in our institution. The indications for treatment (vertebroplasty or surgery) were severe pain that was not responsive to medical treatment and MR imaging−confirmed active edematous lesions (hyperintense on STIR sequences and/or contrast enhancement on fat-suppressed gadolinium-enhanced T1-weighted imaging). Preprocedural anteroposterior and lateral radiographs were obtained. In addition, each patient underwent preprocedural sitting lateral radiography centered on the fractured vertebra and a supine cross-table lateral radiography centered on the index vertebra with a bolster (10 cm in height) placed beneath it.1 As an outcome measurement, a VAS with 10 divisions was used.
Digital files of the patients' radiographs were retrieved from the PACS for analysis. Two of the authors (D.-F.L. and Y.-J.C.) performed these measurements. Intraobserver and interobserver reproducibility of these measurements was evaluated by using intraclass correlation coefficients. The kyphotic angles of the vertebral compression fractures were measured from the superior and inferior endplates of the fractured (compressed) vertebra. The change of kyphotic angle was calculated as the sitting angle minus the supine (with bolster) angle. From the lateral projection, 6 points were hand-selected and marked on each fractured vertebra (index vertebra) and the nearest nonfractured vertebra (referent vertebra) on the basis of the techniques used by McKiernan et al.7 The anterior vertebral body height of the fractured vertebra was measured. To remove the inter-radiographic magnification error, we matched each index VCF to the referent vertebra on the sitting lateral radiograph. Each index-referent vertebral pair remained constant throughout the analysis. In supine cross-table with bolster lateral radiographs, dimensions of the index vertebra were expressed as a percentage of the analogous dimension of the referent vertebra and were then scaled to the absolute dimensions of the original sitting lateral radiograph. This process cancels out any residual inter-radiographic magnification error and allows direct radiographic comparisons. According to the height change, we defined the vertebra as nonmobile (height change < 2 mm), mildly mobile (between 2 and 6 mm), and mobile (>6 mm).
Statistical Analysis
The results were expressed as the mean ± SD. The statistical significance of changes in vertebral body height and kyphotic angle was evaluated with the paired t test, in which a P value < .05 was considered to indicate a statistically significant difference. All statistical analyses were performed by using the Statistical Package for the Social Sciences, Version 12.0 (SPSS, Chicago, Illinois), Windows version.
Results
One hundred five patients underwent vertebroplasty or surgical procedures to treat 144 MR imaging−proved edematous VCFs. The patients' ages ranged from 62 to 90 years (mean, 76 years). There were 19 men and 86 women. Seventy-one patients (67.6%) had 1-level fractures, 30 patients had 2-level fractures, and 4 patients had 3-level fractures. L1 was the most commonly affected level in 37 patients, followed by T12 in 30 patients, and L2 and L3 in 17 patients.
Pain assessed by the VAS significantly (P < .001) decreased from a mean of 8.9 ± 0.7 (range, 7–10) before the procedure to 1.8 ± 1.5 (range, 0–9) after 1-month follow-up. Ninety-eight patients (93%) were satisfied with the results. Only 1 patient described no improvement in pain after vertebroplasty.
Intraobserver (Y.-J.C.) reproducibility was 0.95 for height of the vertebral body and 0.96 for kyphotic angle. Interobserver reproducibility was 0.94 for height and 0.97 for kyphotic angle. The average kyphotic angle in sitting lateral radiographs was 18.18° ± 8.22° (mean ± SD, range, 0°-36°) and changed to 7.52° ± 7.25° (range, −15°–26°) in supine cross-table with bolster radiographs. The average difference between sitting and supine with bolster was 10.67° ± 6.67° (range, −2°–27°), which was statistically significant (P < .001). The average anterior vertebral height in sitting lateral radiographs was 13.53 ± 6.80 mm (range, 0.98–29.48 mm) and increased to 22.01 ± 6.13 mm (range, 6.09–38.53 mm) in supine cross-table with bolster lateral radiographs. The average vertebral body height increase was 8.48 ± 5.36 mm (range, −1.17–24.04 mm), which was statistically significant (P < .001).
Of these 144 MR imaging−proved edematous fractured vertebrae, 126 (87.5%) were mobile and 18 (12.5%) were nonmobile. However, in all 105 treated patients, 104 (99%) had at least 1 mobile VCF; only 1 patient had a single-level nonmobile compression fracture at L5. Seventeen patients had both mobile and nonmobile VCFs. In the patients with 1-level VCF, 98.6% (70/71) had a mobile VCF. In the patients with 2- or 3-level VCFs, 100% (34/34) had at least 1 mobile VCF.
Discussion
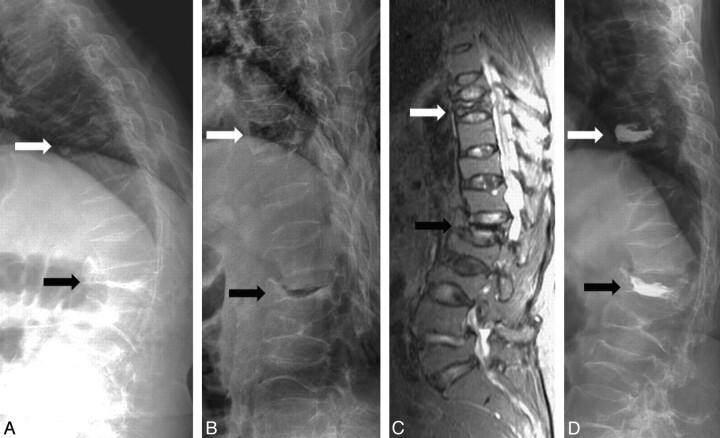
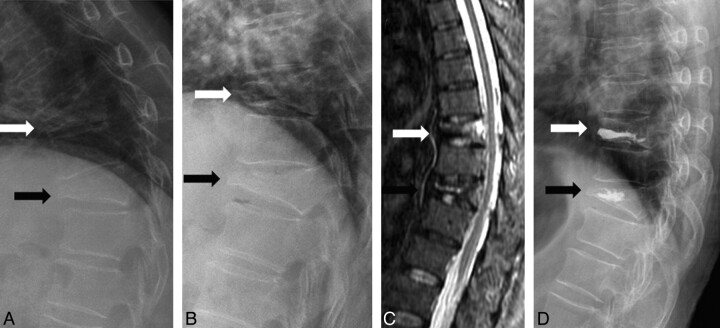
Toyone et al8 used supine and standing radiographs, and McKiernan et al1 used standing and supine (with or without bolster) radiographs to demonstrate mobility. In the study of McKiernan et al, dynamic fracture mobility was demonstrated in only 44% of patients, but they did not use a bolster in supine lateral radiographs in all patients. The vertebral body height is taller in supine with bolster radiographs (Fig 1B, white arrow) than in supine-only radiographs (Fig 1C, white arrow). In the study of McKiernan et al, 23 mobile fractures all showed marked mobility and the average anterior vertebral height increased 106% compared with the initial fracture height.1 No case of mild mobility was noted in their study. However, in another study by McKiernan et al,9 they demonstrated latent mobility of osteoporotic VCFs that was not obvious in their current standing and supine lateral radiographs. This means that mild mobility cannot be demonstrated in standing and supine lateral radiographs. To get the best comparison effect, we modified this technique and used sitting (instead of standing) and supine cross-table with bolster lateral radiographs in every patient. Although 99% of our patients showed dynamic mobility, 24 patients showed only mild mobility (Fig 2, white arrow). The mild mobility in these patients may be not obvious in standing and supine radiographs. If the patients with mildly mobile VCFs are excluded, then the percentage drops to 76.2%.
Fig 1.
A 69-year-old woman with severe back pain due to T9 and L1 compression fractures. A and B, Sitting (A) and supine with bolster (B) lateral radiographs show mobility at T9 (white arrow) and L1 (black arrow). C, Sagittal STIR MR image demonstrates hyperintensity at T9 but hypointensity at L1. D, Postvertebroplasty lateral radiograph shows cement filling in T9 and L1.
Fig 2.
A 65-year-old woman with severe back pain due to T8 and T10 compression fractures. A and B, Sitting (A) and supine with bolster (B) lateral radiographs show mild mobility at T8 (white arrow) and no mobility at T10 (black arrow). C, Sagittal STIR MR image demonstrates hyperintensity at T8 and T10. D, Postvertebroplasty lateral radiograph shows cement filling in T8 and T10.
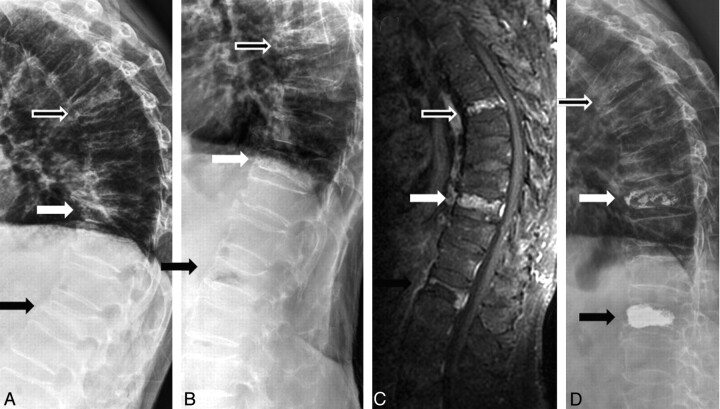
In this study, 87.5% of 144 MR imaging−proved edematous VCFs were demonstrated to be mobile. The sensitivity of dynamic radiographs in diagnosing the MR imaging−proved edematous VCFs is 0.87. However, in patients with painful VCFs that need vertebroplasty or surgical intervention, 99% of patients can be shown to have at least 1 mobile VCF. The sensitivity of dynamic radiographs in diagnosing the painful vertebrae in patients with severe pain is 0.99. An explanation is that not all edematous vertebrae are mobile; however, in patients with severe back pain who need vertebroplasty or surgical treatment, there is always at least 1 mobile vertebra. Toyone et al8 demonstrated a significant correlation between back pain and changes in the wedging rate from a supine to standing position. Changes in the wedging rate of >10% were always associated with more severe back pain. If the vertebrae are edematous but not mobile, the pain severity should be lower. So in a patient with mobile and nonmobile MR imaging−proved edematous VCFs, the mobile VCF should be the major pain source. In this study, 1 patient had 3-level compression fractures: 1 mobile and 2 nonmobile. We only treated 2 vertebrae (1 mobile and 1 nonmobile), and he still experienced dramatic pain improvement (Fig 3).
Fig 3.
A 74-year-old man with severe back pain due to T6, T10, and L1 compression fractures. A and B, Sitting (A) and supine with bolster (B) lateral radiographs show mobility at L1 (black arrow) but no mobility at T6 (hollow arrow) and T10 (white arrow). C, Contrast-enhanced T1-weighted MR image demonstrates contrast enhancement at T6, T10, and L1. D, Postvertebroplasty lateral radiograph shows cement filling in T10 and L1. Vertebroplasty was not performed at T6, but the patient still showed dramatic improvement.
Because MR imaging can provide an accurate diagnosis, what is the role of dynamic radiographs? In the time that elapses between the initial MR imaging evaluation and vertebroplasty, it is possible for additional fractures to occur. Benz et al10 recommended a repeat preprocedural MR imaging obtained within 1 week in select candidates to help ensure that all painful fractures are treated. However, the disadvantages of preprocedural MR imaging include the time, expense, and demands on the radiology department. Because dynamic radiographs are sensitive in diagnosing the painful vertebrae, they can be used as a preprocedural re-evaluation examination to rule out any new lesions if MR imaging was not recently performed. The dynamic radiographs will be more valuable in patients who cannot undergo MR imaging. In addition to its diagnostic value, dynamic radiographs can help interventionalists estimate the postprocedural vertebral height and shape and cement injection area and amount. It can also help interventionalists assess the feasibility of vertebroplasty in the vertebral plana (Fig 1, black arrow).
Although dynamic radiographs are valuable in diagnosing painful vertebrae in VCFs, they cannot replace MR imaging. MR imaging not only accurately diagnoses the painful VCFs but also, most important, differentiates simple compression from pathologic fractures. MR imaging is still recommended in every patient who undergoes vertebroplasty or surgical intervention.
Conclusions
A modified radiographic technique (sitting and supine with bolster lateral radiographs) can be valuable in diagnosing the painful vertebrae in osteoporotic VCFs. The sensitivity is 0.88 in this study. On the basis of our results, we suggest using dynamic sitting and supine with bolster lateral radiographs as a screening examination or preprocedural examination if MR imaging was not recently performed.
Abbreviations
- STIR
short-tau inversion recovery
- VAS
Visual Analog Scale
- VCF
vertebral compression fracture
Footnotes
Paper previously presented at: Annual Meeting of Taiwan Spine Society and Taiwan Orthopedic Association, October 23–25, 2009; Taipei, Taiwan.
References
- 1. McKiernan F, Jensen R, Faciszewski T. The dynamic mobility of vertebral compression fractures. J Bone Miner Res 2003;18:24–29 [DOI] [PubMed] [Google Scholar]
- 2. Teng MM, Wei CJ, Wei LC, et al. Kyphosis correction and height restoration effects of percutaneous vertebroplasty. AJNR Am J Neuroradiol 2003;24:1893–900 [PMC free article] [PubMed] [Google Scholar]
- 3. Hiwatashi A, Moritani T, Numaguchi Y, et al. Increase in vertebral body height after vertebroplasty. AJNR Am J Neuroradiol 2003;24:185–89 [PMC free article] [PubMed] [Google Scholar]
- 4. Chin DK, Kim YS, Cho YE, et al. Efficacy of postural reduction in osteoporotic vertebral compression fractures followed by percutaneous vertebroplasty. Neurosurgery 2006;58:695–700 [DOI] [PubMed] [Google Scholar]
- 5. Lee ST, Chen JF. Closed reduction vertebroplasty for the treatment of osteoporotic vertebral compression fractures: technical note. J Neurosurg 2004;100:392–96 [DOI] [PubMed] [Google Scholar]
- 6. Orler R, Frauchiger LH, Lange U, et al. Lordoplasty: report on early results with a new technique for the treatment of vertebral compression fractures to restore the lordosis. Eur Spine J 2006;15:1769–75. Epub 2006 May 25 [DOI] [PubMed] [Google Scholar]
- 7. McKiernan F, Faciszewski T, Jensen R. Reporting height restoration in vertebral compression fractures. Spine (Phila Pa 1976) 2003;28:2517–21, discussion 2523 [DOI] [PubMed] [Google Scholar]
- 8. Toyone T, Tanaka T, Wada Y, et al. Changes in vertebral wedging rate between supine and standing position and its association with back pain: a prospective study in patients with osteoporotic vertebral compression fractures. Spine 2006;31:2963–66 [DOI] [PubMed] [Google Scholar]
- 9. McKiernan F, Faciszewski T, Jensen R. Latent mobility of osteoporotic vertebral compression fractures. J Vasc Interv Radiol 2006;17:1479–87 [DOI] [PubMed] [Google Scholar]
- 10. Benz BK, Gemery JM, McIntyre JJ, et al. Value of immediate preprocedure magnetic resonance imaging in patients scheduled to undergo vertebroplasty or kyphoplasty. Spine 2009;34:609–12 [DOI] [PubMed] [Google Scholar]