Abstract
BACKGROUND AND PURPOSE:
Revascularization of large cerebral artery occlusion is the therapeutic goal in stroke therapy. Currently, many recanalization devices are in clinical use. This study compares the outcome parameters, efficacy, and safety of the new generation of stent-retriever devices with the well-established Merci retriever.
MATERIALS AND METHODS:
All patients who received endovascular mechanical recanalization therapy were prospectively registered. One hundred twenty-two patients were treated with either new stent retrievers, including the Trevo and Solitaire devices, or the Merci retriever system. Recanalization of the occluded vessel was assessed in accordance with the modified TICI score, and outcome parameters, including the NIHSS and mRS scores, were documented. Clinical status was recorded after neurointervention, at time of discharge, and after 90 days.
RESULTS:
The mean age of all patients was 68 years; 54% were male, with no statistical differences in demographics between both groups. Successful recanalization (TICI 3 and TICI 2b) was achieved in 82% of patients treated with stent retrievers compared with 62% of patients treated with Merci retrievers (P = .016). In the 90-day follow-up, 65% of patients treated with stent retrievers and 35% of those treated with the Merci had achieved a good (mRS = 0–2) clinical outcome (P = .002). Patients treated with stent retrievers had a significantly shorter treatment time (72 versus 122 minutes, P < .01) and less severe intracerebral hemorrhages (10% versus 28%, P < .01).
CONCLUSIONS:
Patients treated with Trevo and Solitaire stents had a better revascularization rate, better clinical outcome, and lower complication rate than patients treated with the Merci retriever.
There have been numerous advances in cerebral revascularization strategies for acute ischemic stroke during the past decade. The clinical impact of salvaging penumbral tissue in acute ischemic stroke continues to drive the quest for increasingly more effective revascularization strategies.1
The only proved drug therapy for acute ischemic stroke is still thrombolysis with recombinant tissue plasminogen activator, which has been proved in many clinical trials to be effective in improving clinical outcome.2,3 Treatment of large cerebral artery occlusion still remains a challenge because intravenous thrombolysis reaches its limit.1
Ever since the publication of some promising data from the Prolyse in Acute Cerebral Thromboembolism II trial, in which a recanalization rate of 66% was achieved, several other trials have shown the efficacy of a mechanical approach.4–9
The MERCI and Multi MERCI trials demonstrated that thrombectomy is technically efficacious in achieving recanalization in large cerebral artery occlusions with or without bridging therapy with intravenous thrombolysis.4,10–12 The most recent thrombectomy devices are the stent retrievers, most notably Trevo (Concentric Medical, Mountain View, California) and Solitaire (ev3, Irvine, California), promising even better outcomes by combining elements of a stent scaffold to engage the clot with the existing retrieval concept.1,13
Patient selection, type of device, and adjunctive therapies, including intra-arterial and intravenous thrombolysis, add to the complexity of stroke therapy and make comparisons across various studies difficult. The potential impact of device selection on patient outcomes is best explored through a dataset in which all other screening, treatment, and follow-up variables are controlled as much as possible. The entire cohort analyzed in this article was treated in a single center, consistently following the same protocol.
This is the first comparison that analyzes the clinical outcome and angiographic results between patients treated with the Merci retriever (Concentric Medical) or stent-retriever devices.
Materials and Methods
Study Population
All patients with stroke who were admitted to our stroke unit with large cerebral artery occlusion were registered prospectively in a nationwide data base. One hundred twenty-two patients treated with either the Merci retriever or with a stent retriever between September 2006 and March 2011 were analyzed for this study.
Our data base includes demographic characteristics, time of onset of symptoms, and baseline and follow-up stroke severity, measured by NIHSS information on functional outcome at discharge (7–14 days after stroke onset) and at 90 days by the mRS. Good clinical outcome was defined as mRS 0–2,14 and death was recorded as mRS 6. Clinical progress was documented by a stroke neurologist.
Classification of Recanalization
EMR of the primary large cerebral artery occlusion was assessed by the TICI score.15,16 Success was defined as a score of TICI 2b or 3.
Radiologic Investigations
All patients were assessed by using CT, including a CTA on admission, or MR imaging with perfusion-weighted sequences and DWI and MRA. Large cerebral artery occlusion, defined as complete obstruction of the flow in the ICA, MCA, or BA, was confirmed in all cases.
The first follow-up CT was performed within 24 hours after thrombectomy or at the time of clinical deterioration. Complications, including ICH and the need for decompressive surgery due to space-occupying infarctions, were documented. An ICH was defined as severe when an increase of ≥4 points in the NIHSS score within 24 hours in concordance with the evidence of any blood on the 24-hour head CT/MR imaging was documented. Intracerebral hemorrhagic transformation in the infarction area without clinical deterioration was defined as mild or moderate.
Treatment
Patients admitted to our stroke unit were treated according to stroke guidelines.2 Patients without contraindication received IVT as a bridging concept based on the European Cooperative Acute Stroke Study III.2,3,17,18 In our internal guidelines, the time window was extended up to 12 hours in patients with BA occlusion if unconsciousness was <4 hours. If indicated, the patient was transferred immediately to the angiography suite under bridging therapy. Patients with undefined symptom onset beyond 4.5 hours were treated with EMR only if a mismatch in MR imaging was diagnosed. Treatment time was recorded and defined from arterial access to the end of the procedure.
Device Selection
The selection of the respective clot retriever was determined by the chronologic order of availability of each device. It was not dependent on the patient's symptoms and history or doctor's preference. Because the Merci retrieval system was primarily obtainable, all patients were consecutively treated with this device. In 2009, the Solitaire stent became the next available thrombectomy device. From that time on, all patients were consecutively treated with the Solitaire device. Since 2011, the Trevo retriever was used routinely in our institution. Since then, we have treated all patients included in this study consecutively with the Trevo device.
Description of Clot-Retriever Devices
The Merci retriever system is a nitinol wire with an imprinted shape-memory effect covered with a platinum coil to improve the visibility under fluoroscopy. It is inserted through a braided microcatheter to a position distal to the thrombus. After release from the microcatheter, it assumes a shape similar to a corkscrew and has to be slowly pulled back under continuous aspiration via the guiding catheter.19
The main component of stent-retriever devices (Solitaire and Trevo retrievers) is a stent-like mesh of wires, attached to a core wire and delivered through a microcatheter. Trevo and Solitaire can create a temporary endovascular bypass after expansion into the clot. Additionally, Trevo has a stent cell geometry specifically designed to integrate the clot into the stent structure for clot removal.1,13
Endovascular Procedure
DSA was performed on a biplane high-resolution angiography system (Artis zee; Siemens, Erlangen, Germany) via a femoral approach. All procedures were performed exclusively by 1 neurointerventionalist (M.K.-O.) with the patient under general anesthesia.
Routinely, a 6F guiding catheter (Envoy; Cordis, Miami Lakes, Florida) was placed with the help of a guidewire (Radifocus Guide wire angled; MicroVention Terumo, Aliso Viejo, California) into the targeted artery. Using standard cerebral catheterization techniques, we guided the respective microcatheter (Merci or Trevo 18; or Rebar, ev3) into the occluded vessel and passed beyond it the thrombus. In cases with tortuous vessels, a long sheath (Strada; St. Jude, Minnetonka, Minnesota) was used because it gives better support during catheter manipulation and has the possibility of using a distal access catheter (DAC; Concentric Medical).
According to our preference, a DAC 044 or 057 was used as a coaxial system to increase the stability of the microcatheter. The microcatheter and DAC were navigated together and placed just proximal to the clot to apply suction directly at the proximal face of the clot instead of at the guiding catheter. A selective angiogram with 1–2 mL of contrast was obtained distal to the thrombus to evaluate the distal vasculature and verify the correct position of the microcatheter.
Procedure by Using the Merci Retriever
In cases using the Merci retriever, the retriever was advanced through the microcatheter and several of the helical loops were deployed distal to the thrombus. The Merci retriever was then retracted to the face of the thrombus, and the proximal loops were then deployed within the thrombus. The Merci retriever with the ensnared thrombus and the microcatheter were withdrawn together into the guide catheter lumen or DAC. Manual aspiration with a 50-mL syringe was performed through the hemostatic valve during retrieval to reverse the flow and to aspirate clot debris present in the lumen of the guide catheter or DAC, respectively.
Procedure by Using Stent Retrievers
In cases using a stent retriever, the device was placed in the same manner as the Merci retriever, distal to the clot. Then the microcatheter was retracted to a position where the distal marker was aligned with the proximal marker of the stent. On device deployment, an angiographic control was performed to evaluate the correct placement and expansion of the device. After the angiographic run, the device was maintained in place for a few minutes (1–4 minutes) to allow device expansion and clot integration. After this time, the fully deployed device and the delivery microcatheter were gently pulled back together and recovered through the guiding catheter or DAC. The integrity of the stent was consistently checked after every pass. Continuous aspiration was applied during the retrieval maneuver, as described above. If, after several passes (4–6) with either the Merci or stent-retriever devices, no obvious clot removal was realized, another clot retriever device was used for the next pass. In case of a proximal high-grade stenosis of the ICA, a carotid stent was placed, to gain access to the distal territory. At the end of the procedure, an Angio-Seal 6F (St. Jude Medical) vessel closure system was used.
Therapies Additional to Thrombectomy
If not contraindicated and if a 100% reperfusion was not achieved by the first pass, during the following passes, additional intra-arterial delivery of tPA (IAT) (Actilyse; 2–20 mg) or abciximab (ReoPro; 1–5 mg) was performed. In instances in which an underlying stenosis was noted at the occlusion site or a very hard thrombus could not be removed, a stent was implanted. In cases of acute stent placement, a bolus of abciximab (0.5 mg/kg) was given, half intra-arterial and half intravenous. Then, continuous intravenous application of 0.125 μg/kg/min of abciximab was given for 24 hours. The first day after the procedure, oral medication with acetylsalicylic acid, 100 mg, and clopidogrel (Plavix), 75 mg, was started if there was no contraindication seen in the 24-hour postprocedural CT scan.
Statistical Analysis
Descriptive statistics such as means, percentages, and ranges were computed for several variables. The Fisher 2-sided exact test was used to compare percentages between the Merci and Trevo/Solitaire group. A repeated-measures ANOVA with 1 fixed effect (Merci versus stent retriever) was used together with 2-sided unpaired Student t tests post hoc to compare both groups over time. A whisker-plot with 95% confidence intervals was used to illustrate the mean NIHSS scores between both groups with time. A P level < 5% indicated a statistically significant difference. All analyses were done by using Statistica 6.1 (2004) (StatSoft, Tulsa, Oklahoma) and Mathematica 7.0 (2008) (Wolfram Research, Champaign, Illinois).
Results
Among the 122 patients included in this study, 49% (60/122) were treated with Merci retriever devices, and 51% (62/122), with stent retrievers. Because there were no significant statistical differences, we put the patients treated with the Solitaire and Trevo devices into 1 group. Patients treated with Merci had a mean age of 65 years, including 50% women, and a mean NIHSS score at admission of 17. In the patients treated with stent retrievers, the mean age was 68 years, including 58% women, and the mean NIHSS score at admission was 17. The On-line Table shows that there were no statistically significant differences in age, sex, or admission NIHSS score between both groups. Only a small difference was found in the number of patients with ICA and MCA occlusions. A detailed demographic overview is summarized in the On-line Table.
Time to Treatment
Eighteen percent of the stent-retriever cohort and 8% of the Merci cohort had fluctuating symptoms and unclear symptom onset. According to the last known well time, the mean time from symptom onset to treatment in the stent-retriever cohort was 3 hours and 30 minutes (range, 40 minutes–10 hours and 30 minutes); and in the Merci cohort, it was 4 hours and 26 minutes (range, 1 hour and 55 minutes–16 hours) (P = .23).
Occluded Vessels
MCA occlusion was documented in 58% of the stent-retriever group and in 62% of the Merci group. ICA and MCA occlusions occurred in 29% of the stent-retriever cohort and 13% of the Merci cohort, whereas 13% of the patients treated with stent retrievers and 25% of those treated with Merci were documented with BA occlusion.
Additional Medical Lytic Treatment
IVT as a bridging therapy was performed in 42% of the patients treated with a stent retriever and in 13% of the patients treated with Merci. Synergistic treatment of EMR and IAT was documented in 15% of patients treated with the stent retriever and in 27% of patients treated with the Merci retriever. A combination of IVT, EMR, and IAT was documented in 27% of the patients treated with the stent retriever and in 55% of the patients treated with Merci. Isolated EMR treatment was documented in 16% of the stent-retriever group and in 5% of the Merci-treated group.
DAC Usage
In 26% (16/62) of the patients treated with a stent retriever and in 30% (18/60) of the patients treated with Merci, a DAC was additionally used.
Additional Thrombectomy Devices
Among the patients treated with the stent retriever, 1 patient (2%) was treated additionally with the Phenox clot retriever (phenox, Bochum, Germany). Among the patients treated with the Merci device, 17% were treated with additional devices. Two were treated with the Solitaire device; another 6, with the Catch system (Balt, Montmorency, France); and another 2, with the Phenox system (Bochum, Germany).
Additional Stents
The additional use of intracranial and/or extracranial stents was necessary in 13% (8/62) of the patients treated with a stent retriever and 15% (9/60) of the patients treated with Merci (P = .72).
Angiographic Outcome
Successful recanalization (TICI 3 and TICI 2b) could be achieved in 82% of the patients treated with stent retrievers and in 62% of the patients treated with Merci retrievers (P = .016). A detailed analysis of all TICI results is given in the On-line Table.
Treatment Time
The mean procedural duration, defined as the time from the arterial puncture to the final angiogram, was 72 minutes (range, 10–166 minutes) for the stent-retriever cohort. This was significantly shorter than the procedural duration for patients treated with Merci (122 minutes; range, 55–200 minutes; P < .01).
We noticed that patients who needed a longer treatment time were treated additionally with stent placement and angioplasty or needed more steps for recanalization. Overall, we documented, for revascularization, a mean of 2.5 passes (range, 1–6 steps) by using stent-retriever devices and 3.3 passes (range, 1–10) by using the Merci device (P = .003). One pass procedure was documented in 19% (12/62) of patients treated with a stent retriever and in 10% (6/60) of patients treated with the Merci retriever (P = .16).
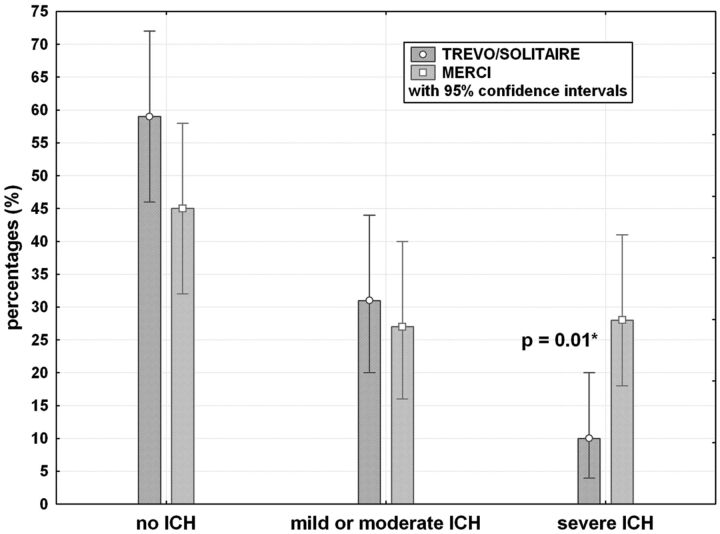
Complications
Severe ICH occurred in 10% (6/62) of the patients treated with a stent retriever and in 28% (17/60) of the patients treated with Merci (P = .01). A slight hemorrhagic transformation of the cerebral infarction was documented in 31% (19/62) of patients treated with a stent retriever compared with 27% (16/60) of patients treated with Merci (P = .629) (Fig 1). Decompressive surgery was necessary because of EMR failure and space-occupying infarction in 5% of the patients treated with stent retriever and in 17% of the patients treated with Merci (P = .035). Procedural complications were documented in 1 patient treated with the Merci retriever and in none of the patients treated with stent retriever.
Fig 1.
Overview of occurrence of ICH in patients treated with the Merci retriever and stent retrievers.
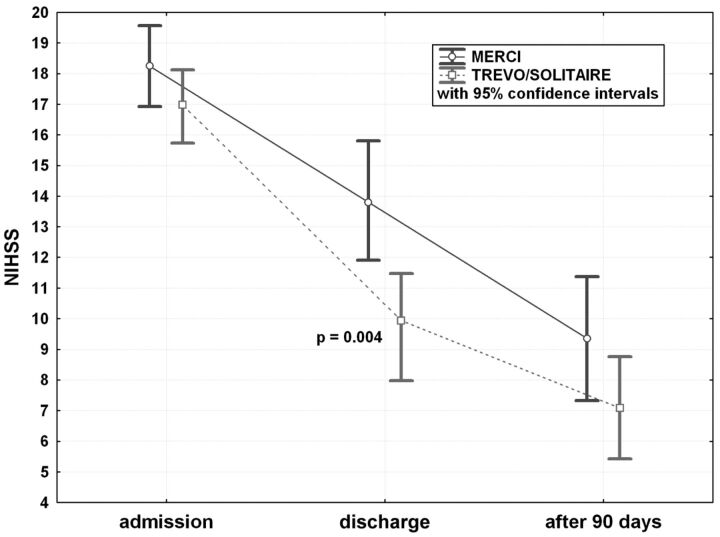
Clinical Outcome
At the time of discharge, patients treated with a stent retriever had a mean NIHSS of 10, and patients treated with Merci had a mean NIHSS of 14 (Fig 1, P = .004). After 90 days, 55 patients treated with a stent retriever (1 was lost to follow-up and 1 was deceased) and 40 patients treated with Merci (1 was lost to follow-up and 4 were deceased) completed the 90-day examination. At this time, we documented a good outcome (mRS ≤ 2) in 59% of the patients treated with stent retrievers and in 25% of patients treated with the Merci retriever (P < .003). A detailed analysis of the outcome parameters is given in Fig 2 and the On-line Table. The overall mortality rate was 10% (6/61) in the stent-retriever cohort and 30% (17/57) in the Merci cohort (P < .01).
Fig 2.
Categorized whisker plots of mean NIHSS scores at admission, at discharge, and after 90 days in both groups.
Discussion
Large cerebral vessel occlusion in ischemic stroke is associated with a high degree of morbidity. When intravenous thrombolysis fails, mechanical thrombectomy can provide an alternative or synergistic method for flow restoration.20–22
The MERCI and Multi MERCI trials demonstrated for the first time that thrombectomy is technically efficacious in achieving recanalization and improving outcome of patients with severe stroke.10–12,23 In the years following the introduction of the Merci retriever, numerous new devices for thrombectomy have been developed. One of the newest developments is the stent-retriever device. In several single-center studies, promising results for the Solitaire device have been reported.24,25 In the United States, the SOLITAIRE FR With the Intention For Thrombectomy Study is now ongoing, aiming to demonstrate substantial equivalence of the Solitaire device to the Merci device.26
Promising data from the Trevo stent-retriever device has been presented at numerous meetings, but to date, no case series have been published, to our knowledge. The Thrombectomy Revascularization of Large Vessel Occlusions in acute ischemic stroke trial has just recently completed enrollment,13 and an animal study has shown good recanalization results (TICI 2–3) by using the Trevo device.27 In the United States, the Trevo stent retriever is being studied in a randomized trial comparing it with the Merci device.28 Our article is the first study, to our knowledge, that compares the different technical and clinical results in patients treated with either the well-known Merci retriever system or the new stent-retriever devices.
Angiographic and Clinical Outcome
An overall good recanalization (TICI 3 and TICI 2b) was documented in 82% of patients treated with stent retrievers and in 62% of patients treated with Merci. A significantly better complete recanalization rate (TICI 3) could be demonstrated in 53% of patients treated with a stent retriever compared with 30% of patients treated with Merci (P = .016).
In concordance with our findings, the Solitaire studies in 90% (n = 20), 84% (n = 50), or even in 100% (n = 8) of patients showed successful recanalization29,31 and the MERCI trial reported partial or complete recanalization in 54% of subjects.4
A recently published Solitaire study reported a mean procedural duration of 50 minutes.30 Another Solitaire study reported a recanalization time of 45 minutes.29 In the MERCI and Multi MERCI trials, the documented mean procedural duration was 96 minutes.10,12 In accordance with these results, our patients treated with stent retrievers had a significantly shorter treatment time than patients treated with the Merci retriever (72 versus 122 minutes, P = < .001). In 52% of our patients treated with stent retrievers, a complete recanalization could be reached within a 45-minute interventional time, according to the formerly mentioned study. A recently published Solitaire study reported a mean number of passes of 1.4 in 20 patients, and the MERCI and Multi MERCI trials reported 2.1 passes in MCA M2 and 3.1 in MCA M1 occlusions of 178 analyzed patients.31 Overall, patients treated with stent retrievers were documented with significantly fewer procedural passes than patients treated with the Merci device (P = .003). A trend toward more 1-pass procedures was documented in patients treated with stent retrievers than those treated with the Merci device (18% versus 10%; P = .16).
The first results of previous Solitaire studies revealed a higher recanalization rate but only slightly better outcome in 54% (n = 50), in 33.3% (n = 18), or in 42% (n = 26) of patients than the results of the Merci trials have shown.1,24,32 The MERCI trial revealed, in 27.7% of 151 analyzed patients, a good clinical outcome (mRS ≤ 2) at 90 days, whereas the Multi MERCI trial reported good outcomes in 36% of 164 analyzed patients.10,12 We could demonstrate that patients treated with stent retrievers showed a significantly better clinical outcome (mRS 0–2) than patients treated with the Merci retriever (59% versus 25%), after 90 days of follow-up (P = .002), but still we had a high discrepancy between the excellent recanalization rate and the percentage rate of good clinical outcome.
Adjunctive Therapeutics
In our patients, we used a high rate of adjunctive therapeutic strategies. Overall, we had a higher rate of patients treated with stent retrievers who received bridging therapy (42% versus 13%), whereas patients treated with the Merci retriever were documented as more frequently receiving IAT than patients treated with stent retrievers (27% versus 15%, P = .09). Fewer patients treated with stent retrievers had to be treated with a combination of IAT and IVT than patients treated with Merci (27% versus 55%, P = .002). To some degree, these differences reflect our own learning process with time, which showed us that bridging therapy may gap the time until the patient arrives in the angiography suite.
The more frequent use of IAT or the combination of IAT and IVT in patients treated with the Merci retriever could be an explanation for their higher bleeding rate in accordance with the results of Prolyse in Acute Cerebral Thromboembolism II, which demonstrated hemorrhagic infarction in 45% of patients, 17% being severe ICH (n = 108).33
Complications and Mortality Rate
Recently published Solitaire studies documented ICH in 40% (8/20), in 14% (3/22), and in 8% (2/26).1,30,34 The Multi MERCI trial reported a symptomatic ICH rate of 9.8% and an asymptomatic ICH rate of 30.5%.12 Although we treated many patients with adjunctive therapies, we did not have a higher ICH rate in comparison with other studies.
In our patients, significantly fewer patients treated with stent retrievers (10%) (P = .01) were documented with severe ICH than patients treated with the Merci retriever (28%). Intracerebral hemorrhage in the infarction area without clinical deterioration was similar to that in previous studies (31% for stent retrievers and 27% for Merci; P = .63). An explanation for these lower severe rates of cerebral bleedings in the stent-retriever cohort may be that fewer vessel injuries seem to occur with stent retrievers, but this is just speculation.
Several studies revealed that ICH is a predictor of bad outcomes in patients with stroke.35 Despite the high ICH rate in our patients, we saw a high rate of good clinical outcome after 90 days, especially in the stent-retriever cohort. One of the reasons might be that more patients developed an intracerebral hemorrhage only involving the infarction area. Severe hemorrhage occurred primarily in patients after stent placement and angioplasty due to a reperfusion syndrome.
Solitaire studies documented a mortality rate of 20% or 18.1% during a follow-up period of 90 days.34,36 A recently published study analyzing 50 patients treated with the Solitaire reported a mortality rate of 12%, similar to our results.24 The MERCI and Multi MERCI trials revealed a mortality rate of 31.8% in a cohort of 173 patients.4 Although we treated many patients with adjunctive therapies in both groups, we documented, in the patients treated with stent retrievers, a significantly lower mortality rate in comparison with the patients treated with the Merci retriever (10% versus 28%, P = .012).
Limitations of the Study
Our analyzed patient number was small, though similar to those in previously reported case series. Our results have multiple explanations: First, the procedures were always performed by the same neurointerventionalist gaining more experience with time. Second, the same anesthesiology team performed acute and routine procedures during the working hours. Third, another reason could be the additional use of the DAC in difficult anatomic vessels. The usefulness of the DAC was reported in a recently published article.37 However, we used the DAC in both groups, almost equally often. Fourth, the availability of all necessary imaging tools and the presence of a diagnostic neurointerventionalist for 24 hours improved our patient selection based on an interdisciplinary decision.
Conclusions
Patients treated with stent retrievers had better overall results and shorter procedural duration. Adjunctive therapies such as intravenous and intra-arterial thrombolysis were not associated with a higher bleeding rate.
Supplementary Material
ABBREVIATIONS:
- BA
basilar artery
- EMR
endovascular mechanical recanalization
- IAT
intra-arterial thrombolysis
- ICH
intracerebral hemorrhage
- IVT
intravenous thrombolysis
- MERCI
Mechanical Embolus Removal in Cerebral Ischemia
- mRS
modified Rankin Scale
- TICI
Thrombolysis in Cerebral Infarction
Footnotes
Disclosures: Monika Killer-Oberpfalzer—RELATED: Support for Travel to Meetings for the Study or Other Purposes: Concentric, Comments: Travel expenses for user meeting concerning the Thrombectomy Revascularization of Large Vessel Occlusions in acute ischemic stroke study, UNRELATED: Consultancy: Stryker for an intracranial stent user meeting, and Depuy for an aneurysm workshop, Grants/Grants Pending: MicroVention Terumo,* Comments: research grant, Payment for Lectures (including service on Speakers Bureaus): MicroVention Terumo. *Money paid to the institution.
References
- 1. Miteff F, Faulder KC, Goh AC, et al. Mechanical thrombectomy with a self-expanding retrievable intracranial stent (Solitaire AB): experience in 26 patients with acute cerebral artery occlusion. AJNR Am J Neuroradiol 2011;32:1078–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hacke W, Donnan G, Fieschi C, et al. , for the ATLANTIS Trials Investigators, ECASS Trials Investigators, NINDS rt-PA Study Group Investigators. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet 2004;363:768–74 [DOI] [PubMed] [Google Scholar]
- 3. Hacke W, Kaste M, Bluhmki E, et al. , for the ECASS Investigators. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008;25:1317–29 [DOI] [PubMed] [Google Scholar]
- 4. Josephson SA, Saver JL, Smith WS, for the Merci and Multi Merci Investigators. Comparison of mechanical embolectomy and intraarterial thrombolysis in acute ischemic stroke within the MCA: MERCI and Multi MERCI compared to PROACT II. Neurocrit Care 2009;10:43–49 [DOI] [PubMed] [Google Scholar]
- 5. Yoon W, Park MS, Cho KH. Low-dose intra-arterial urokinase and aggressive mechanical clot disruption for acute ischemic stroke after failure of intravenous thrombolysis. AJNR Am J Neuroradiol 2010;31:161–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mayer TE, Hamann GF, Schulte-Altedorneburg G, et al. Treatment of vertebrobasilar occlusion by using a coronary waterjet thrombectomy device: a pilot study. AJNR Am J Neuroradiol 2005;26:1389–94 [PMC free article] [PubMed] [Google Scholar]
- 7. Nedeltchev K, Remonda L, Do DD, et al. Acute stenting and thromboaspiration in basilar artery occlusions due to embolism from the dominating vertebral artery. Neuroradiology 2004;46:686–91 [DOI] [PubMed] [Google Scholar]
- 8. Qureshi AI, Siddiqui AM, Suri MF, et al. Aggressive mechanical clot disruption and low-dose intra-arterial third generation thrombolytic agent for ischemic stroke: a prospective study. Neurosurgery 2002;51:1319–27 [DOI] [PubMed] [Google Scholar]
- 9. Tomsick T, Broderick J, Carrozella J, et al. , for the Interventional Management of Stroke II Investigators. Revascularization results in the Interventional Management of Stroke II trial. AJNR Am J Neuroradiol 2008;29:582–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Smith WS, Sung G, Starkman S, et al. Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke 2005;36:1432–38 [DOI] [PubMed] [Google Scholar]
- 11. Flint AC, Duckwiler GR, Budzik RF, et al. , for the MERCI and Multi MERCI Writing Committee. Mechanical thrombectomy of intracranial internal carotid occlusion: pooled results of the MERCI and Multi MERCI Part I trials. Stroke 2007;38:1274–80 [DOI] [PubMed] [Google Scholar]
- 12. Smith WS, Sung G, Saver J, et al. Mechanical thrombectomy for acute ischemic stroke: final results of the multi MERCI trial. Stroke 2008;39:1205–12 [DOI] [PubMed] [Google Scholar]
- 13. Revascularization of Large Vessel Occlusions in Acute Ischemic Stroke. http://clinicaltrials.gov/ct2/show/NCT01088672. Accessed November 3, 2011
- 14. Fields JD, Lutsep HL, Smith WS, for the MERCI and Multi MERCI Investigators. Higher degrees of recanalization after mechanical thrombectomy for acute stroke are associated with improved outcome and decreased mortality: pooled analysis of the MERCI and Multi MERCI trials. AJNR Am J Neuroradiol 2011;32:2170–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fields JD, Lindsay K, Liu KC, et al. Mechanical thrombectomy for the treatment of acute ischemic stroke. Expert Rev Cardiovasc Ther 2010;8:581–92 [DOI] [PubMed] [Google Scholar]
- 16. Bamford JM, Sandercock PA, Warlow CP, et al. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1989;20:828. [DOI] [PubMed] [Google Scholar]
- 17. Micieli G, Marcheselli S, Tosi PA. Safety and efficacy of alteplase in the treatment of acute ischemic stroke. Vasc Health Risk Manag 2009;5:397–409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Stemer A, Lyden P. Evolution of the thrombolytic treatment window for acute ischemic stroke. Curr Neurol Neurosci Rep 2010;10:29–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Martinez H, Zoarski GH, Obuchowski AM, et al. Mechanical thrombectomy of the internal carotid artery and middle cerebral arteries for acute stroke by using the retriever device. AJNR Am J Neuroradiol 2004;25:1812–15 [PMC free article] [PubMed] [Google Scholar]
- 20. Schellinger PD, Kohrmann M, Hacke W. Thrombolytic therapy for acute stroke. Handb Clin Neurol 2008;94:1155–93 [DOI] [PubMed] [Google Scholar]
- 21. Goto H, Fujisawa H, Oka F, et al. Neurotoxic effects of exogenous recombinant tissue-type plasminogen activator on the normal rat brain. J Neurotrauma 2007;24:745–52 [DOI] [PubMed] [Google Scholar]
- 22. Kaur J, Zhao Z, Klein GM, et al. The neurotoxicity of tissue plasminogen activator? J Cereb Blood Flow Metab 2004;24:945–63 [DOI] [PubMed] [Google Scholar]
- 23. Gobin YP, Starkman S, Duckwiler GR, et al. MERCI 1: a phase 1 study of mechanical embolus removal in cerebral ischemia. Stroke 2004;35:2848–54 [DOI] [PubMed] [Google Scholar]
- 24. Costalat V, Machi P, Lobotesis K, et al. Rescue, combined, and stand-alone thrombectomy in the management of large vessel occlusion stroke using the Solitaire device: a prospective 50-patient single-center study: timing, safety, and efficacy. Stroke 2011;42:1929–35 [DOI] [PubMed] [Google Scholar]
- 25. Nayak S, Ladurner G, Killer M. Treatment of acute middle cerebral artery occlusion with a Solitaire AB stent: preliminary experience. Br J Radiol 2010;83:1017–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. SOLITAIRE™ FR With the Intention For Thrombectomy. http://clinicaltrials.gov/ct2/show/NCT01054560. Accessed November 3, 2011
- 27. Nogueira RG, Levy EI, Gounis M, et al. The Trevo device: preclinical data of a novel stroke thrombectomy device in two different animal models of arterial thrombo-occlusive disease. J Neurointerv Surg 2012;4:295–300 [DOI] [PubMed] [Google Scholar]
- 28. Randomized Trial Evaluating Performance of the Trevo Retriever Versus the Merci Retriever in Acute Ischemic Stroke. http://clinicaltrials.gov/ct2/show/NCT01270867. Accessed November 3, 2011
- 29. Park H, Hwang GJ, Jin SC, et al. A retrieval thrombectomy technique with the Solitaire stent in a large cerebral artery occlusion. Acta Neurochir (Wien) 2011;153:1625–31 [DOI] [PubMed] [Google Scholar]
- 30. Castaño C, Dorado L, Guerrero C, et al. Mechanical thrombectomy with the Solitaire AB device in large artery occlusions of the anterior circulation: a pilot study. Stroke 2010;41:1836–40 [DOI] [PubMed] [Google Scholar]
- 31. Shi ZS, Loh Y, Walker G, et al. , for the MERCI and Multi-MERCI Investigators. Clinical outcomes in middle cerebral artery trunk occlusions versus secondary division occlusions after mechanical thrombectomy: pooled analysis of the Mechanical Embolus Removal in Cerebral Ischemia (MERCI) and Multi MERCI trials. Stroke 2010;41:953–60 [DOI] [PubMed] [Google Scholar]
- 32. Stampfl S, Hartmann M, Ringleb PA, et al. Stent placement for flow restoration in acute ischemic stroke: a single-center experience with the Solitaire stent system. AJNR Am J Neuroradiol 2011;32:1245–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Roberts HC, Dillon WP, Furlan AJ, et al. Computed tomographic findings in patients undergoing intra-arterial thrombolysis for acute ischemic stroke due to middle cerebral artery occlusion: results from the PROACT II trial. Stroke 2002;33:1557–65 [DOI] [PubMed] [Google Scholar]
- 34. Roth C, Papanagiotou P, Behnke S, et al. Stent-assisted mechanical recanalization for treatment of acute intracerebral artery occlusions. Stroke 2010;41:2559–67 [DOI] [PubMed] [Google Scholar]
- 35. Khatri P, Wechsler LR, Broderick JP. Intracranial hemorrhage associated with revascularization therapies. Stroke 2007;38:431–40 [DOI] [PubMed] [Google Scholar]
- 36. Khalessi AA, Natarajan SK, Orion D, et al. Acute stroke intervention. JACC Cardiovasc Interv 2011;4:261–69 [DOI] [PubMed] [Google Scholar]
- 37. Spiotta AM, Hussain MS, Sivapatham T, et al. The versatile distal access catheter: the Cleveland Clinic experience. Neurosurgery 2011;68:1677–86 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.