SUMMARY:
The aim is to describe the technique of preoperative CT-guided hookwire localization of small, but suspicious, cervical lymph nodes. We present 3 patients who underwent the procedure for nonpalpable cervical nodes detected on PET/CT prior to complete surgical resection of the nodes. The details of the radiological procedure, surgical outcomes, and pathologic results are described. The mean intervention time for preoperative hookwire localization was 9 minutes (range 7–14 minutes). There were no complications. All surgeons felt that the lengths of the surgical skin incision and operative times were reduced because of localization. The pathologic diagnoses were 2 benign nodes and 1 case of metastatic ovarian carcinoma. In conclusion, preoperative CT-guided hookwire localization is a useful technique for guiding surgical excision, especially when cervical nodes are small and deep in location.
FDG-PET is a helpful imaging technique that can detect metastases to the lymph nodes that are otherwise negative clinically and radiographically. When such lymph nodes are deep or small, they may be difficult to locate during surgery and there is a risk that the incorrect node may be excised.
Impalpable lesions in the breast can be preoperatively localized with a hookwire by using mammographic or sonographic guidance.1,2 For the neck, hookwire localization of small but suspicious cervical lymph nodes could enable the head and neck surgeon to resect the correct node while keeping the procedure minimally invasive. The aim of this report is to describe the technique and outcome in 3 patients who underwent preoperative CT-guided hookwire localization for small FDG-avid cervical nodes.
Technique
Subjects
Patient A was a 58-year-old woman with a T2a adenoid cystic carcinoma of the left nasopharynx. A pretreatment staging neck PET/CT study found a 9-mm left level IIb lymph node with a SUVmax of 3.4 g/mL.
Patient B was a 62-year-old woman with a history of large B-cell lymphoma of the cecum who was imaged 13 months after chemotherapy. A whole-body PET/CT study found a new 9-mm left level V cervical lymph node with an SUVmax of 9.2 g/mL. Initially a CT-guided core-needle biopsy of this lesion was performed, but the pathologic result was nondiagnostic.
Patient C was a 65-year-old woman with stage IIIc high-grade serous ovarian carcinoma who was imaged 18 months after surgical resection and chemotherapy. A whole-body PET/CT study found a new 8-mm left level VI lymph node with an SUVmax of 5.4 g/mL.
Hookwire Localization Technique
Before the procedure, the surgeon and radiologist reviewed the PET/CT images to identify the lesion and discuss the best approach for CT-guided localization. The localization procedure was then scheduled for the morning of the surgery.
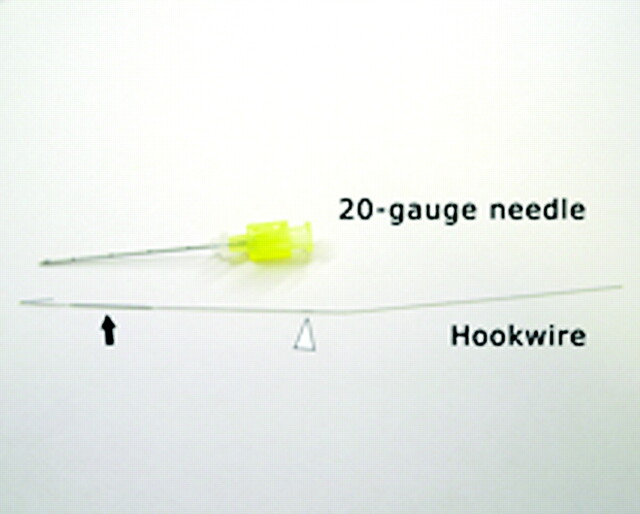
All procedures required a 20-gauge Kopans spring hook localization needle (Cook, Bloomington, Indiana), which consisted of an introducer needle and a hookwire (Fig 1).3 This needle kit is available from the breast imaging division of most radiology departments.
Fig 1.
Photograph of the Kopans spring hook localization needle kit that consists of an introducer needle and a hookwire. The distal 1 cm of the hookwire is hooked so that it can be advanced in the lumen of the introducer needle and then spring open when the needle is removed. A black marker on the wire (arrowhead) should be level with the needle hub when the tip of the wire is at the tip of the needle. There is also a thicker component on the wire (arrow), which is visible and palpable by the surgeon so that they can anticipate the depth to the tip.
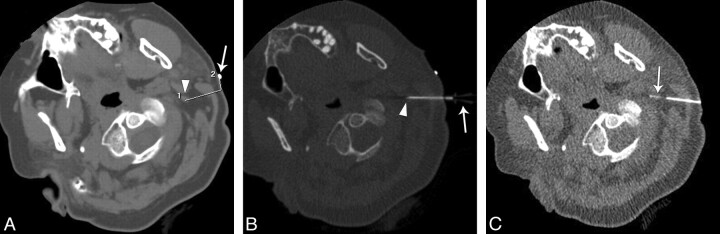
After consent, patients were positioned on the CT scanner and a radiopaque skin marker was placed on the neck on the side of the lesion. First, a planning unenhanced CT scan was obtained to cover the neck just above and below the lesion. From the CT images, the level of the lesion was identified and the needle approach was planned (Fig 2A). Planning included the following: 1) determining the pathway that avoided the vascular structures being in the needle path or being immediately deep to the hookwire in case of deep migration of the wire, and 2) marking the skin entry site from the radiopaque marker. The distance from skin to the lesion was measured to select the appropriate length of the introducer needle (available in 5-, 7-, and 9-cm lengths).
Fig 2.
A 58-year-old woman with a history of left nasopharyngectomy for a T2a adenoid cystic carcinoma of the left nasopharynx. A, An image from the planning unenhanced CT with calipers shows the small left level IIb node (arrowhead), the pathway of the needle for localization (line 1), and distance (line 2) from the radiopaque marker (arrow) to the skin entry site. B, An axial CT fluoroscopy image shows the introducer needle positioned with the node (arrowhead). Note that the hub of the needle (arrow) can also be appreciated. C, An axial fluoroscopic image shows the hookwire within the node (arrow) after the needle is removed.
The skin was prepared and draped by using a sterile technique; local anesthesia was achieved with 1% lidocaine. Using intermittent CT fluoroscopy, we advanced the introducer needle through the skin and directed it to the lymph node (Fig 2B). Once the needle tip was positioned within the node, the wire was placed through the needle until a black marker on the wire was level with the hub of the needle (Fig 1): This indicates that the tip of wire is at the tip of the needle. The hookwire was then held in place, and the introducer needle was carefully withdrawn over the wire. The hook of the wire springs open to anchor the wire in the node after the needle is withdrawn by more than 1 cm (Fig 1). The position of the hookwire within the node was confirmed with CT fluoroscopy or a limited CT scan (Fig 2C).
Finally, the protruding end of the wire was bent and taped to the skin to prevent displacement. Patients were also advised to avoid movement of the neck in extreme ranges of rotation, flexion, and extension. Within 1–3 hours after hookwire localization, patients underwent surgical resection of the lymph node (Fig 3).
Fig 3.
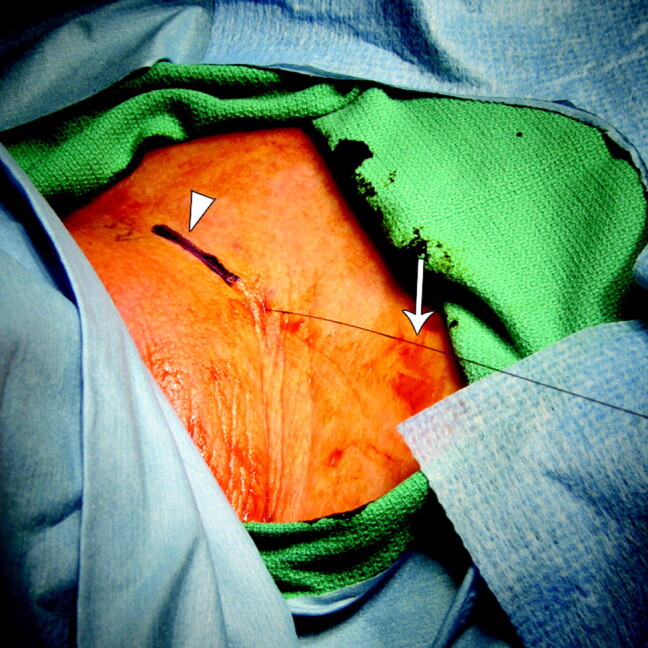
Intraoperative photograph of the hookwire (arrow) protruding from the skin and the planned surgical incision site, which has been marked (arrowhead) for resection of a left level VI lymph node in a 65-year-old woman with stage IIIc high-grade serous ovarian carcinoma. The right side of the image is the head, and the left side is the chest.
Results
Hookwire localization was successfully performed in all patients by the same radiologist (J.K.H). The mean intervention time for localization was 9 minutes (range, 7–14 minutes). The mean procedure time in the CT scanning room was 24 minutes (range, 17–29 minutes). The mean fluoroscopic radiation exposure time was 7.1 seconds (range, 4–12.5 seconds). None of the hookwires dislodged from the neck before surgery.
Three different surgeons performed complete lymph node resections. All surgeons found that the localization accurately identified the lymph node. All surgeons thought that localization helped to reduce the lengths of the surgical skin incision and operative times. The mean operative time was 75 minutes (range, 60–98 minutes). All patients were discharged from the hospital on the same day of surgery.
The pathologic diagnoses were as follows: Patient A had a benign lymph node with no evidence of malignancy, patient B had follicular hyperplasia without features suggestive of lymphoma, and patient C had metastatic carcinoma that was morphologically consistent with an ovarian primary tumor.
Discussion
Mammographic and sonographic guided-hookwire localization for impalpable breast lesions is a well-established technique that facilitates surgical excision.1,2 We describe a similar technique of localization of cervical lymph nodes under CT guidance to aid the surgeon during surgical resection.
All suspicious cervical nodes in our series were identified on PET/CT. Although FDG-PET is an important imaging technique that can detect small occult metastases, it also raises the problem of indeterminate nodes that could represent false-positive inflammatory nodes, as seen in patients A and B.4 FNA of indeterminate nodes could be performed instead of a surgical excision, but the latter was preferred for our patients because complete resection was desired and FNA can have false-negative and nondiagnostic rates in the head and neck of up to 15% and 30%, respectively.5 Other possible indications for use of hookwire localization in the neck include resection of residual or recurrent disease in the treated neck, where there may be extensive scar, or for resection of deep nodes, such as the retropharyngeal nodes.
In our patients, image guidance with CT was chosen because the nodes were originally identified on PET/CT. An alternative method of hookwire placement is by sonographic guidance, which has the benefits of real-time imaging and no ionizing radiation exposure. However, differences in imaging planes and appearances between CT and sonography could potentially result in incorrect node localization when using the latter technique.
We have shown that preoperative hookwire localization of neck masses before their surgical resection is a minimally invasive and quick procedure that can potentially result in shorter operative times and reduced postoperative morbidity. This technique is valuable when resection of small deep nodes is required because the skin incision would otherwise be larger to explore the neck for an impalpable node. The technique can also minimize chances that an adjacent small node is incorrectly resected. Similar advantages have been discussed in other reports of CT-guided localization of musculoskeletal, pulmonary, and abdominal lesions.6–9
In conclusion, preoperative CT-guided hookwire localization of cervical lymph nodes is a safe and effective technical innovation. It is particularly useful in the setting of surgical resection of small and deep lesions. We expect this technique to have an ongoing role because patients with tumor are increasingly imaged with PET/CT.
ABBREVIATIONS:
- FDG
fluorodeoxyglucose
- FNA
fine-needle aspiration
- PET
positron-emission tomography
- SUVmax
maximum standard uptake value
Footnotes
Disclosures: Jenny Hoang, Research Support (including provision of equipment or materials): GE Healthcare. Details: Recipient of the General Electric-Radiology Research Academic Fellowship (GERRAF) grant 2010–2012.
References
- 1. Abrahamson PE, Dunlap LA, Amamoo MA, et al. Factors predicting successful needle-localized breast biopsy. Acad Radiol 2003;10:601–06 [DOI] [PubMed] [Google Scholar]
- 2. Sailors DM, Crabtree JD, Land RL, et al. Needle localization for nonpalpable breast lesions. Am Surg 1994;60:186–89 [PubMed] [Google Scholar]
- 3. Kopans DB, DeLuca S. A modified needle-hookwire technique to simplify preoperative localization of occult breast lesions. Radiology 1980;134: 781 [DOI] [PubMed] [Google Scholar]
- 4. Wong RJ. Current status of FDG-PET for head and neck cancer. J Surg Oncol 2008;97:649–52 [DOI] [PubMed] [Google Scholar]
- 5. Tandon S, Shahab R, Benton JI, et al. Fine-needle aspiration cytology in a regional head and neck cancer center: comparison with a systematic review and meta-analysis. Head Neck 2008;30:1246–52 [DOI] [PubMed] [Google Scholar]
- 6. Finch IJ. Preoperative CT-guided percutaneous localization of small masses with a Kopans needle. AJR Am J Roentgenol 1991;157:179–80 [DOI] [PubMed] [Google Scholar]
- 7. Morrison WB, Sanders TG, Parsons TW, et al. Preoperative CT-guided hookwire needle localization of musculoskeletal lesions. AJR Am J Roentgenol 2001;176:1531–33 [DOI] [PubMed] [Google Scholar]
- 8. Chen YR, Yeow KM, Lee JY, et al. CT-guided hook wire localization of subpleural lung lesions for video-assisted thoracoscopic surgery (VATS). J Formos Med Assoc 2007;106:911–18 [DOI] [PubMed] [Google Scholar]
- 9. Kagalwala DZ, Shankar S, Zota V, et al. Preoperative computed tomography-guided hookwire needle localization of a peritoneal multilocular inclusion cyst. J Comput Assist Tomogr 2005;29:602–03 [DOI] [PubMed] [Google Scholar]