Abstract
Anxiety sensitivity (AS) is a promising intervention target due to its relevance to negative health behaviors broadly, and substance use specifically. The aim of the current study was to evaluate the direct and indirect pathways through which elevated AS could relate to recent substance use among a national adolescent sample recruited via social-media. As predicted, AS was indirectly associated with greater likelihood of using alcohol, cigarettes, and electronic nicotine delivery systems in the past-month through anxiety symptoms. Regarding cannabis, AS was directly related to increased likelihood of past-month cannabis use; however, the indirect relation between AS and likelihood of past-month use via anxiety symptoms was not significant. Through chained indirect effects, AS was related positively to past-month alcohol and cannabis use via anxiety symptoms and coping-related motives, and through withdrawal symptoms and coping-related motives. Study findings can be used to generate hypotheses on potential pathways through which AS could prospectively relate to substance use among youth.
Keywords: Anxiety sensitivity, anxiety, cannabis, marijuana, alcohol, nicotine, youth, adolescents
Substance use is common among adolescents, and problematic use often co-occurs with other psychopathology (Brewer et al., 2017; Centers for Disease Control and Prevention, 2016). Indeed, co-occurring disorders consistently increase the risk for problematic substance use (e.g., earlier age of initiation, heavier use, and dependence) and are linked to poorer treatment outcomes (Rowe et al., 2004; Shane et al., 2003). Examination of transdiagnostic mechanisms that have the potential to reduce incidence and prevalence of substance use along with co-occurring disorders is thus an important public health priority (Leventhal & Zvolensky, 2015).
Anxiety sensitivity (AS) is a malleable, cognitive vulnerability factor concerning the fear of the negative consequences of anxiety that has been linked to negative health behaviors broadly, such as sleep dysfunction and anxiety psychopathology, as well as substance use specifically (Noel & Francis, 2011; Otto et al., 2016). Elevated levels of AS are associated with risk of cannabis and alcohol use disorders as well as smoking lapse and relapse among adults (Schmidt et al., 2007; Zvolensky, Stewart, Vujanoyic, Garvic, & Steeves, 2009). As such, AS has been conceptualized as a promising mechanistic variable and potential intervention target.
Individuals with elevated AS may be more prone to use substances to escape or avoid anxiety, more sensitive to the effects of withdrawal symptoms, and more vulnerable to relapse to escape these intolerable symptoms (Bruce et al., 1995; Kushner et al., 2001; Reiss, 1991; Stewart & Kushner, 2001). Based on a synthesis of the available literature, DeMartini and Carey (2011) developed a model in which AS was posited to indirectly contribute to alcohol use problems through the effect of anxiety on maladaptive substance use motives (e.g., drinking to cope). Most recently, Otto and colleagues (2016) proposed a comprehensive framework regarding the influence of AS on the initiation and maintenance of negative health behaviors, including substance use. Specifically, AS may amplify negative affect that is perceived as intolerable, leading to impulsive behaviors such as substance use to lessen or eliminate those negative feelings or sensations. This framework underscored the importance of coping motives in attempting to eliminate the distress, as well as the role of withdrawal symptoms in initiating and perpetuating the problematic cycle. For example, similar to negative affect, AS may intensify withdrawal symptoms, increasing the likelihood of lapse or relapse to escape the distressing state (Brown, Lejuez, Kahler, & Strong, 2002; Zvolensky et al., 2009; Zvolensky, Farris, Guillot, & Levanthal, 2014). Despite solid theory, the empirical work remains mixed.
Broad examination of the empirical literature highlights inconsistent direct relations between AS and substance use and related problems. Some studies have found that adolescents with elevated levels of AS report more problems related to substance use; whereas other studies have not detected associations between AS and substance use outcomes, and some studies have even found negative relations between AS and substance use outcomes (Ali et al., 2016; Bilsky, Feldner, Knapp, Rojos, & Leen-Feldner, 2016; Buckner et al., 2009; Guillot et al., 2019; Levanthal et al., 2016; Malmberg et al., 2013; Malmberg et al., 2010; Wolitzky-Taylor et al., 2015). These equivocal findings might be due, in part, to the different ways in which substance use outcomes have been captured (e.g., frequency of substance use; problems related to substance use; use of substances due to coping-related motives), and the need to examine more comprehensive models. Indeed, no work has yet tested contemporary theory linking AS and substance use through anxiety, withdrawal symptoms, and coping motives among adolescents.
The current investigation aimed to examine the role of AS in substance use among a large sample of adolescents. We hypothesized that 1) elevated AS would be associated with an increased likelihood of using substances (i.e., cannabis, alcohol, combustible cigarettes, and electronic nicotine delivery systems) in the past month through anxiety symptoms, and 2) among users, elevated AS would be related to more days of substance use in the past month through anxiety symptoms, withdrawal symptoms, and coping-related motives. Please see Figures 1a-1b for graphical depictions of the hypothesized models based on prior work synthesizing AS and substance use (Otto et al., 2016; Stewart & Kushner, 2001).
Figures 1a-1b.
Conceptualized indirect relations between AS and substance use outcomes. Conceptual model demonstrating the tested indirect pathways from AS to the substance use outcomes (alcohol, cannabis, cigarettes, electronic nicotine delivery systems). AS = Anxiety sensitivity.
Method
Participants and Recruitment
A nationally-recruited sample of adolescents aged 13–17 years from all geographic regions in the US completed an online survey disseminated through paid advertisements displayed on Facebook and Instagram from January 26th, 2018-April 18th, 2018. A hyperlink within the advertisement about teen health and substance use directed teens to the informed consent page hosted by Qualtrics (Provo, UT). Qualtrics data functions prevented multiple responses from a single individual, ensured no responses from Internet bots, and preserved anonymity by not collecting IP addresses. Adolescents aged 13–17 years who provided consent and correctly answered Qualtrics data quality-check questions were eligible for the survey. Parental consent was waived. Youth who completed the survey were entered into a lottery to win a $10 Amazon gift code. All procedures were approved by the Institutional Review Board.
Survey
A battery of measures was administered using Qualtrics. Substance use questions separately assessed alcohol, cannabis, combustible cigarette, and electronic nicotine delivery systems use frequency, withdrawal symptoms, and motives. A series of questions also assessed AS, anxiety symptoms, and demographic characteristics of age, gender, and race.
Anxiety sensitivity and anxiety symptoms.
The 18-item Child Anxiety Sensitivity Index (CASI; Silverman et al., 1991) (α = .87 for the current sample) used a 3-point Likert-type scale (1 None to 3 A lot) to assess global anxiety sensitivity. An example item from the CASI is “When I notice my heart is beating fast, I worry that there might be something wrong with me.” The anxiety subscale of the Revised Child’s Anxiety and Depression Scale- Short Version Anxiety Scale was used to index anxiety symptoms (Ebesutani et al., 2012) (α = .89 for the current sample) and asked adolescents to rate how often the anxiety items happened to them using the scale Never, Sometimes, Often, and Always.
Past-month use.
Cannabis use items were administered to assess use of cannabis in the past month (yes/no) and asked those who endorsed using to select the frequency of days used from 0–30 days (Knapp et al., 2018). Similarly, the alcohol use items and nicotine use items measured past month use (yes/no) and frequency of days used for alcohol, combustible cigarettes, and electronic nicotine delivery systems, respectively, in the past month.
Coping motives.
The Marijuana Motives Measure-Coping Motives Subscale (Simons et al., 1998) (α = .88 for the current sample) measured coping-related motives for cannabis use, the Drinking Motive Measure-Coping Factor measured coping-related motives for drinking alcohol (Cooper, 1994) (α = .92 for the current sample), and the Teen Smoking Motives Questionnaire-Coping Factor (Comeau et al., 2000) (α = .87 for the current sample) measured coping-related reasons for smoking cigarettes. All coping factor subscales had a 5-point Likert response scale ranging from Almost Never/Never to Almost Always/Always.
Withdrawal symptoms.
The Revised Marijuana Withdrawal Checklist (MWC; α = .92 for the current sample) (Budney et al., 1999) measured the mood, behavioral, and physical symptoms, from the 4-point Likert scale ranging from None to Severe, related to cannabis withdrawal after adolescents last stopped using cannabis. The Short Alcohol Withdrawal Scale (SAWS; α = .93 for the current sample) (Elholm et al., 2010) measured the physical and psychological symptoms associated with alcohol withdrawal after adolescents last stopped drinking alcohol, with the 4-point Likert scale response options ranging from None to Severe. The Minnesota Tobacco Withdrawal Scale-Revised (MTWS-R; α = .95 for the current sample) (Hughes & Hatsukami, 1986; Toll et al., 2007) measured the severity of withdrawal symptoms, from the 5-point Likert scale ranging from None to Severe, that adolescents experienced after they last stopped using tobacco.
Data Analytic Plan
Descriptive statistics were first conducted in SPSS 25 to assess for nonnormality at the item-level, skew, and kurtosis (West et al., 1995). Mahalanobis distance was computed to assess for multivariate nonnormality with a chi-square (χ2) cut-off of p < .001. The substance use variables were not included in the outlier analysis as they were expected to have a large pile-up of zeroes, reflecting lack of substance use. Models were analyzed with and without multivariate outliers and missing data to determine whether they impacted model results. For use variables, if participants reported not using in the past month, a 0 was carried forward into their past 30 days use variable.
Confirmatory factor analysis (CFA) was conducted in Mplus 8.3 (Muthén & Muthén, 1998–2017) to examine fit for each measurement construct independently. All factors were scaled by setting the factor variance to 1. For factors in which unidimensional and multidimensional models could be fit (i.e., AS, Anxiety), unidimensional, multidimensional, and bifactor models were each fit to the data. Withdrawal and Coping were fit as unidimensional factors. Based on recent recommendations, items with five or more response options were treated as continuous data (AS, Anxiety, Nicotine Withdrawal Symptoms, Coping factors) and items with less than five response options (Alcohol Withdrawal Symptoms, Cannabis Withdrawal Symptoms) were treated as ordinal data (Rhemtulla et al., 2012). Models treating the data as continuous were estimated using robust full information maximum likelihood with Satorra-Bentler (when there was no missing data) and Yuan-Bentler (Y-B; when missing data were present) corrections. Models treating the data as ordinal were estimated using means and variance adjusted weighted least squares (WLSMV in Mplus), which handles missing data using pairwise deletion. Across all models, model fit was assessed using the likelihood ratio test (LRT) based on the χ2. Because the χ2 might suggest rejecting models with minor misspecifications, especially when modeling scale scores as factors (Browne & Cudeck, 1993; Moshagen, 2012), agreement was sought across multiple fit indices. Comparative fit index (CFI) values greater than .90 suggest marginal-to-adequate fit and values greater than .95 suggest adequate-to-good fit. Root mean square error of approximation (RMSEA) values and 90% CI below .08 suggest marginal-to-adequate fit and values below .05 suggest adequate-to-good fit (Browne & Cudeck, 1993; Hu & Bentler, 1998).
Nested CFA models (AS, Anxiety) were compared using the LRT and the appropriate scaling adjustment with a non-significant value indicating the more parsimonious model should be accepted. If the bifactor model fit the data best, additional model indices were examined, including omega hierarchical (ωh), percentage of variance accounted for by the general factor when error variance is excluded (explained common variance [ECV]), the percentage of uncontaminated variance (PUC), and the factor determinacy score. Higher ωh suggests a reliable general factor. ECV and PUC values > .70 suggest that the scale is essentially unidimensional (Rodriguez et al., 2016). A factor determinacy score > .90 suggests the presence of a well-measured factor (Gorsuch, 1983). If there were support for unidimensional AS and Anxiety factors, these models were treated as unidimensional in the final remaining analyses.
Following fit of the CFA models, structural equation modeling (SEM) was conducted to examine indirect pathways from AS to 1) likelihood of past month alcohol use and frequency of days used, 2) likelihood of past month cannabis use and frequency of days used, 3) likelihood of past month cigarette use and frequency of days used, and 4) likelihood of past month electronic nicotine delivery systems use and frequency of days used. Two-part modeling was used to divide past 30 days use variables into the likelihood of using a substance in the past month (0 = no use, 1 = use) and the log-transformed days using that substance. The proposed conceptual model is provided in Figure 1. Indirect effects were tested via the conservative significance test as bootstrapping is not available in Mplus when conducting two-part modeling. In all analyses, age and gender were included as covariates on all outcomes.
Results
Demographic and Substance Use Characteristics
The ads were displayed on 312,461 individuals’ digital devices, of which 5,084 selected the ad and were directed to the survey. The final sample included 1467 adolescents, aged 13–17 years (Mage = 15.75 years, SD = 1.13), who completed the informed consent and correctly answered the data quality-check questions. Self-reported gender included 54.3% female, 33.5% male, 9.2% transgender, and 3.0% other. The racial/ethnic breakdown of the sample was: 58.1% Caucasian/White, 9.1% African American/Black, 10.8% Asian, 9.7% Hispanic, and 12.3% other (e.g., identified with more than one race/ethnicity). All four geographic regions in the United States were represented, with most adolescents reporting residence in the South (35.2%) and West (30.9%), followed by the Midwest (19.1%) and Northeast (14.9%). Data was taken from recent census data to provide comparisons as to the representativeness of our sample. Recent data on gender and geographic regions was available for teenagers between the ages of 15 and 19 years. Gender was reported to be 51.2% male and 48.8% female. Similar to our study, the largest proportion of teenagers reside in the South (38.8%), followed by the West (23.5%), Midwest (21.1%) and Northeast (16.6%). Census data on race/ethnicity was available for children between the ages of 0 and 17 and was as follows: 60.4% Non-Hispanic/Latino White, 13.4% African American/Black, 5.9% Asian, 18.3% Hispanic/Latino of any race, 0.2% Native Hawaiian/Pacific Islander, 1.0% American Indian/Alaska Native and 2.7% Multiracial (U.S. Census Bureau Population Division, 2018). Although different age groups, compared to the census data, the current sample over-represented youth who identified as Asian and transgender, and under-represented youth who identified as Hispanic and male.
Regarding substance use characteristics, 46.8% of youth had used alcohol in their lifetime, and about 44.4% of lifetime users drank alcohol in the past month. About 29.3% of adolescents endorsed lifetime use of cannabis, and the majority (55.8%) of those lifetime cannabis users reported using cannabis in the past month. As for lifetime use of nicotine, 20.2% of adolescents reported lifetime use of electronic nicotine delivery systems and 15.5% reported lifetime use of combustible cigarettes. Most of lifetime electronic nicotine delivery system users reported use in the past month (52.2%), and 41% of lifetime cigarette users smoked cigarettes in the past month. The current sample endorsed comparable rates of lifetime substance use as those reported in the 2018 Monitoring the Future national survey results on adolescent drug use (Johnston et al., 2019) (i.e., cannabis use [29.7%]; cigarette use [16.1%]; alcohol use [41.2%]; vaping nicotine [25.2%]).
Descriptive Statistics
Descriptive statistics and correlations between scale scores are provided in Table 1. The substance use outcome variables reflect likelihood of past month substance use and frequency of days used. Correlations involving the likelihood variables included the entire sample and were calculated as Spearman’s rho. Correlations involving the frequency of past month substance use variables included only those adolescents who reported using that substance at least one day over the past 30 days.
Table 1.
Descriptive Statistics and Correlations for Anxiety Sensitivity, Substance Use Withdrawal, Anxiety, Coping Motives, and Substance Use Outcomes
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Anxiety Sensitivity | -- | |||||||||||||||
| 2. | Alcohol Withdrawal | .31* | -- | ||||||||||||||
| 3. | Cannabis Withdrawal | .33* | .65* | -- | |||||||||||||
| 4. | Cigarette Withdrawal | .27* | .60* | .57* | -- | ||||||||||||
| 5. | Anxiety | −.66* | −.40* | −.41* | −.39* | -- | |||||||||||
| 6. | Alcohol Cope | .21* | .51* | .39* | .40* | −.34* | -- | ||||||||||
| 7. | Cannabis Cope | .26* | .29* | .47* | .32* | −.34* | .53* | -- | |||||||||
| 8. | Cigarette Cope | .27* | .34* | .26* | .60* | −.35* | .48* | .44* | -- | ||||||||
| 9. | Recent Alcohol Use | .11* | .18* | .13* | .11 | .13* | .34* | .06 | .05 | -- | |||||||
| 10. | Alcohol Use Frequency | .05 | .29* | .25* | .30* | −.11 | .42* | .23* | .16 | -- | -- | ||||||
| 11. | Recent Cannabis Use | .13* | .20* | .34* | .20* | −.10* | .33* | .29* | .06 | .39* | .30* | -- | |||||
| 12. | Cannabis Use Frequency | −.16* | −.08 | .15* | .07 | .04 | .19* | .28* | .04 | .16* | .29* | -- | -- | ||||
| 13. | Recent Cigarette Use | .12* | .16* | .16* | .36* | −.17* | .32* | .27* | .35* | .28* | .25* | .34* | .26* | -- | |||
| 14. | Cigarette Use Frequency | −.01 | −.30* | −.06 | .27* | −.04 | −.02 | .38* | .20 | .03 | .01 | .09 | .34* | -- | -- | ||
| 15. | Recent ENDSa Use | .08* | .19* | .19* | .37* | −.12* | .27* | .14* | .27* | .29* | .24* | .41* | .07 | .31* | .23* | -- | |
| 16. | ENDSa Use Frequency | −.07 | −.11 | .09 | −.14 | −.04 | .28* | .13 | −.24* | .10 | .29* | .17* | .31* | .29* | .17 | -- | -- |
| Mean (% Using Substances) | 36.47 | 4.03 | 8.30 | 13.85 | 40.62 | 10.21 | 12.86 | 10.65 | 19.9% | 3.62 | 15.8% | 7.90 | 6.3% | 11.48 | 10.2% | 8.87 | |
| SD | 7.44 | 6.20 | 9.07 | 15.21 | 9.40 | 6.15 | 5.95 | 5.71 | 5.25 | 8.94 | 11.20 | 10.30 | |||||
Note. Spearman‟s rho was calculated when the likelihood of use variables were part of the correlations calculated.
p < .05.
Electronic nicotine delivery system
No participants were missing item-level CASI scores, 103 participants (.07%) were missing all item-level RCADS anxiety scores, 38 participants (.03%) were missing data on past month alcohol use, 9 participants (.01%) were missing data on past month cannabis use, 24 participants (.02%) were missing data on past month cigarette use, and 22 participants (.01%) were missing past month electronic nicotine delivery systems use data. Analyses conducted with and without missing data did not substantively differ. Therefore, all participants were included in the analyses.
For all scales treated continuously, all item-level skew and kurtosis values were within acceptable ranges. Examination of Mahalanobis distance revealed 48 participants that could be considered outliers. Examining the final SEM models with and without these participants data included revealed no substantive differences in the models. Therefore, all participants were included in the analyses.
Preliminary Confirmatory Factor Analysis Models
All CFA model fit statistics and indices are provided in Table 2. Comparing CFA models of AS revealed that the bifactor model with an Overall AS and four specific lower-order AS orthogonal factors fit the data best (Δ χ2 = 117.15, Δ df = 11, p < .001 compared to the four-factor model). Further, this model provided the best overall fit to the data (χ2 = 593.00, df = 117, CFI = .92, RMSEA = .06, 90% confidence interval [CI; .05, .06]). Reliability for the Overall AS factor was good (ωh = .83). Further, the factor determinacy score (.94) and ECV (.93) and PUC (.74) considered together support the use of the Overall AS factor (see Appendix Table A for standardized factor loadings).
Table 2.
Model Fit Statistics and Indices for Confirmatory Factor Analyses Models
| CFA Models | S-B χ2 | df | Δ χ2 | CFI | RMSEA | 90% CI | |
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| AS | |||||||
| One-Factor | 1306.21*** | 135 | -- | .81 | .08 | .08 | .09 |
| Two-Factor | 1097.24*** | 134 | 144.70*** | .85 | .07 | .07 | .08 |
| Three-Factor | 793.58*** | 132 | 279.70*** | .90 | .06 | .06 | .07 |
| Four-Factor | 733.28*** | 128 | 58.94*** | .90 | .06 | .06 | .06 |
| Bifactor | 593.00*** | 117 | 117.15*** | .92 | .06 | .05 | .06 |
| RCADS-15 | |||||||
| One-Factor | 1120.33*** | 90 | -- | .82 | .10 | .09 | .10 |
| Five-Factor | 314.01*** | 80 | 694.45*** | .96 | .05 | .04 | .06 |
| Bifactor | 212.08*** | 75 | 101.92*** | .98 | .04 | .03 | .05 |
| Withdrawal Factors | |||||||
| Alcohol One-Factor | 149.32*** | 35 | -- | .99 | .07 | .06 | .08 |
| Cannabis One-Factor | 192.03*** | 54 | -- | .98 | .08 | .07 | .09 |
| Nicotine One-Factor | 119.51*** | 20 | -- | .99 | .15 | .12 | .18 |
| Coping Factors | |||||||
| Alcohol One-Factor | 107.69*** | 5 | -- | .96 | .18 | .15 | .21 |
| MI Alcohol One-Factor | 12.30** | 3 | -- | 1.00 | .07 | .03 | .11 |
| Cannabis One-Factor | 77.09*** | 5 | -- | .94 | .19 | .15 | .22 |
| MI Cannabis One-Factor | 4.85 | 2 | -- | 1.00 | .06 | .00 | .13 |
| Nicotine One-Factor | 35.58*** | 5 | -- | .95 | .16 | .12 | .22 |
| MI Nicotine One-Factor | 2.83 | 4 | -- | 1.00 | .00 | .00 | .09 |
Note. S-B = Satorra-Bentler. CFI = comparative fit index. RMSEA = root mean square error of approximation. CI = confidence interval. SRMR = square root mean square residual. LL = lower limit. UL = upper limit. MI = Modification indices model.
p < .01.
p < .001.
Comparing CFA models of Anxiety revealed that the bifactor model with an Overall Anxiety factor and five specific lower-order anxiety factors fit the data best (Δ χ2 = 101.92, Δ df = 5, p < .001 compared to the five-factor model). Further, this model provided the best overall fit (χ2 = 212.08, df = 75, CFI = .98, RMSEA = .04, 90% CI [.03, .05]). Reliability for the Overall Anxiety factor was good (ωh = .84). Further, the factor determinacy score (.93) and ECV (.91) and PUC (.86) considered together support the use of an Overall Anxiety factor (see Appendix Table B for standardized factor loadings).
Examination of the withdrawal items with five response choices revealed many adolescents responding at the floor. All withdrawal factors were thus modeled treating the items as ordinal. Appendix Table C contains standardized factor loadings for all withdrawal factors. The Alcohol Withdrawal factor demonstrated adequate model fit (χ2 = 149.32, df = 35, CFI = .99, RMSEA = .07, 90% CI [ .06, .08]). The Cannabis Withdrawal factor demonstrated adequate fit as well (χ2 = 192.03, df = 54, CFI = .98, RMSEA = .08, 90% CI [.07, .09]). Finally, the Nicotine Withdrawal factor demonstrated marginal-to-adequate fit (χ2 = 119.51, df = 20, CFI = .99, RMSEA = .15, 90% CI [.12, .18]). The RMSEA was improved after allowing a correlated residual between items 7 (severity of insomnia experienced) and 8 (severity of restlessness).
Standardized factor loadings for all coping motives factors are provided in Appendix Table D. The Alcohol Coping Motives factor demonstrated marginal-to-adequate fit (χ2 = 107.69, df = 5, CFI = .99, RMSEA = .18, 90% CI [.15, .21]). However, the model demonstrated adequate fit after allowing empirically supported correlated residuals between items 1 (“to forget my worries”) and 4 (“to forget my problems”) and items 3 (“to cheer me up when I am in a bad mood”) and 5 (“to feel more self-confident”; χ2 = 12.30, df = 3, CFI = 1.00, RMSEA = .07, 90% CI [.03, .11]). The Cannabis Coping Motives factor demonstrated marginal fit to the data (χ2 = 77.09, df = 5, CFI = .94, RMSEA = .19, 90% CI [.15, .22]). Model fit was improved after allowing empirically supported correlated residuals between items 1 (“to forget your worries”) and 3 (“to forget your problems”), items 1 and 2 (“because it helps you when you feel depressed or nervous”), and items 2 and 4 (“to cheer up when you are in a bad mood”). The Cigarette Coping Motives factor also demonstrated marginal fit to the data (χ2 = 77.09, df = 5, CFI = .94, RMSEA = .19, 90% CI [.15, .22]). However, after allowing empirically supported correlated residuals between items 2 (“because it helps me when I feel depressed or nervous”) and 4 (“to forget about my problems”) this model demonstrated excellent fit to the data (χ2 = 2.83, df = 4, CFI = 1.00, RMSEA = .00, 90% CI [.00, .09]).
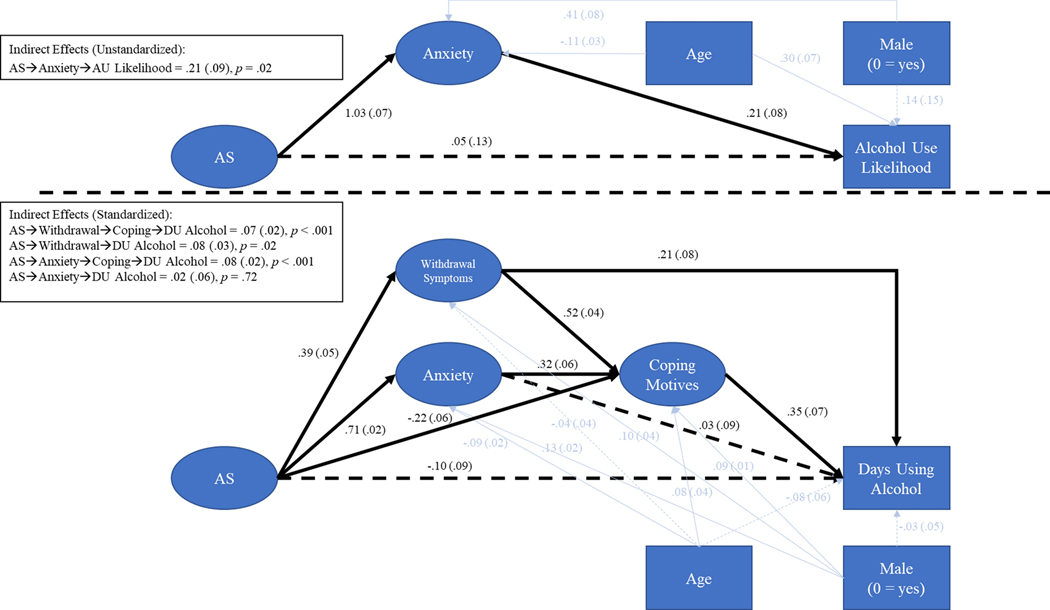
Structural Equation Model: Chained Indirect Relations between AS and Alcohol Use
Using two-part modeling, the relations between AS and alcohol use likelihood as well as days using alcohol, conditional on using alcohol were examined. Age and gender were included as control variables. Because MLR was used to properly conduct two-part modeling, and MLR in the context of categorical data does not allow for calculation of model fit statistics, model fit information for the full indirect effect models was not available. Alcohol use likelihood was treated as a dichotomous variable and unstandardized results are reported. Figure 2a comprises the indirect effect of AS on alcohol use likelihood. In this model, AS was significantly, positively associated with Anxiety (B = 1.03, p < .001). Anxiety was, in turn, associated with alcohol use likelihood (B = .21, p = .01). Together, this resulted in a significant indirect relation between AS and alcohol use likelihood, through the Anxiety factor (B = .21, p = .02; Odds ratio [OR] = 1.23). After controlling for this indirect effect, AS was not significantly associated with alcohol use likelihood (B = .05, p = .66).
Figures 2a-2b.
Indirect relations between AS and alcohol use likelihood and log-transformed days using alcohol. Item-level indicators, error terms, and residual covariances are omitted from the figures for clarity. Solid lines indicate significant paths (p < .05). Dashed lines indicate nonsignificant paths (p > .05). Unstandardized B’s are reported for alcohol use likelihood and standardized βs are reported for log-transformed days using alcohol. AU = Alcohol use. DU = Days using.
Figure 2b comprises the indirect effect of AS on log-transformed days using alcohol over the past 30 days. Days using alcohol was treated as a continuous variable and standardized results are reported. AS was positively associated with Withdrawal Symptoms (β = .39, p < .001) and Anxiety (β = .71, p < .001). Withdrawal Symptoms (β = .52, p < .001) and Anxiety (β = .32, p < .001) were both positively associated with Coping Motives. AS was also directly, negatively associated with Coping Motives (β = −.22, p < .001). Coping Motives (β = .35, p < .001) and Withdrawal Symptoms (β = .21, p < .01) were positively associated with days using alcohol. Neither Anxiety (β = .03, p = .72) nor AS (β = −.10, p = .26) were directly associated with days using alcohol. However, significant chained indirect paths were found from AS to days using alcohol through Withdrawal Symptoms and then through Coping Motives (β = .07, p < .001) and through Anxiety and then through Coping Motives (β = .08, p < .001). There was also a significant simple indirect effect from AS to days using alcohol through Withdrawal Symptoms (β = .08, p = .02). Overall, this model accounted for 23% of the variance in days using alcohol.
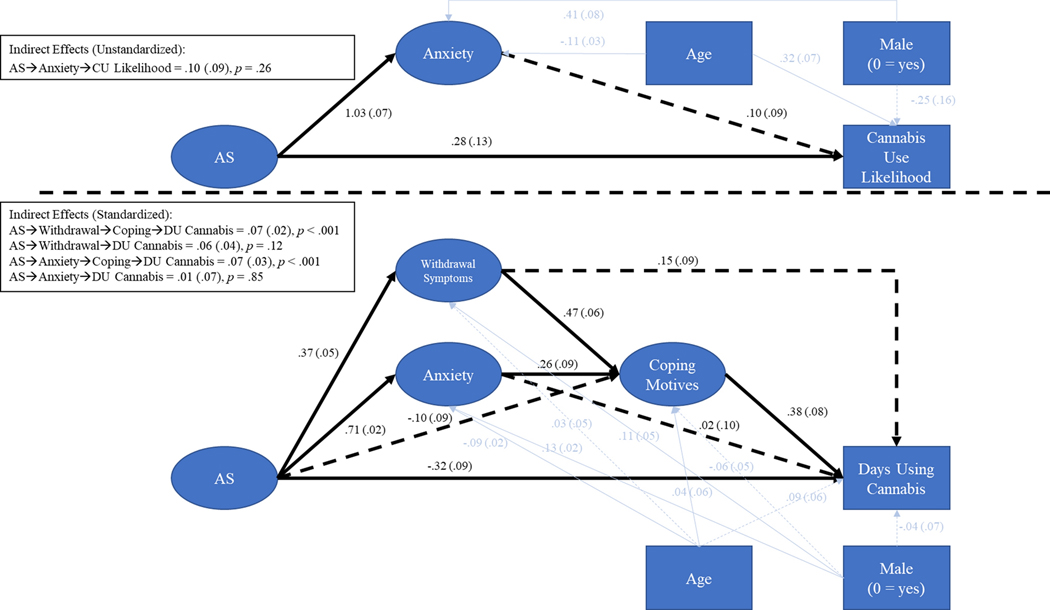
Structural Equation Model: Chained Indirect Relations between AS and Cannabis Use
Using two-part modeling, the relations between AS and cannabis use likelihood as well as days using cannabis over the past 30 days were examined. Cannabis use likelihood was treated as a categorical variable and unstandardized results are reported. Figure 3a comprises the indirect effect of AS on likelihood of having used cannabis. In this model, AS was significantly, positively associated with anxiety (B = 1.05, p < .001). Anxiety was not associated with the likelihood of having used cannabis (B = .04, p = .68). The indirect relation between AS and the likelihood of using cannabis was also not significant (Indirect = .04, p = .68). Finally, the direct relation between AS and the likelihood of using cannabis was significant (B = .34, p < .01).
Figures 3a-3b.
Note. Indirect relations between AS and cannabis use likelihood and log-transformed days using cannabis. Item-level indicators, error terms, and residual covariances are omitted from the figures for clarity. Solid lines indicate significant paths (p < .05). Dashed lines indicate nonsignificant paths (p > .05). Unstandardized B’s are reported for cannabis use likelihood and standardized βs are reported for log-transformed days using cannabis. DU = Days using.
Figure 3b comprises the indirect effect of AS on log-transformed days using cannabis over the past 30 days. Days using cannabis was treated as a continuous variable and standardized results are reported. AS was positively associated with Withdrawal Symptoms (β = .37, p < .001) and Anxiety (β = .72, p < .001). Withdrawal Symptoms (β = .42, p < .001) and Anxiety (β = .23, p < .001) were both positively associated with Coping Motives. Coping Motives (β = .30, p < .001) and Withdrawal Symptoms (β = .18, p < .05) were positively associated with days using cannabis. Anxiety was not significantly associated with days using cannabis (β = .05, p = .61). Significant chained indirect paths were found from AS to days using cannabis through Withdrawal Symptoms and then Coping Motives (β = .07, p < .001) and through Anxiety and the Coping Motives (β = .07, p < .001). In addition to the indirect effects, AS was significantly, negatively associated with days using cannabis (β = −.32, p < .001). Overall, this model accounted for 24% of the variance in days using cannabis.
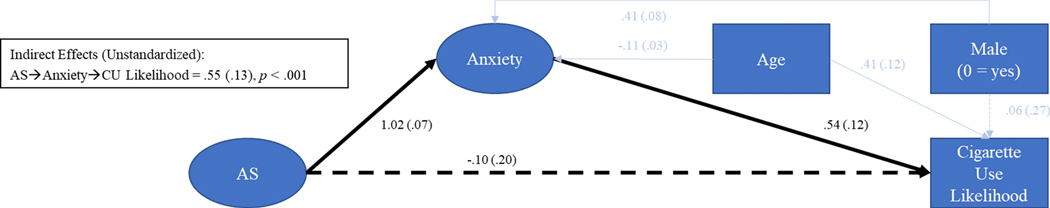
Structural Equation Model: Chained Indirect Relations between AS and the Likelihood of Cigarette Smoking
Only 92 participants reported smoking cigarettes in the past 30 days. Because this sample size would likely be too small to arrive at reliable parameter estimates, only cigarette use likelihood was included as an outcome (see Figure 4). In this model, AS was positively associated with Anxiety (B = 1.02, p < .001) and Anxiety was associated with greater cigarette smoking likelihood (B = .54, p = .01). Finally, the indirect relation between AS and cigarette smoking likelihood was also significant (Indirect = .55, p < .001; OR = 1.73). AS was not significantly directly associated with cigarette smoking likelihood after accounting for the indirect effect (B = − .10, p = .60).
Figure 4.
Indirect relations between AS and cigarette use likelihood. Item-level indicators, error terms, and residual covariances are omitted from the figures for clarity. Solid lines indicate significant paths (p < .05). Dashed lines indicate nonsignificant paths (p > .05). Unstandardized B’s are reported. CU = Cigarette use.
Structural Equation Model: Chained Indirect Relations between AS and the Likelihood of Electronic Nicotine Delivery Systems Use
Only 150 participants reported using electronic nicotine delivery systems in the past 30 days. Because this sample size would likely be too small to arrive at reliable parameter estimates, only electronic nicotine delivery systems use likelihood was included as an outcome (see Figure 5). In this model, AS was positively associated with Anxiety (B = 1.02, p < .001) and Anxiety was associated with a greater electronic nicotine delivery systems use likelihood (B = .28, p = .01). Finally, the indirect relation between AS and electronic nicotine delivery systems use likelihood was also significant (Indirect = .29, p < .001; OR = 1.34). AS was not significantly directly associated with electronic nicotine delivery systems use likelihood after accounting for the indirect effect (B = −.10, p = .60).
Figure 5.
Indirect relations between AS and electronic nicotine delivery systems (ENDS) use likelihood. Item-level indicators, error terms, and residual covariances are omitted from the figures for clarity. Solid lines indicate significant paths (p < .05). Dashed lines indicate nonsignificant paths (p > .05). Unstandardized B’s are reported. eCU = ENDS use.
Discussion
Based on prior frameworks on the role of AS in the development and maintenance of problematic substance use (Otto et al., 2016; Stewart & Kushner, 2001), the current study examined different pathways through which elevated AS could relate to substance use among a large sample of youth. Regarding its association with the likelihood of using substances over the past month, similar patterns were found across most substances. As predicted, AS was associated with greater likelihood of using alcohol, cigarettes, and electronic nicotine delivery systems over the past month through anxiety symptoms. In the cannabis model, the association between AS and increased likelihood of past month cannabis use was direct, and the indirect relation via anxiety symptoms was not significant. We further examined the relations between AS and days using alcohol and cannabis in the past month via several direct and indirect pathways. As expected, AS was indirectly related to higher frequencies of both alcohol and cannabis use through anxiety symptoms and coping-related motives, as well as through withdrawal symptoms and coping-related motives. After accounting for those indirect effects, AS was negatively related to cannabis use frequency (the direct pathway).
In the current study, adolescents with high AS levels had a higher likelihood of past month use of combustible cigarettes, electronic nicotine delivery systems, and drinking alcohol through their elevated anxiety symptoms. These results add to the study conducted by Guillot et al. (2019) that found AS was related to alcohol use problems and tobacco dependence through anxiety and depression symptoms among a large sample of youth from the Los Angeles, CA area. Our results extend these findings in a national sample of youth to suggest that AS may also relate to likelihood of recent alcohol and nicotine use through anxiety symptoms. Together, this suggests that adolescents with elevated AS may be more likely to experience amplified internalizing symptoms, leading them to engage in higher frequencies of alcohol and nicotine use and have more problems related to use.
As reported, among those using alcohol and cannabis in the past month, adolescents with elevated levels of AS reported higher frequency of use through their anxiety and then coping-related motives. These findings indicate that for those with high AS, the pathway to alcohol and cannabis use may be partially explained by the indirect path from AS to substance use frequency through the indirect anxiety-coping motives pathway. This model is consistent with adult work that found AS was associated with increased problems related to alcohol use through general anxiety symptoms and then through drinking to cope with negative affect (Allan et al., 2014).Additionally, the present model extends previous work with adolescents (Guillot et al., 2019) that detected associations between AS and problems related to alcohol and other drug use through anxiety and depression symptoms. The current findings provide support for a more comprehensive picture of the role AS may play in past month alcohol and cannabis use among adolescents, and highlight the potentially important function of motives to use cannabis and alcohol to cope with anxiety symptoms. An interesting next step would be to examine if adolescents have a preferred substance, or substance type (e.g., sedative/anxiolytic), to use to regulate or lessen distressing emotions and sensations (e.g., anxiety), or if substance use in general will satisfy this desire.
A similar pattern was detected with withdrawal symptoms among adolescents who had used alcohol and cannabis in the past month. High-AS adolescents reported higher alcohol and cannabis use frequency in the past month due to the influence of withdrawal symptoms and then coping-related motives. While past empirical work has not yet explored this full model, these results do align with the few studies that have detected positive direct effects between AS and severity of cannabis withdrawal symptoms among adults (Bonn-Miller et al., 2007; Paulus et al., 2017). The current results expand these findings to suggest that adolescents with elevated AS may be more likely to experience intensified withdrawal symptoms, which may lead to higher rates of alcohol and cannabis use to escape those distressful symptoms. The collective chained indirect effect findings have promising implications for youth interventions that target AS (Edalati & Conrod, 2018). They suggest that attenuation of AS in adolescence may reduce the risk to use substances to regulate the intolerable symptoms of withdrawal and anxiety.
The direct effects of the two cannabis models tested are interesting, in that AS was positively and directly associated with an increased likelihood of using cannabis in the past month within the simple indirect effect model; yet, AS was negatively, directly associated with days using cannabis in the chained indirect effect model. This may help explain the inconsistent results reported in the extant literature. These findings are consistent with theoretical models suggesting that individuals gravitate toward anxiolytic substances, such as alcohol, to address anxiety. This is also potentially why we see more clear pathways in the alcohol literature. Yet, this issue gets to be more complex when also considering the popular opinion of cannabis as anxiety-reducing, with dispensaries marketing particular product use to lesson anxiety (Piper et al., 2017). Future prospective work is needed to help discern the motivations of adolescents to use cannabis, and other substances, in real-time when experiencing anxiety, and also the effect particular substances have on anxiety after use.
When interpreting these findings, there are several limitations to consider. The data utilized are cross-sectional; thus, causality or temporality between the variables and paths depicted in the models cannot be directly tested. The current findings can, however, be used to generate hypotheses for future AS-substance use data collected among youth. Longitudinal assessments could help decipher if elevated AS levels during early adolescence predicts substance use and problems later in adolescence, as well as the relative role of use experience on other model variables (e.g., potential bi-directional links between use and anxiety). Indeed, this study focused on between-person differences at a single timepoint. Whereas the assumption is that the risk factor variables of interest are primarily ‘trait-level’ variables, this is an assumption that is increasingly recognized as in need of verifying (Buckner et al., 2013; Dvorak et al., 2014). Further, explication of the dynamic interplay among these processes at a more granular level may help clarify whether state- and trait-level dynamics are similar (Sliwinski, 2008). Finally, only self-report measures were used. It would be valuable to consider whether these results are replicable using additional measurement approaches.
The current study has several notable strengths. Through social-media based advertising, we were able to recruit a large and representative national sample of adolescents to report on their emotions and use of substances. Due to this large sample size, we were able to comprehensively test theoretical models aimed at clarifying the role of AS in the development and maintenance of multiple types of problematic substance use. Overall, these results support past theories that suggest pathways of AS to substance use include those through anxiety, withdrawal, and coping-related motives (Otto et al., 2016; Stewart & Kushner, 2001). In other words, adolescents with high AS may be more prone to experience withdrawal and anxiety symptoms, perceive the symptoms as intolerable, and in turn use substances to attenuate those symptoms. These hypotheses can now be tested longitudinally among youth. The current study also identified both consistency and divergence across substances within a single sample; whereas the majority of the substance use literature focuses on a target substance, a significant minority of youth actively engage in use of multiple substances (Moss et al., 2014). If prospective data support the current findings, the implications are exciting, in that interventions designed to attenuate AS in at-risk adolescent could have the potential to later reduce problematic substance use (Edalati & Conrod, 2018; Knapp et al., 2020).
Acknowledgments
Research supported by National Institute of Mental Health [T32MH115882], National Institute on Drug Abuse [T32DA037202; P30DA029926; R01DA015186; 1F31DA041105], and the National Institute on Alcohol Abuse and Alcoholism [R15AA026079].
Appendix Table A.
Standardized Factor Loadings of the Final Child Anxiety Sensitivity Index Confirmatory Factor Analysis Model
| Items | General AS | AS Dis | AS Uns | AS COG | AS SOC | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| λ | SE | λ | SE | λ | SE | λ | SE | λ | SE | |
| 3 | .62*** | .02 | .07 | .04 | ||||||
| 6 | .62*** | .03 | .57*** | .15 | ||||||
| 9 | .67*** | .02 | .34*** | .08 | ||||||
| 11 | .59*** | .02 | −.04 | .04 | ||||||
| 13 | .43*** | .03 | −.08 | .05 | ||||||
| 14 | .67*** | .02 | .04 | .05 | ||||||
| 16 | .64*** | .02 | −.08 | .06 | ||||||
| 18 | .69*** | .02 | .02 | .05 | ||||||
| λ | SE | λ | SE | λ | SE | λ | SE | λ | SE | |
| 4 | .51*** | .02 | .45*** | .19 | ||||||
| 7 | .42*** | .03 | −.01 | .10 | ||||||
| 8 | .53*** | .02 | .23* | .11 | ||||||
| 10 | .59*** | .02 | .25** | .09 | ||||||
| λ | SE | λ | SE | λ | SE | λ | SE | λ | SE | |
| 2 | .46*** | .03 | .76*** | .08 | ||||||
| 12 | .47*** | .02 | .33*** | .04 | ||||||
| 15 | .64*** | .02 | .29*** | .04 | ||||||
| λ | SE | λ | SE | λ | SE | λ | SE | λ | SE | |
| 1 | .26*** | .03 | .64*** | .06 | ||||||
| 5 | .15*** | .03 | .29*** | .04 | ||||||
| 17 | .27*** | .03 | .64*** | .06 | ||||||
Note. AS = Anxiety sensitivity. Dis = Disease concerns. Uns = Unsteady concerns. Cog = Cognitive concerns. Soc = Social concerns.
p < .001,
p ≤ .01,
p < .05.
Appendix Table B.
Standardized Factor Loadings of the Final RCADS Confirmatory Factor Analysis ModelIte ms
| Items | Anxiety | Social | Separation | GAD | PD | OCD | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| λ | SE | λ | SE | λ | SE | λ | SE | λ | SE | λ | SE | |
| 1 | .38*** | .03 | .37*** | .03 | ||||||||
| 5 | .53*** | .02 | .59*** | .04 | ||||||||
| 13 | .64*** | .02 | .50*** | .04 | ||||||||
| λ | SE | λ | SE | λ | SE | λ | SE | λ | SE | λ | SE | |
| 2 | .51*** | .03 | .50*** | .13 | ||||||||
| 4 | .62*** | .02 | .10* | .04 | ||||||||
| 6 | .52*** | .03 | .51*** | .14 | ||||||||
| λ | SE | λ | SE | λ | SE | λ | SE | λ | SE | λ | SE | |
| 3 | .58*** | .02 | .18* | .08 | ||||||||
| 11 | .60*** | .02 | .15* | .07 | ||||||||
| 15 | .71*** | .02 | .68* | .27 | ||||||||
| λ | SE | λ | SE | λ | SE | λ | SE | λ | SE | λ | SE | |
| 7 | .61*** | .02 | .42** | .13 | ||||||||
| 9 | .65*** | .02 | .48** | .15 | ||||||||
| 12 | .76*** | .02 | .08* | .04 | ||||||||
| λ | SE | λ | SE | λ | SE | λ | SE | λ | SE | λ | SE | |
| 8 | .50*** | .03 | .49*** | .04 | ||||||||
| 10 | .53*** | .03 | .51*** | .04 | ||||||||
| 14 | .57*** | .02 | .50*** | .04 | ||||||||
Note. Social = Social anxiety. Separation = Separation anxiety. GAD = Generalized anxiety disorder. PD = Panic disorder. OCD = Obsessive-compulsive disorder.
p < .001,
p ≤ .01,
p < .05.
Appendix Table C.
Standardized Factor Loadings of the Final Withdrawal Confirmatory Factor Analysis Models
| Items | Alcohol WD | Cannabis WD | Cigarette WD | |||
|---|---|---|---|---|---|---|
| λ | SE | λ | SE | λ | SE | |
| 1 | .85*** | 0.02 | .73*** | 0.04 | .93*** | 0.01 |
| 2 | .88*** | 0.02 | .80*** | 0.03 | .90*** | 0.02 |
| 3 | .89*** | 0.02 | .72*** | 0.03 | .92*** | 0.02 |
| 4 | .87*** | 0.02 | .86*** | 0.02 | ||
| 5 | .86*** | 0.02 | .85*** | 0.02 | .93*** | 0.02 |
| 6 | .90*** | 0.02 | .80*** | 0.03 | .75*** | 0.04 |
| 7 | .81*** | 0.02 | .69*** | 0.04 | .88*** | 0.03 |
| 8 | .86*** | 0.02 | .88*** | 0.02 | ||
| 9 | .84*** | 0.02 | .81*** | 0.03 | ||
| 10 | .76*** | 0.03 | .78*** | 0.03 | ||
| 11 | .92*** | 0.02 | ||||
| 12 13 |
.80*** | 0.03 | ||||
| 14 | .60*** | 0.04 | ||||
| 15 | .87*** | 0.02 | ||||
Note. WD = Withdrawal.
p < .001.
Appendix Table D.
Standardized Factor Loadings of the Final Coping Confirmatory Factor Analysis Models
| Alcohol Cope | Cannabis Cope | Cigarette Cope | ||||
|---|---|---|---|---|---|---|
| λ | SE | λ | SE | λ | SE | |
| 1 | .86*** | 0.02 | .70*** | 0.04 | .79*** | 0.04 |
| 2 | .86*** | 0.02 | .82*** | 0.04 | .87*** | 0.03 |
| 3 | .83*** | 0.02 | .74*** | 0.04 | .76*** | 0.04 |
| 4 | .89*** | 0.02 | .91*** | 0.04 | .90*** | 0.03 |
| 5 | .59*** | 0.04 | .57*** | 0.04 | .51*** | 0.06 |
Note.
p < .001
Footnotes
Declarations of interest: none.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- Ali A, Carré A, Hassler C, Spilka S, Vanier A, Barry C, & Berthoz S. (2016). Risk factors for substances use and misuse among young people in France: What can we learn from the Substance Use Risk Profile Scale? Drug Alcohol Depend, 163, 84–91. [DOI] [PubMed] [Google Scholar]
- Allan NP, Capron DW, Raines AM, & Schmidt NB (2014). Unique relations among anxiety sensitivity factors and anxiety, depression, and suicidal ideation. J Anxiety Disord, 28(2), 266–275. doi: 10.1016/j.janxdis.2013.12.004 [DOI] [PubMed] [Google Scholar]
- Bilsky SA, Feldner MT, Knapp AA, Rojas SM, & Leen-Feldner EW (2016). The roles of sex, anxious reactivity to bodily arousal, and anxiety sensitivity in coping motives for cigarette smoking among adolescents. Experimental and Clinical Psychopharmacology, 24(3), 147. doi: 10.1037/pha0000071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ, Marshall EC, & Bernstein A. (2007). Incremental validity of anxiety sensitivity in relation to marijuana withdrawal symptoms. Addict Behav, 32(9), 1843–1851. doi: 10.1016/j.addbeh.2006.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer S, Godley MD, & Hulvershorn LA (2017). Treating Mental Health and Substance Use Disorders in Adolescents: What Is on the Menu? Curr Psychiatry Rep, 19(1), 5. [DOI] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, & Strong DR (2002). Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology, 111(1), 180–185. [PubMed] [Google Scholar]
- Browne MW, & Cudeck R. (1993). Alternative ways of assessing model fit. In Bollen KA & Long JS (Eds.), Testing structural equation models. Newbury Park, CA: Sage. [Google Scholar]
- Bruce TJ, Spiegel DA, Gregg SF, & Nuzzarello A. (1995). Predictors of alprazolam discontinuation with and without cognitive behavior therapy in panic disorder. Am J Psychiatry, 152(8), 1156–1160. doi: 10.1176/ajp.152.8.1156 [DOI] [PubMed] [Google Scholar]
- Buckner JD, Leen-Feldner EW, Zvolensky MJ, & Schmidt NB (2009). The interactive effect of anxiety sensitivity and frequency of marijuana use in terms of anxious responding to bodily sensations among youth. Psychiatry Res, 166(2–3), 238–246. doi: 10.1016/j.psychres.2008.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Zvolensky MJ, & Ecker AH (2013). Cannabis use during a voluntary quit attempt: an analysis from ecological momentary assessment. Drug Alcohol Depend, 132(3), 610–616. doi: 10.1016/j.drugalcdep.2013.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budney AJ, Novy PL, & Hughes JR (1999). Marijuana withdrawal among adults seeking treatment for marijuana dependence. Addiction, 94(9), 1311–1322. Retrieved from [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2016). Surveillance Summaries- Alcohol and other drug use. Morbidity and Mortality Weekly Report, 65, SS–6. [Google Scholar]
- Comeau N, Stewart SH, & Loba P. (2000). Adolescents’ motives for smoking and marijuana use: Factor structure and relations to motives for alcohol use. Paper presented at the 3rd Joint Meeting of the British Experimental Psychology Society and the Canadian Society for Brain Behavior, and Cognitive Science, Cambridge, UK. [Google Scholar]
- Cooper ML (1994). Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment, 6(2), 117. [Google Scholar]
- DeMartini KS, & Carey KB (2011). The role of anxiety sensitivity and drinking motives in predicting alcohol use: a critical review. Clin Psychol Rev, 31(1), 169–177. [DOI] [PubMed] [Google Scholar]
- Dvorak RD, Pearson MR, & Day AM (2014). Ecological momentary assessment of acute alcohol use disorder symptoms: associations with mood, motives, and use on planned drinking days. Exp Clin Psychopharmacol, 22(4), 285–297. doi: 10.1037/a0037157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebesutani C, Reise SP, Chorpita BF, Ale C, Regan J, Young J, … Weisz JR (2012). The Revised Child Anxiety and Depression Scale-Short Version: scale reduction via exploratory bifactor modeling of the broad anxiety factor. Psychol Assess, 24(4), 833–845. doi: 10.1037/a0027283 [DOI] [PubMed] [Google Scholar]
- Edalati H, & Conrod PJ (2018). A review of personality-targeted interventions for prevention of substance misuse and related harm in community samples of adolescents. Front Psychiatry, 9, 770. doi: 10.3389/fpsyt.2018.00770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elholm B, Larsen K, Hornnes N, Zierau F, & Becker U. (2010). A psychometric validation of the Short Alcohol Withdrawal Scale (SAWS). Alcohol Alcohol, 45(4), 361–365. [DOI] [PubMed] [Google Scholar]
- Gorsuch R. (1983). Factor analysis (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Guillot CR, Blackledge SM, Douglas ME, Cloutier RM, Liautaud MM, Pang RD,… Leventhal AM (2019). Indirect Associations of Anxiety Sensitivity with Tobacco, Alcohol, and Other Drug Use Problems Through Emotional Disorder Symptoms in Adolescents. Behav Med, 1–9. doi: 10.1080/08964289.2019.1573797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, & Bentler P. (1998). Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods, 3, 424–453. [Google Scholar]
- Hughes JR, & Hatsukami D. (1986). Signs and symptoms of tobacco withdrawal. Arch Gen Psychiatry, 43(3), 289–294. doi: 10.1001/archpsyc.1986.01800030107013 [DOI] [PubMed] [Google Scholar]
- Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, & Patrick ME (2019). Monitoring the Future national survey results on drug use 1975–2018: Overview, key findings on adolescent drug use. Retrieved from Ann Arbor: [Google Scholar]
- Knapp AA, Felnder M, Allan NP, Schmidt NB, Keough ME, & Leen-Feldner EW (2020). Test of an anxiety sensitivity amelioration program for at-risk youth (ASAP-Y). Behavior Research and Therapy, 126, 103544. doi: 10.1016/j.brat.2019.103544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knapp AA, Lee DC, Borodovsky JT, Auty SG, Gabrielli J, & Budney AJ (2018). Emerging Trends in Cannabis Administration Among Adolescent Cannabis Users. J Adolesc Health. doi: 10.1016/j.jadohealth.2018.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner MG, Thuras P, Abrams K, Brekke M, & Stritar L. (2001). Anxiety mediates the association between anxiety sensitivity and coping-related drinking motives in alcoholism treatment patients. Addict Behav, 26(6), 869–885. [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Strong DR, Sussman S, Kirkpatrick MG, Unger JB, Barrington-Trimis JL, & Audrain-McGovern J. (2016). Psychiatric comorbidity in adolescent electronic and conventional cigarette use. Journal of psychiatric research, 73, 71–78. doi: 10.1016/j.jpsychires.2015.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal AM, & Zvolensky MJ (2015). Anxiety, depression, and cigarette smoking: a transdiagnostic vulnerability framework to understanding emotion-smoking comorbidity. Psychol Bull, 141(1), 176–212. doi: 10.1037/bul0000003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malmberg M, Kleinjan M, Overbeek G, Vermulst AA, Lammers J, & Engels RC (2013). Are there reciprocal relationships between substance use risk personality profiles and alcohol or tobacco use in early adolescence? Addict Behav, 38(12), 2851–2859. [DOI] [PubMed] [Google Scholar]
- Malmberg M, Overbeek G, Monshouwer K, Lammers J, Vollebergh WA, & Engels RC (2010). Substance use risk profiles and associations with early substance use in adolescence. J Behav Med, 33(6), 474–485. doi: 10.1007/s10865-010-9278-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moshagen M. (2012). The model size effect in SEM: Inflated goodness-of-fit statistics are due to the size of the covariance matrix. Structural Equation Modeling: A Multidisciplinary Journal, 19, 86–98. [Google Scholar]
- Moss HB, Chen CM, & Yi HY (2014). Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug Alcohol Depend, 136, 51–62. doi: 10.1016/j.drugalcdep.2013.12.011 [DOI] [PubMed] [Google Scholar]
- Noël VA, & Francis SE (2011). A meta-analytic review of the role of child anxiety sensitivity in child anxiety. J Abnorm Child Psychol, 39(5), 721–733. [DOI] [PubMed] [Google Scholar]
- Otto MW, Eastman A, Lo S, Hearon BA, Bickel WK, Zvolensky M, … Doan SN (2016). Anxiety sensitivity and working memory capacity: Risk factors and targets for health behavior promotion. Clin Psychol Rev, 49, 67–78. doi: 10.1016/j.cpr.2016.07.003 [DOI] [PubMed] [Google Scholar]
- Paulus DJ, Manning K, Hogan JBD, & Zvolensky MJ (2017). The role of anxiety sensitivity in the relation between anxious arousal and cannabis and alcohol use problems among low-income inner city racial/ethnic minorities. J Anxiety Disord, 48, 87–94. [DOI] [PubMed] [Google Scholar]
- Piper BJ, DeKeuster RM, Beals ML, Cobb CM, Burchman CA, Perkinson L, … Abess AT. (2017). Substitution of medical cannabis for pharmaceutical agents for pain, anxiety, and sleep. J Psychopharmacol, 31(5), 569–575. doi: 10.1177/0269881117699616 [DOI] [PubMed] [Google Scholar]
- Reiss S. (1991). Expectancy model of fear, anxiety, and panic. Clinical Psychology Review, 11(2), 141–153. doi: 10.1016/0272-7358(91)90092-9 [DOI] [Google Scholar]
- Rhemtulla M, Brosseau-Liard P, & Savalei V. (2012). When can categorical variables be treated as continuous? A comparison of robust continuous and categorical SEM estimation methods under suboptimal conditions. Psychol Methods, 17(3), 354–373. [DOI] [PubMed] [Google Scholar]
- Rodriguez A, Reise SP, & Haviland MG (2016). Applying Bifactor Statistical Indices in the Evaluation of Psychological Measures. J Pers Assess, 98(3), 223–237. [DOI] [PubMed] [Google Scholar]
- Rowe CL, Liddle HA, Greenbaum PE, & Henderson CE (2004). Impact of psychiatric comorbidity on treatment of adolescent drug abusers. J Subst Abuse Treat, 26(2), 129–140. doi: 10.1016/S0740-5472(03)00166-1 [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Buckner JD, & Keough ME (2007). Anxiety sensitivity as a prospective predictor of alcohol use disorders. Behav Modif, 31(2), 202–219. [DOI] [PubMed] [Google Scholar]
- Shane PA, Jasiukaitis P, & Green RS (2003). Treatment outcomes among adolescents with substance use problems: The relationship between comorbidities and post-treatment substance involvement. Evaluation and Program Planning, 26(4), 393–402. [Google Scholar]
- Silverman WK, Fleisig W, Rabian B, & Peterson RA (1991). Childhood Anxiety Sensitivity Index. Journal of Clinical Child Psychology, 20, 162–168. [DOI] [PubMed] [Google Scholar]
- Simons J, Correia CJ, Carey KB, & Borsari BE (1998). Validating a five-factor Marijuana Motives Measure: Relations with use, problems, and alcohol motives. Journal of Counseling Psychology, 45(3), 265–273. [Google Scholar]
- Sliwinski M. (2008). Measurement-burst designs for social health research. Social and Personality Psychology Compass, 2(1), 245–261. [Google Scholar]
- Stewart SH, & Kushner MG (2001). Introduction to the Special Issue on “Anxiety Sensitivity and Addictive Behaviors”. Addict Behav, 26(6), 775–785. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/11768544 [DOI] [PubMed] [Google Scholar]
- Toll BA, O’Malley SS, McKee SA, Salovey P, & Krishnan-Sarin S. (2007). Confirmatory factor analysis of the Minnesota Nicotine Withdrawal Scale. Psychol Addict Behav, 21(2), 216–225. doi: 10.1037/0893-164X.21.2.216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau Population Division. (2018). Characteristics of Teenagers 15 to 19 years: 2010–2018. American Community Survey. https://data.census.gov/cedsci/table?q=teenagers&hidePreview=false&tid=ACSST1Y2018.S0902&vintage=2018 [Google Scholar]
- West SG, Finch JF, & Curran PJ (1995). Structural equation models with nonnormal variables: Problems and remedies. In Hoyle RH (Ed.), Structural equation modeling: Concepts, issues, and applications (pp. 56–75). Thousand Oaks, CA: Sage Publications, Inc. [Google Scholar]
- Wolitzky-Taylor K, Guillot CR, Pang RD, Kirkpatrick MG, Zvolensky MJ, Buckner JD, & Leventhal AM (2015). Examination of anxiety sensitivity and distress tolerance as transdiagnostic mechanisms linking multiple anxiety pathologies to alcohol use problems in adolescents. Alcohol Clin Exp Res, 39(3), 532–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Farris SG, Guillot CR, & Leventhal AM (2014). Anxiety sensitivity as an amplifier of subjective and behavioral tobacco abstinence effects. Drug and Alcohol Dependence, 142, 224–230. doi: 10.1016/j.drugalcdep.2014.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Stewart SH, Vujanovic AA, Gavric D, & Steeves D. (2009). Anxiety sensitivity and anxiety and depressive symptoms in the prediction of early smoking lapse and relapse during smoking cessation treatment. Nicotine Tob Res, 11(3), 323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]