Abstract
BACKGROUND AND PURPOSE:
The Y-stent technique, including crossing-Y and kissing-Y, is a promising therapeutic option for some complex bifurcation aneurysms. Here, its efficacy and safety are evaluated on the basis of 11 bifurcation aneurysms.
MATERIALS AND METHODS:
A retrospective review was conducted for all patients who underwent endovascular treatment of aneurysms in our department between January 2009 and June 2011 to identify and analyze cases with bifurcation aneurysms reconstructed by using Y-stents.
RESULTS:
Eleven patients (4 ruptured and 7 unruptured aneurysms) were identified (4 men, 7 women) with a mean age of 60.4 years. Nine aneurysms (2 AcomAs, 3 MCA-Bifs, 1 PcomA, 3 BA apexes) were treated by using the crossing-Y technique, and 2 (both BA apexes) were treated with the kissing-Y technique, achieving complete occlusion in 6 aneurysms, residual neck in 4, and partial occlusion in 1. Perioperatively, a single thromboembolic event occurred in 1 case without neurologic deficit, which required a salvaging second stent implantation. Means of 9.9 months of angiographic and 13.7 months of clinical follow-up were available. As a result, 9 (81.8) aneurysms were completely occluded, 1 with a residual neck remained stable, and 1 residual aneurysm sac was recanalized, which was retreated and achieved a complete occlusion. All patients were independent with an mRS score of 0–1 at discharge and follow-up.
CONCLUSIONS:
In selected patients, the reconstruction of bifurcation aneurysms by using the Y-stent can be successfully achieved with satisfactory midterm results.
Advances in endovascular treatment strategies and stent characteristics have greatly improved the ability to treat wide-neck aneurysms.1–6 However, it remains a challenge to successfully treat some complex wide-neck bifurcation aneurysms by using a single-stent technique. Although kissing-balloon-assisted coiling has been attempted,7,8 this technique is almost impossible for treating extremely wide-neck bifurcation aneurysms such as those reported in this article. Moreover, multiple balloon inflations may increase the risk of complications, such as ischemic events, thromboembolism, and even vessel tears secondary to overinflation,9,10 though the increase of these adverse events remains controversial during single-balloon-assisted coiling.11 According to some series, in some complex bifurcation aneurysms, especially those in which the base of the aneurysm directly involves both bifurcation branches, a better option may be preserving both branches by using the Y-stent technique.2,3,12 However, its safety remains yet unknown. The purpose of this study was to evaluate the efficacy and safety of the Y-stent technique and to report our experiences based on 11 cases.
Materials and Methods
Patients
A retrospective chart review was conducted for all patients who underwent endovascular treatment of aneurysms in our department between January 2009 and June 2011 to identify cases with bifurcation aneurysms reconstructed by using the Y-stent technique (On-line Table). Eleven patients (4 men, 7 women) were identified with an age range of 42–78 years (mean age, 60.4 years). These patients had 11 bifurcation lesions that were successfully treated by using the Y-stent technique. Clinical characteristics are detailed in the On-line Table. In this series, all patients opted for coiling when the benefits and risks associated with surgical and endovascular treatment were explained in detail, and all patients were considered suitable candidates for Y-stent implantation based on individualized evaluations.
Aneurysms
Of the 11 aneurysms, 2 were located at the AcomA, 3 at the MCA-Bif, 1 at the origin of fetal PCA, and 5 at the BA apex. Ten were small (≦10 mm), and 1 was large (10 to ≦25 mm).13 All 11 aneurysms were wide-neck (neck >4 mm and/or dome/neck ratio < 2).
Y- Stent Technique
The Y-stent technique includes the crossing-Y and kissing-Y. Before the procedure, patients with acutely ruptured aneurysms were treated at 2 hours before stent placement with a rectal loading dose of clopidogrel and aspirin (300 mg, each), and patients with unruptured aneurysms were treated with dual antiplatelet drugs consisting of clopidogrel (75 mg) and aspirin (300 mg) each day for 3 days. All procedures were performed via a unilateral or bilateral transfemoral approach under general anesthesia with full anticoagulation therapy with intravenous heparin. The activated clotting time was maintained at 2–3 times the baseline throughout the procedure. For the crossing-Y stent technique, a 6F Envoy guiding catheter (Cordis, Miami Lakes, Florida) was first navigated into the distal ICA for the anterior circulation aneurysms or into the distal VA for basilar bifurcation aneurysms. Two 6F Envoy guiding catheters were navigated into the bilateral VA for the kissing-Y stent technique. The crossing-Y stent technique was based on the strategy that a second stent would be advanced over the wire through the first stent interstices and into the contralateral branch vessel. By contrast, 2 stents were deployed in a parallel fashion from both P1 segments down to the BA trunk, forming a kissing-Y configuration. Following the procedure, low-molecular-weight heparin (40 mg every 12 hours, hypodermic injection) was administered for 3 days, and patients were discharged home with a prescription for 6 weeks of clopidogrel (Plavix), 75 mg, and aspirin, 300 mg, daily, then 300 mg of aspirin for 6 months and 100 mg for lifetime maintenance.
Occlusion-Grade Analysis
According to Raymond et al,14 the postoperative angiographic occlusion grade was classified as “total occlusion (class I),” “neck remnant (class II),” and “aneurysm filling (class III).” The classifications were independently evaluated by 2 authors (P.-F.Y. and Q.-H.H. with 4–8 years of experience in neurointerventions).
Stents
Of the 11 aneurysms, 1 pair of stents was implanted by using 2 different stents, and 10 pairs of stents were embedded with 2 identical stents. Moreover, all 6 anterior circulation aneurysms were treated by using the crossing-Y stent technique (100%) with double open- or closed-cell stents (On-line Table): 2 AcomA aneurysms (Fig 1, case 2) and 1 PcomA (fetal PCA, Fig 2 , case 6) aneurysm with 2 Enterprise stents (Cordis), 1 MCA-Bif aneurysm with 2 Enterprise stents (Fig 3 , case 3), and 2 MCA-Bif aneurysms with 2 Neuroform stents (Boston Scientific, Natick, Massachusetts). In addition, 3 of the 5 posterior circulation aneurysms were reconstructed by the crossing-Y stent technique, and the 2 BA apex aneurysms were reconstructed by using the kissing-Y stent technique with at least 1 Enterprise closed-cell stent (On-line Table): 4 BA-Bif aneurysms with 2 Enterprise stents and 1 BA-Bif aneurysm with 2 different stents. Of the 11 treated lesions, the percentages of the first implanted stents were as follows: Enterprise, 77.3% (8/11); Neuroform, 22.7% (3/11).
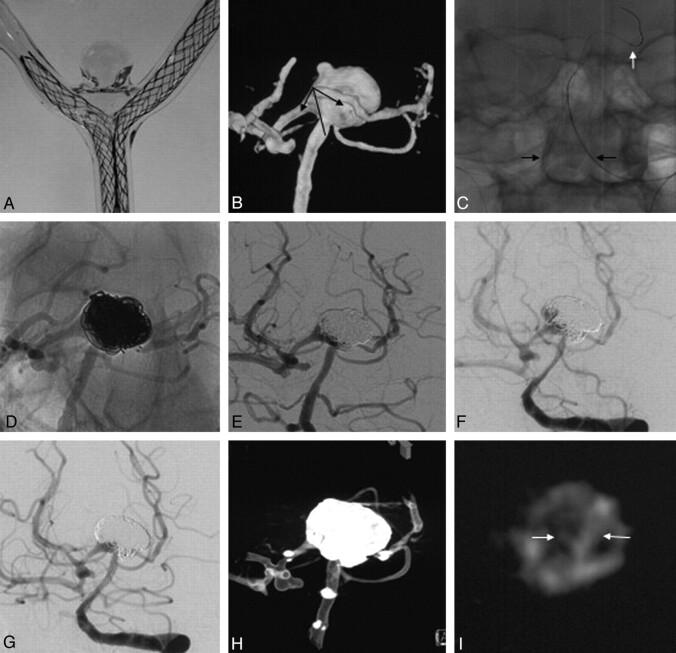
Fig 1.
A crossing-Y stent for an AcomA aneurysm with Enterprise stents. Experimental model (A), single stent-assisted coiling for an AcomA aneurysm (B and C), and local thrombus formation (C). D, Markers of salvaging Y-stent and coils. E and F, Comparison of the postprocedural and 6-month follow-up angiograms.
Fig 2.
Crossing-Y stents for the ICA-PcomA aneurysm originating from the origin of the fetal PCA. A, ICA-PcomA aneurysm arising from the origin of the fetal PCA. B and C, The first Enterprise stent has been deployed (black arrow), followed by a second Enterprise stent. D, Postprocedural reconstruction image. E and F, Comparison of postprocedural and 8-month follow-up angiograms.
Fig 3.
A crossing-Y stent for a MCA-Bif aneurysm. A, Wide-neck MCA-Bif aneurysm. B, Stent and coil microcatheters in position. C, The first Enterprise stent was deployed, followed by a second (salvaging) Enterprise stent, due to the protrusion of the coil loop. D and E, Postprocedural angiograms show the patency of parent arteries and a residual neck. F, Coils and markers of 2 stents.
Clinical and Angiographic Follow-Up
Clinical and angiographic follow-up were performed between 6 and 12 months, and annually thereafter. The angiographic results were interpreted independently by 2 authors (P.-F.Y. and Q.-H.H.) by using the classification of Raymond et al.14
Results
Immediate Embolization Results
Twenty-two stents were successfully implanted into target vessels with a technical success rate of 100%, and control angiography confirmed total occlusion in 6 cases (54.5%), residual neck in 4 (36.4%), and residual aneurysm in 1 (9.1%).
Technical Difficulty
In cases 3 and 4, we encountered difficulty while delivering the second Neuroform stent through the interstices of the first Neuroform stent for 2 MCA-Bif aneurysms treated with the crossing-stent technique. Two BA-Bif aneurysms had unfavorable distal limb configurations, such as a “T” (case 11) or “arrow” (Fig 4 , case 10) configuration, resulting in difficulty in the catheterization.
Fig 4.
The kissing-Y stent for a BA apex aneurysm. A, Experimental model. B, The arrow-configuration bifurcation. C−E, Double microcatheters in position (C) and the kissing-Y stent-assisted coiling (D), obtaining a residual sac (E). Twenty-four month angiograms demonstrate coil compaction (F) and a second coiling, achieving a complete occlusion (G). H and I, DynaCT shows coils, markers, and lumens of 2 stents (white arrows).
Angiographic Follow-Up
Postoperative follow-up angiograms were obtained in all 11 coiled aneurysms at a mean of 9.9 months. Of the 6 aneurysms with initial total occlusion, none developed recurrence and compromise of parent vessels; of the 4 aneurysms (cases 3–5 and 11) with residual necks, follow-up angiograms demonstrated total occlusion in 3 cases and stability in 1 (case 11). However, at 24 months after initial coiling, a BA apex aneurysm with initial residual aneurysm filling was retreated once for an evident coil compaction and achieved complete occlusion (Fig 4, case 10).
Clinical Outcome
Overall, 11 patients were independent, with an mRS score of 0–1 at discharge and follow-up (mean, 13.7 months), and none showed any neurologic deterioration.
Complications
Thrombus formation resulting from a coil loop protrusion was encountered and solved by using the salvaging Y-stent technique and 1 hour of tirofiban hydrochloride infusion in case 2 (Fig 1). Technical complications of the Y-stent technique itself were not encountered. There was no procedure-related morbidity or mortality in this series.
Discussion
The advent of self-expanding neurovascular stents and continued advances in endovascular techniques, such as balloon remodeling,15–17 single stent reconstruction,4,18 and transcirculation techniques8 have greatly improved the ability to treat intracranial aneurysms. However, achieving an uncomplicated and complete obliteration of complex bifurcation aneurysms remains technically challenging. Currently, the Y-stent technique, including the crossing-Y2,6,12 and kissing-Y,3 is increasingly emerging as a promising therapeutic option for some complex bifurcation aneurysms. However, its efficacy and safety remain unclear. In this retrospective study, we evaluated the efficacy and safety of the Y-stent technique and introduced our preliminary experiences based on 11 patients with bifurcation aneurysms previously treated by using the Y-stent technique.
Planned and Unplanned Y-Stent Placement
In general, when wide-neck bifurcation aneurysms simultaneously involve 2 branch vessels, the planned-Y stent strategy will be selected. Furthermore, the relatively good posterior circulation access facilitates the success of the Y-stent technique. Therefore, planned Y-stent strategies were performed for most posterior circulation aneurysms in this series. When bifurcation aneurysms mainly involve 1 of the branch vessels, a single stent-assisted coiling is first attempted. However, herniation of coil loops, even local thrombus formation (case 2, Fig 1) may affect the other branch vessel, which requires a salvaging Y-stent placement. In this series, most anterior circulation bifurcation aneurysms were treated with the unplanned Y-stent strategy. This was because we preferred to try single stent-assisted coiling for these aneurysms, considering the tortuous vessel access. Generally, a single stent provided us the protection of 2 branches of wide-neck bifurcation aneurysms. Occasionally, the protrusion of a coil loop or coil mass19 might affect the other branch blood flow, resulting in the salvaging Y-stent implantation.
Crossing and Kissing Y-Configuration Stent Placement
Generally, the crossing-Y stent placement, which means deploying a second stent through the interstices of the first stent, is the traditional and most commonly used Y-stent technique. However, the crossing Y-stent technique is technically challenging, sometimes impossible for some large complex bifurcation aneurysms with unfavorable anatomic configurations, including sharp angles and an extremely wide neck. According to the angle between the distal limbs and parent trunk vessel, the most common intracranial bifurcation vessels are composed of 3 types of anatomic configurations, approximately the following: 1) T-configuration(Figs 5 and 6C), with an angle between the limbs and the trunk vessel approximately 90°; 2) Y-configuration(Fig 6A, -B), with an angle between the limbs and the trunk vessel >90°; 3) arrow(↑)-configuration(Fig 6D), with an angle between the limbs and the trunk vessel <90°. Of these anatomic configurations, the Y-configuration is technically favorable for catheterization. The T-configuration can be catheterized but with relative difficulties, and the arrow(↑)-configuration is technically the most challenging. For the arrow-configuration vessels in case 10 (Fig 4B), the catheterization of the distal branches was technically difficult. Once catheterization is successful for 1 branch, catheterizing the other branch across the interstices of the first stent is more troublesome. Moreover, the delivery and deployment of stents across the sharp angles formed by parent vessels are also very troublesome.
Fig 5.
A crossing-Y stent for a BA apex aneurysm. A, T-configuration. B and C, After coil basketing, the first Enterprise stent was deployed, followed by the deployment of a second Enterprise stent through the interstices of the first Enterprise stent. D and E, Continuous coiling until a satisfactory embolization for the angle between stents is achieved. E and F, Comparison of postprocedural and 6-month follow-up angiograms.
Fig 6.
Sketch of the geometries of bifurcation anatomy and 2 necks. A, D1D2 and E1E2 represent 2 necks (E1E2 > D1D2). B−D, Y-configuration, T-configuration, and arrow-configuration with approximately 2 equal aneurysm necks.
Bifurcation aneurysms have 2 necks (Fig 6) on each branch, and width is also crucial for the selection of the crossing or kissing Y-stent technique. For the crossing-Y stent technique, we usually first catheterize the branch with a relatively narrow aneurysm neck and deploy the first stent, which means that the first stent is relatively stable with a lower risk of herniation into the aneurysm sac, while catheterizing the contralateral branch through its interstices. However, some large bifurcation aneurysms, such as in case 10 (Fig 4), have 2 extremely wide necks on each branch. No matter which branch vessel was first implanted with a stent, the risk of stent protrusion into aneurysm sac was unavoidable when performing the crossing-Y technique. Consequently, in these 2 situations, and especially for cases with both sharp angles and extremely wide necks, the kissing-Y stent implantation, with 2 stents placed parallel to both distal branches down to the parent artery trunk, is preferred. Moreover, stent deployment after partial coiling is advocated for the kissing-Y stent implantation, which may provide sufficient support for the stent and increase its stability, and is favored by our experience.
In 2004, the kissing-stent technique was attempted for a BA apex aneurysm, resulting in permanent implantation of the microguidewires,3 which was not a successful kissing-stent technique. In our current series, we reported 2 cases of BA apex aneurysms reconstructed by using the kissing-Y stent technique, which are actually the first successful cases ever reported (Fig 4), to our knowledge. However, there were 2 issues of concern for us after the kissing-Y stent implantation. The first was whether these 2 stents could open well within the BA trunk. A DynaCT (Siemens, Erlangen, Germany) image showed us an excellent patency of the 2 stents (Fig 4I). The second was whether the kissing-Y stent implantation was accompanied by an increased risk of thromboembolic events due to the disturbance of regional blood flow. Although we found that the kissing-Y stent technique was safe on the basis of 2 cases of satisfactory follow-up results (1 case with a 24-months follow-up [case 10]), this technique still needs further investigation to determine its effectiveness.
Stent Selection
Since the initial report of the Y-configuration stent implantation, the recommended stent, especially the first stent, has been the Neuroform thanks to its open-cell design, which may facilitate the navigation of the second stent. However, we encountered significant difficulty in the first 2 cases (cases 3 and 4) while delivering the second stent through the interstices of the first Neuroform stent, as we previously reported.19 During the same period, we had performed 4 unplanned Y-stent techniques without any difficulty, for which the first and second choices were both Enterprise stents (cases 2 and 5–7). These experiences indicate that the use of the Enterprise stent may ease the catheterization, delivery, and deployment of the Y-configuration stent implantation. Although with the second stent there was a possibility of narrowing, especially in vessels with a small diameter, postprocedural angiograms and clinical follow-ups demonstrated the patency of 2 branch vessels and uneventful outcomes. Also, in a published study, there has been confirmation that the implantation of the Enterprise stent can potentially reduce intra-aneurysmal hemodynamic activities with the increasing likelihood of inducing aneurysm thrombotic occlusion.20 For these reasons, the Enterprise stent is preferred for the Y-stent technique in our institution. In this series, a total of 7 bifurcation aneurysms were successfully reconstructed by using the crossing-Y stent technique with double Enterprise stents, with excellent angiographic and clinical follow-up results. In addition, the Enterprise is particularly advocated for the kissing-Y stent technique because these aneurysms have unfavorable anatomic configurations. For the catheterization, delivery, and deployment of stents, these unfavorable anatomic configurations demand high stent navigability and conformability. Hence, it is reasonable for Enterprise to be selected for the kissing-Y stent technique, as demonstrated by cases 10 and 11.
Efficacy and Safety of the Y-Stent Technique
On angiograms at a mean of 9.9 months, 9 (81.8%) aneurysms were completely occluded; 1 with a residual neck remained stable, and 1 was recanalized and subsequently retreated, achieving a complete occlusion. These excellent results demonstrated the efficacy and durability of the Y-stent technique for intracranial bifurcation aneurysms, which coincided with the findings in recently published literature.21,22 In this series, the success rate of the techniques associated with the crossing-Y or kissing-Y stent was 100%. Although a thrombus event (1/11) resulting from a coil loop protrusion was encountered in case 2 (Fig 1), a salvaging Y-stent was used, achieving the patency of double branches.
Limitations
In this series, there are some limitations, such as the retrospective design, patient selection bias, limited cases in a single institution, and short follow-up time.
Conclusions
In selected patients, Y-configuration stent placement (crossing and kissing) for endovascular reconstruction of wide-neck cerebral aneurysms located at 4 different bifurcation sites can be successfully achieved with satisfactory midterm results.
Supplementary Material
ABBREVIATIONS:
- AcomA
anterior communicating artery
- BA
basilar artery
- Bif
bifurcation
- mRS
modified Rankin Scale
- PCA
posterior cerebral artery
- PcomA
posterior communicating artery
- VA
vertebral artery
Footnotes
This work was supported by National Natural Science Foundation of China (grant No. 81000494–81171902), Shanghai Science and Technology Committee (grant No. 11QA1408400), and the Shanghai Municipal Education Commission (grant No. 11CG43).
References
- 1. Kim JW, Park YS.. Endovascular treatment of wide-necked intracranial aneurysms: techniques and outcomes in 15 patients. J Korean Neurosurg Soc 2011;49:97–101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lozen A, Manjila S, Rhiew R, et al. Y-stent-assisted coil embolization for the management of unruptured cerebral aneurysms: report of six cases. Acta Neurochir (Wien) 2009;151:1663–72 [DOI] [PubMed] [Google Scholar]
- 3. Henkes H, Kirsch M, Mariushi W, et al. Coil treatment of a fusiform upper basilar trunk aneurysm with a combination of “kissing” Neuroform stents, TriSpan-, 3D- and fibered coils, and permanent implantation of the microguidewires. Neuroradiology 2004;46:464–68 [DOI] [PubMed] [Google Scholar]
- 4. Kelly ME, Turner R, Gonugunta V, et al. Stent reconstruction of wide-necked aneurysms across the circle of Willis. Neurosurgery 2007;61:249–54, discussion 54–55 [DOI] [PubMed] [Google Scholar]
- 5. Pierot L, Cognard C, Spelle L, et al. Safety and efficacy of balloon remodeling technique during endovascular treatment of intracranial aneurysms: critical review of the literature. AJNR Am J Neuroradiol 2012;33:12–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Klisch J, Eger C, Sychra V, et al. Stent-assisted coil embolization of posterior circulation aneurysms using Solitaire AB: preliminary experience. Neurosurgery 2009;65:258–66, discussion 66 [DOI] [PubMed] [Google Scholar]
- 7. Mewissen MW, Beres RA, Bessette JC, et al. Kissing-balloon technique for angioplasty of the popliteal artery trifurcation. AJR Am J Roentgenol 1991;156:823–24 [DOI] [PubMed] [Google Scholar]
- 8. Albuquerque FC, Gonzalez LF, Hu YC, et al. Transcirculation endovascular treatment of complex cerebral aneurysms: technical considerations and preliminary results. Neurosurgery 2011;68:820–29, discussion 29–30 [DOI] [PubMed] [Google Scholar]
- 9. Sluzewski M, van Rooij WJ, Beute GN, et al. Balloon-assisted coil embolization of intracranial aneurysms: incidence, complications, and angiography results. J Neurosurg 2006;105:396–99 [DOI] [PubMed] [Google Scholar]
- 10. Soeda A, Sakai N, Sakai H, et al. Thromboembolic events associated with Guglielmi detachable coil embolization of asymptomatic cerebral aneurysms: evaluation of 66 consecutive cases with use of diffusion-weighted MR imaging. AJNR Am J Neuroradiol 2003;24:127–32 [PMC free article] [PubMed] [Google Scholar]
- 11. Layton KF, Cloft HJ, Gray LA, et al. Balloon-assisted coiling of intracranial aneurysms: evaluation of local thrombus formation and symptomatic thromboembolic complications. AJNR Am J Neuroradiol 2007;28:1172–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Perez-Arjona E, Fessler RD.. Basilar artery to bilateral posterior cerebral artery ‘Y stenting' for endovascular reconstruction of wide-necked basilar apex aneurysms: report of three cases. Neurol Res 2004;26:276–81 [DOI] [PubMed] [Google Scholar]
- 13. Plowman RS, Clarke A, Clarke M, et al. Sixteen-year single-surgeon experience with coil embolization for ruptured intracranial aneurysms: recurrence rates and incidence of late rebleeding: clinical article. J Neurosurg 2011;114:863–74 [DOI] [PubMed] [Google Scholar]
- 14. Raymond J, Guilbert F, Weill A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke 2003;34:1398–403 [DOI] [PubMed] [Google Scholar]
- 15. Baldi S, Mounayer C, Piotin M, et al. Balloon-assisted coil placement in wide-neck bifurcation aneurysms by use of a new, compliant balloon microcatheter. AJNR Am J Neuroradiol 2003;24:1222–25 [PMC free article] [PubMed] [Google Scholar]
- 16. Spiotta AM, Bhalla T, Hussain MS, et al. An analysis of inflation times during balloon-assisted aneurysm coil embolization and ischemic complications. Stroke 2011;42:1051–55 [DOI] [PubMed] [Google Scholar]
- 17. Wolfe SQ, Farhat H, Moftakhar R, et al. Intraaneurysmal balloon assistance for navigation across a wide-necked aneurysm. J Neurosurg 2010;112:1222–22 [DOI] [PubMed] [Google Scholar]
- 18. Cross DT, 3rd, Moran CJ, Derdeyn CP, et al. Neuroform stent deployment for treatment of a basilar tip aneurysm via a posterior communicating artery route. AJNR Am J Neuroradiol 2005;26:2578–81 [PMC free article] [PubMed] [Google Scholar]
- 19. Yang P, Liu J, Huang Q, et al. Endovascular treatment of wide-neck middle cerebral artery aneurysms with stents: a review of 16 cases. AJNR Am J Neuroradiol 2010;31:940–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tremmel M, Xiang J, Natarajan SK, et al. Alteration of intra-aneurysmal hemodynamics for flow diversion using Enterprise and Vision stents. World Neurosurg 2010;74:306–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Spiotta AM, Gupta R, Fiorella D, et al. Mid-term results of endovascular coiling of wide-necked aneurysms using double stents in Y configuration. Neurosurgery 2011;69:421–29 [DOI] [PubMed] [Google Scholar]
- 22. Akgul E, Aksungur E, Balli T, et al. Y-stent-assisted coil embolization of wide-neck intracranial aneurysms: a single-center experience. Interv Neuroradiol 2011;17:36–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.