Abstract
BACKGROUND AND PURPOSE:
It remains unclear whether SSCD syndrome, characterized by onset of vestibular symptoms in the setting of loud noises, is a congenital or acquired condition. The purpose of this investigation was to assess the prevalence of SSCD on imaging among multiple age groups to determine whether this condition is more likely to be congenital or acquired.
MATERIALS AND METHODS:
Following approval of the institutional review board, 306 consecutive temporal bone CT examinations performed between July 2005 and March 2007 were retrospectively reviewed. Of these, 2 patients were eliminated due to destructive processes in the inner ear. Patients ranged in age from 7 months to 89 years. Images were independently evaluated by 2 neuroradiologists, and the superior semicircular canal was characterized as normal, thin, or frankly dehiscent in each temporal bone. Any discrepancies were resolved by consensus. The patient list was then subcategorized into 5 age groups, and the prevalence of SSCD was calculated for each group.
RESULTS:
Twenty-four patients were identified with SSCD, of which 6 demonstrated dehiscence bilaterally. One hundred thirty-seven subjects were identified with thinning, of which 50 demonstrated thinning bilaterally. Each successively older age category experienced a 93% increase (95% CI, 30%–187%) in the prevalence of SSCD (P = .001) and a 9% increase (95% CI, −5%–25%) in the prevalence of thinning (P = .21). Neither crude nor age-adjusted models demonstrated a significant association between thinning and contralateral dehiscence or vice versa.
CONCLUSIONS:
The increased radiologic prevalence of SSCD among older age groups suggests that this is more commonly an acquired rather than congenital condition.
SSCD syndrome was initially described by Minor et al1 and is classically characterized by vertiginous symptoms, oscillopsia, and rotatory and vertical nystagmus occurring in the setting of loud noises (Tullio phenomenon). The symptoms are thought to result from a bony defect in the roof of the superior semicircular canal, creating a “third window” effect with disruption of endolymphatic homeostasis particularly with loud auditory stimulations. While the classic presentation can be suspected on clinical and audiometric data, imaging plays an important role in the evaluation of these patients. Advances in CT now allow submillimeter high-resolution images to demonstrate the bony defect, while multiplanar reformations can also aid in the radiologic diagnosis.
Despite the increasing volume of literature on this condition, it remains unclear whether the bony defect is congenital or acquired. Certainly, a congenital/developmental basis for the condition has been described.2–6 To our knowledge, however, there are no large-scale investigations specifically addressing age and the prevalence of SSCD on imaging. The purpose of this study was, therefore, to investigate the prevalence of SSCD on imaging among different age groups and to assess whether there may be an acquired component to the condition.
Materials and Methods
Following approval of the institutional review board, consecutive temporal bone CT studies performed between July 2005 and March 2007 were retrospectively reviewed. All examinations were referred by the otolaryngology service at our institution. Temporal bone studies ordered through the emergency department were not included because these were typically performed in conjunction with head CT, and data are acquired from an axial rather than the typical helical technique used for dedicated temporal bone CT imaging at our institution. The examinations were performed for a variety of clinical indications, including conductive, sensorineural, and mixed hearing loss; tinnitus; and vestibular symptoms. All studies were performed on a 64−detector row CT scanner by using 0.625-mm section thickness and 0.3-mm interval reconstructions. All studies were helically acquired without contrast and were reconstructed by using a bone plus algorithm. Coronal and sagittal (1 pixel thickness) interactive reconstructions were performed at the workstation at the time of retrospective analysis (Centricity AW Suite, Version 5.5.3; GE Healthcare, Milwaukee, Wisconsin). In equivocal cases, additional oblique reconstructions, including Poschl and Stenver planes, were evaluated.
All CT examinations were independently reviewed by 2 fellowship-trained neuroradiologists, and the right and left superior semicircular canal was characterized as “normal,” “thin,” or frankly “dehiscent” in each case. The radiologists were blinded to the clinical history and formal radiologic impression at the time of review. Results were recorded in table format, and any discrepancies were resolved by consensus. The age of each patient was also recorded.
Data were analyzed by using the SAS statistical system, Version 9.1 (SAS Institute, Cary, North Carolina). All hypothesis tests were 2-sided by using an .05 significance level. Age was categorized into 5 groups: 0–20 years, 21–40 years, 41–60 years, 61–80 years, and 81–100 years. The radiologic prevalence of SSCD and thinning was calculated for each age group. Log-linear regression models were used to estimate a trend in prevalence ratios by age category. Logistic regression models were used to evaluate the association of thinning with contralateral dehiscence and vice versa. These models were fit with generalized estimating equations to account for multiple observations per subject.
Results
Three hundred six patients (612 temporal bones) were initially identified as meeting eligibility criteria. Of these, 2 patients were excluded due to unilateral destructive skull base masses involving the inner ear. Thus, the final sample was 304 patients (608 temporal bones). Patients ranged in age from 7 months to 89 years. The patient population consisted of 163 females and 141 males. There was little interobserver variability with high (>90%) concordance of classifications.
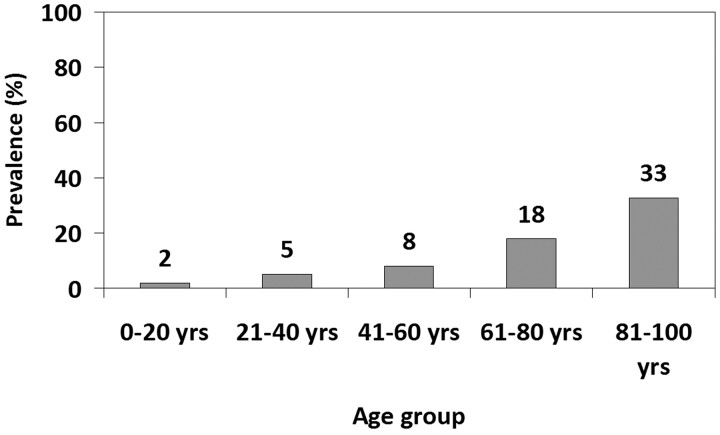
Of the 304 patients evaluated for dehiscence and thinning, 24 patients were identified with SSCD, of which 6 demonstrated dehiscence bilaterally. Categorization of these 24 patients with respect to age group is outlined in Table 1. The prevalence of canal dehiscence was calculated with respect to each age group with results outlined in Fig 1.
Table 1:
Age groups of patients with SSCD
| Age Group (yr) | Total Patients Reviewed | Total Patients with SSCD |
|---|---|---|
| 0–20 | 46 | 1 |
| 21–40 | 92 | 5 |
| 41–60 | 120 | 9 (3a) |
| 61–80 | 40 | 7 (3a) |
| 81–100 | 6 | 2 |
Number of patients with bilateral dehiscence.
Fig 1.
Prevalence of patients with SSCD and age.
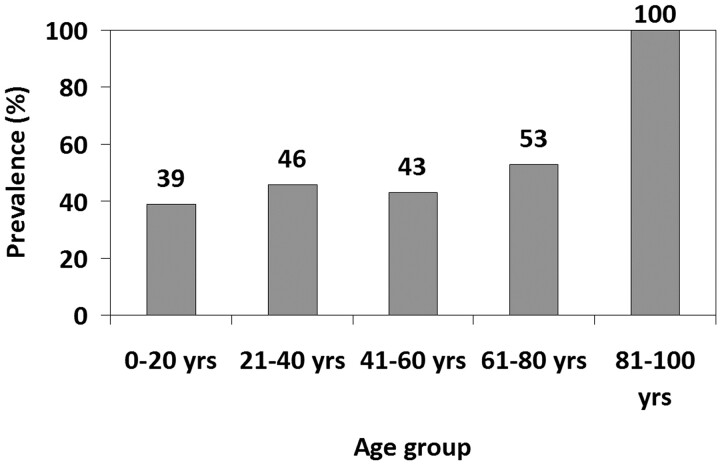
Of the 304 patients evaluated, 137 were identified with thinning of the superior semicircular canal, of whom 50 demonstrated the finding bilaterally. Categorization of these 137 patients with respect to age group is outlined in Table 2. Prevalence of canal thinning was calculated with respect to each age group with results as outlined in Fig 2.
Table 2:
Age groups of patients with canal thinning
| Age Group (yr) | Total Patients Reviewed | Total Patients with Thinning |
|---|---|---|
| 0–20 | 46 | 18 (7a) |
| 21–40 | 92 | 42 (17a) |
| 41–60 | 120 | 50 (19a) |
| 61–80 | 40 | 21 (5a) |
| 81–100 | 6 | 6 (2a) |
Number of patients with bilateral thinning.
Fig 2.
Prevalence of patients with canal thinning and age.
On average each successively older age category experienced a 93% increase (95% CI, 30%–187%) in the prevalence of the SSCD (P = .001) and a 9% increase (95% CI, −5%–25%) in the prevalence of thinning (P = .21). Neither crude nor age-adjusted models demonstrated a significant association between thinning and contralateral dehiscence (P = .63) nor between dehiscence and contralateral thinning (P = .73).
Discussion
Despite the large volume of literature regarding diagnosis and treatment of the SSCD syndrome, it still remains unclear whether the condition has a predominantly congenital/developmental basis or whether it is acquired in life. There is some literature suggesting a congenital basis for the condition, with 1 case report describing the syndrome in a young child.2 A report from a radiologic series suggested a developmental basis for the condition, demonstrating greater prevalence of unilateral canal thinning when the opposite side is affected by dehiscence.3 In a large postmortem series by Carey et al,4 the superior semicircular canal roof was demonstrated to show progressive thickening during the first 3 years of life, with data suggesting that dehiscence arises from a defect in postnatal development. Certainly, congenital aplasia of inner ear structures, including the superior semicircular canal, has been described in both syndromic and nonsyndromic cases of congenital hearing loss.5,6 However, in practical experience at our institution, the radiologic diagnosis of SSCD is made more commonly among middle and older age groups. To our knowledge, there have been no large-scale investigations to date addressing imaging prevalence of SSCD with respect to age.
Our data demonstrate a statistically significant increase in the prevalence of radiographic dehiscence as age increases and an increasing trend but no significant increase in prevalence of thinning with age. Furthermore, our data show no significant association between thinning and contralateral dehiscence or vice versa, suggesting that thinning occurs independently of dehiscence. While there may be a congenital basis for some cases of SSCD, our data support the impression that SSCD is more commonly an acquired rather than a congenital/developmental condition.
The etiology for the increased prevalence of dehiscence with age remains unclear; while literature on the clinical diagnosis and treatment of canal dehiscence is plentiful, there is a paucity of literature on possible etiologies, to our knowledge. We conjecture that our finding of the increasing prevalence of SSCD with age may be related to systemic bony demineralization generally observed to increase with age. However, while bone resorption in the inner ear in the setting of osteoporosis has been shown in animal models,7 to our knowledge, it has not been confirmed in human studies. Certainly, the utility of CT bone attenuation measurement in the diagnosis of otosclerosis has been investigated, with some but not all groups showing focal diminished bone attenuation in patients with otosclerosis compared with controls.8–11 Change in bone attenuation with age in the inner ear is of great interest to the authors and is currently under investigation by our group. Alternatively, we conjecture that the condition may be the cumulative result of repetitive microtrauma, which would increase in number throughout the course of life, but this is yet to be proved.
While this investigation reviewed the radiologic prevalence of SSCD, we did not specifically address the long-term clinical outcome analysis of our patients in this particular investigation, which could be considered a limitation. The relevance of the imaging finding of SSCD, therefore, remains unclear but is currently under investigation by our group.
Conclusions
While there may be a congenital basis for some cases of SSCD, our data support the impression that SSCD is more commonly an acquired rather than congenital or developmental condition.
Abbreviations
- CI
confidence interval
- SSCD
superior semicircular canal dehiscence
Footnotes
Paper previously presented at: Annual Meeting of the American Society of Neuroradiology and the Neuroradiology Education and Research Foundation Symposium, May 31–June 5, 2008; New Orleans, Louisiana.
References
- 1. Minor LB, Solomon D, Zinreich JS, et al. Sound- and/or pressure-induced vertigo due to bone dehiscence of the superior semicircular canal. Arch Otolaryngol Head Neck Surg 1998;124:249–58 [DOI] [PubMed] [Google Scholar]
- 2. Zhou G, Ohlms L, Liberman J, et al. Superior semicircular canal dehiscence in a young child: implication of developmental defect. Int J Pediatr Otorhinolaryngol 2007;71:1925–28 [DOI] [PubMed] [Google Scholar]
- 3. Hirvonen TP, Weg N, Zinreich SJ, et al. High-resolution CT findings suggest a developmental abnormality underlying superior canal dehiscence syndrome. Acta Otolaryngol 2003;123:447–81 [DOI] [PubMed] [Google Scholar]
- 4. Carey JP, Minor LB, Nager GT. Dehiscence or thinning of bone overlying the superior semicircular canal in a temporal bone survey. Arch Otolaryngol Head Neck Surg 2000;126:137–47 [DOI] [PubMed] [Google Scholar]
- 5. Morimoto AK, Wiggins RH, 3rd, Hudgins PA, et al. Absent semicircular canals in CHARGE syndrome: radiologic spectrum of findings. AJNR Am J Neuroradiol 2006;27:1663–71 [PMC free article] [PubMed] [Google Scholar]
- 6. Satar B, Mukherji SK, Telian SA. Congenital aplasia of the semicircular canals. Otol Neurotol 2003;24:437–46 [DOI] [PubMed] [Google Scholar]
- 7. Horner KC. The effect of sex hormones on bone metabolism of the otic capsule: an overview. Hear Res 2009;252:56–60. Epub 2008 Dec 24 [DOI] [PubMed] [Google Scholar]
- 8. Tringali S, Pouget JF, Bertholon P, et al. Value of temporal bone density measurements in otosclerosis patients with normal-appearing computed tomographic scan. Ann Otol Rhinol Laryngol 2007;116:195–98 [DOI] [PubMed] [Google Scholar]
- 9. Kawase S, Naganawa S, Sone M, et al. Relationship between CT densitometry with a slice thickness of 0.5 mm and audiometry in otosclerosis. Eur Radiol 2006;16:1367–73 [DOI] [PubMed] [Google Scholar]
- 10. Grayeli AB, Yrieix CS, Imauchi Y, et al. Temporal bone density measurements using CT in otosclerosis. Acta Otolaryngol 2004;124:1136–40 [DOI] [PubMed] [Google Scholar]
- 11. Huizing EH, de Groot JA. Densitometry of the cochlear capsule and correlation between bone density loss and bone conduction hearing loss in otosclerosis. Acta Otolaryngol 1987;103:464–68 [PubMed] [Google Scholar]