Abstract
BACKGROUND AND PURPOSE:
TCCFs are a common complication following craniofacial trauma and are usually treated by coils or detachable balloons. The use of the liquid embolic agent Onyx as the sole agent for the treatment of TCCFs has been rarely reported. Herein, we summarized the preliminary experience and effectiveness of treating TCCFs with Onyx in 23 patients.
MATERIALS AND METHODS:
From the 36 type A CCFs treated in our department between September 2005 and March 2011, a total of 23 posttraumatic direct CCFs were treated by using Onyx only via transarterial approach.
RESULTS:
Immediate postprocedural angiograms demonstrated complete occlusion in all patients. All the patients underwent a single procedure except 1 with bilateral TCCFs. Up to 24-month clinical and 3-month angiographic follow-ups revealed an ongoing complete occlusion without any complications.
CONCLUSIONS:
In this series, the use of Onyx for the transarterial embolization of TCCFs was feasible and effective. Associated adverse events were rare.
TCCFs are direct arteriovenous communications between the ICA and CS, resulting from a traumatic tear of the cavernous segment of the ICA by skull fracture fragments following craniofacial trauma. TCCFs are always treated with endovascular therapy because of the high flow rates of the fistula site. Embolic agents, including detachable balloons, coils, nBCA, and the nonadhesive liquid embolic agent ethylene-vinyl alcohol copolymer (Onyx; ev3 Neurovascular, Irvine, California) are delivered via a transarterial or transvenous approach. Currently Onyx is usually used in combination with other solid embolic agents. The use of Onyx as the sole embolic agent for TCCFs has been rarely reported.1,2 In this article, we report our preliminary experience of the use of Onyx for TCCFs in 23 patients.
Materials and Methods
Patient Population
We reviewed records of 156 patients treated in our department between September 2005 and March 2011 with 4 types of carotid cavernous fistulas, according to the classification established by Barrow et al.3 Among these patients, 36 had type A, of whom 23 (15 men and 8 women; age range, 23–65 years; average age, 36.3 years) were both posttraumatic and treated with Onyx. For the other 13 patients, 4 were treated with detachable balloons for economic reasons, 8 were treated with Onyx and coils, and 1 had spontaneous CCF without trauma.
The onset of first symptom was within 1–4 months after trauma. Three patients had undergone treatment with detachable balloon embolization before admission, but recurrences developed or clinical symptoms persisted due to detachable balloon deflation or residual fistulas. The study was reviewed and approved by the institutional review board at Changhai Hospital.
Clinical Presentations
All patients had pulsating tinnitus, proptosis, and significant conjunctival chemosis. Seventeen had vision problems, such as blurred vision, diplopia, and hypoposia; 2 also presented with blepharoptosis and limitation of ocular movement. No cerebral hemorrhage was identified in these patients. Posttraumatic CT scans of 14 patients revealed skull fractures, and axial MR imaging of 17 patients demonstrated dilated superior ophthalmic veins and orbital tissue edema.
Angiographic Features
Complete cerebral angiography of both internal and external carotid arteries and bilateral vertebral arteries was performed in 23 patients. To identify the main site of a fistula, we performed an injection from the contralateral carotid or 1 vertebral artery, while manually compressing the ipsilateral carotid artery. Twelve fistulas were located on the right ICA and 10 on the left. Only 1 case had TCCFs in the bilateral ICAs. ICA injection revealed that 17 fistula ostiums were located in the C3 portion of the carotid siphon and 7, in the C4 portion of the carotid siphon. Drainage veins included the superior (17/24) and inferior (13/24) ophthalmic veins, superior (20/24) and inferior (19/24) petrosal sinuses, cortex veins (14/24), and contralateral cavernous sinuses (12/24). Three angiograms revealed venectasia, and ICA dissection was observed in 4 patients.
Endovascular Procedure
All the procedures were performed with the patients under general anesthesia. A 6F Envoy guiding catheter (Cordis Endovascular, Miami Lakes, Florida) was introduced through the femoral artery into the ICA where the fistula was located. Then a HyperGlide balloon (4 mm in diameter and 20 mm in length; ev3 Neurovascular) was placed across the fistula ostium, and an Echelon-10 (ev3 Neurovascular) microcatheter was superselectively navigated into the CS through the fistula. The balloon was inflated under road-mapping, and it was confirmed that the balloon totally covered the fistula by CS injection through the Echelon-10 microcatheter and/or ICA injection through the guiding catheter. Onyx-18 or Onyx-34 was injected under real-time road-mapping. When the unwanted cast of Onyx was observed, we stopped injection for 30 seconds to 2 minutes to solidify the Onyx polymerization; the injection was then restarted.4 During the procedure, the balloon was deflated and angiography was performed through the guiding catheter to confirm total occlusion of the fistula. All the interventional procedures were performed by extensively experienced interventional vascular neurosurgeons (J.L., Y.X., Q.H., B.H., W.Z.).
Results
In all 23 patients, transarterial embolization by using Onyx was technically successful. There was only 1 case with bilateral fistulas that were treated by a staged procedure to reduce the risk of hyperperfusion, due to concern about the great change of cerebral hemodynamics after total occlusion of the fistula. As for the other 22 cases with fistulas in 1 ICA, immediate postembolization angiograms confirmed complete occlusion with good preservation of the ICA in single procedure, with a success rate of 100%. A significant improvement was obtained with resolution of pulsating tinnitus, eye symptoms, and neurologic deficits within 2–7 days in all cases, and no new neurologic signs were observed on discharge from the hospital.
The 3-month follow-up digital subtraction angiography in 9 patients and MR angiography in 8 patients confirmed stable obliteration with good preservation of the ICA. None of the 23 patients experienced recurrent pulsating tinnitus and eye symptoms during and up to a 24-month clinical follow-up. In this series, the volume of Onyx was 3.6–4.7 mL (3.94 mL on average). The total time of Onyx injection was 27–70 minutes. No microcatheter retention or other complications occurred during or after the procedure, such as embolic or hemorrhagic complications, hypotension, and bradycardia because of trigeminocardiac reflex.5 All the follow-ups were performed by 2 neurologists from the neurology department of our clinical center (B.D., Y.W) as a part of usual clinical care.
Discussion
Endovascular treatment for TCCFs aims at total occlusion of the fistulous communications to decrease the pressure in the CS and improve cerebral perfusion. However, controversy still exists regarding the optimal treatment strategy for these lesions. Transarterial embolization with detachable balloons used to be the standard treatment of TCCFs.6,7 The reported cure rate with balloon embolization of direct CCFs is 88%–99%,8–10 and the ICA preservation is 88%–98%.8,11 However, technical problems of detachable balloons, such as early detachment, deflation, and rupture of the balloon caused by bone fragments, may result in some severe complications or recurrence of the fistula.10 Among the 23 patients in our series, 3 had been treated by detachable balloon embolization before admission to our hospital, with total occlusion in 2 patients and partial occlusion in 1 patient. However, postprocedural symptoms, including pulsating tinnitus, proptosis, and chemosis, recurred in 1–3 months. Angiographic follow-ups in all these cases demonstrated deflation of the balloon and recurrence of the fistula. The FDA approved the first detachable balloons, Silicone Mini Balloon (Becton-Dickinson, Rutherford, New Jersey), for peripheral vessel occlusion in 1982, and in 1990 the manufacturer withdrew this device for financial reasons.12 Detachable balloons (DSB; Boston Scientific-Target, Fremont, California) for intracranial use were approved by the FDA in 1991. Because of balloon valve leaks, these were withdrawn from use in United States13; however, the balloon remains in clinical use for the treatment of TCCFs in many other countries, especially in China. Coils, especially hydrogel-coated coils, for the embolization of TCCFs were reported to be safe, effective, and controllable and a stable method of maintaining high carotid artery patency.14 However, the cost of this therapy is so high that many patients cannot afford it, especially in developing countries like China. Moreover, it is difficult to identify herniation of coil loops in the ICA when the fistula ostium is too large. To some extent, stent-assisted coil embolization for TCCFs may solve this technical problem,15 but anticoagulant and antiplatelet therapy after stent placement may decrease the complete occlusion rate of the fistula. In recent years, the covered stent also became available for patients with TCCFs whose fistulas cannot be successfully occluded with detachable balloons or detachable coils.16–18 Its main drawback for intracranial use is the limited longitudinal flexibility, and more investigation is required to further develop its specifications and indications.17
Onyx is a liquid mixture of ethylene-vinyl alcohol copolymer and suspended tantalum powder for radiopacity in a DMSO solvent. Mixed in varying proportions, the manufacturer can produce Onyx in different concentrations for different vascular disorders. This nonadhesive embolic polymer precipitates and solidifies in the vessel as DMSO diffuses away in blood. The nonadhesive nature of Onyx permits a long and controlled infusion. The direction of the Onyx casting in the vessel changes as the injection speed slows down. Therefore, Onyx can be cast in the sinus or vessels adequately. Onyx embolizations become the preferred treatment for brain AVMs and DAVFs, and its safety and efficacy have been fully evaluated.19–22
TCCFs are different from spontaneous cavernous sinus DAVFs. The latter are often complicated and with a bilateral arterial or both internal and external carotid artery supply. The feeding artery is often so tiny that the transarterial approach still remains a technical challenge. The former are the direct communications between ICA and CS, where embolization via a transarterial approach is very convenient because the microcatheter may be easily navigated to the CS through the fistula with a guidewire. Although the use of Onyx is well-controlled with long injection features, it has a potential risk of occluding ICA-external carotid artery anastomoses.23 However, injection resistance in the CS is low and especially for TCCFs, the fistula is directed to the CS. Accordingly, the risk of misembolization of pre-existing collateral vessels is also relatively lower than that in cavernous sinus DAVFs. Therefore, the avoidance of Onyx reflux to the ICA from the CS through the fistula ostium is the key to avoiding severe embolic complications. In our series, we used a nondetachable balloon within the ICA to cover the fistula ostium before Onyx injection and confirmed total coverage with angiography of CS injection through the microcatheter and/or ICA injection through the guiding catheter.
Despite the protection of nondetachable balloons, there is no denying that a tiny quantity of Onyx may spill over the ostium and cast between the artery and the nondetachable balloon at the end of the Onyx injection, but the quantity of the excess Onyx is too tiny to be observed. What bothered us was that the flaking of the Onyx might cause new infarctions. We are delighted that no ischemic complications occurred, and all the treated ICAs were well preserved among these 23 patients.
However, TCCFs usually follow a traumatic tear of the cavernous segment of the ICA by skull fracture fragments, so the location and the size of the fistula ostium are very difficult to ascertain due to the high flow rates, especially in the case of total arterial steal. Furthermore, the superselective navigation of a nondetachable balloon to the distal ICA may be difficult due to a large fistula because of high rates of blood flow of the fistula. Under such circumstances, pre-embolization with a detachable balloon could be performed first. The detachable balloon in the CS decreases the blood flow rates of the fistula and facilitates the navigation of the protective balloon, and at the same time, pre-embolization with a detachable balloon may reduce the volume of Onyx and the injection time. In addition, the Onyx casting around the detachable balloon also protects the balloon from rupture by bone fragments. In 1 case, as depicted in Fig 1, the patient underwent detachable balloon embolization before being admitted to our department, and angiograms demonstrated deflation of the balloons and a total arterial steal. In the treatment procedure, it was very difficult to navigate the guidewire of the nondetachable balloon across the fistula site superselectively to the distal part of the ICA. Therefore, we performed an unplanned pre-embolization with a detachable balloon first to decrease the blood rate of the fistula ostium. Afterward, we successfully positioned the protective nondetachable balloon within the ICA and occluded the fistula completely with 3.6 mL of Onyx-34. The 3-month digital subtraction angiography confirmed the complete occlusion of the TCCFs.
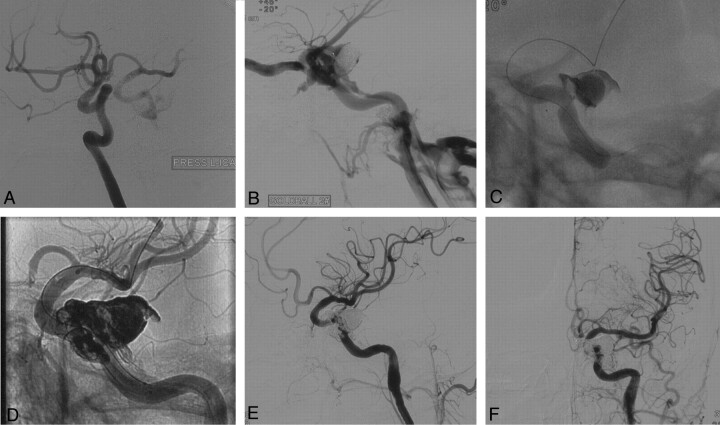
Fig 1.
A, The fistula ostium is definitely identified by the pressing test of the left ICA. B, Pre-embolization with a detachable balloon first. C, Onyx-34 is injected under the protection of a nondetachable balloon within the ICA. D, The Onyx cast postembolization. E, Immediate angiogram reveals complete occlusion. F, The 3-month digital subtraction angiography confirms complete occlusion of the TCCF.
Delayed cranial nerve palsy has been reported with the use of coils24 and nBCA.25 We were concerned about the same complication with the use of Onyx, especially that the solvent DMSO might have neurotoxicity26 on cranial nerves in the CS. Nevertheless, after an up-to 24-month follow-up, there was no demonstrated aforementioned complication among these 23 patients. The reasons might be as follows: First, for a direct CCF, we just needed to occlude the ostium of the fistula; therefore, there should be more Onyx around the ostium instead of in the CS and less compression to the nerves in the CS. Second, we did find delayed cranial nerve palsies with the use of Onyx for the treatment of cavernous sinus DAVFs due to devascularization of the vasa nervorum. The risk of misembolization of pre-existing collateral vessels with the use of Onyx for the treatment of TCCFs is relatively smaller than that in cavernous sinus DAVFs as mentioned above.
The change of cerebral hemodynamics after complete occlusion of the fistula may result in hyperperfusion syndrome. Thus for patients with bilateral fistulas and total arterial steal, a staged procedure may be very important to reduce the risk of hemorrhagic reperfusion, as in the case demonstrated in Fig 2.
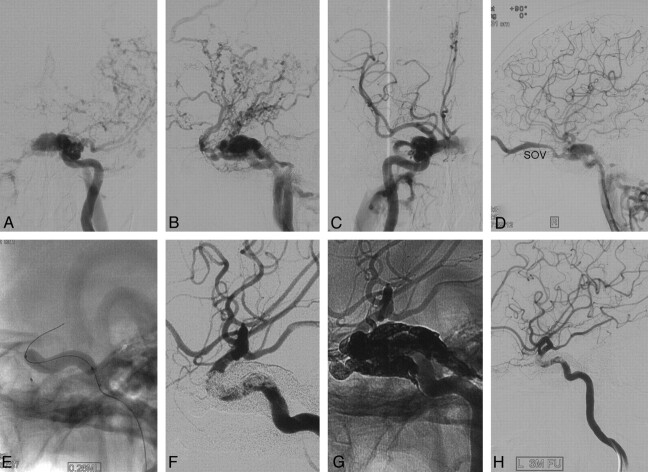
Fig 2.
A and B, Left ICA (L-ICA) injection demonstrates total arterial steal. The fistula mostly drains from vertex veins into the superior sagittal sinus. C and D, Right ICA injection shows the other fistula. The superior ophthalmic vein as a draining vein could be identified easily. E, The microcatheter navigates into the cavernous sinus superselectively, and the nondetchable balloon is inflated within the L-ICA before starting the Onyx injection. F, The immediate postembolization angiograms confirm complete occlusion with good preservation of the L-ICA and a great change of remote cerebral hemodynamics. G, The Onyx cast after injection. H, Three-month follow-up reveals stable complete occlusion of left TCCF.
There are some limitations to our study. Because of high blood rates of fistulas, even in total arterial steal, the damaged side of the cerebral hemisphere is in a state of relative hypoperfusion. Pre- and postoperative MR imaging should have been performed to identify asymptomatic cerebral infarction related to nondetachable balloons and flaking of solidified Onyx around the ostium, even though there is no significant relationship between balloon inflation practices and ischemic events, as reported by Spiotta et al,27 and no new ischemic events were observed in any of these 23 patients either. Besides, long-term follow-up and larger case series are needed for further evaluation of the safety and efficacy of Onyx for the transarterial balloon-assisted embolization for TOCFs.
Conclusions
In this series, the use of Onyx for the transarterial balloon-assisted embolization of TCCFs was feasible and effective. Associated adverse events were rare.
ABBREVIATIONS:
- CCF
carotid cavernous fistula
- CS
cavernous sinus
- DAVF
dural arteriovenous fistula
- DMSO
dimethyl-sulfoxide
- nBCA
n-butyl 2-cyanoacrylate
- TCCF
traumatic carotid cavernous fistula
Footnotes
Disclosures: The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this article.
References
- 1. Zenteno M, Santos-Franco J, Rodriguez-Parra V, et al. Management of direct carotid-cavernous sinus fistulas with the use of ethylene-vinyl alcohol (Onyx) only: preliminary results. J Neurosurg 2010;112:595–602 [DOI] [PubMed] [Google Scholar]
- 2. Elhammady MS, Wolfe SQ, Farhat H, et al. Onyx embolization of carotid-cavernous fistulas. J Neurosurg 2010;112:589–94 [DOI] [PubMed] [Google Scholar]
- 3. Barrow DL, Spector RH, Braun IF, et al. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg 1985;62:248–56 [DOI] [PubMed] [Google Scholar]
- 4. Suzuki S, Lee DW, Jahan R, et al. Transvenous treatment of spontaneous dural carotid-cavernous fistulas using a combination of detachable coils and Onyx. AJNR Am J Neuroradiol 2006;27:1346–69 [PMC free article] [PubMed] [Google Scholar]
- 5. Lv X, Li Y, Jiang C, et al. The incidence of trigeminocardiac reflex in endovascular treatment of dural arteriovenous fistula with Onyx. Interv Neuroradiol 2010;16:59–63. Epub 2010 Mar 25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Goto K, Hieshima GB, Higashida RT, et al. Treatment of direct carotid cavernous sinus fistulae: various therapeutic approaches and results in 148 cases. Acta Radiol Suppl 1986;369:576–79 [PubMed] [Google Scholar]
- 7. Teng MM, Chang CY, Chiang JH, et al. Double-balloon technique for embolization of carotid cavernous fistulas. AJNR Am J Neuroradiol 2000;21:1753–56 [PMC free article] [PubMed] [Google Scholar]
- 8. Higashida RT, Halbach VV, Tsai FY, et al. Interventional neurovascular treatment of traumatic carotid and vertebral artery lesions: results in 234 cases. AJNR Am J Neuroradiol 1989;153:577–82 [DOI] [PubMed] [Google Scholar]
- 9. Kobayashi N, Miyachi S, Negoro M, et al. Endovascular treatment strategy for direct carotid-cavernous fistulas resulting from rupture of intracavernous carotid aneurysms. AJNR Am J Neuroradiol 2003;24:1789–96 [PMC free article] [PubMed] [Google Scholar]
- 10. Lewis AI, Tomsick TA, Tew JM, Jr. Management of 100 consecutive direct carotid-cavernous fistulas: results of treatment with detachable balloons. Neurosurgery 1995;36:239–44 [DOI] [PubMed] [Google Scholar]
- 11. Gupta AK, Purkayastha S, Krishnamoorthy T, et al. Endovascular treatment of direct carotid cavernous fistulae: a pictorial review. Neuroradiology 2006;48:831–39 [DOI] [PubMed] [Google Scholar]
- 12. Melvin R, Kevin WD. Varicocele and female infertility. In: Curtis WB, James ES, Jacob C, et al., eds. Vascular and Interventional Radiology: Principles and Practice. New York: Thieme; 2002:327 [Google Scholar]
- 13. Gemmete JJ, Ansari SA, Gandhi DM.. Endovascular techniques for treatment of carotid-cavernous fistula. J Neuroophthalmol 2009;29:62–71 [DOI] [PubMed] [Google Scholar]
- 14. Wang ZG, Ding X, Zhang JQ, et al. HydroCoil occlusion for treatment of traumatic carotid-cavernous fistula: preliminary experience. Eur J Radiol 2009;71:456–60 [DOI] [PubMed] [Google Scholar]
- 15. Eddleman CS, Surdell D, Miller J, et al. Endovascular management of a ruptured cavernous carotid artery aneurysm associated with a carotid cavernous fistula with an intracranial self-expanding microstent and hydrogel-coated coil embolization: case report and review of the literature. Surg Neurol 2007;68:562–67, discussion 567 [DOI] [PubMed] [Google Scholar]
- 16. Tiewei Q, Ali A, Shaolei G, et al. Carotid cavernous fistulas treated by endovascular covered stent grafts with follow-up results. Br J Neurosurg 2010;24:435–40 [DOI] [PubMed] [Google Scholar]
- 17. Gomez F, Escobar W, Gomez AM, et al. Treatment of carotid cavernous fistulas using covered stents: midterm results in seven patients. AJNR Am J Neuroradiol 2007;28:1762–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Archondakis E, Pero G, Valvassori L, et al. Angiographic follow-up of traumatic carotid cavernous fistulas treated with endovascular stent graft placement. AJNR Am J Neuroradiol 2007;28:342–47 [PMC free article] [PubMed] [Google Scholar]
- 19. Pierot L, Januel AC, Herbreteau D, et al. Endovascular treatment of brain arteriovenous malformations using Onyx: results of a prospective, multicenter study. J Neuroradiol 2009;36:147–52 [DOI] [PubMed] [Google Scholar]
- 20. Saraf R, Shrivastava M, Kumar N, et al. Embolization of cranial dural arteriovenous fistulae with Onyx: indications, techniques, and outcomes. Indian J Radiol Imaging 2010;20:26–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Katsaridis V, Papagiannaki C, Aimar E.. Curative embolization of cerebral arteriovenous malformations (AVMs) with Onyx in 101 patients. Neuroradiology 2008;50:589–97 [DOI] [PubMed] [Google Scholar]
- 22. Cognard C, Januel AC, Silva NA, Jr, et al. Endovascular treatment of intracranial dural arteriovenous fistulas with cortical venous drainage: new management using Onyx. AJNR Am J Neuroradiol 2008;29:235–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gandhi D, Ansari SA, Cornblath WT.. Successful transarterial embolization of a Barrow type D dural carotid-cavernous fistula with ethylene vinyl alcohol copolymer (Onyx). J Neuroophthalmol 2009;29:9–12 [DOI] [PubMed] [Google Scholar]
- 24. Roy D, Raymond J.. The role of transvenous embolization in the treatment of intracranial dural arteriovenous fistulas. Neurosurgery 1997;40:1133–41 [DOI] [PubMed] [Google Scholar]
- 25. Wakhloo AK, Perlow A, Linfante I, et al. Transvenous n-butyl-cyanoacrylate infusion for complex dural carotid cavernous fistulas: technical considerations and clinical outcome. AJNR Am J Neuroradiol 2005;26:1888–97 [PMC free article] [PubMed] [Google Scholar]
- 26. Otrock ZK, Beydoun A, Barada WM, et al. Transient global amnesia associated with the infusion of DMSO-cryopreserved autologous peripheral blood stem cells. Haematologica 2008;93:36–37 [DOI] [PubMed] [Google Scholar]
- 27. Spiotta AM, Bhalla T, Hussain MS, et al. An analysis of inflation times during balloon-assisted aneurysm coil embolization and ischemic complications. Stroke 2011;42:1051–55 [DOI] [PubMed] [Google Scholar]