Abstract
BACKGROUND AND PURPOSE:
Low-tube-voltage acquisition has been shown to facilitate substantial dose savings for neck CT with similar image contrast compared with standard 120-kVp acquisition. However, its potential for the detection of neck pathologies is uncertain. Our aim was to evaluate the effects of low-tube-voltage 80-kV(peak) acquisitions for neck CT on diagnostic accuracy and interobserver agreement.
MATERIALS AND METHODS:
Three radiologists individually analyzed 80-kVp and linearly blended 120-kVp image series of 170 patients with a variety of pathologies who underwent dual-energy neck CT. Reviewers were unblinded to the clinical indication for CT but were otherwise blinded to any other data or images and were asked to state a final main diagnosis. Findings were compared with medical record charts, CT reports, and pathology results. Sensitivity, specificity, positive predictive value, and negative predictive value were calculated for each observer. Interobserver agreement was evaluated by using intraclass correlation coefficients.
RESULTS:
Diagnoses were grouped as squamous cell carcinoma–related (n = 107, presence/absence of primary/recurrent squamous cell carcinoma), lymphoma-related (n = 40, presence/absence of primary/recurrent lymphoma), and benign (n = 23, eg, abscess). Cumulative sensitivity, specificity, positive predictive value, and negative predictive value for 80-kVp and blended 120-kVp images were 94.8%, 93.0%, 95.9%, and 91.1%, respectively. Results were also consistently high for squamous cell carcinoma–related (94.8%/95.3%, 89.1%/89.1%, 94.3%/94.4%, 90.1%/91.0%) and lymphoma-related (95.0%, 100.0%, 100.0%, 95.2%) 80-kVp/120-kVp image series. Global interobserver agreement was almost perfect (intraclass correlation coefficient, 0.82, 0.80; 95% CI, 0.76–0.74, 0.86–0.85). Calculated dose-length product was reduced by 48% with 80-kVp acquisitions compared with the standard 120-kVp scans (135.5 versus 282.2 mGy × cm).
CONCLUSIONS:
Low-tube-voltage 80-kVp CT of the neck provides sufficient image quality with high diagnostic accuracy in routine clinical practice and has the potential to substantially decrease radiation exposure.
CT is a standard imaging technique in routine clinical practice for detection, staging, and follow-up evaluation of various pathologies of the neck, including squamous cell carcinoma (SCC), cervical lymphoma or lymphadenopathy, and parapharyngeal or retropharyngeal abscess.1–5 CT examinations contribute a substantial amount of cumulative radiation exposure to patients with cervical pathologies, especially if follow-up CT is required.6 Thus, various approaches for dose reduction of CT of the neck, brain, paranasal sinus, and the facial skeleton have been proposed, including reduction of tube current and tube potential, high-pitch acquisition, and application of automated exposure-control software.7–10 The combination of such techniques with an iterative reconstruction algorithm can also provide similar image quality while substantially reducing exposure to ionizing radiation compared with the standard 120-kVp acquisitions.11,12
Several studies have demonstrated that low-tube-voltage acquisitions at 80 kVp can increase iodine attenuation and image contrast of soft-tissue structures and reduce radiation exposure.13–15 However, only a few studies have investigated low-tube-voltage acquisition CT techniques for imaging of the neck.16–18 We hypothesized that an 80-kVp acquisition may provide comparable image quality for evaluation of the neck region. To evaluate the efficacy of this technique in simulated routine clinical practice, we retrospectively assessed the diagnostic accuracy of low-tube-voltage 80-kVp image series from dual-energy neck CT (DECT) for evaluation of a variety of cervical pathologies, and the results were compared with linearly blended images representing a standard 120-kVp acquisition. We also assessed interobserver agreement and calculated the potential radiation dose reduction.
Materials and Methods
Patient Selection and Study Design
This retrospective study was approved by the ethics committee of our hospital, and written informed consent was waived. Of 404 clinically indicated neck DECT examinations performed between February 2010 and November 2010 at our institution, we included 170 consecutive examinations. During that timeframe, neck CT examinations were performed by using 2 different CT systems at our facility; only the patients scanned by using the dual-source system capable of DECT mode were included in this study. However, assignment to either scanner was completely random on the basis of available timeslots and was not influenced for research purposes.
Contraindications for DECT imaging were known allergies to iodinated contrast material, pregnancy, and impaired renal function (estimated glomerular filtration rate below 40 mL/min). Exclusion criteria for this study were age younger than 18 years (n = 15), noncontrast studies (n = 4), CT angiography examinations (n = 26), and severe motion (n = 21) or metal artifacts (n = 49) in case-relevant anatomic regions. Furthermore, to retain study group homogeneity, we excluded patients referred for evaluation of cervical metastasis from distal neoplasms (n = 6). In case a patient underwent multiple DECT examinations during this timeframe, we included only the first examination and excluded subsequent studies (n = 113).
To simulate routine clinical practice, we aggregated 3 main groups of indications for imaging: SCC-related (group 1, n = 107), lymphoma-related (group 2, n = 40), and benign conditions (group 3, n = 23). Groups 1 and 2 included CT examinations for the primary staging of known malignancy, detection of suspected malignancy, and follow-up CT to rule out recurrence. Patients with follow-up DECT were only included if the prior non-DECT scan did not show a recurrent SCC or pathologically enlarged lymph nodes in patients with known lymphoma to avoid miscategorizing patients with tumor remnants as having recurrent tumors. Group 3 consisted of patients referred for detection or evaluation of suspected benign conditions (eg, para-/retropharyngeal abscess, sialadenitis with possible sialolithiasis, Warthin tumor). A detailed list of indications for CT is summarized in Table 1.
Table 1:
Indications for neck CT imaging (n = 170)
| Indication | No. |
|---|---|
| Squamous cell carcinoma | 107 |
| Primary staging or detection of suspected squamous cell carcinoma | 66 |
| Follow-up to detect tumor recurrence | 41 |
| Lymphoma | 40 |
| Primary staging or detection of suspected lymphoma | 19 |
| Follow-up to detect lymphoma recurrence | 21 |
| Benign conditions | 23 |
| Suspected benign cervical mass (eg, Warthin tumor, adenoma) | 5 |
| Suspected cervical abscess | 13 |
| Suspected sialadenitis | 3 |
| Suspected branchial cleft cyst | 2 |
The criterion standard in this study for comparison of observer results was based on the combination of the electronic medical records, results from histopathology, and the original CT imaging report, ranked in that order. However, because the original CT imaging reports of the evaluated scans may have resulted in false-positive or false-negative findings, especially in initial and follow-up examinations of patients with SCC, we ranked the final clinical diagnosis first because it also included clinical knowledge from physical examinations and biopsy; correlation with clinical diagnosis is especially important in SCC of the oral cavity, for example, which may be missed on neck CT. Thus, a final diagnosis of recurrent head-neck SCC based on histopathologic findings overruled a false-negative or uncertain finding in the original CT imaging report.
DECT Protocol
All CT examinations in this study were performed by using a second-generation 128-section dual-source CT in dual-energy mode (Somatom Definition Flash; Siemens, Erlangen, Germany). Both x-ray tubes were operated at a different tube potential. Examination parameters were as follows: tube A: 80 kVp, reference current-time product of 302 mAs per rotation; tube B: Sn140 kVp with a tin filter; 151 mAs per rotation; rotation time, 0.5 seconds; pitch, 0.9; collimation, 2 × 64 × 0.6 mm. Real-time automatic milliampere-second-modulation software (CareDose4D; Siemens) was used to regulate the tube current, depending on the patient's anatomy. Images were acquired in a craniocaudal direction in expiratory breath-hold with the patient in a supine position. The scan range extended from the upper orbital rim to the aortic arch. DECT imaging was initiated 70 seconds after the start of intravenous administration of 100 mL of nonionic iodinated contrast agent (iopamidol, Imeron 400; Bracco-Altana Pharma, Konstanz, Germany) through an antecubital vein at a flow rate of 2 mL/s.
On the basis of the DECT raw data, the scanner automatically reconstructed an image series with a standard linear blending setting (M_0.3), merging 30% of the 80-kVp and 70% of the 140-kVp data spectrum, representing a 120-kVp acquisition. All images were reconstructed with a dedicated dual-energy medium-soft convolution kernel (D30f) and a section thickness of 2.0 mm. Evaluation of image series was limited to axial images, and multiplanar reformations were not assessed. Quantitative DECT data were also not analyzed in this study.
Image Analysis
Initially only the 80-kVp image series was evaluated on a regular PACS workstation by 3 radiologists with 7, 3, and 2 years of experience in neck CT, respectively. All image series were assessed in random order. To avoid potential recall bias, readers were aware of the indication for CT imaging but were blinded to any other clinical information or auxiliary image series (ie, prior imaging studies). Readers were allowed to scroll through the whole stack of CT images. Window settings were automatically set to predetermined standard values for evaluation of soft tissue (width, 400 Hounsfield units; level, 80 Hounsfield units) but were freely adjustable. After a time interval of 12 weeks, all blended 120-kVp images from these cases were evaluated by the same readers in the same fashion and random order to allow an assessment of the diagnostic accuracy of a standard 120-kVp acquisition.
Radiation Dose Estimations
Examination protocols were evaluated, and the resulting volume CT dose index (CTDIvol) and dose-length-product (DLP) were recorded for each scan. Currently, examination protocols provided by the second-generation dual-source CT scanner used in this study only display cumulative CTDIvol and DLP values when scans are obtained in dual-energy mode and do not allow a further division of emitted radiation between both tubes with different voltage settings. However, to allow an intraindividual analysis of the estimated radiation dose without additional radiation exposure and to avoid potential bias among different study groups, we used dedicated software designed specifically for this study so that all DICOM datasets and CTDIvol values of each of the 80-kVp series were extracted and averaged. CTDIvol values are, in great part, also present in the patient protocols of each examination, which are usually used for analysis of the radiation dose. The given DLP of the cumulative DECT examination was divided by the cumulative CTDIvol to calculate a conversion factor. The calculated mean CTDIvol of the 80-kVp series based on the extracted data was then multiplied by this conversion factor to calculate the resulting estimated DLP for the low-tube-voltage acquisition.
Statistical Analysis
All statistical analyses were conducted by using dedicated software (SPSS, Version 21; IBM, Armonk, New York; and MedCalc for Windows, Version 13; MedCalc Software, Mariakerke, Belgium). Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated for each observer and type of image series. The means and SDs of metric data were calculated. The paired t test was used to compare the CTDIvol and DLP between the calculated values of the 80-kVp tube and the cumulative dual-energy CT examination. A P value < .05 indicated a statistically significant difference for all used tests.
Interobserver agreement among the 3 radiologists was evaluated by using intraclass correlation coefficient (ICC) statistics. Cumulative and subgroup-related ICC values were calculated. The ICC value was interpreted in the following way: ICC < 0.20, slight agreement; ICC = 0.21–0.40, fair agreement; ICC = 0.41–0.60, moderate agreement; ICC = 0.61–0.80, substantial agreement; ICC = 0.81–1.0, almost perfect agreement.
Results
The study group consisted of 170 patients (57.2 ± 16.3 years [range, 18–94 years]), comprising 114 male (56.3 ± 16.2 years [range, 18–94 years]) and 56 female (58.9 ± 16.6 years [range, 23–89 years]) patients.
All DECT examinations were performed without any complications, and no severe motion or metal artifacts were present. The mean cumulative CTDIvol of all examinations was 10.04 ± 0.80 mGy, and the calculated isolated CTDIvol of the 80-kVp tube was 4.82 ± 0.41 mGy (P < .001). The mean cumulative DLP was 282.2 ± 30.2 mGy × cm, and the mean calculated isolated 80-kVp DLP was 135.5 ± 14.7 mGy × cm (P < .001), resulting in an estimated dose reduction of approximately 48.0%.
Criterion Standard Final Clinical Diagnoses
One hundred seven patients underwent SCC-related neck DECT. The findings of the 3 observers for 80-kVp and blended 120-kVp images were compared with the criterion standard on the basis of the combination of the electronic medical records, results from histopathology, and the original CT imaging report. Primary neck SCC was present in 50 cases and absent in 16 cases. SCC recurrence was diagnosed in 15 cases and ruled out in 26 cases. The primary and recurrent SCC sites were the hypopharynx and larynx (n = 21), oropharynx (n = 17), nasopharynx (n = 11), buccal soft tissue (n = 6), floor of mouth (n = 5), tongue (n = 3), and nose (n = 2). On the basis of the Tumor, Node, Metastasis classification, we evaluated 15 T1 tumors, 17 T2 tumors, 12 T3 tumors, and 21 T4 tumors. Data for the degree of spread to the lymph nodes were not available for all cases and thus were not included. Average follow-up of SCC-related cases was 21.3 months.
Forty patients completed lymphoma-related neck DECT. Primary lymphoma was diagnosed in 12 patients and ruled out in 7. Recurrent cervical lymphoma was present in 8 patients and ruled out in 13.
Twenty-three patients underwent neck DECT to assess suspected benign conditions. A primary benign tumor (eg, Warthin tumor, adenoma) was present in 5 patients. Primary abscess was diagnosed in 7 patients and ruled out in 4. Abscess recurrence was present in 1 patient and ruled out in 1. Findings of sialadenitis or sialolithiasis as the main diagnosis were present in 3 patients. A branchial cleft cyst was diagnosed in 2 patients.
Diagnostic Accuracy of 80-kVp and Blended 120-kVp Scans
The mean global (and individual) sensitivity and NPV for all 3 observers for evaluation of 80-kVp and blended 120-kVp image series in this study were 94.8% and 91.1%, respectively. Specificity and PPV were 93.0% and 95.9% for both image series. Summarized results regarding the analysis of diagnostic accuracy are listed in Table 2.
Table 2:
Comparison of diagnostic accuracy of the 3 observersa
| Value | Global (n = 170) | SCC-Related (n = 107) | Lymphoma-Related (n = 40)b | Benign Conditions (n = 23) |
|---|---|---|---|---|
| 80-kVp image series | ||||
| Sensitivity | 94.8% (93.5%–95.4%) | 94.8% (91.4%–97.2%) | 95.0% | 94.3% (88.9%–100.0%) |
| Specificity | 93.0% (91.9%–95.1%) | 89.1% (86.5%–91.7%) | 100.0% | 93.3% (80.0%–100.0%) |
| PPV | 95.9% (95.3%–97.2%) | 94.3% (93.1%–95.8%) | 100.0% | 98.2% (94.7%–100.0%) |
| NPV | 91.1% (89.1%–92.1%) | 90.1% (84.6%–94.3%) | 95.2% | 85.7% (71.4%–100.0%) |
| 120-kVp image series | ||||
| Sensitivity | 94.8% (92.6%–96.3%) | 95.3% (91.4%–97.2%) | 95.0% | 92.5% (88.9%–94.4%) |
| Specificity | 93.0% (91.9%–95.1%) | 89.1% (86.5%–91.7%) | 100.0% | 93.3% (80.0%–100.0% |
| PPV | 95.9% (95.3%–97.2%) | 94.4% (93.2%–95.8%) | 100.0% | 98.1% (94.4%–100.0%) |
| NPV | 91.1% (87.7%–93.5% | 91.0% (84.6%–94.3%) | 95.2% | 79.0% (71.4%–85.7%) |
Values are given as mean (range).
No interobserver differences, therefore no ranges, are given.
Compared with the global scores, diagnostic accuracy for the evaluation of the subgroup of SCC showed a similarly high sensitivity for 80-kVp and 120-kVp images (94.8%, 95.3%), a decreased specificity (both 89.1%), and slightly lower PPV (94.3%, 94.4%) and NPV (90.1%, 91.0%).
Diagnostic accuracy was consistently higher for lymphoma-related imaging with a sensitivity of 95.0%, a specificity and PPV of 100.0%, and an NPV of 95.2% for both image series.
Evaluation of 80- and 120-kVp image series from examinations performed due to benign indications showed a sensitivity of 94.3%/92.5%, a specificity of 93.3%/93.3%, a PPV of 98.2%/98.1%, and an NPV of 85.7%/79.0%.
Interobserver Agreement
The global ICC score for all 3 reviewers for 80-kVp images was 0.82 (95% CI, 0.76–0.86), and for blended 120-kVp images, it was 0.80 (95% CI, 0.74–0.85), interpreted as almost perfect agreement. Interobserver agreement for SCC-related CT examinations was substantial for 80-kVp image series with an ICC score of 0.79 (95% CI, 0.70–0.85) and for blended 120-kVp images with an ICC of 0.76 (95% CI, 0.66–0.82). Evaluation of lymphoma-related examinations resulted in a perfect interobserver agreement with an ICC score of 1.0 for both image series. The 80-kVp imaging for the evaluation of benign conditions showed a substantial interobserver agreement for the 80-kVp image series with an ICC score of 0.72 (95% CI, 0.45–0.87) and for the blended 120-kVp images with an ICC of 0.69 (95% CI, 0.41–0.83).
Discussion
The findings of our study indicate that compared with standard 120-kVp imaging, low-tube-voltage 80-kVp CT provides sufficient image quality for evaluation of the neck region in routine clinical practice and simultaneously allows a distinct reduction of radiation exposure. We found very high global sensitivity, specificity, PPV, and NPV and substantial interobserver agreement for the 3 reviewers with varying levels of experience with neck CT. Our results suggest that low-tube-voltage 80-kVp acquisitions may be used in routine clinical practice to substantially lower the cumulative radiation dose for patients undergoing neck CT.
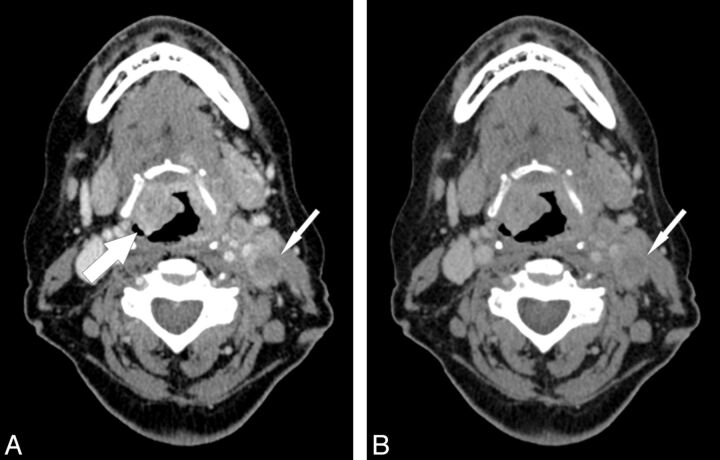
While clinicians unacquainted with low-tube-voltage acquisitions might be concerned about false-negative findings regarding the detection of cervical malignancy, our results indicate that cervical SCC can be reliably diagnosed by using this technique with a consistently high sensitivity, though malignancy and especially SCC recurrence in the early stages may be present but undetectable on CT as a general limitation of the technique.19 The high NPV in our study also indicates that neck SCC was reliably ruled out with this technique in our patient population. The additional evaluation of blended 120-kVp images representing standard acquisitions showed no significant differences for this subgroup. Furthermore, we found that low-tube-voltage acquisitions provided an increased signal attenuation and consequently improved SCC border contrast (Fig 1). Consequently, necrotic metastatic lymph nodes may also be better depicted with low-tube-voltage acquisitions as demonstrated in Fig 1. Nevertheless, the increased signal attenuation usually requires modifying the window width and level settings for evaluation of 80-kVp studies compared with standard 120-kVp examinations. In addition, low-tube-voltage acquisitions may result in an increased focal spot blooming and more severe metal artifacts. Nevertheless, these limitations may be mitigated with the recently introduced third-generation dual-source CT.20
Fig 1.
A 61-year-old female patient with a primary supraglottic laryngeal carcinoma (T4a N2c). Low-tube-voltage acquisition (A) improves tumor attenuation (large arrow) compared with the standard blended 120-kVp image series (B) and also shows a higher contrast and improved depiction of cervical lymph node metastasis (small arrows) (window settings: width, 400 HU; level, 80 HU).
Prior studies have also demonstrated that low-tube-voltage neck CT results in a superior contrast-to-noise ratio compared with 120-kVp scans.16,18 Because patients with neck SCC often undergo multiple CT examinations and radiation therapy, the benefit for this specific patient group from low-tube-voltage acquisitions may be limited. Nevertheless, younger patients with suspected or known lymphoma and patients in whom primary neck SCC can be ruled out on the basis of CT findings may particularly benefit from a dose-saving 80-kVp CT technique.
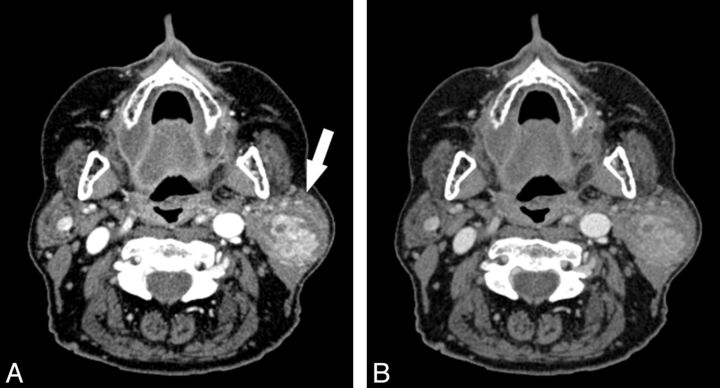
Several previous studies have demonstrated that the radiation dose during head and neck CT angiography can be substantially reduced with low-tube-voltage acquisitions.21–23 Intravenously administered iodinated contrast material shows an increased signal attenuation when exposed to lower tube voltages, which can also improve soft-tissue contrast (Fig 2).13–15 However, only a few prior studies evaluated low-tube-voltage CT acquisitions for imaging the soft-tissue structures of the neck region.16–18 Gnannt et al16 demonstrated that the consecutive increase in soft-tissue attenuation on 70-kVp scans is higher than the corresponding increase in image noise, therefore resulting in a superior contrast-to-noise ratio for neck imaging. They reported a dose reduction of 34% with 70-kVp acquisitions compared with standard 120-kVp acquisitions. We found an estimated dose reduction of 48% with 80-kVp acquisitions based on extraction of CTDIvol values from DECT datasets, but the actual dose savings may be less with single-energy 80-kVp acquisitions. Toepker et al18 reported a peak in image quality for the 80-kVp images of neck DECT in patients with oral cancer, emphasizing the clinical applicability of low-tube-voltage acquisitions.
Fig 2.
A 66-year-old female patient with a vascularized mass (arrow) in the left parotid gland. She underwent excision, and a Warthin tumor was confirmed by histopathology. The increased iodine attenuation with an 80-kVp acquisition (A) results in a distinctly increased image contrast of the mass compared with the standard 120-kVp acquisition (B) (window settings: width, 400 HU; level, 80 HU).
The results of this study should be interpreted in the context of the study design and consequent limitations. First, although a study group of 170 patients was reasonable for this initial study, further re-evaluation of our findings with low-tube-voltage acquisitions in larger patient cohorts is necessary. Second, there may be differences regarding the average radiation exposure of neck DECT among various dual-source CT systems. We also expect differences between single- or dual-source 80-kVp CT, and our results from retrospective analysis of the 80-kVp images from DECT should be evaluated in additional studies with phantom measurements. Especially single-source 80-kVp CT may also show a different image quality because the 140-kVp tube in DECT may have an effect on the 80-kVp DECT images. However, 80-kVp neck CT can still be expected to result in a distinct dose reduction.16 DECT may result in a slower scan speed than certain single- or dual-source CT systems, which may lead to more motion artifacts, which were a potential exclusion criterion in our study. Third, there were far more SCC-related examinations included than the other subgroups. While we also excluded patients undergoing neck CT for evaluation of cervical metastasis from distant neoplasm, we assumed that our results regarding the detection of cervical lymphoma can be transferred to the detection of metastatic cervical lymph nodes. Fourth, although the mathematic calculations of the DICOM-reading software used in our study are ordinary and only use data that are included in the DICOM headers per se and are included in the patient protocols, the diagnostic accuracy of this technique for the estimation of low-tube-voltage radiation exposure from DECT examinations has not been validated in prior studies. Fifth, to allow an optimal comparability, we compared image series from the same patients, which may have led to potential bias though there was a 12-week interval between evaluations of both series. In addition, reviewers were blinded to any auxiliary previous imaging studies and only assessed axial images; this process does not reflect routine clinical practice for follow-up CT in patients with known neck malignancy and may have influenced diagnostic accuracy.
Conclusions
Our results demonstrate that low-tube-voltage 80-kVp neck CT provides a high diagnostic accuracy and interobserver agreement for the evaluation of various cervical pathologies and suggests that this technique may be used in routine clinical practice to substantially reduce cumulative radiation exposure for patients.
ABBREVIATIONS:
- CTDIvol
volume CT dose index
- DECT
dual-energy CT
- DLP
dose-length product
- ICC
intraclass correlation coefficient
- NPV
negative predictive value
- PPV
positive predictive value
- SCC
squamous cell carcinoma
Footnotes
Disclosures: J. Matthias Kerl—UNRELATED: Payment for Lectures (including service on Speakers Bureaus): Siemens. Ralf W. Bauer—UNRELATED: Payment for Lectures (including service on Speakers Bureaus): Siemens.
References
- 1. Sadick M, Schoenberg SO, Hoermann K, et al. Current oncologic concepts and emerging techniques for imaging of head and neck squamous cell cancer. GMS Curr Top Otorhinolaryngol Head Neck Surg 2012;11:Doc08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hermans R. Staging of laryngeal and hypopharyngeal cancer: value of imaging studies. Eur Radiol 2006;16:2386–400 [DOI] [PubMed] [Google Scholar]
- 3. Castelijns JA, van den Brekel MW. Imaging of lymphadenopathy in the neck. Eur Radiol 2002;12:727–38 [DOI] [PubMed] [Google Scholar]
- 4. Hoang JK, Branstetter BF 4th, Eastwood JD, et al. Multiplanar CT and MRI of collections in the retropharyngeal space: is it an abscess? AJR Am J Roentgenol 2011;196:W426–32 [DOI] [PubMed] [Google Scholar]
- 5. Clavel S, Charron MP, Bélair M, et al. The role of computed tomography in the management of the neck after chemoradiotherapy in patients with head-and-neck cancer. Int J Radiat Oncol Biol Phys 2012;82:567–73 [DOI] [PubMed] [Google Scholar]
- 6. Brenner DJ, Hall EJ. Computed tomography: an increasing source of radiation exposure. N Engl J Med 2007;357:2277–84 [DOI] [PubMed] [Google Scholar]
- 7. Kalra MK, Maher MM, Toth TL, et al. Techniques and applications of automatic tube current modulation for CT. Radiology 2004;233:649–57 [DOI] [PubMed] [Google Scholar]
- 8. Bodelle B, Bauer RW, Holthaus L, et al. Dose and image quality of high-pitch dual source computed tomography for the evaluation of cervical lymph node status: comparison to regular 128-slice single source computed tomography. Eur J Radiol 2013;82:e281–85 [DOI] [PubMed] [Google Scholar]
- 9. Schell B, Bauer RW, Lehnert T, et al. Low-dose computed tomography of the paranasal sinus and facial skull using a high-pitch dual-source system–first clinical results. Eur Radiol 2011;21:107–12 [DOI] [PubMed] [Google Scholar]
- 10. Becker HC, Augart D, Karpitschka M, et al. Radiation exposure and image quality of normal computed tomography brain images acquired with automated and organ-based tube current modulation multiband filtering and iterative reconstruction. Invest Radiol 2012;47:202–07 [DOI] [PubMed] [Google Scholar]
- 11. Bodelle B, Klein E, Naguib NN, et al. Acute intracranial hemorrhage in CT: benefits of sinogram-affirmed iterative reconstruction techniques. AJNR Am J Neuroradiol 2014;35:445–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schulz B, Beeres M, Bodelle B, et al. Performance of iterative image reconstruction in CT of the paranasal sinuses: a phantom study. AJNR Am J Neuroradiol 2013;34:1072–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nakayama Y, Awai K, Funama Y, et al. Abdominal CT with low tube voltage: preliminary observations about radiation dose, contrast enhancement, image quality, and noise. Radiology 2005;237:945–51 [DOI] [PubMed] [Google Scholar]
- 14. Macari M, Spieler B, Kim D, et al. Dual-source dual-energy MDCT of pancreatic adenocarcinoma: initial observations with data generated at 80 kVp and at simulated weighted-average 120 kVp. AJR Am J Roentgenol 2010;194:W27–32 [DOI] [PubMed] [Google Scholar]
- 15. Nakaura T, Awai K, Oda S, et al. Low-kilovoltage, high-tube-current MDCT of liver in thin adults: pilot study evaluating radiation dose, image quality, and display settings. AJR Am J Roentgenol 2011;196:1332–38 [DOI] [PubMed] [Google Scholar]
- 16. Gnannt R, Winklehner A, Goetti R, et al. Low kilovoltage CT of the neck with 70 kVp: comparison with a standard protocol. AJNR Am J Neuroradiol 2012;33:1014–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hoang JK, Yoshizumi TT, Nguyen G, et al. Variation in tube voltage for adult neck MDCT: effect on radiation dose and image quality. AJR Am J Roentgenol 2012;198:621–27 [DOI] [PubMed] [Google Scholar]
- 18. Toepker M, Czerny C, Ringl H, et al. Can dual-energy CT improve the assessment of tumor margins in oral cancer? Oral Oncol 2014;50:221–27 [DOI] [PubMed] [Google Scholar]
- 19. Sullivan BP, Parks KA, Dean NR, et al. Utility of CT surveillance for primary site recurrence of squamous cell carcinoma of the head and neck. Head Neck 2011;33:1547–50 [DOI] [PubMed] [Google Scholar]
- 20. Meinel FG, Canstein C, Schoepf UJ, et al. Image quality and radiation dose of low tube voltage 3(rd) generation dual-source coronary CT angiography in obese patients: a phantom study. Eur Radiol 2014;24:1643–50 [DOI] [PubMed] [Google Scholar]
- 21. Zhang WL, Li M, Zhang B, et al. CT angiography of the head-and-neck vessels acquired with low tube voltage, low iodine, and iterative image reconstruction: clinical evaluation of radiation dose and image quality. PLoS One 2013;8:e81486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Xia W, Wu JT, Yin XR, et al. CT angiography of the neck: value of contrast medium dose reduction with low tube voltage and high tube current in a 64-detector row CT. Clin Radiol 2014;69:e183–89 [DOI] [PubMed] [Google Scholar]
- 23. Kayan M, Köroğlu M, Yešildağ A, et al. Carotid CT-angiography: low versus standard volume contrast media and low kV protocol for 128-slice MDCT. Eur J Radiol 2012;81:2144–47 [DOI] [PubMed] [Google Scholar]