Abstract
Background
Vaccination may be critical to curtailing the spread of the SARS-CoV-2 virus responsible for the COVID-19 pandemic, but herd immunity can only be realized with high vaccination coverage. There is a need to identify empirically supported strategies to increase uptake, especially among young adults as this subpopulation has shown relatively poor adherence to physical distancing guidelines. Social norms – estimates of peers’ behavior and attitudes – are robust predictors of health behaviors and norms-based intervention strategies may increase COVID vaccine uptake, once available. This study examined the extent that vaccination intentions and attitudes were associated with estimated social norms as an initial proof-of-concept test.
Method
In November of 2020, 647 undergraduate students (46.21% response rate) completed online surveys in which they reported intentions to get COVID and influenza vaccines, perceived importance of these vaccines for young adults, and estimated social norms regarding peers’ vaccination behaviors and attitudes.
Results
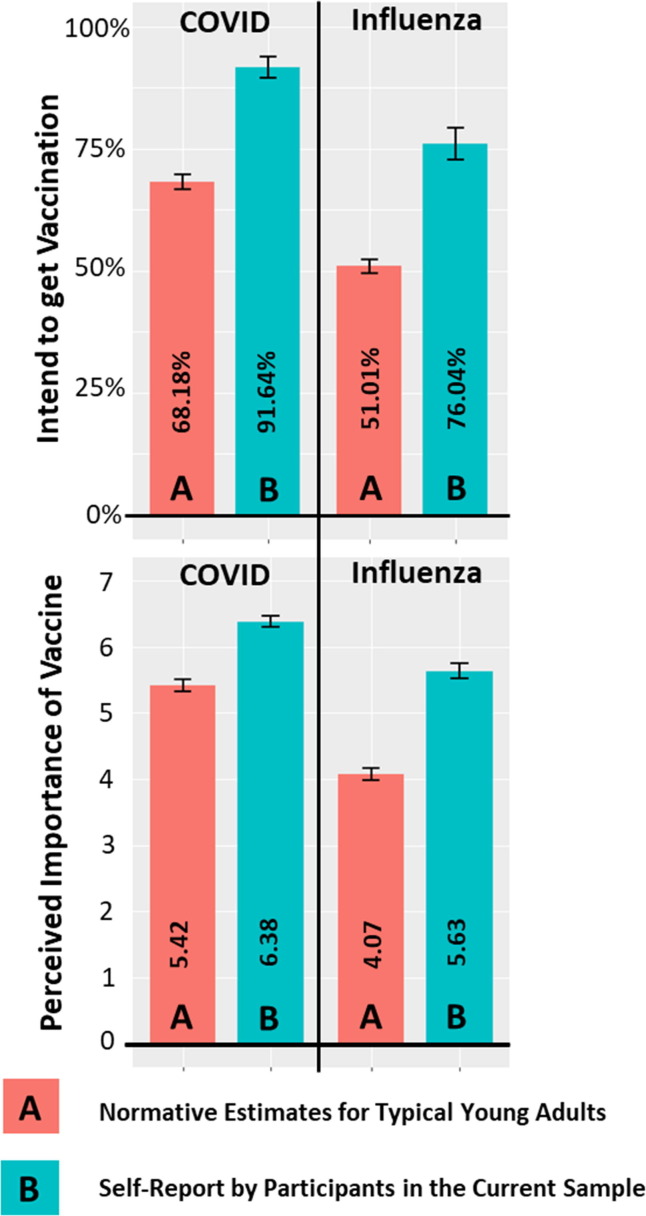
Students reported significantly greater intentions to get a COVID vaccine (91.64%) than an influenza vaccine (76.04%), and perceived COVID vaccination as significantly more important than influenza vaccination. The sample generally held strong intentions to receive a COVID vaccine and thought that doing so was of high importance, but participants, on average, perceived that other young adults would be less likely to be vaccinated and would not think vaccination was as important. Multiple regression models indicated that estimated social norms were positively associated with participants’ own intentions and perceived importance of getting a COVID vaccine.
Conclusions
These significant associations highlight the potential value in developing and testing norms-based intervention strategies, such as personalized normative feedback, to improve uptake of forthcoming COVID vaccines among young adults.
Keywords: COVID-19, SARS-CoV-2, Vaccination coverage, Vaccine uptake, Young adults
Introduction
The global burden associated with the SARS-CoV-2 virus (i.e., the COVID-19 pandemic) remains an unmitigated public health crisis. In the United States, the Centers for Disease Control (CDC) have endorsed numerous empirically-supported mitigation strategies to reduce person-to-person spread of the virus (e.g., wearing face masks) [1] and state governments have implemented physical distancing measures (e.g., travel restrictions, curfews). Despite these efforts, new cases have continued to rise across the fall and winter of 2020, with the U.S. continuing to face record-high numbers of new cases (e.g., 227,885 cases on a single day in December 2020 [2]). As the virus continues to spread, it has become clear that the most promising strategy for combatting COVID-19 is the rapid development of a prophylactic vaccine which can, optimistically, facilitate sufficient herd immunity [3]. Vaccinologists have made major headway; there are more than 200 COVID vaccines currently in development [4] and at the time of this writing, COVID vaccines have been made available to frontline essential workers and high-risk elderly in some states [5], and a fully public release is imminent [6]. While these prospects are encouraging, a critical question remains: Will people be willing to get a COVID vaccine, once available to the public?
Societal uptake of a COVID vaccine is a critical concern given that vaccines can only facilitate herd immunity if there is high vaccine coverage among the population [7]. Early estimates from May of 2020 show that acceptability and intentions to receive a COVID vaccine are relatively high, but perhaps not high enough to achieve population-wide protection. One study found that 69% of U.S. adults reported being either “definitely willing” or “probably willing” to get a COVID vaccine [8], and another found that most U.S. adults reported being likely to get a COVID vaccine (i.e., mean score of 5.24 with responses ranging from 1 = Very unlikely to 7 = Very likely) [9]. Depending on the efficacy and duration of COVID vaccines, experts estimate that approximately 70–90% of people need to be vaccinated to achieve herd immunity [10], but higher coverage rates are always desirable, especially considering the unknown efficacy of these novel vaccines. As such, there is a dire need for behavioral scientists to identify antecedents/correlates of intentions and attitudes towards COVID vaccinations to inform behavioral strategies that promote uptake.
1.1. COVID-19 among young adults
Once released to the public, COVID vaccines have first been made available to high-risk subgroups including elderly, those in assisted care facilities, and frontline health care workers [5], [6]. Although this prioritization is prudent, COVID-19 incidence rates are highest among young adults, making this age group a major factor for continued community transmission [11]. Indeed, many young adults feel less at-risk for the consequences of COVID-19 and this age group has reported the poorest adherence to mitigation strategies [12]. On one hand, young adults do have lower risk of developing severe symptoms and complications associated with COVID-19 [13], but because symptoms are often minor, young adults may be less likely to isolate and therefore more likely to unknowingly spread the virus [14]. It follows that vaccination may be especially critical for young adults as a key step towards curbing community transmission, including spread to high-risk people (e.g., elderly relatives).
Despite efforts to reduce spread, such as virtual and remote class formats, COVID-19 incidence rates were particularly high on U.S. college campuses throughout fall of 2020 [15]. Achieving high vaccine coverage among college students is a key step towards returning to societal normalcy as it pertains to higher education, but it is unclear whether sufficient coverage is likely. Nationally representative survey data indicate a need to improve vaccination attitudes and willingness among young adults: In April of 2020, only 50% of young adults reported intentions to get a COVID vaccine (41% reported being unsure) [16]. While initial estimates also indicate that educational attainment and household income are positively associated with vaccination intentions [17], college students remain a high priority group given low adherence to physical distancing guidelines and rampant spread of COVID-19 among this subpopulation.
1.2. Social norms approach to increase COVID vaccine uptake
Young adults’ health behaviors and attitudes are powerfully influenced by the behaviors and attitudes of their peers (i.e., social norms) [18]. Social norms are often categorized as either descriptive norms that entail individuals’ perceptions of others’ behavior, or injunctive norms that involve perceptions of others’ attitudes or opinions towards a behavior [19]. Both descriptive and injunctive norms have been shown to be salient predictors of health behaviors, such as seatbelt adherence [20] and alcohol use [21], [22]. Notably, there is some evidence that estimates of social norms are associated with college students’ intentions to receive the Human Papillomavirus (HPV) [23] and influenza vaccines [24]. As such, estimated peer norms may be an important antecedent of students’ intentions to receive a COVID vaccine.
As it pertains to the accuracy of normative estimates, people tend to misperceive the actual norms for others’ attitudes towards and engagement in health-related behaviors (i.e., social norms theory [18]). Specifically, people tend to overestimate the extent that others engage in health-risk behaviors (e.g., heavy alcohol use [25]) and underestimate the extent that others engage in preventive or health-enhancing behaviors (e.g., using mosquito nets to prevent malaria [26]). Related to the COVID-19 pandemic, researchers have found that young adults tend to underestimate how well their peers adhere to the physical distancing guidelines [27]. Although normative misperceptions can facilitate increased engagement in health-risk behavior, correcting such misperceptions has been an effective prevention/intervention strategy that can motivate individuals to engage in healthier behavior. For example, highlighting that most students do not engage in as much heavy alcohol use as people think can motivate college students to reduce their own drinking levels [28]. One proven norms-based intervention strategy is personalized normative feedback, which corrects individuals’ inaccurate normative estimates by showing individually tailored feedback contrasting (a) personal behavior, (b) estimates of others’ behaviors, and (c) others’ actual behaviors [29]. On a larger scale, social norms also can be leveraged within marketing campaigns that entail publicly highlighting the actual norms for a behavior, which can shift perceptions and promote healthier behavior [e.g., 30]. Although norms-based strategies have been successfully employed across numerous domains of prevention science, these strategies are only thought to be effective when (a) peoples’ estimates of social norms for a given behavior tend to be inaccurate, and (b) data show that the actual norm is a favorable comparison, relevant to most peoples’ estimates. Norms-based strategies may be able to increase vaccination intentions and attitudes, but a key preliminary step entails examining the extent that college students underestimate peers’ intentions (i.e., descriptive norms) and attitudes (i.e., injunctive norms) regarding COVID vaccination, as well as demonstrating proof-of-concept that estimated social norms are associated with individuals’ own vaccine intentions and attitudes.
1.3. Perceived barriers and reasons for COVID vaccine hesitancy
Although the development and initial evidence supporting the efficacy of COVID vaccines is encouraging, this has been a polarizing topic and there are many fears and misperceptions that may act as barriers to high vaccine coverage [31]. Given the rapid pace of development, many U.S. adults have reported concerns for the efficacy and safety of a COVID vaccine [17], though a recent in-depth review concluded that there is no evidence indicating the vaccines currently in development are linked to safety concerns or side effects, such as vaccine-associated enhanced disease [32]. Nevertheless, understanding college students’ perceived barriers and reasons for vaccine hesitancy – even among only a small portion of this population – is critical to achieving sufficient vaccine coverage to facilitate herd immunity [31].
1.4. Current study
Given the low-adherence to physical distancing guidelines among young adults [12], and high incidence rates of COVID-19 on college campuses [15], vaccination is particularly critical for college students. The current study examined college students’ intentions and perceived importance of getting a COVID vaccination (i.e., attitudes), as well as college students’ estimates of descriptive and injunctive norms for the behaviors and attitudes of typical young adults. These estimates were first contrasted to behaviors, attitudes, and norms pertaining to the influenza vaccine. On one hand, the influenza vaccine is generally perceived as safe and effective among U.S. adults [33], while many are still skeptical of the COVID vaccines [17]. Alternatively, given the severity of the current COVID-19 pandemic it is possible that college students would have greater intentions to receive a COVID vaccine than an influenza vaccine and would view COVID vaccination as more important than influenza vaccination.
The second aim of this study was to contrast college students’ own vaccination intentions and attitudes to their estimates of descriptive and injunctive norms for typical young adults. Given the tendency to underestimate peers’ engagement in healthful behaviors [18], we hypothesized that more college students would report intentions to receive vaccinations, relative to their estimates of descriptive norms for typical young adults. Similarly, we hypothesized that the college students in our sample would report greater perceived importance of COVID and influenza vaccines, relative to estimated injunctive norms for typical students.
The third aim entailed estimating the extent that vaccination intentions and perceived importance were associated with participants’ estimates of descriptive and injunctive norms. Despite being a novel question, previous studies have found positive associations between social norms and college students’ intentions to receive Human Papillomavirus (HPV) [23] and influenza vaccines [24]. We therefore hypothesized that vaccination intentions and perceived importance would be associated with both descriptive and injunctive norms.
The final aim of the current study entailed exploring potential barriers and reasons that college students may be hesitant to receive a COVID vaccination. Participants indicated barriers and/or reasons they may not get a COVID vaccination, and percentages were calculated to identify the most salient factors impacting college students’ likelihood of receiving a vaccination.
2. Method
2.1. Participants and procedures
Randomly selected from the university registrar list, 1400 undergraduate students from a large public university in the northwest United States were e-mailed an invitation to complete a brief online survey on student health behaviors. The survey was open from November 2nd through November 13th of 2020, at which point no COVID vaccine had been publicly released but public health experts and media sources had begun highlighting that a public release was imminent [6]. Remuneration entailed a $10 e-gift card, and all procedures were approved by the Institutional Review Board at the author’s university.
2.2. Measures
To assess vaccination intentions, two yes/no items were asked: “When available, do you intend to get a COVID vaccination/shot?” and “Have you received, or do you intend to get a flu vaccine/shot for the 2020/2021 flu season (i.e., influenza)?” Perceived importance of COVID and influenza vaccines were assessed on a 7-point scale ranging from 1 = Not at all important to 7 = Extremely important: “How important do you think it is for young adults to get a [COVID]/[flu] vaccination/shot?”
Estimated descriptive norms for typical young adults was assessed on a scale from 0% to 100%: “Considering typical young adults in America, what percentage do you think will get a [COVID]/[flu] vaccination/shot?” Finally, estimated injunctive norms were assessed on the same 7-point scale as participants’ own perceived importance: “In your estimation, how important do typical young adults think it is to get a [COVID]/[flu] vaccination/shot?”
To explore potential barriers and reasons that young adults may be hesitant to get a COVID vaccine, we adapted a list of items from Fisher and colleagues [17]. The full list of barriers and reasons for hesitancy is shown in Table 3. Participants were asked to check-all-that-apply, but could instead indicate that they had no concerns about receiving a COVID vaccine, which was an exclusive response option.
Table 3.
Barriers and reasons for COVID vaccine hesitancy.
| Stem: Below are potential reasons why a young adult may not get a COVID-19 vaccination/shot. Please select all that apply to you: |
% Endorsed |
|
|---|---|---|
| Full sample | Those who do not intend to get a COVID vaccine | |
|
59.51% | 85.19% |
|
12.52% | 25.93% |
|
10.67% | 11.11% |
|
16.38% | 24.07% |
|
2.78% | 1.85% |
|
22.72% | 29.63% |
|
49.61% | 68.52% |
|
24.11% | 3.70% |
Note:N = 647. 1. Item 8 was an exclusive response option; if item 8 was endorsed, none of the other concerns could be endorsed.
2.3. Analyses
Paired-samples t-tests were used to test Aim 1, contrasting students’ intentions, perceived importance, and estimated norms for COVID vaccination to those pertaining to influenza vaccination. For Aim 2 a one-sample t-test was used to compare participants’ estimated descriptive norms for peers’ vaccine uptake to the sample mean values for the percentage of participants who intend to receive the respective vaccines. Aim 2 also entailed a paired-samples t-test to contrast self-reported vaccine attitudes to estimated injunctive norms. To facilitate interpretation, these contrasts were displayed graphically using bar plots with corresponding 95% confidence intervals.
Multiple regression models were fit to examine associations between vaccine intentions/attitudes and estimates of peers’ descriptive and injunctive norms, controlling for age and sex (Aim 3). Norms variables corresponded specifically to the vaccine being examined in the respective models (e.g., in the model examining COVID vaccination intentions, norms variables referred to estimates of peers’ intentions/attitudes regarding COVID vaccination). Whereas perceived importance of COVID/influenza vaccines were continuous outcome variables, intentions to get a COVID or influenza vaccine were dichotomous outcome variables and, as such, these models entailed using logistic regression to estimate adjusted odds ratios.
To accomplish the final aim of exploring potential barriers and reasons for COVID vaccine hesitancy, we calculated the proportion of the sample that endorsed each of the potential barriers/reasons. Proportions were displayed as percentages to facilitate interpretation. Reasons for vaccine hesitancy were examined both for the full sample as well as for those participants who specifically indicated that they did not intend to get a COVID vaccine.
3. Results
Complete survey responses were received from 647 students (46.21% response rate). The sample comprised 64.78% women (M age = 19.77, SD = 1.35) and the demographics approximately matched the available data published on the university website. Most participants were either Caucasian (43.10%) or Asian/Asian American (44.65%), 97.21% were fulltime students, 16.38% were affiliated with a Greek organization, and 43.43% reported living at home with their parents during the COVID-19 pandemic. Participants were approximately evenly distributed across undergraduate class-levels: 24.42% first-year, 23.96% second-year, 27.36% third-year, 20.24% fourth-year, and 4% reported being fifth-year or higher.
3.1. Aim 1: Contrasting COVID and influenza vaccine intentions, attitudes, and estimated norms
Descriptive statistics and bivariate correlation estimates are displayed in Table 1 . In the current sample of college students, 91.64% reported intentions to get a COVID vaccine, which was markedly higher than the percent of participants who reported that they got or will get an influenza vaccine this year (i.e., 76.04%; t = 7.79, p<.001). Similarly, college students perceived COVID vaccination to be of greater importance than influenza vaccination (t = 10.14, p<.001), though on average, the sample viewed both as being of high importance. Pertaining to estimates of descriptive norms, participants thought that peers would be more likely to get a COVID vaccine than an influenza vaccine (t = 16.67, p<.001). This pattern held for injunctive norms: Participants estimated that peers perceive COVID vaccination as being more important than influenza vaccination (t = 20.49, p<.001).
Table 1.
Bivariate correlations and descriptive statistics pertaining to the COVID vaccine and flu vaccine. N = 647.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| COVID Vaccine | ||||||||
| 1. Intentions to get the COVID Vaccine (0 = No, 1 = Yes) | ||||||||
| 2. Perceived Importance of COVID Vaccine | 0.60** | |||||||
|
3. Descriptive Norms for Typical Young Adults (Estimated % that will get the COVID Vaccine) |
0.33** | 0.40** | ||||||
|
4. Injunctive Norms for Typical Young Adults (Estimate of peers’ attitudes toward COVID Vaccine) |
0.26** | 0.39** | 0.62** | |||||
| Influenza Vaccine | ||||||||
| 5. Got or Plan to get the Flu Vaccine (0 = No, 1 = Yes) | 0.17** | 0.21** | 0.02 | -0.01 | ||||
| 6. Perceived Importance of Flu Vaccine | 0.29** | 0.39** | 0.06 | 0.04 | 0.58** | |||
|
7. Descriptive Norms for Typical Young Adults (Estimated % that will get the Flu Vaccine) |
0.01 | 0.05 | 0.22** | 0.09* | 0.16** | 0.29** | ||
|
8. Injunctive Norms for Typical Young Adults (Estimate of peers’ attitudes toward Flu Vaccine) |
0.10* | 0.09* | 0.14** | 0.24** | 0.18** | 0.37** | 0.51** | |
| Mean | 0.92 | 6.38 | 68.18 | 5.42 | 0.76 | 5.63 | 51.01 | 4.07 |
| Standard Deviation | 0.28 | 1.15 | 19.35 | 1.19 | 0.43 | 1.48 | 17.65 | 1.17 |
| Possible Response Range | 0 – 1 a | 1 – 7b | 0 – 100c | 1 – 7b | 0 – 1 a | 1 – 7b | 0 – 100c | 1 – 7b |
Note: The variable numbers across the top of the table correspond to the variables listed in the first column. a. 0 = No, 1 = Yes. b. 1 = Not at all important, 7 = Extremely important.c. Estimated percentages ranged from 0% to 100%. *p < .05, **p < .01.
3.2. Aim 2: Contrasting self-reported vaccine intentions/attitudes to estimated peer norms
Contrasts between self-reported intentions/attitudes and estimated norms for typical young adults are displayed graphically in Fig. 1 . Pertaining to descriptive norms, a greater proportion of participants self-reported intentions to receive a COVID vaccine (i.e., 91.64%), relative to the samples’ average estimate of the percentage of peers that would get a COVID vaccine (i.e., 68.18%; t = −30.82, p < .001). Similarly, a greater proportion of the sample reported that they got or will get an influenza vaccine (i.e., 76.04%), relative to estimated descriptive norms for peers (i.e., 51.01; t = −36.08, p<.001). Similar patterns emerged for perceived importance of COVID and influenza vaccinations. Regarding a COVID vaccine, participants reported higher perceived importance, on average, relative to estimates of how important typical young adults think this vaccine is (i.e., injunctive norms; t = 14.82, p<.001). This was also the case for perceived importance of an influenza vaccine (t = 20.95, p<.001).
Fig. 1.
Bar plots comparing (A) normative perceptions for typical young adults, and (C) self-reported vaccine-related behaviors and attitudes. *p < .01, **p < .001.
3.3. Aim 3: Associations between vaccine intentions/attitudes and estimated peer norms
Results from regression models examining vaccination intentions and perceived importance are displayed in Table 2 . Notably, across all models, neither age nor birth sex were associated with intentions or perceived importance of COVID and influenza vaccines.
Table 2.
Regression models predicting COVID and influenza vaccine intentions and perceived importance for young adults to receive these vaccinations.
|
Intend to get COVID vaccine (0 = No, 1 = Yes) |
Perceived importance of COVID vaccine |
Got or plan to get flu vaccine (0 = No, 1 = Yes) |
Perceived importance of flu vaccine |
|||||
|---|---|---|---|---|---|---|---|---|
| Adj. OR [95% CI] | p-value | b (SE) | p-value | Adj. OR [95% CI] | p-value | b (SE) | p-value | |
| STEP 1 | ||||||||
| Age | 0.93 [0.74, 1.16] | 0.494 | 0.04 (0.03) | 0.202 | 0.91 [0.80, 1.04] | 0.177 | 0.01 (0.04) | 0.832 |
| Sex (0 = Men, 1 = Women) | 0.83 [0.59, 1.60] | 0.593 | 0.03 (0.09) | 0.685 | 1.34 [0.91, 1.95] | 0.135 | 0.15 (0.11) | 0.184 |
| Estimated Descriptive Norms | 1.05 [1.03, 1.07] | <0.001 | 0.02 (0.00) | <0.001 | 1.02 [1.01, 1.03] | 0.047 | 0.01 (0.00) | 0.002 |
| Estimated Injunctive Norms | 1.27 [0.96, 1.70] | 0.099 | 0.22 (0.04) | <0.001 | 1.29 [1.07, 1.56] | 0.008 | 0.39 (0.05) | <0.001 |
| R2 = 0.23 | R2 = 0.19 | R2 = 0.07 | R2 = 0.15 | |||||
Note: Descriptive norms are participants’ estimates of the percentage of young adults that will get the COVID/influenza vaccine. Injunctive norms are participants’ estimates of how important young adults think the COVID/influenza vaccines are. Norms variables refer to the specific vaccine that is in focus for each model (e.g., in the model predicting intentions to get the COVID vaccine, norms variables refer to estimates pertaining to the COVID vaccine).
Estimated descriptive norms regarding the percentage of typical young adults that will get a COVID vaccine were positively associated with participants’ own intentions and perceived importance of getting a COVID vaccine. Notably, every 1% increase in estimated descriptive norms was associated with 1.05 times greater odds of intending to get a COVID vaccine. Estimated injunctive norms regarding how important typical young adults think COVID vaccination is was also positively associated with participants’ perceived importance of getting a COVID vaccine but was not significantly associated with vaccination intentions.
As it pertains to influenza vaccination, intentions and perceived importance were both significantly associated with estimated descriptive and injunctive norms for typical young adults.
3.4. Aim 4: Exploring barriers and reasons for COVID vaccine hesitancy
Participants indicated which barriers and potential reasons for not getting a COVID vaccine applied to them (shown in Table 3). Nearly 60% of the full sample and over 85% of those not intending to get a COVID vaccine indicated that they were afraid/nervous about unknown side effects. Similarly, nearly 50% of the full sample and almost 70% of those not intending to get a COVID vaccine indicated that they did not think a COVID vaccine would be sufficiently tested before being made available. Pertaining to the full sample, approximately 23% indicated being afraid a COVID vaccine could give them COVID or make them sick, over 16% indicated that they do not have sufficient health insurance to afford a vaccine, and 12.52% did not think that a vaccine would work. These percentages were slightly higher among those not intending to get a COVID vaccine, with approximately one-in-four indicating they did not think a COVID vaccine would work and/or indicating that they did not think they would be able to financially afford a vaccine. Just over 10% of the full sample noted a fear of needles/shots as a potential barrier, and approximately 3% of students felt that a COVID vaccine was incongruent with their religious beliefs. Nevertheless, nearly a quarter of the full current sample (24.11%) indicated that they had no concerns about getting a COVID vaccine, while only 3.70% of participants not intending to get a COVID vaccine noted that they had no concerns.
4. Discussion
As we approach a fully public release of COVID vaccines (beyond frontline workers and high-risk subgroups), the current study examined college students’ intentions, attitudes, perceived social norms, and hesitancies pertaining to vaccine uptake. Data from the current study (collected in November 2020) indicated that most college students intend to get a COVID vaccine when available (i.e., 91.64%), which was much higher than the percentage who reported getting or planning to get an influenza vaccine (i.e., 76.04%). This is encouraging preliminary evidence, given a strong theoretical link between intentions and behavior [34], but there is also evidence that vaccine intentions do not perfectly predict uptake [35]. Participants, on average, also felt that it was more important for young adults to get a COVID vaccine, relative to an influenza vaccine.
We also asked students to estimate the percentage of typical young adults that they thought would receive COVID and influenza vaccines (i.e., descriptive norms) and to estimate how important typical young adults thought these vaccines were for young adults (i.e., injunctive norms). Across these normative estimates, a clear pattern emerged in which the sample self-reported greater likelihood of getting COVID and influenza vaccinations relative to estimated descriptive norms, and also reported greater perceived importance of these vaccines relative to estimated injunctive norms. These patterns show early indication that students may underestimate descriptive and injunctive norms regarding peers’ intentions and attitudes toward vaccine uptake, though more representative data is needed to strengthen this conclusion.
Regression models revealed students’ vaccination intentions were associated with estimated descriptive norms: Those who thought a greater proportion of typical young adults would get vaccinated were more likely to report intentions to get COVID and influenza vaccines, respectively. Interestingly, estimated injunctive norms were not significantly associated with COVID vaccine intentions, which may indicate that social norms regrading peers’ vaccination behaviors (i.e., descriptive norms) may be a more salient influence than perceptions of peers’ vaccination attitudes (i.e., injunctive norms). Nevertheless, perceived importance of these vaccines was positively associated with estimates of both descriptive and injunctive norms, which highlights potential value in both types of social norms. Finally, we found that the most frequently endorsed reasons for COVID vaccine hesitancy were fears/concerns related to unknown side effects and fears that a vaccine could cause illness.
4.1. COVID vaccination compared to influenza vaccination
Assessing students’ intentions and attitudes regarding influenza vaccination enabled us to make direct comparisons to students’ intentions and attitudes towards COVID vaccines. Over the past ten years, the seasonal influenza virus in the U.S. has resulted in between 9 million – 45 million illnesses, between 140,000 – 810,000 hospitalizations, and between 12,000 – 61,000 deaths annually [36]. While these estimates demonstrate the severity of the influenza virus, there is concern that the SARS-CoV-2 virus may be even more devastating. Although direct ‘apples-to-apples’ comparisons may not yet be fully possible [37], meta-analytic evidence shows that hospitalization durations are significantly longer for COVID patients (i.e., 14 days) compared influenza patients (i.e., 6–7 days) and mortality rates are higher for COVID (i.e., 6.5%) compared to influenza (i.e., 6.0% for influenza type A and 3.0% for Type B) [38]. Given the acute burden of the COVID-19 pandemic, even beyond the direct health implications (e.g., government-enforced distancing protocols), it is intuitive that young adults would view the COVID vaccine as being relatively more important than the influenza vaccine. The salient effects on society and the global economy associated with the COVID-19 pandemic may also explain why more students in our sample reported intentions to get the COVID vaccine, relative to the influenza vaccine. Considering concerns regarding the efficacy and safety of a COVID vaccination [17], it is encouraging that over 90% of the students in our sample intend to get the vaccine. Furthermore, the fact that over 76% of students in our sample reported getting or intending to get the influenza vaccine is a major improvement over estimated rates from previous years that are only around 40% among college students [39], [40]. Additional research is needed, but one silver-lining of the COVID-19 pandemic may be increased intentions to receive annual influenza vaccination.
4.2. Applied implications
As behavioral scientists seek to develop strategies that can increase societal uptake of COVID vaccines, the findings from the current study indicate that norms-based approaches may be promising. We found that students may, on average, tend to underestimate their peers’ intentions and attitudes towards getting a COVID vaccine and, as such, norm-correcting strategies may be promising. Indeed, the results indicated significant associations between vaccination intentions and perceptions of social norms for typical young adults – highlighting the potential value of increasing young adults’ perceptions of how many young adults actually intend to get a COVID vaccine as well as how important most young adults think getting vaccinated is for young adults. Specifically, personalized normative feedback interventions could be a prudent strategy to correct normative misperceptions and could be used by university stakeholders to increase uptake and vaccine coverage on college campuses. The current findings should also be considered alongside existing evidence that norms-based approaches may effectively promote uptake of HPV vaccines among college-aged women [41], [42], improve attitudes and intentions to receive the influenza vaccine among healthcare workers [39], and increase Hepatitis B vaccine intentions among men who have sex with men [43]. Nevertheless, additional translational studies are needed to develop, test, and optimize norms-based intervention strategies specific to the circumstances surrounding the COVID-19 pandemic.
Although most students in our sample reported intentions to get a COVID vaccination, only a quarter of the sample indicated that they had no concerns about doing so. Most notably, students reported being concerned about the vaccine not being properly tested and potential unknown side effects. These concerns were particularly prevalent among those who did not intend to be vaccinated, highlighting a key point of focus for efforts to improve vaccine coverage. To increase confidence in available COVID vaccines, it may be helpful to show the depths of the clinical trial protocols and the evidence indicating that the vaccines under development are indeed safe [3]. Nearly a quarter of the sample indicated that they were concerned a COVID vaccine could make them sick, despite evidence against this concern [32]. Indeed, the scientific community has struggled to overcome widespread misinformation throughout the COVID-19 pandemic, but particularly as it pertains to COVID vaccines [44]. This is deeply concerning given that the World Health Organization listed vaccine hesitancy as a top-ten global health threat, even before the emergence of COVID-19 [45]. Nevertheless, apprehension may be warranted given that long-term effects and safety are not yet known. Behavioral interventions or campaigns to increase uptake should also be careful not to invalidate peoples’ concerns, which may yield defensive responses and actually decrease uptake [46]. One notable perceived barrier among those not intending to get a COVID vaccine is lack of health insurance or financial means to be vaccinated. Fortunately, COVID vaccines are being made available for free, regardless of health insurance (see details: https://www.cms.gov/covidvax-provider); however, these initiatives will only help increase vaccine coverage if this information reaches the general public. As a final implication, most participants – even those not intending to be vaccinated – believed that a COVID vaccination would work, so simply highlighting the efficacy statistics may not be enough to overcome vaccine hesitancy.
4.3. Limitations and future directions
Alongside of the timely implications of the current study, several limitations must be carefully considered. The estimates presented herein are not intended to reflect nationwide estimates of vaccination intentions or attitudes, but rather to generate proof-of-concept evidence from which to build upon. While we argue that high vaccine coverage among young adults will be critical to our overall efforts to combat COVID-19 [11], [14], the inferences drawn from the current results may not extend beyond undergraduate college students from the northwest United States. Indeed, those with higher educational attainment may be more likely to be accepting of vaccines [17]. A second related limitation is that our sample comprised mostly Caucasian and Asian/Asian-American students, whereas other minority groups have been hit especially hard by the COVID-19 pandemic [47] and may also be less accepting/trusting of vaccines [31]. So, although the current study provides proof-of-concept for the role of social norms on vaccination uptake, more in-depth research is needed to increase uptake within historically marginalized communities and higher-risk groups. The response rate (46.21%) was understandably low given the randomized online recruitment during a global pandemic, as has been the case with other COVID-related studies on this age group [22], but it has been shown that low response rates do not necessarily bias the results of survey-based research [48]. A third limitation to note is that we asked participants to estimate social norms for typical young adults, so direct comparisons with our sample to estimate the accuracy of normative estimates were not possible. Larger representative data is needed to estimate true and accurate norms. Relatedly, the measures used to assess COVID vaccine intentions, attitudes, and norms may have adequate face validity, but further psychometric validation is a prudent step for researchers seeking to identify antecedents/correlates of COVID vaccine uptake. Finally, it is important to consider the timing of this study given that COVID vaccine development has evolved rapidly, as has public perception of the COVID vaccines [3], [6], [8]. These data were collected in November of 2020 which was before a public release of any COVID vaccines, so we were limited to assessing participants’ vaccine intentions while future studies will be able to assess more objective indices of uptake. It is also plausible that people will become more assured that there are not harmful side effects as vaccination rollout continues throughout early 2021 and, as such, research on vaccine hesitancy should continue to be monitored throughout the pandemic. As the public continues to learn more about the efficacy and safety of COVID vaccines, it would be important to further examine the extent that perceived social norms relate to young adults’ intentions and attitude towards a COVID vaccine. It is also worth noting that data were collected during a time period in which many in the U.S. associated the ongoing vaccine development with partisan political agendas [49].
5. Conclusions
The development of an effective COVID vaccine is a key step towards curtailing the spread of the SARS-CoV-2 virus, but high vaccination coverage is needed to achieve herd immunity [10]. We first contrasted COVID vaccine intentions and attitudes to those pertaining to influenza vaccines and found that college students, on average, have greater intentions to get a COVID vaccine than an influenza vaccine and also perceive COVID vaccination as relatively more important than influenza vaccination. Nevertheless, intentions and perceived importance was quite high for both COVID and influenza vaccines. Then, building upon recent research by Reiter and colleagues [8] on public acceptability of the COVID vaccines, the current study examined estimates of social norms related to peers’ intentions and attitudes towards COVID vaccination as a theoretically important antecedent/correlate of young adults’ own vaccinations intentions and attitudes [18], [19]. We found proof-of-concept evidence: Young adults’ estimates of the percentage of typical young adults that will get a COVID vaccine (i.e., descriptive norms) and estimates of how important typical young adults think COVID vaccination is (i.e., injunctive norms) were both significantly associated with self-reported intentions and perceived importance of COVID vaccination. These significant associations highlight the potential value in developing and testing norms-based intervention strategies, such as personalized normative feedback, to improve uptake of COVID vaccines among young adults.
Funding
This research conducted with support of a training fellowship from the National Institute on Alcohol Abuse and Alcoholism (T32AA007455) and a small project grant from the Addictions, Drug, & Alcohol Institute at the University of Washington. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the University of Washington.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2021.03.018.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.CDC. Implementation of mitigation strategies for communities with local COVID-19 transmission. Atlanta, GA US Dep Heal Hum Serv CDC; 2020
- 2.Andone D., Maxouris C. The US hit a record 7-day average of new Covid-19 cases as hospitals are further strained. CNN Heal. 2020 December 5:https://www.cnn.com/2020/12/05/health/us-coronavir. [Google Scholar]
- 3.Graham B.B.S. Rapid COVID-19 vaccine development. Science (80-) 2020;368:945–946. doi: 10.1126/science.abb8923. [DOI] [PubMed] [Google Scholar]
- 4.WHO. Draft landscape of COVID-19 candidate vaccines. World Heal Organ Https//WwwWhoInt/Publications/m/Item/Draft-Landscape-of-Covid-19-Candidate-Vaccines 2020
- 5.CDC CDC’s COVID-19 vaccine rollout recommendations. Centers Dis Control Prev. 2021 [Google Scholar]
- 6.Iacobucci G. Covid-19: GPs are told to be ready to deliver vaccine from next month T. BMJ. 2020;371:4291. doi: 10.1136/bmj.m4291. [DOI] [PubMed] [Google Scholar]
- 7.Corey L., Mascola J.R., Fauci A.S., Collins F.S. A strategic approach to COVID-19 vaccine R&D. Science (80-) 2020;368:948–950. doi: 10.1126/science.abc5312. [DOI] [PubMed] [Google Scholar]
- 8.Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine. 2021;38:6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Head K.J., Kasting M.L., Sturm L.A., Hartsock J.A., Zimet G.D. A national survey assessing SARS-CoV-2 vaccination intentions: Implications for future public health communication sfforts. Sci Commun. 2020;42:698–723. doi: 10.1177/1075547020960463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anderson R.M., Vegvari C., Truscott J., Collyer B.S. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet. 2020;396:1614–1616. doi: 10.1016/s0140-6736(20)32318-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.CDC. Changing age distribution of the COVID-19 pandemic — United States, May-August 2020. Centers Dis Control Morb Mortal Wkly Rep 2020;69:1404–9. [DOI] [PMC free article] [PubMed]
- 12.Jørgensen F., Bor A., Petersen M.B. Compliance without fear: Predictors of protective behavior during the first wave of the COVID-19 pandemic. PsyArXiv. 2020 doi: 10.1111/bjhp.12519. https://psyarxiv.com/uzwgf/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhu T, Wang Y, Zhou S, Zhang N, Xia L. A comparative study of chest computed tomography features in young and older adults with Corona Virus Disease (COVID-19). J Thorac Imaging 2020:Ahead of Print. https://doi.org/10.1097/RTI.0000000000000513. [DOI] [PMC free article] [PubMed]
- 14.Farber S.E., Johnson J. New data shows young people need to take social distancing seriously: Younger people may be spreading the virus among themselves. ABC News. 2020 [Google Scholar]
- 15.Dickler J. Coronavirus cases on college campuses spike, linked to parties. CNBC Heal Sci. 2020 November 2:https://www.cnbc.com/2020/11/20/coronavirus-cases- [Google Scholar]
- 16.Fisher KA, Barile JP, Guerin RJ, Esschert KL Vanden, Jeffers A, Tian LH, et al. Factors associated with cloth face covering use among adults during the COVID-19 pandemic - United States, April and May 2020. Morb Mortal Wkly Rep 2020;69. [DOI] [PubMed]
- 17.Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: A survey of U.S. adults. Ann Intern Med 2020:Ahead of Print. https://doi.org/10.7326/M20-3569. [DOI] [PMC free article] [PubMed]
- 18.Berkowitz AD. The social norms approach: Theory, research and annotated bibliography. Higher Education Center for Alcohol and Other Drug Abuse and Violence Prevention. US Department of Education; 2004
- 19.Cialdini R.B., Reno R.R., Kallgren C.A. A focus theory of normative conduct: Recycling the concept of norms to reduce littering in public places. J Pers Soc Psychol. 1990;58:1015–1026. doi: 10.1037/0022-3514.58.6.1015. [DOI] [Google Scholar]
- 20.Litt D.M., Lewis M.A., Linkenbach J.W., Lande G. Normative misperceptions of peer seat belt use among high school students and their relationship to personal seat belt use. Traffic Inj Prev. 2014;15:748–752. doi: 10.1080/15389588.2013.868892.Normative. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Graupensperger S., Turrisi R.J., Jones D.E., Evans M.B. Longitudinal associations between perceptions of peer group drinking norms and students’ alcohol use frequency within college sport teams. Alcohol Clin Exp Res. 2020 doi: 10.1111/acer.14270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Graupensperger S, Jaffe AE, Fleming CB, Kilmer JR, Lee CM, Larimer ME. Changes in college student alcohol use during the COVID-19 pandemic: Are perceived drinking norms still relevant? Emerg Adulthood 2021:Ahead of Print. [DOI] [PMC free article] [PubMed]
- 23.Stout M.E., Christy S.M., Winger J.G., Vadaparampil S.T., Mosher C.E. Self-efficacy and HPV vaccine attitudes mediate the relationship between social norms and intentions to receive the HPV vaccine among college students. J Community Health. 2020;45:1187–1195. doi: 10.1007/s10900-020-00837-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Quinn S.C., Hilyard K.M., Jamison A.M., An J., Hancock G.R., Musa D., et al. The influence of social norms on flu vaccination among African American and White adults. Health Educ Res. 2017;32:473–486. doi: 10.1093/her/cyx070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cox MJ, DiBello AM, Meisel MK, Ott MQ, Kenney SR, Clark MA, et al. Do misperceptions of peer drinking influence personal drinking behavior? Results from a complete social network of first-year college students. Psychol Addict Behav 2019:Online First. https://doi.org/10.1037/adb0000455. [DOI] [PMC free article] [PubMed]
- 26.Perkins J.M., Krezanoski P., Takada S., Kakuhikire B., Batwala V., Tsai A.C., et al. Social norms, misperceptions, and mosquito net use: A population-based, cross-sectional study in rural Uganda. Malar J. 2019;18:189–202. doi: 10.1186/s12936-019-2798-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Graupensperger S, Lee C, Larimer M. Young adults underestimate how well peers adhere to COVID-19 preventive behavioral guidelines. J Prim Prev 2021:Ahead of Print. [DOI] [PMC free article] [PubMed]
- 28.Labrie J.W., Lewis M.A., Atkins D.C., Neighbors C., Zheng C., Kenney S.R., et al. RCT of web-based personalized normative feedback for college drinking prevention: Are typical student norms good enough? J Consult Clin Psychol. 2013;81:1074–1086. doi: 10.1037/a0034087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dotson K.B., Dunn M.E., Bowers C.A. Stand-alone personalized normative feedback for college student drinkers: A meta-analytic review, 2004 to 2014. PLoS ONE. 2015;10:1–17. doi: 10.1371/journal.pone.0139518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mattern JL, Neighbors C. Social norms campaigns: Examining the relationship between changes in perceived norms and changes in drinking levels 2003:489–93. [DOI] [PubMed]
- 31.Malik A.A., Mcfadden S.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26 doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haynes B.F., Corey L., Fernandes P., Gilbert P.B., Hotez P.J., Rao S., et al. Prospects for a safe COVID-19 vaccine. Sci Transl Med. 2020:1–13. doi: 10.1126/scitranslmed.abe0948. [DOI] [PubMed] [Google Scholar]
- 33.Lutz C.S., Fink R.V., Cloud A.J., Stevenson J., Kim D., Fiebelkorn A.P. Factors associated with perceptions of influenza vaccine safety and effectiveness among adults, United States, 2017–2018. Vaccine. 2020;38:1393–1401. doi: 10.1016/j.vaccine.2019.12.004. [DOI] [PubMed] [Google Scholar]
- 34.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 35.Ye L., Fang T., Cui J., Zhu G., Ma R., Sun Y. The intentions to get vaccinated against influenza and actual vaccine uptake among diabetic patients in Ningbo, China: Identifying motivators and barriers. Hum Vaccin Immunother. 2020:1–13. doi: 10.1080/21645515.2020.1761201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.CDC. Disease burden of influenza. Centers Dis Control 2020:https://www.cdc.gov/flu/about/burden/index.html
- 37.Faust J.S., del Rio C. Assessment of deaths from COVID-19 and from seasonal influenza. JAMA Intern Med. 2020;180:1045–1046. doi: 10.1136/bmj.331.7529.1412. [DOI] [PubMed] [Google Scholar]
- 38.Pormohammad A., Ghorbani S., Khatami A., Hossein M., Ehsan R., Mohammad A., et al. Comparison of influenza type A and B with COVID - 19: A global systematic review and meta-analysis on clinical, laboratory and radiographic findings. Rev Med Virol. 2020 doi: 10.1002/rmv.2179. e2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ng T.W.Y., Cowling B.J., Chi H., Ip D.K.M., Liao Q. Testing an integrative theory of health behavioural change for predicting seasonal influenza vaccination uptake among healthcare workers. Vaccine. 2020;38:690–698. doi: 10.1016/j.vaccine.2019.10.041. [DOI] [PubMed] [Google Scholar]
- 40.Rogers C.J., Bahr K.O., Benjamin S.M. Attitudes and barriers associated with seasonal influenza vaccination uptake among public health students; a cross- sectional study. BMC Public Health. 2018;18:1131. doi: 10.1186/s12889-018-6041-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Allen J.D., Mohllajee A.P., Shelton R.C., Othus M.K.D., Fontenot H.B., Hanna R. Stage of adoption of the human papillomavirus vaccine among college women. Prev Med (Baltim) 2009;48:420–425. doi: 10.1016/j.ypmed.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 42.Hopfer S., Clippard J.R. College women’s HPV vaccine decision narratives. Qual Health Res. 2011;21:262–277. doi: 10.1177/1049732310383868. [DOI] [PubMed] [Google Scholar]
- 43.Vet R., de Wit J.B.F., Das E. The efficacy of social role models to increase motivation to obtain vaccination against hepatitis B among men who have sex with men. Health Educ Res. 2011;26:192–200. doi: 10.1093/her/cyq074. [DOI] [PubMed] [Google Scholar]
- 44.Cornwall W. Officials gird for a war on vaccine misinformation. Science (80-) 2020;369:14–5. https://doi.org/10.1126/science.369.6499.14. [DOI] [PubMed]
- 45.WHO. Ten threats to global health in 2019. World Heal Organ Https//WwwWhoInt/News-Room/Spotlight/Ten-Threats-to-Global-Health-in-2019; 2019
- 46.Omer S.B., Poland C.M., Chamberlain A.T. In: Vaccinations. Poland G., Whitaker J.A., editors. Elsevier; St. Louis, MO: 2018. Interpersonal communication approaches to increase adult vaccine acceptance; pp. 25–34. [Google Scholar]
- 47.Yancy C.W. COVID-19 and African Americans. JAMA. 2020;323:1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 48.Fosnacht K., Howe E., Peck L.K. How important are high response rates for college surveys? Rev High Educ. 2017;40:245–265. [Google Scholar]
- 49.Fiddler DP. Vaccine nationalism’s politics. Science (80-) 2020;369:749. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.