Abstract
BACKGROUND AND PURPOSE:
CTA-like datasets can be reconstructed from whole-brain VPCTA. The aim of our study was to compare VPCTA with CTA for detection of intracranial stenosis and occlusion in stroke patients. Omitting CTA from stroke CT could reduce radiation dose.
MATERIALS AND METHODS:
One hundred sixty-three patients were included in this retrospective analysis. Inclusion criterion was suspected stroke within 4.5 hours after onset of symptoms. All examinations were performed on a 128-section multidetector CT scanner. Axial, coronal, and sagittal maximum intensity projections were reconstructed from CTA and from peak arterial phase of VPCTA. Images were scored for quality and presence of intracranial stenosis >50% or occlusion. For statistical analysis, the Wilcoxon signed-rank test and Fisher exact test were used, with a 2-tailed P value of .05 or less for statistical significance.
RESULTS:
Average image quality was superior in CTA (P < .05). However, image quality dichotomized for diagnostic significance was without difference between CTA and VPCTA (P > .05). Comparative statistical analysis revealed no significant difference for detection of intracranial stenosis and occlusion between CTA and VPCTA (P > .05). Substitution of intracranial CTA by VPCTA would lower radiation dose by 0.5 mSv.
CONCLUSIONS:
VPCTA is suited to assess the intracranial vasculature in patients with stroke and might have the potential to decrease radiation dose by substituting for intracranial CTA in stroke CT. Additional studies are necessary to further evaluate potential benefits of the dynamic nature of VPCTA.
Stroke is one of the leading causes of morbidity and mortality worldwide and a common cause of depression, epilepsy, and dementia in the elderly. Demographic changes will result in an increase in both incidence and prevalence in the future.1
Imaging of the brain and cerebral vessels is crucial in the assessment of patients with acute stroke and transient ischemic attack. In many institutions, imaging in patients with suspected stroke within 4.5 hours after onset of symptoms is performed using MMCT. NCCT distinguishes ischemic stroke from intracranial hemorrhage and stroke mimics. CTA may define the site and cause of arterial occlusion, grade collateral blood flow, and identify patients at high risk of stroke recurrence.2 PCT may delineate the infarct core and the ischemic penumbra.3,4
Until recently, a significant limitation of PCT was its limited coverage in the z-axis, which was restricted to the detector width (2–4 cm).5 Thus, only a limited part of the brain could be imaged at once. To overcome this restriction, several vendors developed different approaches to extend the scan range to 8–16 cm, offering whole-brain VPCT coverage.6,7 Typically, axial sections of 5- to 8-mm thickness are reconstructed from the VPCT source data for the subsequent calculation of perfusion parameter maps (TTP, MTT, CBF, and CBV). However, depending on the CT scanner used, it is possible to generate thin, high-resolution section datasets, comparable with conventional 3D CTA datasets but additionally offering temporal information (VPCTA). As these are reconstructed from the VPCT source data, no additional radiation exposure or administration of contrast agents is necessary. This technique may have the potential to substitute for CTA for the evaluation of the cerebral vasculature. Omitting CTA of the intracranial vessels from the MMCT protocol could decrease radiation dose.
Recently, Frölich et al8 described the feasibility of VPCTA for detection of intracranial large vessel occlusion. However, they did not evaluate stenoses and only reported a relatively small patient group. In our study, we evaluated a larger cohort and assessed the intracranial vessels for presence of occlusions and clinically relevant stenoses >50%.
The purpose of our study was to investigate whether VPCTA offers image quality comparable with CTA and reliably demonstrates intracranial vascular stenosis and occlusion. The hypothesis was that VPCTA is comparable with CTA in patients with stroke.
Materials and Methods
Study Population
Institutional review board approval was obtained before the commencement of this retrospective study. Informed consent of the patient or next of kin was obtained according to local laws and regulations.
A total of 197 patients who underwent MMCT in our department between January and August 2011 were screened retrospectively for the study. Inclusion criterion was suspected stroke within 4.5 hours after onset of symptoms. Exclusion criteria were an age <18 years, incomplete examinations, and signs of hemorrhage in the NCCT.
Multimodal CT
All scans were acquired with a standardized MMCT protocol, consisting of NCCT, VPCT with 9.6-cm coverage in the z-axis, and supra-aortic CTA. All examinations were performed on a 128-section CT scanner (Somatom Definition AS+; Siemens, Erlangen, Germany). Scan order was NCCT, VPCT, and CTA in all patients. In each patient, 2 contrast agent injections were performed: 1 for VPCT and 1 for CTA. Image reconstruction parameters were identical for VPCTA and CTA (section thickness, 0.6 mm; increment, 0.4 mm; reconstruction kernel, B20f for CTA and H20f for VPCTA).
Acquisition Parameters
VPCT was performed in an adaptive 4D spiral mode (tube voltage, 80 kV; tube current-time product, 200 mAs; collimation, 128 × 0.6 mm; rotation time, 0.3 seconds; CT dose index volume, 220 mGy). The coverage in the z-axis included 9.6 cm from the skull base. Thirty spiral scans were performed within 45 seconds. In the adaptive 4D spiral mode, the table continuously performs a smooth, periodic motion between 2 end positions while acquiring spiral scans. This generates multiple 3D scans that are sequential over time. The effective dose was 4.2 mSv (personal communication by T. Struffert).
Thirty mL of iodinated contrast agent (iomeprol, Imeron 400; Bracco Imaging, Konstanz, Germany), followed by 30 mL of saline flush, were injected via an 18-gauge cannula into a cubital vein at a rate of 5 mL/s using a double-piston power injector (Medtron, Saarbruecken, Germany). The VPCT scan was initiated after a start delay of 4 seconds; 30 consecutive 3D datasets were reconstructed with the parameters described above.
CTA was performed in the caudocranial scan direction, with coverage in the z-axis from the aortic arch to the cranial apex (tube voltage, 120 kV; quality reference tube current-time product, 160 mAs; collimation, 128 × 0.6 mm; rotation time, 0.3 seconds; CT dose index volume, 9–12 mGy). Automatic tube current modulation was used (Care Dose4D; Siemens). Effective dose was 3.3 mSv (personal communication).
Fifty mL iodinated contrast agent (iomeprol, Imeron 400), followed by 30 mL of saline flush, were injected via an 18-gauge cannula into a cubital vein at a rate of 5 mL/s using a double-piston power injector (Medtron). Bolus tracking was performed at the level of the aortic arch, with a start delay of 4 seconds. Images were reconstructed with the parameters described above.
Image Processing
Each VPCTA dataset consists of 7140 section images, with a file size of 3.5 gigabytes, an amount of data which is difficult to evaluate and store with the workstations and archiving systems currently available. Therefore, in each VPCTA examination, an arterial opacification curve (Hounsfield units versus time) of both M1 segments and the basilar artery was calculated with the DynEva tool (Syngo; Siemens). The time point with the highest opacification in all 3 vessels was selected from the 30 temporal resolved 3D datasets, and transversal, coronal, and sagittal MIP reconstructions were generated using the 3D tool of the CT scanner workstation (Syngo; Siemens), similar to the approach of Frölich et al.8 Likewise, transversal, coronal, and sagittal MIP reconstructions were generated from each CTA dataset. MIP reconstruction parameters were chosen identical for VPCTA and CTA (image thickness, 10 mm; image distance, 5 mm).
Data Analysis
All MIP images were transferred to a workstation (Multimodality Workplace MMWP; Siemens) running standard software (Syngo; Siemens). Image data analysis was performed by 2 neuroradiologists in consensus. To reduce potential bias memory effect, the CTA and VPCTA images were assessed in random order. Readers were blinded to the patient clinical information, NCCT, and VPCT parameter maps (TTP, MTT, CBF, and CBV).
Image quality was assessed for CTA and VPCTA in each patient using a 4-point scale, previously described by Hinkmann et al9: 1) poor image quality, blurring of the vessel contours; 2) fair image quality, suboptimal arterial enhancement for confident diagnosis; 3) good image quality and arterial enhancement, adequate for confident diagnosis; and 4) excellent image quality and arterial enhancement. Results were dichotomized into nondiagnostic (ratings 1 and 2) and diagnostic (ratings 3 and 4) image quality.
All datasets were evaluated for vascular pathology using a 4-point scale derived from Nabavi et al10: 1) vessel not pictured (out of field of view); 2) vessel open, normal or stenosis <50%; 3) stenosis >50%; and 4) vessel occluded. In all vessel segments, the highest pathology was scored, even if only affecting a part of the vessel segment. In each patient, the following arterial segments were analyzed for vascular pathologies:
distal ICA
middle cerebral artery, proximal part of M1 segment (proximal M1)
middle cerebral artery, distal part of M1 segment (distal M1)
middle cerebral artery, M2 and M3 segments (M2–3)
anterior cerebral artery (ACA)
cranial part of basilar artery
posterior cerebral artery (PCA) .
Twin vessel segments (eg, ICA, M1) were scored independently, resulting in a maximum of 13 analyzed arterial segments per examination in the 7 anatomic regions. Hypoplastic or aplastic vessel segments were not rated pathologic. In CTA datasets, the readers only assessed the intracranial part of the vasculature comparable with the coverage of VPCTA. The readers were asked to report secondary findings (eg, aneurysms or tumors).
Statistical Analysis
For statistical analysis of the ordinal values of image quality and vascular pathology, the Wilcoxon signed-rank test was used. A 2-tailed P value of .05 or less was considered a significant difference. For statistical analysis of the target parameter of vascular pathology, nondiagnostic examinations (image quality ratings of 1 or 2) were excluded and only vessel segments pictured by both modalities (CTA and VPCTA) were considered.
For statistical analysis of the dichotomized image quality, the Fisher exact test was used. A 2-tailed P value of .05 or less was considered as a significant difference.
All statistical analyses were performed using commercially available software (SPSS 11; SPSS, Chicago, Illinois).
Results
Study Population
The study population consisted of 163 patients (84 women, 79 men; mean age, 71.1 ± 13.6 years [women, 74.9 ± 12.6 years; men, 67.1 ± 13.4 years]; time from onset of symptoms to imaging, 2.2 ± 1.1 hours). All eligible patients had received IV thrombolysis according to standard guidelines.11 In selected patients with proximal vessel occlusion, mechanical reperfusion had been performed.
Data Analysis
All datasets could be evaluated as described. In total, 326 examinations (163 CTA and 163 VPCTA) with 4238 vessel segments were analyzed. As a secondary finding, in 1 patient, a dural tumor, most likely a meningioma, was found in both modalities.
The scan range of VPCTA in the z-axis of 9.6 cm was generally sufficient to cover all analyzed intracranial vessels (Figs 1 and 2). In only 3.1% of the examinations, 1 or more assessed vessel segments were not pictured as a result of tilted patient head positioning or suboptimal planning of the scan range. As direct irradiation of the eye lenses during VPCT acquisition has to be avoided for cataract prevention, the V4 segments of the vertebral arteries and the caudal part of the basilar artery were generally not covered (Fig 3).
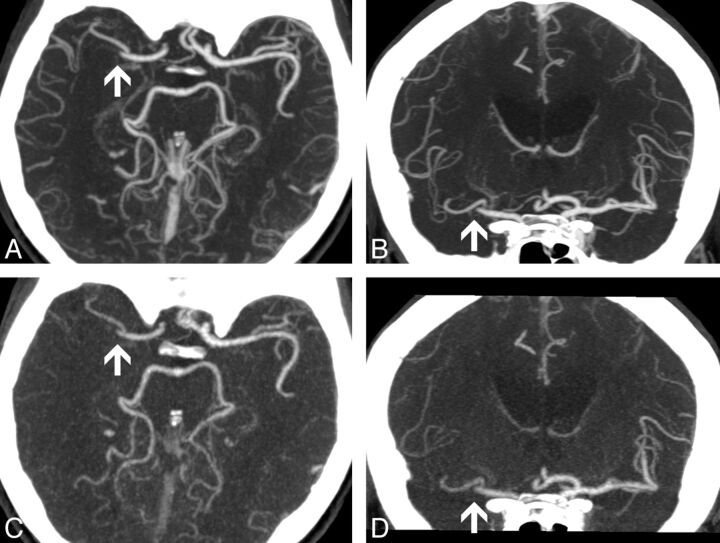
Fig 1.
A and B, CTA, transversal and coronal MIP reconstructions; image thickness 10 mm. C and D, VPCTA, transversal and coronal MIP reconstructions; image thickness 10 mm. The same window settings were used for all reconstructions. Occlusion of the distal main branch of the right middle cerebral artery is demonstrated in CTA and VPCTA (arrows). In VPCTA, veins are less contrasted.
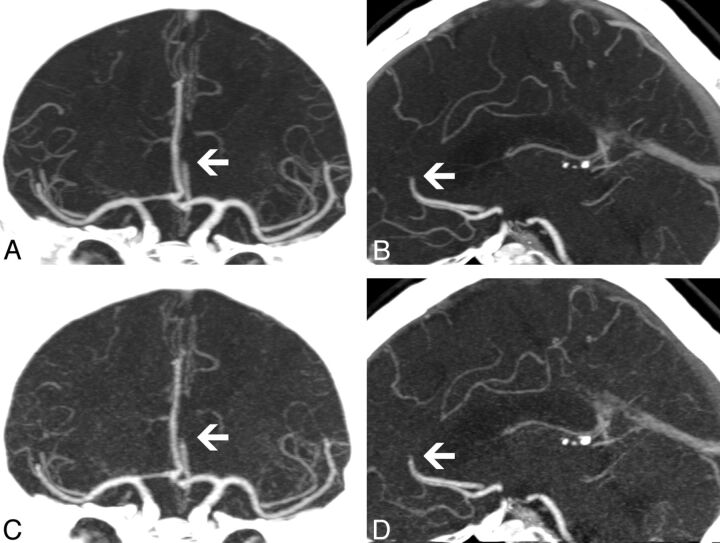
Fig 2.
A and B, CTA, coronal and sagittal MIP reconstructions; image thickness 10 mm. C and D, VPCTA, coronal and sagittal MIP reconstructions; image thickness 10 mm. The same window settings were used for all reconstructions. Occlusion of the A2 segment of the left anterior cerebral artery is clearly visible in CTA and VPCTA (arrows).
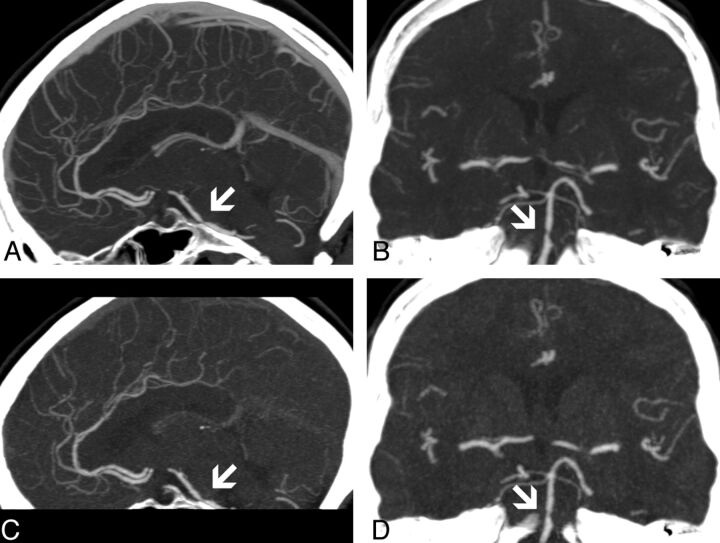
Fig 3.
A and B, CTA, sagittal and coronal MIP reconstructions; image thickness 10 mm. C and D, VPCTA, sagittal and coronal MIP reconstructions; image thickness 10 mm. The same window settings were used for all reconstructions. Stenosis >50% of the basilar artery is pictured in CTA and VPCTA (arrows). Generally, the most caudal part of the basilar artery is not covered in VPCTA, as direct irradiation of the eye lenses has to be avoided.
Image Quality
Overall, image quality was rated 3 or 4, ie, diagnostic, in 98.2% of CTA and 99.4% of VPCTA examinations. The image quality of 3 CTA and 1 VPCTA examinations was scored as nondiagnostic. In the 3 nondiagnostic CTA scans, the timing failed, resulting in a premature (n = 1) or delayed (n = 2) scan initiation. In the 1 nondiagnostic VPCTA, patient head movement deteriorated image quality. Average image quality scoring of CTA was significantly superior to VPCTA (P < .05). The detailed results are presented in Table 1.
Table 1:
Image quality scorings
| Modality | Image Quality |
|||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| CTA (n [%]) | 0 (0.0) | 3 (1.8) | 90 (55.2) | 70 (43.0) |
| VPCTA (n [%]) | 0 (0.0) | 1 (0.6) | 135 (82.8) | 27 (16.6) |
Note:—P < .01.
After dichotomization into the categories of diagnostic and nondiagnostic image quality, no significant difference was found between CTA and VPCTA (P = 1.00). The detailed results are presented in Table 2.
Table 2:
Dichotomized image quality scorings
| CTA |
Total | ||
|---|---|---|---|
| Diagnostic | Nondiagnostic | ||
| VPCTA | |||
| Diagnostic | 159 | 3 | 162 |
| Nondiagnostic | 1 | 0 | 1 |
| Total | 160 | 3 | 163 |
Note:—P = 1.00.
Vascular Pathology
Four pairs of CTA/VPCTA scans with nondiagnostic image quality were excluded from the statistical analysis of the target parameter of vascular pathology. This small number is not estimated to produce a relevant bias.
The readers reported a total of 11 vessel segments (ICA, 8; proximal M1, 1; distal M1, 1; basilar artery, 1) to be not pictured in VPCTA examinations in 5 different patients (3.1% of all examinations). Therefore, 22 vessel segments (11 pairs) were excluded from the statistical analysis. Thus, in the final statistical analysis of the target parameter of vascular pathology, 4164 vessel segments in 318 examinations were included.
The readers reported 82 cerebral vascular pathologies (7 stenoses >50%, 75 occlusions) in 46 patients in CTA (28.9% of patients with diagnostic examinations), and 83 vascular pathologies (8 stenoses >50%, 75 occlusions) in 47 patients in VPCTA examinations (29.6% of patients with diagnostic examinations). Three vessel-segment scorings did not agree between CTA and VPCTA (M2–3 right, 1 stenosis missed in CTA (Fig 4); M2–3 left, 1 occlusion missed in CTA, 1 occlusion missed in VPCTA). There was no statistically significant difference present between the findings reported in CTA and VPCTA (P < .05). The detailed results are presented in Table 3.
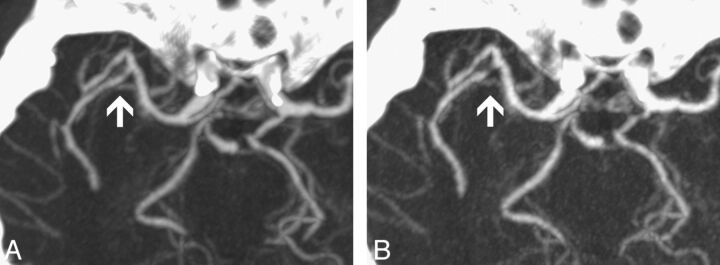
Fig 4.
A, CTA, transversal MIP reconstruction; image thickness 10 mm. B, VPCTA, transversal MIP reconstruction; image thickness 10 mm. The same window settings were used for both reconstructions. While CTA was scored normal, in VPCTA, stenosis >50% of a proximal right M2 segment was rated (arrows).
Table 3:
Vascular pathology scorings
| Vascular Segment | (1) Not Pictured in VPCTA | CTA |
VPCTA |
Number of Discrepancies | P | ||||
|---|---|---|---|---|---|---|---|---|---|
| (2) Normal or Stenosis <50 % | (3) Stenosis >50 % | (4) Occlusion | (2) Normal or Stenosis <50 % | (3) Stenosis >50 % | (4) Occlusion | ||||
| Right ICA | 3 | 152 | 0 | 4 | 152 | 0 | 4 | 0 | 1 |
| Left ICA | 5 | 148 | 0 | 6 | 148 | 0 | 6 | 0 | 1 |
| Right proximal M1 | 1 | 152 | 0 | 6 | 152 | 0 | 6 | 0 | 1 |
| Right distal M1 | 1 | 150 | 0 | 8 | 150 | 0 | 8 | 0 | 1 |
| Left proximal M1 | 0 | 154 | 0 | 5 | 154 | 0 | 5 | 0 | 1 |
| Left distal M1 | 0 | 150 | 1 | 8 | 150 | 1 | 8 | 0 | 1 |
| Right M2–3 | 0 | 148 | 0 | 11 | 147 | 1 | 11 | 1 | .32 |
| Left M2–3 | 0 | 147 | 0 | 12 | 147 | 0 | 12 | 2 | 1 |
| Right ACA | 0 | 159 | 0 | 0 | 159 | 0 | 0 | 0 | 1 |
| Left ACA | 0 | 155 | 0 | 4 | 155 | 0 | 4 | 0 | 1 |
| BA | 1 | 151 | 3 | 4 | 151 | 3 | 4 | 0 | 1 |
| Right PCA | 0 | 155 | 2 | 2 | 155 | 2 | 2 | 0 | 1 |
| Left PCA | 0 | 153 | 1 | 5 | 153 | 1 | 5 | 0 | 1 |
Note:—In CTA, all vessel segments were pictured. ACA indicates anterior cerebral artery; PCA, posterior cerebral artery; BA, basilar artery.
Discussion
We compared VPCTA to conventional CTA for the detection of intracranial clinically relevant stenosis (>50%) and occlusion in patients with acute stroke. Average image quality was superior in CTA. However, image quality dichotomized for diagnostic significance was without difference between CTA and VPCTA. We found no statistically significant difference for detection of intracranial stenosis and occlusion between CTA and VPCTA. In small vessel segments, we found statistically nonsignificant differences between CTA and VPCTA. Our hypothesis that VPCTA is comparable with CTA in this imaging setting was confirmed.
Comparison of Image Quality
Image quality scorings of CTA were significantly superior to VPCTA, due to more excellent (score 4) ratings in CTA than in VPCTA. This finding is most likely attributable to the higher amount of contrast agent injected in CTA. However, image quality was rated diagnostic in both CTA and VPCTA, and dichotomized image quality was without difference between CTA and VPCTA.
In contrast to our results, a comparable image quality of CTA and VPCTA on a 4-point scale was reported previously.8 However, in this work, different reconstruction parameters were used (thicker VPCTA reconstructions) and image quality was scored using an alternative approach (visibility of the distal M2 segments).
Comparison of Detection of Vascular Pathologies
There was no statistically significant difference in the number of vascular pathologies found in CTA and VPCTA. Scorings were identical for the large intracranial arteries. In general, detection of stenoses in distal vessel segments is more challenging. Accordingly, we found slight discrepancies between CTA and VPCTA in the evaluation of the peripheral MCA segments (M2–3 segments). However, these were not statistically significant. To our knowledge, this is the first published work describing the feasibility of VPCTA for assessment of intracranial stenosis.
In contrast to previous reports, in which 90%7 and 85%8 of the pathologic findings in CTA were also found on VPCTA images, our study showed better results without significant difference between CTA and VPCTA. Potential explanations of the discrepancy are the smaller study population and the thicker reconstructions in previous studies.
Mendonça et al12 recently described predictors of the success of IV rtPA therapy in patients with supra-aortic arterial occlusion. They found different predictors for occlusions in the proximal and the distal subsegments of the middle cerebral artery, which may have implications on clinical outcome and recanalization rates. In our evaluation, both VPCTA and CTA allowed differentiation of the site of M1 occlusion in all patients.
General Considerations for VPCTA
A major advantage of VPCTA is its insensitivity against timing issues. As the scans are repeated each 1.5 seconds over a period of 45 seconds, a dataset with optimal arterial opacification is generated for almost every patient. Depending on the experience of the technician, CTA can more easily be mistimed. Furthermore, bone subtraction is possible in VPCTA without increasing radiation dose, as native 3D datasets from the prebolus phase of VPCTA are available.
While the acquisition time of VPCT is only 45 seconds, the relatively long processing time for reconstruction of thin VPCTA sections (currently approximately 10 minutes) may be a disadvantage of VPCTA in the acute-stroke setting. Moreover, a thin, temporal resolved reconstruction of VPCTA generates a large dataset (7140 section images, with a file size of 3.5 gigabytes), which is difficult to read and store with the workstations and archiving systems currently available. With technical progress, both limitations are likely to be overcome in the future.
A general limitation of VPCTA as a substitute for CTA in the stroke setting is the limited coverage in the z-axis. Therefore, the carotid bifurcation is generally not pictured in VPCTA and has to be assessed by using a different technique (CTA, sonography).
Considerations for Radiation Dosage
To minimize radiation dose, the VPCT scan is carried out at a lower tube voltage than CTA (80 kV instead of 120 kV). This setting has the lowest radiation dose for a specific iodine contrast-to-noise ratio.13
The effective dose of the MMCT protocol used and CT scanner adds up to 8.9 mSv, with NCCT accounting for 1.4 mSv, the cervical part of CTA for 2.8 mSv, the intracranial part of CTA for 0.5 mSv, and VPCT for 4.2 mSv (personal communication). If intracranial CTA is substituted by VPCTA, an effective dose reduction of 0.5 mSv can be achieved.
Limitations
Our study is limited in 2 important ways. First, the amount of contrast agent used for VPCT was lower than in CTA. In a prospective approach, the VPCT contrast agent amount could have been increased. However, as for the calculation of VPCT perfusion parameter maps, a narrow bolus geometry is necessary, and the maximum amount of contrast agent used in VPCT is limited. Second, we only evaluated MIP reconstructions of CTA and VPCTA datasets. Evaluation of thin sections might have influence on detection of vascular pathologies.
Further investigations should focus on analysis of the additional hemodynamic information contained in VPCTA datasets, which may potentially impact treatment decisions, eg, evaluation of collateralization of vessel occlusions.
Conclusions
In summary, VPCTA is suited to assess the intracranial vasculature in patients with stroke for clinically relevant stenosis and occlusion, and might have the potential to substitute for intracranial CTA in the stroke imaging protocol. Additional studies are necessary to further evaluate potential benefits of VPCTA.
ABBREVIATIONS:
- MIP
maximum intensity projection
- MMCT
multimodal CT
- NCCT
noncontrast CT
- PCT
perfusion CT
- VPCT
volume perfusion CT
- VPCTA
CTA-like reconstruction from VPCT source data
References
- 1. Lopez AD, Mathers CD, Ezzati M, et al. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006;367:1747–57 [DOI] [PubMed] [Google Scholar]
- 2. European Stroke Organisation (ESO) Executive Committee ESO Writing Committee. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis 2008:25:457–507 [DOI] [PubMed] [Google Scholar]
- 3. Wintermark M, Flanders AE, Velthuis B, et al. Perfusion-CT assessment of infarct core and penumbra: receiver operating characteristic curve analysis in 130 patients suspected of acute hemispheric stroke. Stroke 2006;37:979–85 [DOI] [PubMed] [Google Scholar]
- 4. Wintermark M. Brain perfusion-CT in acute stroke patients. Eur Radiol 2005;15:D28–31 [DOI] [PubMed] [Google Scholar]
- 5. Klotz E, König M. Perfusion measurements of the brain: using dynamic CT for the quantitative assessment of cerebral ischemia in acute stroke. Eur J Radiol 1999;30:170–84 [DOI] [PubMed] [Google Scholar]
- 6. Siebert E, Bohner G, Masuhr F, et al. Neuroimaging by 320-row CT: is there a diagnostic benefit or is it just another scanner? A retrospective evaluation of 60 consecutive acute neurological patients. Neurol Sci 2010;31:585–93 [DOI] [PubMed] [Google Scholar]
- 7. Morhard D, Wirth CD, Fesl G, et al. Advantages of extended brain perfusion computed tomography: 9.6 cm coverage with time resolved computed tomography-angiography in comparison to standard stroke-computed tomography. Invest Radiol 2010;45:363–69 [DOI] [PubMed] [Google Scholar]
- 8. Frölich AM, Psychogios MN, Klotz E, et al. Angiographic reconstructions from whole-brain perfusion CT for the detection of large vessel occlusion in acute stroke. Stroke 2012;43:97–102 [DOI] [PubMed] [Google Scholar]
- 9. Hinkmann FM, Voit HL, Anders K, et al. Ultra-fast carotid CT-angiography: low versus standard volume contrast material protocol for a 128-slice CT-system. Invest Radiol 2009;44:257–64 [DOI] [PubMed] [Google Scholar]
- 10. Nabavi DG, Kloska SP, Nam EM, et al. MOSAIC: Multimodal Stroke Assessment Using Computed Tomography: novel diagnostic approach for the prediction of infarction size and clinical outcome. Stroke 2002;33:2819–26 [DOI] [PubMed] [Google Scholar]
- 11. Adams HP, Jr, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke. Stroke 2007;38:1655–711 [DOI] [PubMed] [Google Scholar]
- 12. Mendonça N, Rodriguez-Luna D, Rubiera M, et al. Predictors of tissue-type plasminogen activator nonresponders according to location of vessel occlusion. Stroke 2012;43:417–21 [DOI] [PubMed] [Google Scholar]
- 13. Wintermark M, Maeder P, Verdun FR, et al. Using 80 kVp versus 120 kVp in perfusion CT measurement of regional cerebral blood flow. AJNR Am J Neuroradiol 2000;21:1881–84 [PMC free article] [PubMed] [Google Scholar]