Abstract
BACKGROUND AND PURPOSE:
CT is a ubiquitous, efficient, and cost-effective method to evaluate pediatric ventricular size, particularly in patients with CSF shunt diversion who often need emergent imaging. We therefore sought to determine the minimum dose output or CT dose index required to produce clinically acceptable examinations.
MATERIALS AND METHODS:
Using a validated noise insertion method and CT projection data from 22 patients, standard pediatric head CT images were reconstructed with weighted filtered back-projection and sinogram-affirmed iterative reconstruction corresponding to routine, 25%, and 10% dose. Reconstructed images were then evaluated by 3 neuroradiologists (blinded to dose and reconstruction method) for ventricular size, diagnostic confidence, image quality, evidence of hemorrhage, and shunt tip location, and compared with the reference standard.
RESULTS:
There was no significant difference in the ventricular size ranking, and the sensitivity for moderate to severe hydrocephalus was 100%. There was no significant difference between the full-dose level and the ventricular size rankings at the 25% or the 10% dose level for either reconstruction kernel (P > .979). Diagnostic confidence was maintained across doses and kernel. Hemorrhage was more difficult to identify as image quality degraded as dose decreased but was still seen in a majority of cases. Shunts were identified by all readers across all doses and reconstruction methods.
CONCLUSIONS:
CT images having dose reductions of 90% relative to routine head CT examinations provide acceptable image quality to address the specific clinical task of evaluating ventricular size.
Before the advent of ventricular CSF shunt devices for the treatment of hydrocephalus, patients had a poor prognosis with a very high mortality rate. In 1949, Nulsen and Spitz1 were the first to prove the efficacy of placing a shunt with a 1-way valve into the venous system of a patient with hydrocephalus to free outflow of CSF into the venous system. The eventual introduction of the Spitz-Holter valve in 1956 made ventricular shunting the standard treatment for hydrocephalus.2 Since then, significant technical advancements in CSF diversion devices have continued; however, device complications remain fairly common even today. One study estimated that an episode of ventricular shunt failure will occur in 85% of patients within 15 years of device insertion3 with 30%–40% of ventricular shunts failing after the first year of insertion.4 Kim et al5 reported a ventricular shunt mortality rate of 2.2%. The clinical diagnosis of shunt malfunction is further complicated by nonspecific clinical signs, which can be attributed to other common pediatric ailments.5,6
CT evaluation of ventricular size, in conjunction with clinical symptoms, is the primary means of assessing ventricular CSF shunt failure/malfunction in pediatric patients with closed fontanelles.5 However, concerns were expressed regarding the use of CT in children,7 primarily because they are more sensitive than adults for some cancers, one of which is radiation-induced brain tumor.8 In some cases, these concerns have prevented judicious use of CT imaging.9
Rapid sequence MR imaging may also be used for evaluation of ventricular size; however, it is not routinely available at large medical centers during off hours, or at small hospitals that do not have MR imaging units. In addition, MR imaging is more time consuming and costly, sometimes requires sedation of young children, and is associated with rare but existing safety risks associated with strong magnetic fields and radiofrequency electromagnetic emissions.10–12
Shunted pediatric patients will require episodic imaging throughout the life of a shunt to ensure proper functionality, and given the wide availability of CT across our large (and often rural) health care network, CT is the principal imaging technique used. However, repeated use of CT in children has recently come into question, with some providers advocating use of MR imaging, despite its associated limitations, because MR imaging does not use ionizing radiation. To allay concerns regarding radiation, we have initiated educational programs for providers and patients that put the very small potential risk associated with a CT examination into proper perspective. In addition, our practice carefully evaluates our scanning protocols to use the lowest doses of radiation necessary to answer the specific diagnostic question.
Because assessment of ventricular size does not require the same level of image quality as a routine head CT examination, we hypothesized that the radiation dose could be greatly reduced for this diagnostic task without compromising diagnostic accuracy. Therefore, the purpose of this specific work was to determine the minimum radiation dose required to produce clinically acceptable head CT examinations for the evaluation of ventricular shunt malfunction. As part of this evaluation, we also examined whether the use of newer image reconstruction algorithms designed to facilitate dose reduction, commonly referred to as iterative reconstruction, were required for accurate diagnoses.11,13
Materials and Methods
Our Institutional Review Board approved this study with a waiver of informed consent. Minnesota Research Authorization was obtained for each study subject. This study used CT projection data from pediatric head CT using 1 of 2 emergency department CT scanners at our institution. All examinations included in this study were performed as the standard of care; the images were retrospectively processed and evaluated. This study was in complete compliance with the Health Insurance Portability and Accountability Act.
Patient Population
Twenty-two pediatric subjects who underwent noncontrast head CT studies at our institution from August 2012 to March 2013 were included in this study. Inclusion criteria included: patient <18 years of age, acquisition of head CT without contrast using our routine head CT protocol, and ability to retrieve and archive CT projection data. CT projection data were collected consecutively on all pediatric patients. Patients were excluded if CT projection data were deleted off the scanner image reconstruction system before archiving or if the patient was without the Minnesota Research Authorization. Some of our study subjects had a ventriculostomy device to treat hydrocephalus.
Image Acquisition and Reconstruction
Patients were scanned using our regular pediatric head CT protocol on a 128-section CT scanner (Definition Flash; Siemens, Erlangen, Germany). Each examination was acquired with a rotation time of 0.5 seconds, a helical pitch of 0.8, a tube energy of 120 kV, a quality reference mAs of 220, and a detector configuration of 128 × 0.6 mm. The automatic exposure control (CARE Dose 4D; Siemens) was used. Because the automatic exposure control setting on this scanner uses an adult-size reference patient for pediatric patients, the actual effective mAs (mAs/pitch) was much lower than 220 because of the adaptation of the mAs to the pediatric head size. There were 5 trauma patients scanned with a slightly higher quality reference mAs at 275 and 4 patients scanned with an adult technique (250 effective mAs, CARE Dose 4D off) because they were older than 6 years according to our clinical protocols.
Using a validated noise insertion program14 that takes into account both the automatic exposure control and the bow-tie filter of the scanner, noise was inserted into the CT projection data of each patient to result in new CT projection data for each patient that corresponded to 25% and 10% of the original routine dose (ie, 75% and 90% dose reduction). Images from these lower-dose CT projection data were reconstructed using a 5-mm section thickness and 5-mm interval with 2 reconstruction kernels used at each dose level, a routine head kernel with weighted filtered back projection (H30), and a head kernel using sinogram-affirmed iterative reconstruction (Siemens) called J30 with a strength setting of 2 (Fig 1).
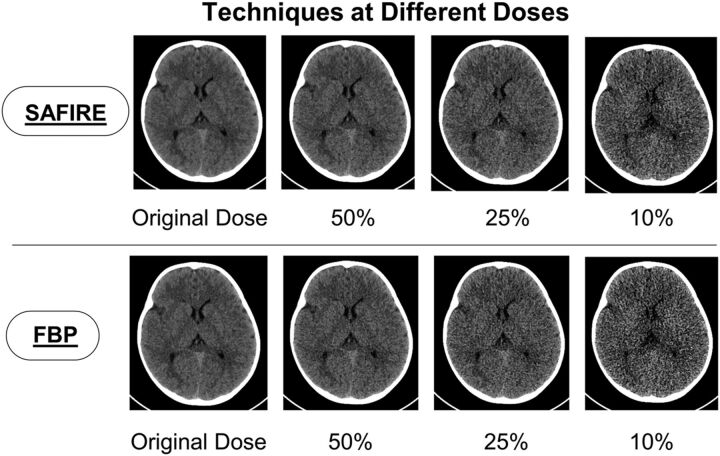
Fig 1.
An actual subject from our study showing the full dose, 50% dose, 25% dose, and 10% dose using sinogram-affirmed iterative reconstruction and filtered back-projection reconstructions.
Image Interpretation
Three board- and Certificate of Added Qualification–certified neuroradiologists with 8, 22, and 23 years of experience (L.J.E., P.H.L., K.N.K.) were asked to evaluate each CT dataset for ventricular size, diagnostic confidence, image quality, evidence of hemorrhage, and shunt tip location using a standard form. Readers were blinded to clinical history, dose level, and reconstruction kernel. A blocked reader design was used so that the neuroradiologist readers were presented with each patient's examination (using a unique dose level/reconstruction method combination) once in every 22 examinations. CT image datasets were presented to the reader in random order, with images evaluated on a computer workstation (Advantage Windows Version 4.3–05; GE Healthcare, Milwaukee, Wisconsin). Ventricular size was graded as normal, mild hydrocephalus, moderate hydrocephalus, or severe hydrocephalus based on a previously published visual scale shown in Fig 2 that was reproduced on the data form, with the two largest ventricle sizes classified as severe. Diagnostic confidence was rated along a 5-point scale similar to comparable previous studies15–17: 1 = nondiagnostic, cannot identify or rule out ventricular enlargement and shunt tube tip location; 2 = will potentially miss mild ventricular enlargement and shunt tube tip location; 3 = will probably not miss ventricular enlargement and shunt tube tip location; 4 = most likely will identify all abnormalities with respect to ventricular enlargement and shunt tube tip; 5 = can detect ventricular enlargement and shunt tube tip without diagnostic compromise. Image quality was also graded along a similar 5-point scale: 1 = nondiagnostic because of excessive noise/artifacts; 2 = diagnosis questionable because of excessive noise/artifacts; 3 = diagnostic with moderate but acceptable noise/artifacts; 4 = mild noise, no change in diagnostic confidence; 5 = routine diagnostic image quality.
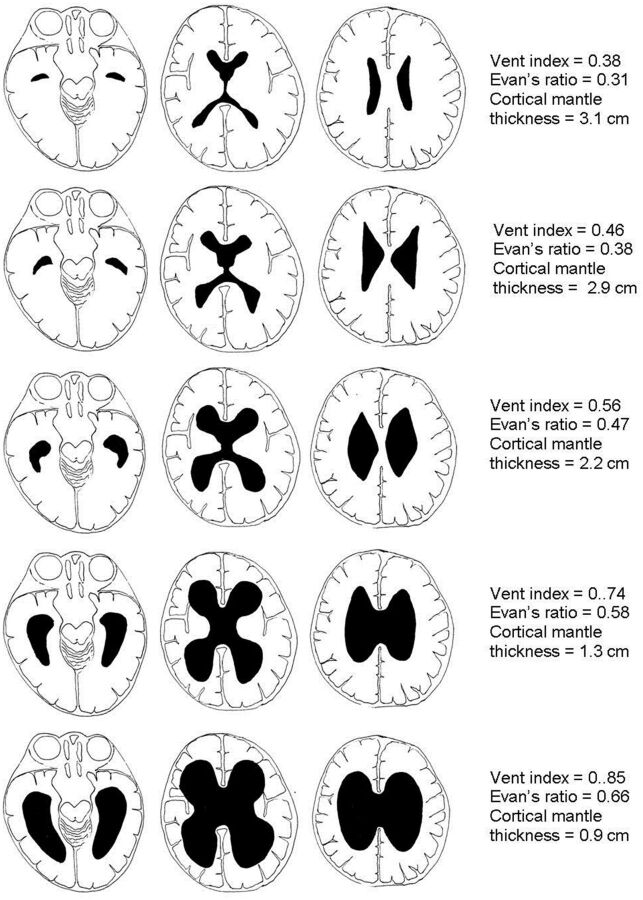
Fig 2.
Ventricular size was classified using a previously published visual scale. Reprinted with permission from Dias MS, Shaffer ML, Iantosca MR, et al. Variability among pediatric neurosurgeons in the threshold for ventricular shunting in asymptomatic children with hydrocephalus. J Neurosurg Pediatr 2011;7:134–42.
Radiologists were also asked to identify intracranial hemorrhage of any type (ie, present, not present, cannot ascertain). If hemorrhage was present, they were asked to identify the location. They were also asked to record the shunt tube tip if present. In addition, readers were given an opportunity to notate additional observations or comments.
Reference Standard
A reference standard for ventricular size for each patient was determined using reader agreement rules. These rules defined the reference standard ventricular size to be the ventricular size determined by at least 2 of the 3 readers when examining the routine-dose head CT using the standard commercial iterative reconstruction kernel (J30). For these 22 routine-dose datasets, all 3 readers rated ventricular size identically in 15 (68%). In the remaining 7 cases, 2 of 3 readers always agreed with the outlying reader ventricular size rank differing by only 1 severity rank.
Statistical Analysis
The accuracy of each reader's ventricular size rankings were compared with the reference standard for each dose level and reconstruction method. The sensitivity and accuracy for moderate and severe hydrocephalus were also determined using ventricular size of 3 or 4 versus ventricular size 1 or 2. Descriptive statistics (ie, mean, standard deviation) were used to report diagnostic confidence and image quality for each dose level and reconstruction method. Wilcoxon rank sum test was performed to determine whether diagnostic confidence and image quality for the reduced dose differed from those in the routine-dose head CT examinations. Reader agreement was calculated for all doses and kernels using a multirater κ statistic.
Results
Twenty-two patients underwent pediatric head CT with subsequent reconstruction of reduced-dose compared with standard head CT images corresponding to 25% and 10% of the original dose. Patient ages ranged from 1 month to 16 years (median 3 years). Indications for examination included evaluation for hydrocephalus (n = 8), trauma (n = 9), and general assessment (n = 5). Of the 22 total patients evaluated in this study, 12 of the children were seen in our emergency department, 2 were being seen in the outpatient clinic and later scanned in the emergency department, and 8 patients were inpatients at the time of the scan.
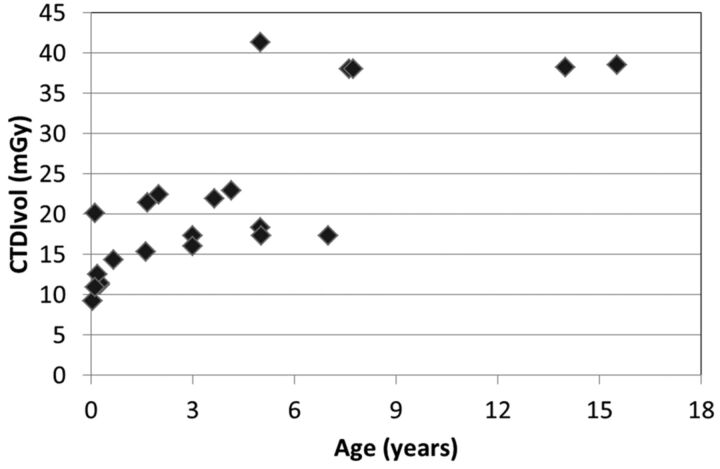
The mean volume CT dose index in the original 22 full-dose examinations was 21.6 milligray (mGy) ± 10.3 mGy (minimum: 9.2 mGy; maximum: 41.3 mGy), as shown in Fig 3. The mean dose-length product was 370 ± 216 mGy × cm (minimum: 98 mGy × cm; maximum: 778 mGy × cm). Using an age-corrected conversion factor from dose-length product to effective dose,18 the estimated mean effective dose was 1.8 ± 0.5 millisievert (mSv) (minimum: 1.0 mSv; maximum: 2.9 mSv). The estimated mean effective dose corresponding to the 10% dose level would be 0.18 ± 0.05 mSv.
Fig 3.
Distribution of volume CT dose index for the 22 patients in their original full-dose examinations (mean, 21.6 ± 10.3 mGy; range, [9.2 mGy, 41.3 mGy]). The volume CT dose index was based on a 16-cm CT dose index phantom.
According to reference standard assessment of ventricular size, there were 12 patients with normal ventricular size, 7 patients with mild hydrocephalus, 2 patients with moderate hydrocephalus, and 1 patient with severe hydrocephalus. There was substantial agreement between the 3 readers when determining ventricular size with a multirater κ of 0.73, which indicates substantial agreement.
The accuracy for an exact match of reference standard ventricular size and each reader's ventricular size rankings for each dose level and reconstruction method are given in Table 1. The accuracy for the full-dose examinations ranged from 86% to 95% across readers, from 73% to 95% at the 25% dose level, and from 77% to 91% at the 10% dose level. The 95% confidence intervals for accuracy of ventricular assessment were virtually identical for each reader (Table 1). Except for 1 case for each reader at the 10% dose level with each reconstruction method, all disagreements at the lower dose levels for either reconstruction method were within 1 rank of ventricular size compared with the reference standard.
Table 1:
Accuracy of ventricular size rank for exact match between reader and reference standard
| 100% Dose |
25% Dose |
10% Dose |
|||
|---|---|---|---|---|---|
| J30 | J30 | H30 | J30 | H30 | |
| Reader 1 | 19/22 | 19/22 | 19/22 | 19/22 | 19/22 |
| 86b (65–97) | 86b (65–97) | 86b (65–97) | 86a (65–97) | 86a (65–97) | |
| Reader 2 | 19/22 | 16/22 | 19/22 | 17/22 | 17/22 |
| 86b (65–97) | 73b (50–89) | 86b (65–97) | 77a (55–92) | 77a (55–92) | |
| Reader 3 | 21/22 | 21/22 | 21/22 | 20/22 | 20/22 |
| 95b (77–100) | 95b (77–100) | 95b (77–100) | 91a (71–99) | 91a (71–99) | |
Indicates that all incorrect ventricular size rankings were discrepant by 1 rank.
Indicates that all cases except for 1 at the lower dose levels were categorized within 1 rank ventricular size, when compared with the reference standard.
The sensitivity for the identification of moderate to severe hydrocephalus was 100% for all 3 readers across all radiation dose levels and reconstruction methods (3 of 3; 95% confidence interval 29%–100%). The accuracy for the identification of moderate or severe hydrocephalus is shown in Table 2 and ranged from 95% to 100% for reader 1, from 91% to 95% for reader 2, and 100% for reader 3.
Table 2:
Accuracy for identification of moderate and severe hydrocephalus (ie, rank 3 or 4 versus rank 1 or 2) per reader compared with reference standard
| 100% Dose |
25% Dose |
10% Dose |
|||
|---|---|---|---|---|---|
| J30 | J30 | H30 | J30 | H30 | |
| Reader 1 | 22/22 | 22/22 | 21/22 | 22/22 | 21/22 |
| 100 (85–100) | 100 (85–100) | 95 (77–100) | 100 (85–100) | 95 (77–100) | |
| Reader 2 | 20/22 | 20/22 | 21/22 | 21/22 | 20/22 |
| 91 (71–99) | 91 (71–99) | 95 (77–100) | 95 (77–100) | 91 (71–99) | |
| Reader 3 | 22/22 | 22/22 | 22/22 | 22/22 | 22/22 |
| 100 (85–100) | 100 (85–100) | 100 (85–100) | 100 (85–100) | 100 (85–100) | |
Radiologists reported their diagnostic confidence on a 5-point scale (Table 3). For all 3 readers, the diagnostic confidence was very high (mean rank = 4.88) on the original dose scan and similar for the 25% dose scans, regardless of reconstruction method (P > .3 except for Reader 2's 25% dose + filtered back-projection, where P = .02). For 1 reader, diagnostic confidence was significantly lower at the 10% dose level, and was worse for the reconstruction kernel without iterative reconstruction (mean confidence rank = 1.18 and 1.09, respectively, for the J30 and H30 kernel). At the 10% dose level, diagnostic confidence was significantly degraded for the filtered back-projection (P < .003 for all readers), but this difference was small in magnitude for 2 of 3 readers who had mean confidence scores of 4.6 and 4.7. With iterative reconstruction, 1 reader no longer had significantly lower confidence scores at the 10% dose level (P = .16), but findings were unchanged for the other 2 (P < .005).
Table 3:
Diagnostic confidence per reader for evaluation of ventricular size
| 100% Dose |
25% Dose |
10% Dose |
|||
|---|---|---|---|---|---|
| J30 | J30 | H30 | J30 | H30 | |
| Reader 1 | 5.0 ± 0.0 | 5.0 ± 0.0 | 5.0 ± 0.2 | 4.7 ± 0.5 | 4.6 ± 0.5 |
| Reader 2 | 5.0 ± 0.2 | 4.8 ± 0.5 | 4.6 ± 0.6 | 3.9 ± 0.9 | 3.3 ± 1.2 |
| Reader 3 | 5.0 ± 0.0 | 5.0 ± 0.0 | 5.0 ± 0.0 | 4.9 ± 0.5 | 4.7 ± 0.6 |
Note:—5-point scale: 1 indicates nondiagnostic, cannot identify or rule out ventricular enlargement and shunt tube tip location; 2, will potentially miss mild ventricular enlargement and shunt tube tip location; 3, will probably not miss ventricular enlargement and shunt tube tip location; 4, most likely will identify all abnormalities with respect to ventricular enlargement and shunt tube tip; 5, can detect ventricular enlargement and shunt tube tip without diagnostic compromise.
Table 4 reports the overall perceived image quality by each reader across dose levels and reconstruction methods. As expected, each reader perceived significantly degraded image quality and more noise artifacts at the lower dose levels, regardless of reconstruction method (P < .002 for all comparisons). At the 25% dose level, 2 of 3 readers rated image quality as significantly better with iterative reconstruction compared with filtered back-projection (P = .02, P = .001). At the 10% dose level, only 1 reader rated iterative reconstruction significantly better (P = .013).
Table 4:
Overall image quality per reader using the 5-point scale described above
| 100% Dose |
25% Dose |
10% Dose |
|||
|---|---|---|---|---|---|
| J30 | J30 | H30 | J30 | H30 | |
| Reader 1 | 4.9 ± 0.4 | 4.1 ± 0.4 | 3.8 ± 0.5 | 3.5 ± 0.5 | 3.2 ± 0.4 |
| Reader 2 | 3.8 ± 1.1 | 2.3 ± 0.7 | 1.6 ± 0.6 | 1.2 ± 0.5 | 1.1 ± 0.3 |
| Reader 3 | 4.1 ± 0.7 | 3.5 ± 0.6 | 3.4 ± 0.6 | 2.2 ± 0.5 | 1.8 ± 0.4 |
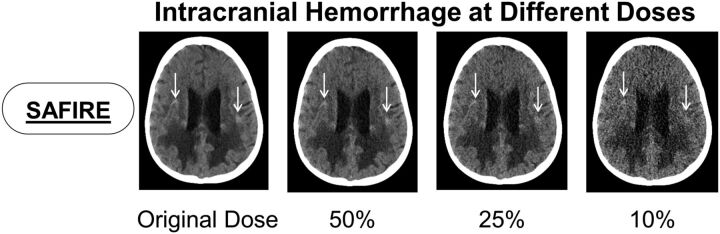
Although the study and examination was not designed to identify intracranial hemorrhage, there were 3 cases by reference standard, with 2 of 3 readers identifying it at all doses (Fig 4). There were 7 cases with intracranial shunts with shunt tip locations correctly identified by all 3 readers.
Fig 4.
Although the study was not designed to identify intracranial hemorrhage, it could be occasionally identified. Images from an actual subject in our study showing intracranial hemorrhage (arrow) at the full, 25%, and 10% dose using sinogram-affirmed iterative reconstruction. As subtle hemorrhage may not be identified at lower doses, the technique should not be used in cases where identification of hemorrhage is suspected or critical.
Discussion
Pediatric patients with CSF shunts are often repeatedly scanned to evaluate for shunt malfunction. Most of these repeat scans are evaluating ventricular morphology, most specifically ventricular size stability, shunt location, and in some cases CSF shunt complications. In our study, we simulated doses that were 25% and 10% of the original dose. We showed that simulated reduction to 10% of the standard dose was diagnostically acceptable. In this blinded study, neuroradiologists were able to accurately detect moderate to severe hydrocephalus across all dose levels and reconstruction kernels without compromising diagnostic performance. As expected, the overall image quality decreased at lower doses; however, this did not compromise the diagnostic accuracy for this specific indication. The resultant volume CT dose index was reduced from 21.6 to 2.2 mGy. The corresponding estimated effective dose was reduced from 1.8 to roughly 0.18 mSv, which is negligible relative to the annual background radiation in the United States from naturally occurring sources (mean, 3.0 mSv; range, 1–10 mSv).
Using validated, reduced dose compared with standard simulation techniques,14 our study demonstrated that a 90% reduction in dose relative to a routine head CT examination was clinically acceptable for the evaluation of ventricular size. In addition, iterative reconstruction is not required to keep observer performance high at the lower doses, so our results can be easily translated across a broad range of CT scanner models of various makes and models.
All 7 cases of intracranial shunts were accurately identified by all readers. This 100% accuracy in identifying shunt position is far more favorable than the literature available for rapid-sequence MR imaging where it is reportedly lower. In 2 studies, from 42%11 to 60%13 of reviews for catheter positions were graded as nondiagnostic or poor in at least 1 sequence. O'Neill et al11 found that insufficient shunt-catheter visualization was especially associated with small ventricles when using half-Fourier acquisition single-shot turbo rapid-sequence MR imaging.
Based on this evaluation study, we have already implemented a reduced-dose technique in our practice for pediatric patients with shunts since March 2013. A quality reference mAs of 25 was used instead of the original 220 quality reference mAs. Image quality continues to be deemed sufficient for the diagnostic task of evaluating potential shunt malfunction.
There were several limitations to our study. This was a pilot retrospective review, and our study was underpowered to perform noninferiority testing. We consequently reported and compared ratios and 95% confidence intervals for accuracy of ventricular size rank. Because of obvious differences in technique (Fig 1), blinded readers were likely able to distinguish the original-dose studies from the reconstructed lower-dose studies at 25% and 10% of the original dose. This could have resulted in bias during subjective image quality evaluation, despite being blinded to technical data. In addition, the design of our questionnaire may have prompted the blinded radiologists to look closer for shunt tube tips and intracranial hemorrhage more than they otherwise would have without prompting.
Conclusions
The accuracy of detection of moderate and severe hydrocephalus was maintained across all dose levels and reconstruction methods. As expected, diagnostic confidence was generally maintained, with image quality decreased at lower dose levels.
CT images at 10%–25% of the dose level of routine head CT examinations provide acceptable image quality to address the specific clinical task of evaluating ventricular size. Extremely low-dose CT examinations for the evaluation of ventricular size and shunt malfunction are a reasonable alternative to emergent MR imaging and avoid the increased cost, workflow inefficiencies, frequent need for sedation, and safety concerns associated with MR imaging. The promising results of this study have already resulted in implementation of this very low-dose head CT protocol at our institution.
Acknowledgments
The authors would like to express their appreciation to Maria M. Shiung and Michael R. Bruesewitz, RT, for their contributions to this work. We would also like to thank Amy L. Nordstrom for assistance in preparation of the manuscript.
ABBREVIATION:
- mGy
milligray
Footnotes
Disclosures: Cynthia McCollough—UNRELATED: Grants/Grants Pending: Siemens Medical Solutions*; Travel/Accommodations/Meeting Expenses Unrelated to Activities Listed: Siemens Healthcare AG, Comments: Travel to present research results for sponsored research unrelated to this work. Joel Fletcher—UNRELATED: Grants/Grants Pending: Siemens Healthcare,* Comments: My institution receives a grant from Siemens Healthcare, which manufactures the iterative reconstruction kernel used in this study. This grant includes personnel time for me as a coinvestigator. Lifeng Yu—UNRELATED: Other: Siemens Healthcare, Comments: The authors and Mayo Clinic have intellectual property rights related to a technology that is not used in the current research. *Money paid to the institution.
References
- 1. Nulsen FE, Spitz EB. Treatment of hydrocephalus by direct shunt from ventricle to jugular vein. Surg Forum 1951:399–403 [PubMed] [Google Scholar]
- 2. Boockvar JA, Loudon W, Sutton LN. Development of the Spitz-Holter valve in Philadelphia. J Neurosurg 2001;95:145–47 [DOI] [PubMed] [Google Scholar]
- 3. Stone JJ, Walker CT, Jacobson M, et al. Revision rate of pediatric ventriculoperitoneal shunts after 15 years. J Neurosurg 2013;11:15–19 [DOI] [PubMed] [Google Scholar]
- 4. George KJ, Roy D. A low radiation computed tomography protocol for monitoring shunted hydrocephalus. Surg Neurol Int 2012;3:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kim TY, Stewart G, Voth M, et al. Signs and symptoms of cerebrospinal fluid shunt malfunction in the pediatric emergency department. Pediatr Emerg Care 2006;22:28–34 [DOI] [PubMed] [Google Scholar]
- 6. Madikians A, Conway EE. Cerebrospinal fluid shunt problems in pediatric patients. Pediatr Ann 1997;26:613–20 [DOI] [PubMed] [Google Scholar]
- 7. Brenner DJ, Elliston CD, Hall EJ, et al. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 2001;176:289–96 [DOI] [PubMed] [Google Scholar]
- 8. United Nations Scientific Committee on the Effects of Atomic Radiation. Sources, effects and risks of ionizing radiation UNSCEAR 2013 Report. New York: United Nations Scientific Committee on the Effects of Atomic Radiation; 2013 [Google Scholar]
- 9. McCollough CH. Defending the use of medical imaging. Health Phys 2011;100:318–21 [DOI] [PubMed] [Google Scholar]
- 10. Kanal E, Barkovich AJ, Bell C, et al. ACR guidance document on MR safe practices: 2013. J Magn Reson Imaging 2013;37:501–30 [DOI] [PubMed] [Google Scholar]
- 11. O'Neill BR, Pruthi S, Bains H, et al. Rapid sequence magnetic resonance imaging in the assessment of children with hydrocephalus. World Neurosurg 2013;80:e307–12 [DOI] [PubMed] [Google Scholar]
- 12. Chaljub G, Kramer LA, Johnson RF, et al. Projectile cylinder accidents resulting from the presence of ferromagnetic nitrous oxide or oxygen tanks in the MR suite. AJR Am J Roentgenol 2001;177:27–30 [DOI] [PubMed] [Google Scholar]
- 13. Ashley WW, McKinstry RC, Leonard JR, et al. Use of rapid-sequence magnetic resonance imaging for evaluation of hydrocephalus in children. J Neurosurg 2005;103:124–30 [DOI] [PubMed] [Google Scholar]
- 14. Yu LF, Shiung M, Jondal D, et al. Development and validation of a practical lower-dose-simulation tool for optimizing computed tomography scan protocols. J Comput Assist Tomogr 2012;36:477–87 [DOI] [PubMed] [Google Scholar]
- 15. Prakash P, Kalra MK, Kambadakone AK, et al. Reducing abdominal CT radiation dose with adaptive statistical iterative reconstruction technique. Invest Radiol 2010;45:202–10 [DOI] [PubMed] [Google Scholar]
- 16. Fletcher JG, Grant KL, Fidler JL, et al. Validation of dual-source single-tube reconstruction as a method to obtain half-dose images to evaluate radiation dose and noise reduction: phantom and human assessment using CT colonography and sinogram-affirmed iterative reconstruction (SAFIRE). J Comput Assist Tomogr 2012;36:560–69 [DOI] [PubMed] [Google Scholar]
- 17. Froemming AT, Kawashima A, Takahashi N, et al. Individualized kV selection and tube current reduction in excretory phase computed tomography urography: potential for radiation dose reduction and the contribution of iterative reconstruction to image quality. J Comput Assist Tomogr 2013;37:551–59 [DOI] [PubMed] [Google Scholar]
- 18. American Association of Physicists in Medicine. The measurement, reporting and management of radiation dose in CT: report of AAPM Task Group 23 of the Diagnostic Imaging Council CT Committee. AAPM report no. 96; 2008. https://www.aapm.org/pubs/reports/RPT_96.pdf. Accessed May 28, 2014.