SUMMARY:
We performed high-resolution DIR-BBI of the cervical arteries at 3T in 19 subjects with cervical dissection. It offered excellent visualization of both the lumen and arterial wall, allowing detection of the primary and secondary features of dissection. We suggest that this is a highly useful technique for diagnosis of cervical dissection, either routinely or in equivocal cases of suspected dissection. It also offers further insight into the pathogenesis of this disorder.
DIR-BBI has proved to be an excellent technique for structural assessment of the vascular system, nulling signal intensity from flowing blood and perivascular fat. When performed with a surface coil at 3T, it offers a high-resolution assessment of the cervical artery wall and lumen. The technique has been widely used for assessment of carotid atheromatous plaque, allowing plaque subcomponents and substructural changes to be identified.1
We were interested in applying this technique to cervical artery dissection, a pathology that arises in the arterial wall, to see if DIR-BBI might either assist in the diagnosis and/or add to the known pathogenesis and imaging appearances of this condition. Dissection is increasingly recognized as an underlying cause of stroke,2–4 which is of significant importance because it is treatable. Various imaging modalities have been used to diagnosis this condition, including digital subtraction angiography5 CTA,6 and MR imaging (MR angiography or T1-weighted fat-saturated imaging).7 The diagnosis of dissection can be challenging for all modalities, often relying on secondary luminal findings. Only CTA and MR imaging can assess the primary site of pathology, the arterial wall, though MR imaging offers a much higher contrast resolution for detection of hemorrhage.
Methods and Technique
We performed DIR-BBI of the cervical arteries in subjects with arterial dissection. A high-resolution approach was used, with 3T MR imaging (Signa Excite; GE Healthcare, Milwaukee, Wisconsin) and a surface coil (phased-array 4-channel; Herman Flick, Flick Engineering Solution BV, the Netherlands). 2D time-of-flight angiography of the neck vessels was used to plan axial 2D BBI (T1-weighted and T2*-weighted).
We applied the technique to 19 subjects (12 men, 7 women; mean age, 47 ± 16 years) with cervical artery dissection in at least 1 vessel, confirmed by CTA (64-section Brilliance CT scanner; Philips Healthcare, Best, the Netherlands) (0.625-mm sections; bolus tracking, 75 mL of contrast at 5 mL/s). Each of the 4 cervical arteries on CTA and BBI was independently reviewed for signs of dissection: 1) intimal flap or double lumen, 2) wall thickening ± T1 hyperintensity of subacute hemorrhage (BBI only), and 3) stenosis, occlusion, or pseudoaneurysm. A conclusion on the presence or absence of dissection was reached for each vessel (CTA, 1 observer; MR imaging, 2 observers, by consensus), and any other potentially relevant observations were noted. Statistical analyses were performed by using the Statistical Package for the Social Sciences software (SPSS, Chicago, Illinois).
Results
Demographics, clinical findings, and brain imaging findings are summarized in Table 1. Vascular findings are summarized in Table 2. MR imaging was performed a median of 4 days after CTA (interquartile range, 1–5 days).
Table 1:
Demographics: clinical and brain imaging findings
| Subject | Sex | Age (yr) | Neurology | Antecedents | Brain Imaging Findings |
|---|---|---|---|---|---|
| 1 | M | 39 | Dizziness and diplopia | Established right PICA infarct, recent right PCA infarct | |
| 2 | F | 28 | Vertigo, diplopia, and left sensory disturbance | Right midbrain infarct | |
| 3 | M | 51 | Right sensory disturbance with left Horner syndrome | Working on overhead light | Lateral medullary infarct |
| 4 | M | 75 | Left facial weakness with expressive dysphasia | Prior transient ischemic attack, smoker | Left occipital infarct |
| 5 | M | 65 | Ataxia, dysphonia, left sensory disturbance | Hypertensive, type 2 diabetes, ex-smoker | Left medullary infarct |
| 6 | F | 35 | Top of basilar syndrome | Right cerebellar and bilateral thalamic infarct | |
| 7 | M | 44 | Dysarthria, left homonymous hemianopia | Left occipital infarct | |
| 8 | M | 41 | Right hemiparesis dysarthria and eye movement disorder | Left PCA infarct | |
| 9 | M | 32 | Dysarthria, ataxia, and photophobia | Playing soccer at time | Right occipital infarct |
| 10 | F | 71 | Diplopia and dizziness | Hypertensive | Bilateral cerebellar and pontine infarcts |
| 11 | M | 40 | Vertigo, right weakness, dysarthria, and nystagmus | Right cerebellar infarct | |
| 12 | F | 26 | Left facial droop and ptosis | Ehlers Danlos syndrome type 1 | Left thalamic and bilateral cerebellar infarcts |
| 13 | F | 19 | Collapse, left weakness; dysarthria and homonymous hemianopia | Weak history of trauma, on injectable contraceptive | Right MCA territory infarct |
| 14 | M | 60 | Left sensorimotor, left homonymous hemianopia | Right total anterior circulatory stroke | |
| 15 | F | 64 | Right weakness and dizziness | Right MCA territory infarct | |
| 16 | M | 45 | Left Horner syndrome | Heavy laborer with prior chiropractic treatment | |
| 17 | M | 68 | Right weakness | Left parietal and insular infarct | |
| 18 | F | 55 | Right weakness and dysphasia | Left basal ganglia infarct | |
| 19 | M | 48 | Right weakness and dysphasia | Left MCA territory infarct |
Table 2:
Vascular imaging findings
| Subject | Dissected Vessel | Modality | Lumena | Wallb | Vessel Contour | Other |
|---|---|---|---|---|---|---|
| 1 | Rt VA | CTA | Intimal flap | Thickened | Stenosis | |
| Rt VA | BBI | Intimal flap | Thickened | Occlusion | Periadvential T2 hyperintensity | |
| T1 hyperintensity + | ||||||
| 2 | Lt VA | CTA | – | Thickened | Stenosis | |
| Lt VA | BBI | – | Thickened | Stenosis | ||
| T1 hyperintensity ++ | ||||||
| T2* hypointensity + | ||||||
| Rt VA | CTA | – | Thickened | Stenosis | ||
| Rt VA | BBI | Intimal flap | Thickened | Stenosis | Periadvential T2 hyperintensity | |
| T1 hyperintensity ++ | ||||||
| 3 | Lt VA | CTA | – | Thickened | Stenosis | |
| Lt VA | BBI | – | Thickened | Stenosis | Periadvential T2 hyperintensity | |
| T1 hyperintensity ++ | ||||||
| 4 | Lt VA | CTA | – | Normal | Stenosis | (Abnormal but equivocal cause) |
| Lt VA | BBI | – | Thickened | Occlusion | Periadvential T2 hyperintensity | |
| T1 hyperintensity ++ | ||||||
| 5 | Lt VA | CTA | – | Thickened | Occlusion | |
| Lt VA | BBI | – | Thickened | Occlusion | Periadvential T2 hyperintensity | |
| T1 hyperintensity + | ||||||
| 6 | Lt VA | CTA | – | Thickened | Stenosis | |
| Lt VA | BBI | – | Thickened | |||
| T1 hyperintensity ++ | Stenosis | |||||
| Rt VA | CTA | – | Thickened | Stenosis | ||
| Rt VA | BBI | – | Thickened | |||
| T1 hyperintensity ++ | Stenosis | |||||
| T2* hypointensity + | ||||||
| 7 | Rt VA | CTA | – | Thickened | Occlusion | |
| Rt VA | BBI | – | Thickened | Occlusion | Periadvential T2 hyperintensity | |
| T1 hyperintensity + | ||||||
| 8 | Lt VA | CTA | – | Thickened | Stenosis | |
| Lt VA | BBI | Intimal flap | Thickened | Stenosis | Periadvential T2 hyperintensity | |
| T1 hyperintensity ++ | ||||||
| 9 | Lt VA | CTA | Intimal flap | Thickened | Occlusion | |
| Lt VA | BBI | Intimal flap | Thickened | Stenosis | Periadvential T2 hyperintensity | |
| T1 hyperintensity + | ||||||
| T2* hypointensity + | ||||||
| 10 | Lt VA | CTA | – | Thickened | Occlusion | |
| Lt VA | BBI | Intimal flap | Thickened | Stenosis | Periadvential T2 hyperintensity | |
| T1 hyperintensity +/++ | ||||||
| Rt VA | CTA | – | Thickened | Stenosis | ||
| Rt VA | BBI | – | Thickened | Stenosis | Periadvential T2 hyperintensity | |
| T1 hyperintensity + | ||||||
| 11 | Rt VA | CTA | Intimal flap | Thickened | Stenosis | (Abnormal but equivocal cause) |
| Rt VA | BBI | Intimal flap | Thickened | Stenosis | Periadvential T2 hyperintensity | |
| T1 hyperintensity +/++ | ||||||
| 12 | Lt VA | CTA | – | Thickened | Occlusion | |
| Lt VA | BBI | Intimal flap | Thickened | Stenosis | Periadvential T2 hyperintensity | |
| T2* hypointensity + | ||||||
| 13 | Rt CA | CTA | – | Thickened | Occlusion | |
| Rt CA | BBI | Intimal flap | Thickened | Occlusion | Periadvential T2 hyperintensity | |
| T1 hyperintensity + | ||||||
| 14 | Rt CA | CTA | – | Thickened | Occlusion | |
| Rt CA | BBI | Intimal flap | Thickened | Occlusion | Periadvential T2 hyperintensity | |
| T1 hyperintensity ++ | ||||||
| 15 | Lt CA | BBI | Intimal flap | Thickened | – | Periadvential T2 hyperintensity |
| T1 hyperintensity + | ||||||
| Rt CA | CTA | Intimal flap | Thickened | Stenosis | ||
| Rt CA | BBI | Intimal flap | Thickened | Stenosis | Periadvential T2 hyperintensity | |
| T1 hyperintensity + | ||||||
| 16 | Rt CA | CTA | Intimal flap | Thickened | Stenosis | Pseudoaneurysm |
| Rt CA | BBI | – | Thickened | Stenosis | Pseudoaneurysm | |
| T1 hyperintensity ++ | Periadvential T2 hyperintensity | |||||
| 17 | Lt CA | CTA | – | Thickened | Occlusion | |
| Lt CA | BBI | Intimal flap | Thickened | Stenosis | Periadvential T2 hyperintensity | |
| T1 hyperintensity ++ | ||||||
| 18 | Lt CA | CTA | Intimal flap | Thickened | Occlusion | |
| Lt CA | BBI | Intimal flap | Thickened | Stenosis | Periadvential T2 hyperintensity | |
| T1 hyperintensity ++ | ||||||
| Rt CA | BBI | Intimal flap | Thickened | Stenosis | Periadvential T2 hyperintensity | |
| T1 hyperintensity ++ | ||||||
| 19 | Lt CA | CTA | Intimal flap | Thickened | Stenosis | |
| Lt CA | BBI | Intimal flap | Thickened | Stenosis | Periadvential T2 hyperintensity | |
| T1 hyperintensity ++ |
Intraluminal flap present or absent.
Wall characteristics: + indicates moderate; ++, strong.
There was no significant difference between CTA and BBI in the number of subjects or individual vessels with dissection (subjects: CTA, n = 17; BBI, n = 19; vessels: CTA, n = 20; BBI, n = 24; McNemar test: P > 0.05). (On CTA review, 2 subjects were thought to show imaging features that could have resulted from atherosclerosis or dissection).
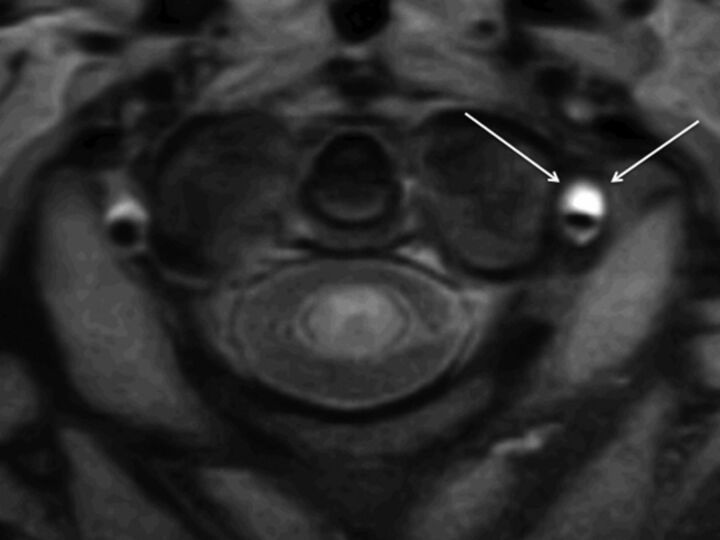
MR imaging detected more intimal flaps or double lumen (MR imaging, n = 15; CTA, n = 7; McNemar test, P < .03) (Fig 1A, -B). Wall thickening was more commonly identified on MR imaging (MR imaging, n = 24; CTA, n = 18; McNemar test, P < .04), and T1 hyperintensity, in keeping with hematoma, was noted in all dissected vessels (Fig 3), while T2* was decreased in 3 (Fig 4 ). In 5, hematoma was localized as subintimal (VA, n = 3; CA, n = 2) (Fig 5), and in 1, it was as intramedial.
Fig 1.
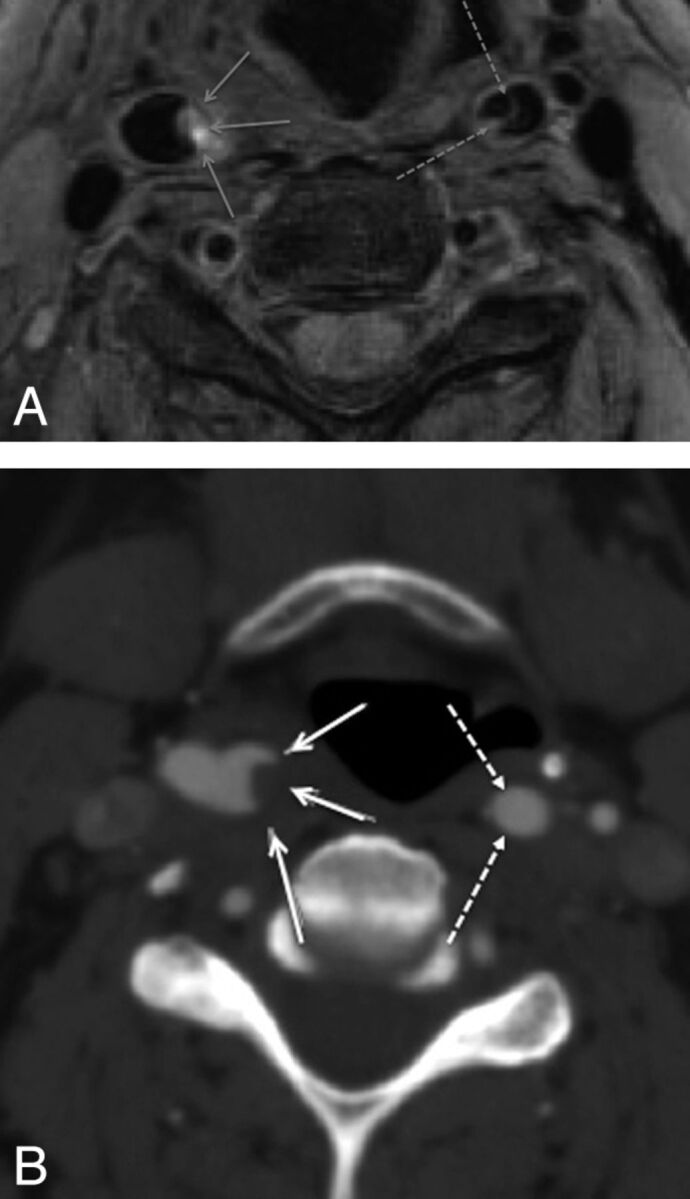
BBI (A) performed 1 day subsequent to CTA (B) demonstrates thrombus within the lumen of the right internal carotid artery (continuous arrows) but also a dissection flap in the left internal carotid artery not appreciated on CTA.
Fig 2.
Double inversion recovery BBI demonstrates crescentic intramural high T1 methemoglobin signal intensity (arrows) in the dissected left VA.
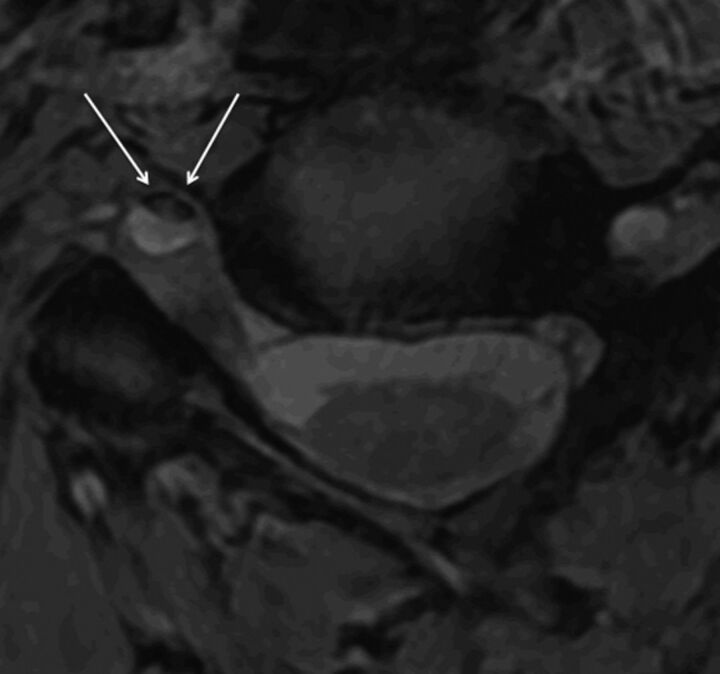
Fig 3.
T2* sequence demonstrates crescentic intramural deoxyhemoglobin signal intensity (arrows) in the dissected right VA.
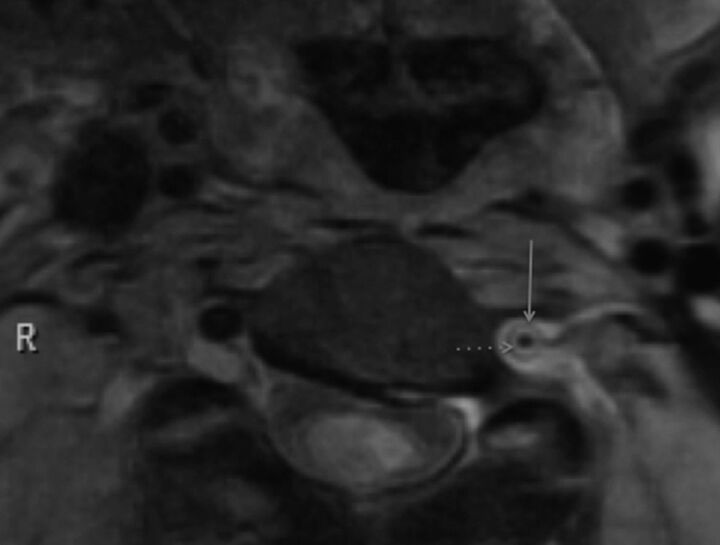
Fig 4.
“Target sign” appearance on BBI caused by hematoma in subintimal dissection. The media (continuous arrow) returns low signal intensity; the hematoma (discontinuous arrow), high signal intensity.
Fig 5.
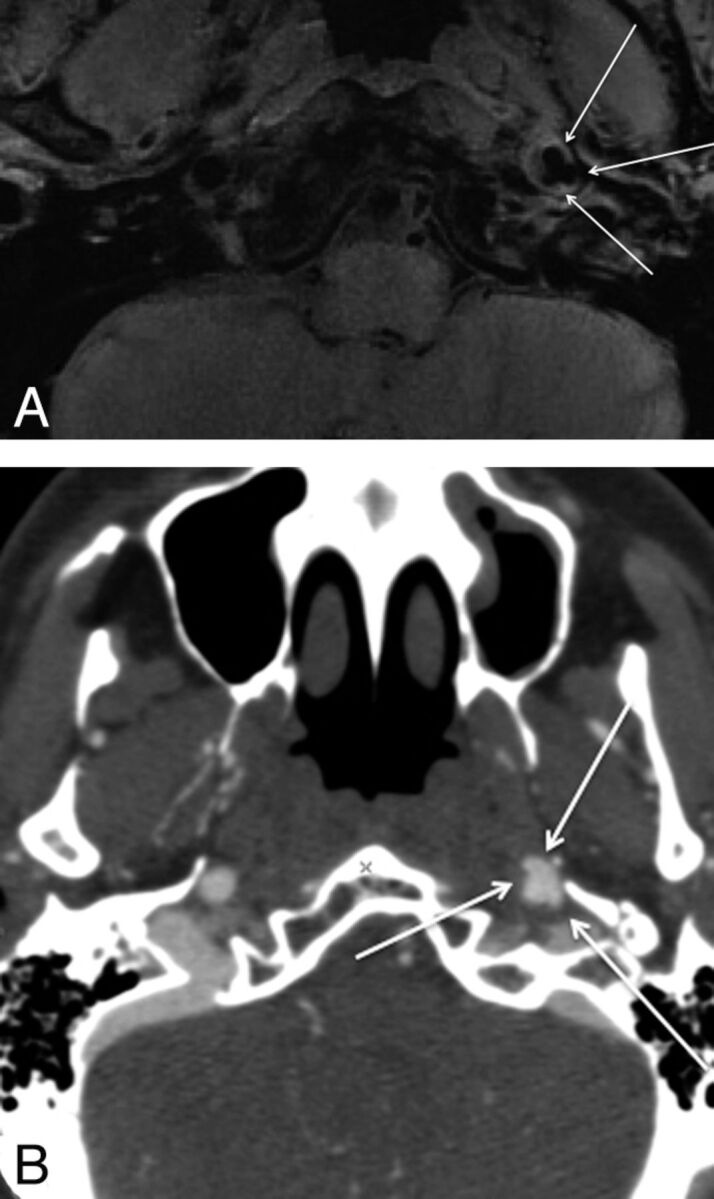
Both BBI (A) and CTA (B) demonstrate pseudoaneurysm formation in the skull base of the dissected left internal carotid artery.
There was no difference in the ability of CTA and MR imaging to detect occlusion (CTA, n = 8; MR imaging, n = 7) or stenosis (CTA, n = 13; MR imaging, n = 15) (McNemar test, no significant difference). A pseudoaneurysm was seen in only 1 dissected CA, on both modalities (Fig 2 A, -B).
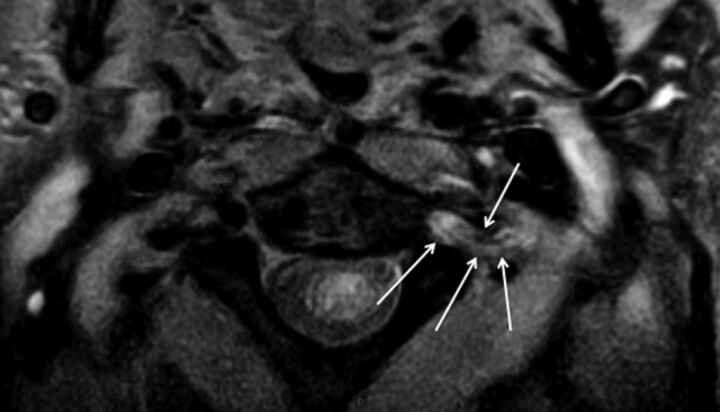
Observational note was made of T2 hyperintense periadventitial edematous signal-intensity change, which tracked into the adjacent parenchyma (dissected vessels, n = 20; normal vessels, n = 0; χ2 test, P < .001) (Fig 6 ).
Fig 6.
Periadventitial signal-intensity change (arrows), presumed due to inflammatory response, surrounding the dissected left VA.
Discussion
This study confirms that BBI is a useful technique for detection of the pathologic findings of dissection, allowing a confident diagnosis to be made.
We chose to perform this technique on subjects with known dissection, as confirmed by CTA, providing a high concentration of pathologic vessels on which to evaluate this sequence. While our study was not designed to compare the sensitivity and specificity of CTA and MR imaging in diagnosing dissection,8 BBI did offer improved detection of intimal flaps and wall thickening, suggesting it might offer some improved sensitivity. This technique allows clear visualization of the vessel lumen: Flowing blood is saturated by inversion pulses, giving a true black-blood appearance, improved over spin-echo sequences and offering a high sensitivity to the detection of intraluminal pathology. It also offers excellent spatial and contrast resolution of the vessel wall, allowing better detection of wall thickening and hemorrhage. High T1 contrast resolution allows detection of subacute hemorrhage. We did notice some variation in the strength of T1 hyperintensity, as yet unexplained and not in our data, related to symptom duration. We included a T2*-weighted sequence to identify the low signal intensity of deoxyhemoglobin in acute dissection, though the numbers were too small to analyze.
The high-resolution DIR-BBI technique may allow us to examine the pathogenesis of dissection further. The traditional belief is that a tear occurs within the intima, allowing entry of arterial blood, creating a false plane of cleavage. This explains why patients with inherent structural collagen weakness9,10 are more prone to the condition, but in total, this accounts for only 1%–5% of those affected; in our series only 1 patient (5%) had such connective tissue disease. Contrary to this theory is that of spontaneous rupture of the vasa vasorum. Following this initial event, dissection can extend either between the intima and media, resulting in stenosis or occlusion, or alternatively and less frequently between media and thinner adventitia, which may lead to pseudoaneurysm formation and occasionally rupture and subarachnoid hemorrhage if intracranial.11 Spontaneous rupture of the vasa vasorum, as an underlying cause of dissection might explain why a flap is uncommonly seen at autopsy. However, we identified a flap in nearly one-third of subjects, suggesting that its presence is more common than previously thought and adding support for an intimal tear as a significant primary pathogenic process of arterial dissection.
With the high-resolution DIR-BBI technique, we found it possible to clearly differentiate intramural hematoma from intraluminal thrombus; furthermore, we could sometimes differentiate intramedial from subintimal hemorrhage.
An observational finding commonly noted was T2 hyperintense periadventitial signal-intensity change. We postulate that during acute dissection, the artery is surrounded by a variable degree of inflammatory edema. A similar response has been demonstrated in spontaneous coronary artery dissection,12,13 and our study confirms similar observation in cervical dissection, as recently reported.14
Conclusions
3T DIR-BBI is useful in the evaluation of acute cervical artery dissection, offering excellent visualization of the lumen, wall, and periadventitia. This technique could be used either for primary diagnosis or as an adjunct in difficult or inconclusive cases. Furthermore, its high spatial and contrast resolution offers a mode of further exploration into the pathogenesis of dissection.
ABBREVIATIONS:
- BBI
black-blood imaging
- CA
carotid artery
- CTA
CT angiography
- DIR
double inversion recovery
- MCA
middle cerebral artery
- PCA
posterior cerebral artery
- PICA
posterior inferior cerebellar artery
- VA
vertebral artery
Footnotes
Paper previously presented at: Annual Meeting of the American Society of Neuroradiology, May 31–June 5, 2008; New Orleans, Louisiana.
References
- 1. DeMarco JK, Ota H, Underhill HR, et al. MR carotid plaque imaging and contrast-enhanced MR angiography identifies lesions associated with recent ipsilateral thromboembolic symptoms: an in vivo study at 3T. AJNR Am J Neuroradiol 31: 1395–402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med 2001; 344: 898– 906 [DOI] [PubMed] [Google Scholar]
- 3. Schievink WI, Mokri B, O'Fallon WM. Recurrent spontaneous cervical artery dissection. N Engl J Med 1994; 330: 393– 97 [DOI] [PubMed] [Google Scholar]
- 4. Schievink WI, Mokri B, Whisnant JP. Internal carotid artery dissection in a community: Rochester, Minnesota, 1987–1992. Stroke 1993; 24: 1678– 80 [DOI] [PubMed] [Google Scholar]
- 5. Provenzale JM. Dissection of the internal carotid and vertebral arteries: imaging features. AJR Am J Roentgenol 1995: 165; 1099– 1104 [DOI] [PubMed] [Google Scholar]
- 6. Chen CJ, Tseng YC, Lee TH, et al. Multisection CT angiography compared with catheter angiography in diagnosing vertebral artery dissection. AJNR Am J Neuroradiol 2004; 25: 769– 74 [PMC free article] [PubMed] [Google Scholar]
- 7. Ozdoba C, Sturzenegger M, Schroth G. Internal carotid artery dissection: MR imaging features and clinical-radiologic correlation. Radiology 1996; 199: 191– 98 [DOI] [PubMed] [Google Scholar]
- 8. Provenzale JM, Sarikaya B. Comparison of test performance characteristics of MRI, MR angiography, and CT angiography in the diagnosis of carotid and vertebral dissection: a review of the medical literature. AJR Am J Roentgenol 2009; 193: 1167– 74 [DOI] [PubMed] [Google Scholar]
- 9. Schievink WI, Michels VV, Piepgras DG. Neurovascular manifestations of heritable connective tissue disorders: a review. Stroke 1994; 25: 889– 903 [DOI] [PubMed] [Google Scholar]
- 10. Brandt T, Orberk E, Weber R, et al. Pathogenesis of cervical artery dissections: association with connective tissue abnormalities. Neurology 2001; 57: 24–30 [DOI] [PubMed] [Google Scholar]
- 11. Dziewas R, Konrad C, Drager B, et al. Cervical artery dissection: clinical features, risk factors, therapy and outcome in 126 patients. J Neurol 2003; 250: 1179– 84 [DOI] [PubMed] [Google Scholar]
- 12. Bateman AC, Gallagher PJ, Vincenti AC. Sudden death from coronary artery dissection. J Clin Pathol 1995; 48: 781– 84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Robinowitz M, Virmani R, McAllister HA. Spontaneous coronary artery dissection and eosinophilic inflammation: a cause and effect relationship? Am J Med 1982; 72: 923– 28 [DOI] [PubMed] [Google Scholar]
- 14. Bachmann R, Nassenstein I, et al. Spontaneous acute dissection of the internal carotid artery: high-resolution magnetic resonance imaging at 3.0 Tesla with a dedicated surface coil. Invest Radiol 2006; 41: 105– 11 [DOI] [PubMed] [Google Scholar]