Abstract
BACKGROUND AND PURPOSE:
Injury to spinal segmental arteries may potentially occur during spinal surgery, particularly during anterior or minimally invasive approaches. Use of a noninvasive radiologic tool to evaluate these arteries before surgery may reduce this risk.
MATERIAL AND METHODS:
We performed spinal CT angiography and reconstructed 3D images of segmental arteries in 41 patients. We classified the pathways and locations of the segmental arteries into 4 zones (A, B, C, and D) according to pedicle and vertebral endplates. We designated segmental arteries from T8 to L1 as “high-level segmental arteries” and those from L2 to L4, as “low-level segmental arteries.” We compared the distribution of segmental arteries between these 2 groups. We also investigated anatomic variations of segmental arteries and the rate of occurrence of the artery of Adamkiewicz.
RESULTS:
In all patients, 3D reconstruction images from spinal CT angiography clearly showed the pathways of segmental arteries on the vertebral bodies. Most of the segmental arteries passed the middle portion of the vertebral body (zones B and C). However, 51 of 738 segmental arteries (6.9%) had uncommon pathways (zones A and D), and segmental arteries from L2 to L4 had a higher incidence of uncommon pathways than higher level vertebrae (P < .05). We also observed 2 types of segmental artery anatomic variation, agenesis and dual supply.
CONCLUSIONS:
We suggest that spinal CT angiography can help to precisely visualize the spinal segmental arteries and surrounding bony structures and can aid clinicians in deciding on optimal approaches for spinal surgery.
Multidetector CT has enlarged our view of human vascular anatomy. 3D reconstruction images of CT angiography provide a view similar to surgical anatomy and can aid in diagnosis and preoperative planning.1,2 This method has been used to evaluate large vessels such as the iliac arteries, iliac veins, aorta, and vertebral arteries for spinal surgery by anterior lumbar and high cervical approaches,1,2 but it is not currently applied to segmental or intercostal arteries.
Spinal segmental arteries are susceptible to surgical injury by anterior and minimally invasive approaches.3–7 The percutaneous lumbar transforaminal endoscopic approach and the extrapedicular approach in vertebroplasty or kyphoplasty may directly cause such injury. Occasionally, segmental artery injury may result in a retroperitoneal hematoma requiring invasive treatment such as endovascular embolization or surgical ligation.3,4
In this study, we tested the feasibility of using 3D spinal CT angiography to determine the positions of spinal segmental arteries before percutaneous lumbar endoscopic diskectomy or extrapedicular vertebroplasty. Such presurgical evaluation may help avoid arterial injury.
Materials and Methods
Patients
From October 2008 to October 2009, we performed spinal CT angiography in patients who were in need of percutaneous vertebroplasty and percutaneous endoscopic lumbar diskectomy. For this study, we enrolled 41 of these patients, including 32 women and 9 men (mean age, 71.2 ± 11.2 years). We excluded patients who showed abnormal blood urea nitrogen or serum creatine levels or skin hypersensitivity to the contrast medium.
We performed this investigation in accordance with our institutional guidelines, which comply with international laws and policies (Hallym University Institutional Review Board, #2009-28).
Spinal CT Angiography and 3D Reconstruction of Segmental Arteries
Spinal CT angiography was performed by using a 64-detector CT scanner (Somatom Sensation 64; Siemens Medical Solutions, Forchheim, Germany) with nonionic iodine contrast medium (iohexol, 300 mg/mL, Omnipaque; GE Healthcare, Milwaukee, Wisconsin). A total of 2.0 mL/kg of body weight of iohexol was administered at 5.5 mL/s through an 18-gauge intravenous catheter in an antecubital vein by using a power injector, while a computer-assisted bolus-tracking system synchronized the flow with the CT acquisition. Data acquisition proceeded from T7 to L5 in a craniocaudal direction in 1.0-mm sections at 0.6-mm intervals. Using commercial 3D reconstruction software (Wizard, Siemens Medical Solutions), we made 3D reconstruction images of spinal segmental arteries with bony structure contours from T7 to the area of L5 (Fig 1).
Fig 1.

A 3D reconstruction image of spinal segmental arteries by using intravenous CT angiography.
Analysis of Pathways and Anatomic Variations of Segmental Arteries
The pathways and locations of bilateral spinal segmental arteries from T8 to L4 were analyzed. Segmental arteries above the T7 area were excluded from analysis because the ascending aorta and rib head interfered with imaging of the left-sided segmental arteries above T7. We also excluded segmental arteries in the area of L5 because these showed frequent anatomic variation and the iliac crest interfered with their imaging. A total of 738 segmental arteries in 41 patients were examined.
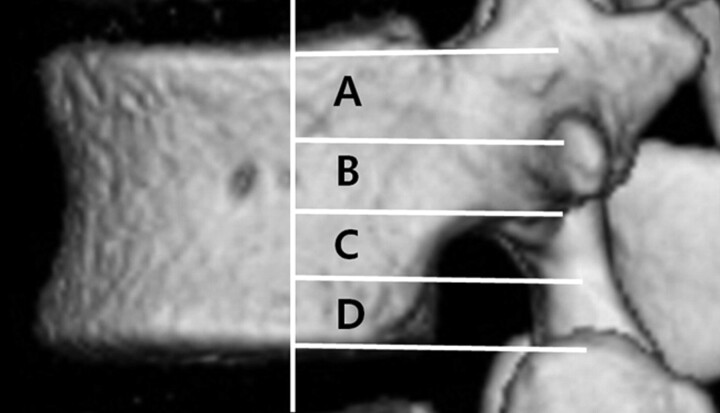
The pathways and locations of segmental arteries were classified into 4 zones (A, B, C, and D) according to pedicle and vertebral endplates (Fig 2). Zone A is the area from the upper margin to the midline of the pedicle. Zone B is the area from the midline to the lower margin of the pedicle. Zones C and D are the area from the lower margin of the pedicle to the lower endplate, with zone C comprising the upper half and zone D, the lower half. The vertebral puncture area in vertebroplasty by the extrapedicular approach and the insertion area for the endoscopic device by the percutaneous transforaminal approach are located within the posterior one-third area of the vertebral body. We, therefore, analyzed the pathways and locations of segmental arteries in this area. We designated segmental arteries from T8 to L1 as “high-level segmental arteries” and those from L2 to L4 as “low-level segmental arteries.” We compared the distribution of segmental arteries between these 2 groups.
Fig 2.
The pathways of segmental arteries were classified into 4 zones (A, B, C, and D).
For analyses of anatomic variation, we defined “agenesis of the segmental artery” as the absence of that artery on both 3D-CT images and axial source CT images and “dual supply” as the branching of 1 segmental artery to supply 2 vertebral bodies.
We also evaluated the rate of occurrence of the artery of Adamkiewicz and the proportion of patients for whom the angiographic evaluation changed the plan for surgery.
Statistical Analysis
Three observers independently viewed 3D reconstruction images from spinal CT angiography and determined the pathway zones and locations of the segmental arteries by using a PACS system (PiViewSTAR 5.0; INFINITT, Seoul, Korea). We measured interobserver agreement by using weighted κ statistics. The Pearson χ2 test was used to compare the high- and low-level segmental artery groups. Calculations were performed with the Statistical Package for the Social Sciences, Version 12.0 for Windows (SPSS, Chicago, Illinois).
Results
In all 41 patients, spinal CT angiography clearly depicted the spinal segmental arteries (Fig 1). The 3D reconstruction images showed arterial pathways on the vertebral bodies and the anatomic relationships of segmental arteries and bony structures.
Most of the segmental arteries (654 of 738, 88.6%) passed the middle portion of the vertebral body (zones B and C, Table 1). However, 51 of the 738 (6.9%) had uncommon pathways (zones A and D, Table 1). The incidence of uncommon pathways was 30 of 241 (12.5%) in low-level segmental arteries, significantly higher than that in high-level segmental arteries (21 of 464 or 4.5%, P < .05; Table 2). The safe puncture zones of thoracic vertebral bodies were slightly above or below zones B and C, and those for lumbar vertebral bodies, slightly above zone B. When we classified pathways and locations of segmental arteries, we found excellent interobserver agreement (κ value=0.895).
Table 1:
Distribution of pathways of segmental arteries
| Zone | T8 (%) | T9 (%) | T10 (%) | T11 (%) | T12 (%) | L1 (%) | L2 (%) | L3 (%) | L4 (%) | Total (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| A | 0 | 1 | 1 | 2 | 3 | 2 | 0 | 1 | 2 | 12 |
| (0) | (1.2) | (1.2) | (2.4) | (3.7) | (2.4) | (0) | (1.2) | (2.4) | (1.6) | |
| B | 13 | 13 | 10 | 14 | 31 | 46 | 38 | 19 | 8 | 192 |
| (15.9) | (15.9) | (12.2) | (17.1) | (37.8) | (56.1) | (46.3) | (23.2) | (9.8) | (26.0) | |
| C | 68 | 65 | 65 | 59 | 36 | 23 | 38 | 52 | 56 | 462 |
| (82.9) | (79.3) | (79.3) | (72.0) | (43.9) | (28.0) | (46.3) | (63.4) | (68.3) | (62.6) | |
| D | 0 | 1 | 3 | 5 | 3 | 0 | 4 | 10 | 13 | 39 |
| (0) | (1.2) | (3.7) | (6.1) | (3.7) | (0) | (4.9) | (12.2) | (15.9) | (5.3) | |
| Agenesis | 1 | 2 | 3 | 2 | 9 | 11 | 2 | 0 | 3 | 33 |
| (1.2) | (2.4) | (3.7) | (2.4) | (11.0) | (13.4) | (2.4) | (0) | (3.7) | (4.5) |
Table 2:
Comparison of the incidence of uncommon pathway of segmental arteries
| High-Level Segmental Arteries (from T8 to L1) | Low-Level Segmental Arteries (from L2 to L4) | |
|---|---|---|
| Common pathway (zones B and C) | 443 (95.5%) | 211 (87.5%) |
| Uncommon pathway (zones A and D)a | 21 (4.5%) | 30 (12.5%) |
P < .05, Pearson χ 2 test.
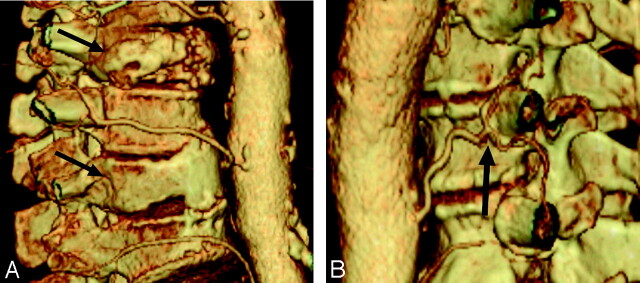
Of the 2 types of anatomic variations observed, agenesis occurred in 33 (4.5%) of 738 segmental arteries (Fig 3 A), and dual supply, at 11 sites in 11 (26.8%) of the 41 patients (Fig 3B).
Fig 3.
Anatomic variations of segmental arteries. A, Agenesis of a segmental artery (arrows). B, Dual supply (1 segmental artery supplies 2 vertebrae, arrow).
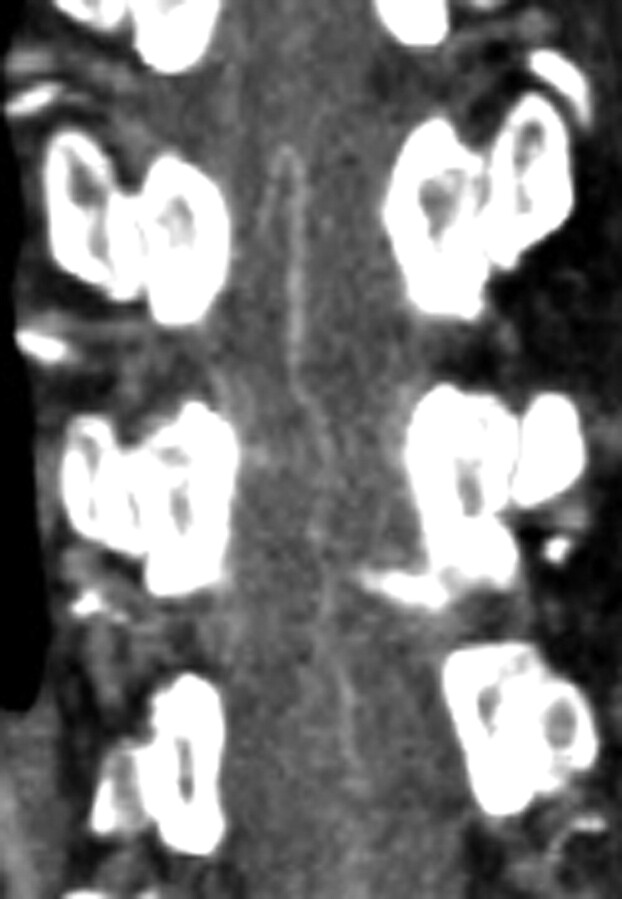
We observed arteries of Adamkiewicz (Fig 4) in 17 of the 41 patients (41.5%). For 2 of the 41 patients (4.9%), spinal CT angiography led to a change in the surgical approach. Extrapedicular vertebroplasty was changed to a transpedicular approach in 1 patient, and the percutaneous endoscopic lumbar approach was changed to an open paramedian approach in 1 patient to minimize the risk of vessel injury due to uncommon pathways of the segmental arteries (Figs 5 and 6).
Fig 4.
Coronal reconstruction CT image showing an artery of Adamkiewicz.
Fig 5.
Radiologic images of a 65-year-old patient with left-sided L4 radiculopathy. A, MR image shows left-sided extraforaminal disk herniation at the L4-5 area (arrow). B and C, Axial source images of CT angiography and 3D-CT show that the left L4 segmental artery passes close to a herniated disk particle and the intervertebral foramen (arrows).
Fig 6.
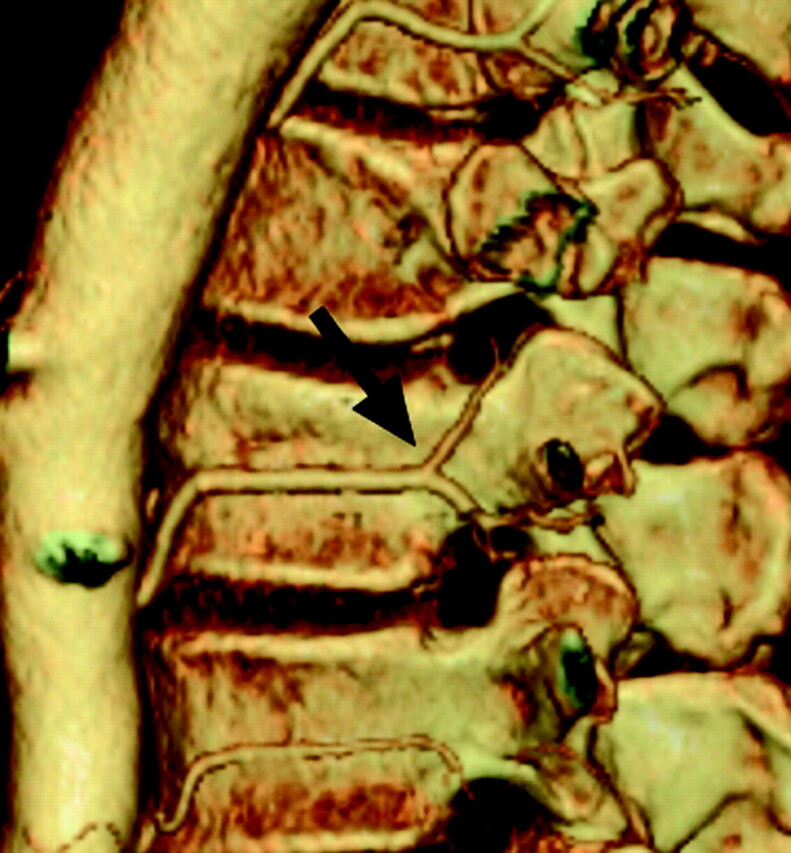
Uncommon location of a segmental artery. 3D-CT shows that the left L1 segmental artery is bifurcated and passes though zones A and B (arrow). Extrapedicular vertebroplasty may have a high risk of vessel injury in this case.
Discussion
Even minimally invasive spinal surgeries, such as transforaminal endoscopic lumbar diskectomy and extrapedicular vertebroplasty, may potentially injure segmental arteries and cause retroperitoneal hematomas.3,4,6 With the patient under regional anesthesia, one can monitor nerve root injury as patients complain of radiating pain or tingling.7 Segmental artery injury may not be monitored, however, and symptoms develop only after surgery. Reports of arterial injury and hematoma after minimally invasive operations are a cause for concern.3,4,6 Our results also show a significantly higher frequency of segmental arteries with uncommon pathways at L2 through L4, a region in which percutaneous transforaminal endoscopic diskectomy is frequently attempted. This finding supports the routine practice at our institution of performing spinal CT angiography and reviewing the anatomic structure of segmental arteries before minimally invasive operations and anterior approaches. The locations and pathways of these arteries may sometimes indicate a change in the surgical plan (Figs 5 and 6).
Although intravenous CT angiography has diverse clinical applications, its use in spinal disease is limited. This noninvasive technique encounters few complications, usually related to injection of the contrast medium (nausea and flush), as we observed. 3D reconstruction CT images show the pathways and locations of arteries on the vertebral body. Conventional angiography can also show these arteries, but this invasive technique carries greater risk for complications. MR angiography can display segmental arteries and the artery of Adamkiewicz but does not provide a clear contour of the vertebral body. We suggest that 3D-CT images bear closer resemblance to the surgical view than MR images.
The recent development of extrapedicular vertebroplasty or kyphoplasty may facilitate treatment at the smaller thoracic vertebrae because puncture occurs at the vertebral body rather than at the pedicle.7–10 This procedure uses a cannula with a relatively large diameter, compatible with low pressure and a high-viscosity filler material, which may decrease complications related to filler leakage.9 Despite these advantages, the extrapedicular approach may injure the segmental artery. In 1 of our patients, a large retroperitoneal hematoma formed after extrapedicular vertebroplasty. This patient received sonography-guided hematoma aspiration following endovascular embolization of the affected segmental artery. We suggest that spinal CT angiography may help to determine a safe puncture area on the vertebral body and guide the decision between transpedicular and extrapedicular approaches.
The artery of Adamkiewicz provides important supplemental blood flow to the thoracic spinal cord, and injury to this artery may lead to cord infarction with severe neurologic outcomes such as paraplegia.11,12 The artery of Adamkiewicz is susceptible to injury in anterior surgical approaches to the thoracolumbar junction, and we suggest that spinal CT angiography may help prevent this complication. CT angiography of the artery of Adamkiewicz has been used in the preoperative evaluation for vascular surgery and endovascular treatment of the aorta.11,12 In our protocol, the concentration and injection rate of the contrast medium (see “Materials and Methods”) were important for a clear image of the artery of Adamkiewicz.11,12
Advantages of spinal CT angiography include its noninvasiveness and capacity to produce coronal, sagittal, and 3D images as well as axial images. The 3D images were similar to the operative anatomy and easy to interpret. For patients with abnormal renal function or iodine hypersensitivity, however, CT angiography should not be used.
Conclusions
We suggest that spinal CT angiography can help to precisely visualize the spinal segmental arteries and surrounding bony structures and can aid clinicians in deciding on optimal approaches for spinal surgery. The clear demonstration of the arteries and surrounding bony structures in 3D reconstructions may also help in planning spinal surgeries, such as endoscopic procedures or a lumbar paramedian, transthoracic, or retroperitoneal approach. Also, our findings suggest that 3D reconstruction imaging provides a simple reliable method for determining the puncture site (safety zone) for extrapedicular vertebroplasty and thereby minimizes the risk for segmental artery injury.
Footnotes
This work was supported by the BioGreen21 Program (200810FTH010103002 and 200810FTH010102001) of the Rural Development Administration.
References
- 1. Hong JT, Park DK, Lee MJ, et al. Anatomical variations of the vertebral artery segment in the lower cervical spine: analysis by three-dimensional computed tomography angiography. Spine 2008; 33: 2422– 26 [DOI] [PubMed] [Google Scholar]
- 2. Inamasu J, Kim DH, Logan L.. Three-dimensional computed tomographic anatomy of the abdominal great vessels pertinent to L4–L5 anterior lumbar interbody fusion. Minim Invasive Neurosurg 2005; 48: 127– 31 [DOI] [PubMed] [Google Scholar]
- 3. Ahn Y, Kim JU, Lee BH, et al. Postoperative retroperitoneal hematoma following transforaminal percutaneous endoscopic lumbar discectomy. J Neurosurg Spine 2009; 10: 595– 602 [DOI] [PubMed] [Google Scholar]
- 4. Gleason TF, McCarthy PL, Butler JP, et al. Arterial injury following percutaneous vertebral augmentation: a case report. Spine 2006; 31: E 84– 87 [DOI] [PubMed] [Google Scholar]
- 5. Inamasu J, Guiot BH.. Vascular injury and complication in neurosurgical spine surgery. Act Neurochir (Wien) 2006; 148: 375– 87 [DOI] [PubMed] [Google Scholar]
- 6. Kim HS, Ju CI, Kim SW, et al. Huge psoas muscle hematoma due to lumbar segmental vessel injury following percutaneous endoscopic lumbar discectomy. J Korean Neurosurg Soc 2009; 45: 192– 95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ryu K, Park C, Kim M, et al. Single balloon kyphoplasty using far-lateral extrapedicular approach: technical note and preliminary results. J Spinal Disord Tech 2007; 20: 392– 98 [DOI] [PubMed] [Google Scholar]
- 8. Boszczyk BM, Bierschneider M, Hauck S, et al. Transcostovertebral kyphoplasty of the mid and high thoracic spine. Eur Spine J 2005; 14: 992– 99 [DOI] [PubMed] [Google Scholar]
- 9. Cho Y, Choi J, Cho S.. Vertebroplasty utilizing percutaneous vertebral body access (PVBA) technique for osteoporotic vertebral compression fractures in the middle thoracic vertebrae. J Korean Neurosurg Soc 2007; 41: 161– 65 [Google Scholar]
- 10. Chung YS, Eun JS, Kim C, et al. Extrapedicular approach of percutaneous vertebroplasty in the treatment of upper and mid-thoracic vertebral compression fracture. Act Radiol 2005; 46: 280– 87 [DOI] [PubMed] [Google Scholar]
- 11. Nakayama Y, Awai K, Yanaga Y, et al. Optimal contrast medium injection protocols for the depiction of the Adamkiewicz artery using 64-detector CT angiography. Clin Radiol 2008; 63: 880– 87 [DOI] [PubMed] [Google Scholar]
- 12. Utsunomiya D, Yamashita Y, Okumura S, et al. Demonstration of the Adamkiewicz artery in patients with descending or thoracoabdominal aortic aneurysm: optimization of contrast-medium application for 64-detector-row CT angiography. Eur Radiol 2008; 18: 2684– 90 [DOI] [PubMed] [Google Scholar]