Abstract
BACKGROUND AND PURPOSE:
Various lines of evidence implicate cerebral involvement beyond the motor cortex in ALS, including the cingulate gyrus and the thalamus. The purpose of this study was to assess neurodegeneration in these regions in vivo by using MRSI.
MATERIALS AND METHODS:
Fourteen patients with ALS and 14 healthy controls underwent MRSI by using a coronal acquisition scheme. The NAA/Cho ratio was quantified in the MCC, thalamus, and motor cortex (PCG).
RESULTS:
NAA/Cho was reduced in the MCC in patients with ALS compared with the controls (P = .0004). There was no difference in NAA/Cho in the thalamus (P = .59). We also found a strong correlation of NAA/Cho among the PCG, MCC, and the thalamus in controls, which was absent in patients with ALS.
CONCLUSIONS:
Neurodegeneration beyond the motor cortex is present in the MCC in ALS. The significant correlation of NAA/Cho among the PCG, MCC, and the thalamus in healthy subjects likely reflects the neuronal connectivity among these regions. The loss of these relationships in patients with ALS suggests that such connectivity is not responsible for the pattern of degeneration in these regions.
ALS is a progressive neurodegenerative disorder involving primarily the motor neurons of the cerebral cortex (UMN), brain stem, and spinal cord (LMN). However, cognitive impairment is present in upwards of 50% of patients, with a significant proportion meeting criteria for dementia,1,2 and there is considerable pathologic and imaging evidence for degeneration beyond the motor system.3–5
The cingulate cortex, the largest part of the limbic system, is divided into the anterior cingulate cortex (Brodmann areas 25, 24, and 32) and the posterior cingulate cortex (Brodmann areas 23 and 31). The anterior cingulate has been further recognized as having 2 divisions: the perigenual cortex and the MCC. The MCC is the posterior parts of areas 24 and 32. This differentiation is based on histology, function, and neuronal connections. Histologically, the MCC has a very dense layer, (Va), which contains small and large pyramidal cells, and a large density of neurofilament-positive layer, (Vb), neurons.
In terms of connections, the perigenual cortex receives input from the thalamic nuclei and amygdala. The MCC receives extensive thalamic afferents, input from the inferior parietal lobes, and less input from the amygdala. The MCC contains the CMA, which project to the motor cortex and spinal cord. It is involved in response selection and reorganizing behavior for changing rewards, while the perigenual cortex has been implicated in emotional behavior, cognition, and autonomic regulation.6 The extensive fibers from the thalamus to the MCC and the consequent ability of MCC to sample more thalamic input than any other cortical area may be a crucial factor in regard to its role in selecting appropriate motor responses.
Given the crucial motor connections and functions of the MCC and the presence of widespread thalamocortical and thalamocingulate projections, we sought to determine the in vivo neurochemical changes in these regions reflective of neuronal degeneration. Thus, we hypothesized that the spectroscopic marker of neuronal integrity, NAA, is reduced in these regions.
Materials and Methods
Subjects were recruited from the ALS Clinic at the University of Alberta. The imaging features of the corticospinal tract in most of these patients have been reported previously.7,8 Fourteen patients with ALS and 14 controls were studied. Two patients had definite ALS, and 12 patients had probable ALS by the El Escorial criteria.9 The mean age of the patient group was 55.9 ± 15.4 years and that of the control group was 53.7 ± 12.4 years. The male/female ratio was 7:7 in patients and 8:6 in the control group. The mean duration of symptoms was 22 ± 17 months. The mean ALSFRS (a measure of general disability; range, 0–40) was 30 ± 6. The rate of disease progression for each patient was estimated as rate = (40-ALSFRS)/symptom duration.10 The study was approved by the Health Research Ethics Board of the University of Alberta. Informed consent was obtained from all subjects.
Imaging
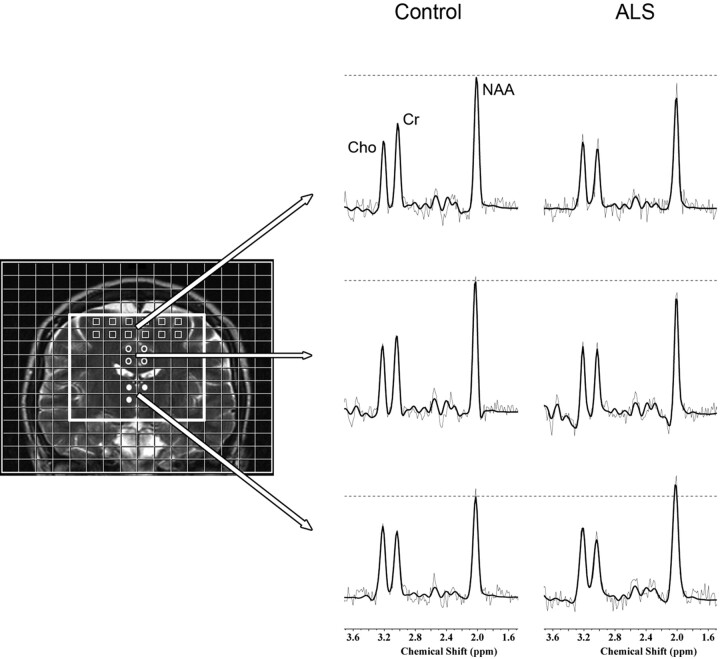
Imaging was performed on a 1.5T MR imaging system (Magnetom Sonata; Siemens, Erlangen, Germany).6 In brief, anatomic locators were followed by a 2D spin-echo MRSI sequence (TR = 1500, TE = 135 ms, n = 4, 12 × 12 phase encodes interpolated to a 16 × 16 matrix, FOV = 160 × 160 mm). The nominal voxel size was 1 × 1 × 1.5 cm and 1.5 cm3 after k-space filtering. The slab was angulated in a coronal plane to enclose the corticospinal tract (Fig 1). This volume of interest intersected the motor cortex, MCC, and thalamus.
Fig 1.
Spectroscopic imaging. A coronal MR image is shown on the left demonstrating placement of the volume of interest (thick white border). Voxels identified for analysis included those in the PCG (squares), MCC (open circles), and thalamus (closed circles). A representative spectrum from each of these regions is presented on the right from a control subject and a patient with ALS.
LCModel (Stephen Provencher, Oakville, Ontario, Canada) was used for off-line processing of the spectroscopic data and quantification of intravoxel metabolite peak areas.11 NAA was expressed as an NAA/Cho ratio. In this regard, Cho was chosen as an internal reference metabolite because previous spectroscopic studies have revealed larger effect sizes and accuracy profiles for NAA/Cho compared with NAA/Cr.8,12–15 Voxels were assigned to the MCC, thalamus, and motor cortex (PCG) (Fig 1) . Metabolite ratios for each region (ie, MCC, thalamus, and PCG) were calculated by determining the average ratio for all voxels assigned to that region.
Statistics
Group differences in NAA/Cho within regions were determined with 2-tailed t tests, and relationships were determined by calculation of Pearson correlation coefficients. Statistical significance was set at a 2-tailed P < .05.
Results
In control subjects, NAA/Cho was highest in the PCG (2.00 ± 0.23) and lowest in the thalamus (1.45 ± 0.46). Patients had reduced NAA/Cho compared with controls in the PCG (1.66 ± 0.14 versus 2.00 ± 0.23, P = .0001) and MCC (1.51 ± 0.13 versus 1.77 ± 0.18, P = .0004), but not in the thalamus (1.41 ± 0.21 versus 1.45 ± 0.46, P = .59). Clinical correlations existed between the rate of disease progression and PCG NAA/Cho (P = .007, r = −0.68) and between the finger-tapping rate and MCC NAA/Cho (P = .02, r = −0.45). NAA/Cho was significantly correlated among regions in healthy subjects (Fig 2). These correlations were not present in patients.
Fig 2.
Loss of neurochemical associations among regions in patients with ALS. Strong correlations of NAA/Cho are present among regions in healthy control subjects (open circles); whereas, in patients (closed circles, regression coefficients not displayed) significant correlations are not observed.
Discussion
There is substantial clinical, pathologic, and radiologic evidence for the involvement of nonmotor areas in ALS.2,16–21 Previous MRSI studies in ALS have demonstrated impaired neuronal integrity in the motor cortex, frontal lobes, and brain stem, with the findings of reduced NAA and NAA normalized to Cr or Cho (NAA/Cr, NAA/Cho).22–25 The objective of this study was to assess in vivo neurochemical changes in the MCC and thalamus, 2 regions not previously studied with MRSI but implicated either by pathologic or imaging studies to be involved in ALS. Furthermore, the MCC has extensive motor connections and a large number of pyramidal neurons. The thalamus, though primarily an organ for sensory integration, also has widespread motor connections. It provides specific connections from the basal ganglia and cerebellum to cortical motor areas, and the thalamocortical system regulates the initiation and execution of movement.26 The reduced NAA/Cho in the PCG in the bulk of these patients was reported previously8 and is consistent with numerous reports of reduced NAA in the motor cortex in ALS. The novel observations reported herein are those with respect to the MCC and thalamus: NAA/Cho was reduced 14% in the MCC and was normal in the thalamus.
Reduced MCC NAA/Cho is consistent with postmortem studies of ALS demonstrating neurodegeneration of the cingulate.27,28 Reduced cingulate neuronal integrity has been corroborated by several radiologic modalities. Reduced blood flow to the cingulate cortex in ALS has been demonstrated by PET.29 Impaired activation of the cingulate cortex was demonstrated by using a letter fluency paradigm with fMRI in patients with ALS.30 These studies reported findings predominantly in the anterior cingulate (but not restricted to the perigenual region), along with changes in other prefrontal regions and the temporal lobe. A recent study of arterial spin-labeling MR imaging in patients with ALS found that the severity of upper motor neuron involvement as measured by finger tapping correlated with perfusion of the middle cingulate gyrus.31 We are aware of a single MRSI study of the anterior cingulate in ALS; it showed reduced NAA/Cr specifically in those with bulbar onset disease.32
Convincing evidence for thalamic involvement in ALS has not been forthcoming from routine postmortem or standard anatomic imaging studies. There have been very few postmortem studies that have specifically examined the thalamus. Ince et al16 reported degeneration of the thalamus, noting the presence of ubiquinated neuronal inclusion bodies and hyaline conglomerates, similar to the involvement of other parts of the nervous system affected by ALS. Smith27 reported the degeneration of the nerve fibers that pass into and out of the thalamus. Voxel-based morphometry has shown gray matter atrophy involving the thalamus in patients with both ALS and ALS/FTD.33–35 Functional imaging studies support involvement of the thalamus, with the finding of reduced activation of the thalamus on PET studies by using cognitive paradigms in patients with ALS29 and hypometabolism with FDG-PET in patients with motor neuron disease and FTD.36 Microglial activation in the thalamus has been demonstrated by using 11C(R)-PK11195–labeled PET.37 In contrast, an 11C-labeled flumazenil (a GABAA receptor ligand) PET study did not reveal thalamic abnormalities in the face of diffusely reduced GABAA receptor attenuation in frontotemporal cortical regions.38 Notably, convincing signs of thalamic degeneration were not observed in the SOD1 transgenic mouse model of ALS.39
TDP-43 has been identified as an important pathologic protein in some forms of FTLD and sporadic ALS.40 The presence of TDP-43 in both implicates common pathophysiologic mechanisms between these disorders that share clinical and pathologic features. The spatial distribution of TDP-43 was reported to include the anterior cingulate and the thalamus in 1 study.41 The widespread finding of TDP-43 outside the pyramidal motor system substantiates the neuroimaging abnormalities found in these regions and the behavioral and cognitive impairments present in some patients with ALS.
Several reasons may underlie the finding of thalamic sparing in our study. MRSI may not be sensitive enough to detect in vivo neurochemical alterations. Because imaging evidence of thalamic involvement comes mainly from functional studies, these functional alterations may precede neurochemical or structural changes. Presumably, the presence of thalamic TDP-43 is not sufficient to produce neurochemical or structural changes that can be detected with the MRSI technique used in this study.
In healthy subjects, a strong linear relationship of NAA/Cho, and thus probably neuronal density, was observed among the thalamic, cingulate, and motor cortex regions. The biologic significance of this is uncertain; however, it may be related to inter-regional neuronal connectivity. Previous studies with tracer injections, fMRI, and DTI have demonstrated a well-defined connectivity among the thalamus, motor areas, and the cingulate cortex.42–44 The CMA in the MCC project directly to the motor cortex and spinal cord in a somatotopic fashion.45–47 The motor information derived from the CMA is separately or simultaneously processed within the basal ganglia and returned to the frontal cortex by way of the thalamus. In ALS, the inter-regional relationships that were observed in controls appear to be lost. The simplest explanation for this is the concomitant degeneration of the PCG and MCC, which is due to a process of degeneration that is not related between these regions with respect to magnitude and rate. If degeneration was dependent on neuronal connections, then one may expect retention of a correlation. For example, this could be envisioned if degeneration began in the PCG with deleterious “downstream” effects (such as excitotoxicity) on neurons in other regions. Such inter-regionally dependent degeneration would presumably proceed at a common rate, and an NAA/Cho relationship would be preserved. This may also reflect the selective vulnerability of neurons in the motor areas, like the giant Betz cells and their axons, along with astrocytic gliosis, with less severe involvement of other neurons in the cingulate cortex and the thalamus, and may support the notion that certain areas may be affected earlier than others.
An inverse association of MCC NAA/Cho with finger-tapping rate (a measure of the functioning of UMN) was observed in patients; we are unable to explain this finding because one would have expected a positive association.
There are limitations to this study. Neuropsychological assessments were not performed in these subjects, which would have been useful to assess associations between cingulate degeneration and cognitive impairment, given that prior studies suggest that cingulate dysfunction is related to verbal fluency deficits.30 Neurochemical ratios were quantified rather than absolute metabolite concentrations. Although elevated Cho could conceptually contribute to the observed decreased NAA/Cho ratio, this is unlikely a major factor. Previous studies measuring absolute metabolites in ALS have inconsistently found increased Cho, yet all additionally documented decreased NAA.14,23,48–50 Compared with absolute quantitation, ratio determination provides a simpler and more reliable method with less experimental error. It would be worthwhile to follow up these findings with a study that incorporates absolute quantitation but with a larger sample size. Our voxel size allowed relatively good tissue specificity of the regions of interest. Although a higher spatial resolution would have improved the accuracy of this, absolute quantification of NAA and Cho levels would have come at the cost of a substantially increased scanning time, which is difficult for this group of patients.
Conclusions
In summary, this study adds to the growing body of evidence of degeneration of the brain beyond the motor cortex in ALS. Future work should aim to determine the association of cingulate pathology with neuropsychological measures to obtain an improved understanding of the role of the cingulate cortex in motor, cognitive, emotional, and behavioral functions. Multimodal imaging, including MRSI, fMRI, and DTI, could help achieve this objective in both healthy and diseased states. DTI in particular would be instructive in better understanding the role of altered connectivity between regions.
Abbreviations
- ALS
amyotrophic lateral sclerosis
- ALSFRS
ALS Functional Rating Scale
- 11C
carbon-11
- Cho
choline
- CMA
cingulate motor areas
- Cr
creatine
- DTI
diffusion tensor imaging
- FDG
fluorodeoxyglucose
- fMRI
functional MR imaging
- FTD
frontotemporal dementia
- FTLD
frontotemporal lobar degeneration
- GABAA
gamma-aminobutyric acid type A receptor
- LMN
lower motor neurons
- MCC
mid-cingulate cortex
- MRSI
MR spectroscopic imaging
- NAA
N-acetylaspartate
- PCG
precentral gyrus
- PET
positron-emission tomography
- TDP-43
TAR DNA−binding protein 43
- THAL
thalamus
- UMN
upper motor neurons
Footnotes
This work was supported by the University of Alberta Hospital Foundation and the M.S.I. Foundation of Alberta.
References
- 1. Ringholz GM, Appel SH, Bradshaw M, et al. Prevalence and pattern of cognitive impairment in sporadic ALS. Neurology 2005;65:586–90 [DOI] [PubMed] [Google Scholar]
- 2. Strong MJ. The syndromes of frontotemporal dysfunction in amyotrophic lateral sclerosis. Amyotroph Lateral Scler 2008;9:323–38 [DOI] [PubMed] [Google Scholar]
- 3. Kiernan JA, Hudson AJ. Frontal lobe atrophy in motor neuron diseases. Brain 1994;117(pt 4):747–57 [DOI] [PubMed] [Google Scholar]
- 4. Ikemoto A, Hirano A, Akiguchi I. Neuropathology of amyotrophic lateral sclerosis with extra-motor system degeneration: characteristics and differences in the molecular pathology between ALS with dementia and Guamanian ALS. Amyotroph Lateral Scler Other Motor Neuron Disord 2000;1:97–104 [DOI] [PubMed] [Google Scholar]
- 5. Ellis CM, Suckling J, Amaro E, Jr, et al. Volumetric analysis reveals corticospinal tract degeneration and extramotor involvement in ALS. Neurology 2001;57:1571–78 [DOI] [PubMed] [Google Scholar]
- 6. Devinsky O, Morrell MJ, Vogt BA. Contributions of anterior cingulate cortex to behaviour. Brain 1995;118(pt 1):279–306 [DOI] [PubMed] [Google Scholar]
- 7. Wong JC, Concha L, Beaulieu C, et al. Spatial profiling of the corticospinal tract in amyotrophic lateral sclerosis using diffusion tensor imaging. J Neuroimaging 2007;17:234–40 [DOI] [PubMed] [Google Scholar]
- 8. Pyra T, Hui B, Hanstock C, et al. Combined structural and neurochemical evaluation of the corticospinal tract in amyotrophic lateral sclerosis. Amyotroph Lateral Scler 2010;11:157–65 [DOI] [PubMed] [Google Scholar]
- 9. Brooks BR, Miller RG, Swash M, et al. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord 2000;1:293–99 [DOI] [PubMed] [Google Scholar]
- 10. Ellis CM, Simmons A, Jones DK, et al. Diffusion tensor MRI assesses corticospinal tract damage in ALS. Neurology 1999;53:1051–58 [DOI] [PubMed] [Google Scholar]
- 11. Provencher SW. Estimation of metabolite concentrations from localized in vivo proton NMR spectra. Magn Reson Med 1993;30:672–79 [DOI] [PubMed] [Google Scholar]
- 12. Block W, Karitzky J, Traber F, et al. Proton magnetic resonance spectroscopy of the primary motor cortex in patients with motor neuron disease: subgroup analysis and follow-up measurements. Arch Neurol 1998;55:931–36 [DOI] [PubMed] [Google Scholar]
- 13. Pohl C, Block W, Karitzky J, et al. Proton magnetic resonance spectroscopy of the motor cortex in 70 patients with amyotrophic lateral sclerosis. Arch Neurol 2001;58:729–35 [DOI] [PubMed] [Google Scholar]
- 14. Suhy J, Miller RG, Rule R, et al. Early detection and longitudinal changes in amyotrophic lateral sclerosis by (1)H MRSI. Neurology 2002;58:773–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kalra S, Hanstock CC, Martin WR, et al. Detection of cerebral degeneration in amyotrophic lateral sclerosis using high-field magnetic resonance spectroscopy. Arch Neurol 2006;63:1144–48 [DOI] [PubMed] [Google Scholar]
- 16. Ince PG, Lowe J, Shaw PJ. Amyotrophic lateral sclerosis: current issues in classification, pathogenesis and molecular pathology. Neuropathol Appl Neurobiol 1998;24:104–17 [DOI] [PubMed] [Google Scholar]
- 17. Lowe J. New pathological findings in amyotrophic lateral sclerosis. J Neurol Sci 1994;124(suppl):38–51 [DOI] [PubMed] [Google Scholar]
- 18. Kawashima T, Doh-ura K, Kikuchi H, et al. Cognitive dysfunction in patients with amyotrophic lateral sclerosis is associated with spherical or crescent-shaped ubiquitinated intraneuronal inclusions in the parahippocampal gyrus and amygdala, but not in the neostriatum. Acta Neuropathol 2001;102:467–72 [DOI] [PubMed] [Google Scholar]
- 19. Okamoto K, Hirai S, Yamazaki T, et al. New ubiquitin-positive intraneuronal inclusions in the extra-motor cortices in patients with amyotrophic lateral sclerosis. Neurosci Lett 1991;129:233–36 [DOI] [PubMed] [Google Scholar]
- 20. Kassubek J, Unrath A, Huppertz HJ, et al. Global brain atrophy and corticospinal tract alterations in ALS, as investigated by voxel-based morphometry of 3-D MRI. Amyotroph Lateral Scler Other Motor Neuron Disord 2005;6:213–20 [DOI] [PubMed] [Google Scholar]
- 21. Mezzapesa DM, Ceccarelli A, Dicuonzo F, et al. Whole-brain and regional brain atrophy in amyotrophic lateral sclerosis. AJNR Am J Neuroradiol 2007;28:255–59 [PMC free article] [PubMed] [Google Scholar]
- 22. Pioro EP, Antel JP, Cashman NR, et al. Detection of cortical neuron loss in motor neuron disease by proton magnetic resonance spectroscopic imaging in vivo. Neurology 1994;44:1933–38 [DOI] [PubMed] [Google Scholar]
- 23. Bowen BC, Pattany PM, Bradley WG, et al. MR imaging and localized proton spectroscopy of the precentral gyrus in amyotrophic lateral sclerosis. AJNR Am J Neuroradiol 2000;21:647–58 [PMC free article] [PubMed] [Google Scholar]
- 24. Abe K, Takanashi M, Watanabe Y, et al. Decrease in N-acetylaspartate/creatine ratio in the motor area and the frontal lobe in amyotrophic lateral sclerosis. Neuroradiology 2001;43:537–41 [DOI] [PubMed] [Google Scholar]
- 25. Cwik VA, Hanstock CC, Allen PS, et al. Estimation of brainstem neuronal loss in amyotrophic lateral sclerosis with in vivo proton magnetic resonance spectroscopy. Neurology 1998;50:72–77 [DOI] [PubMed] [Google Scholar]
- 26. Anderson ME, Turner RS. Activity of neurons in cerebellar-receiving and pallidal-receiving areas of the thalamus of the behaving monkey. J Neurophysiol 1991;66:879–93 [DOI] [PubMed] [Google Scholar]
- 27. Smith MC. Nerve fibre degeneration in the brain in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 1960;23:269–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kato S, Oda M, Hayashi H, et al. Participation of the limbic system and its associated areas in the dementia of amyotrophic lateral sclerosis. J Neurol Sci 1994;126:62–69 [DOI] [PubMed] [Google Scholar]
- 29. Kew JJ, Goldstein LH, Leigh PN, et al. The relationship between abnormalities of cognitive function and cerebral activation in amyotrophic lateral sclerosis: a neuropsychological and positron emission tomography study. Brain 1993;116:1399–423 [DOI] [PubMed] [Google Scholar]
- 30. Abrahams S, Goldstein LH, Simmons A, et al. Word retrieval in amyotrophic lateral sclerosis: a functional magnetic resonance imaging study. Brain 2004;127:1507–17 [DOI] [PubMed] [Google Scholar]
- 31. Rule RR, Schuff N, Miller RG, et al. Gray matter perfusion correlates with disease severity in ALS. Neurology 2010;74:821–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Strong MJ, Grace GM, Orange JB, et al. A prospective study of cognitive impairment in ALS. Neurology 1999;53:1665–70 [DOI] [PubMed] [Google Scholar]
- 33. Chang JL, Lomen-Hoerth C, Murphy J, et al. A voxel-based morphometry study of patterns of brain atrophy in ALS and ALS/FTLD. Neurology 2005;65:75–80 [DOI] [PubMed] [Google Scholar]
- 34. Thivard L, Pradat PF, Lehericy S, et al. Diffusion tensor imaging and voxel based morphometry study in amyotrophic lateral sclerosis: relationships with motor disability. J Neurol Neurosurg Psychiatry 2007;78:889–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Grosskreutz J, Kaufmann J, Fradrich J, et al. Widespread sensorimotor and frontal cortical atrophy in amyotrophic lateral sclerosis. BMC Neurol 2006;6:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jeong Y, Park KC, Cho SS, et al. Pattern of glucose hypometabolism in frontotemporal dementia with motor neuron disease. Neurology 2005;64:734–36 [DOI] [PubMed] [Google Scholar]
- 37. Turner MR, Cagnin A, Turkheimer FE, et al. Evidence of widespread cerebral microglial activation in amyotrophic lateral sclerosis: an [11C](R)-PK11195 positron emission tomography study. Neurobiol Dis 2004;15:601–09 [DOI] [PubMed] [Google Scholar]
- 38. Lloyd CM, Richardson MP, Brooks DJ, et al. Extramotor involvement in ALS: PET studies with the GABA(A) ligand [(11)C]flumazenil. Brain 2000;123(pt 11):2289–96 [DOI] [PubMed] [Google Scholar]
- 39. Leichsenring A, Linnartz B, Zhu XR, et al. Ascending neuropathology in the CNS of a mutant SOD1 mouse model of amyotrophic lateral sclerosis. Brain Res 2006;1096:180–95 [DOI] [PubMed] [Google Scholar]
- 40. Neumann M, Sampathu DM, Kwong LK, et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science 2006;314:130–33 [DOI] [PubMed] [Google Scholar]
- 41. Geser F, Brandmeir NJ, Kwong LK, et al. Evidence of multisystem disorder in whole-brain map of pathological TDP-43 in amyotrophic lateral sclerosis. Arch Neurol 2008;65:636–41 [DOI] [PubMed] [Google Scholar]
- 42. Hatanaka N, Tokuno H, Hamada I, et al. Thalamocortical and intracortical connections of monkey cingulate motor areas. J Comp Neurol 2003;462:121–38 [DOI] [PubMed] [Google Scholar]
- 43. Shibata H, Yukie M. Differential thalamic connections of the posteroventral and dorsal posterior cingulate gyrus in the monkey. Eur J Neurosci 2003;18:1615–26 [DOI] [PubMed] [Google Scholar]
- 44. Guye M, Parker GJ, Symms M, et al. Combined functional MRI and tractography to demonstrate the connectivity of the human primary motor cortex in vivo. Neuroimage 2003;19:1349–60 [DOI] [PubMed] [Google Scholar]
- 45. Hatanaka N, Nambu A, Yamashita A, et al. Somatotopic arrangement and corticocortical inputs of the hindlimb region of the primary motor cortex in the macaque monkey. Neurosci Res 2001;40:9–22 [DOI] [PubMed] [Google Scholar]
- 46. He SQ, Dum RP, Strick PL. Topographic organization of corticospinal projections from the frontal lobe: motor areas on the medial surface of the hemisphere. J Neurosci 1995;15:3284–306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Wang Y, Shima K, Sawamura H, et al. Spatial distribution of cingulate cells projecting to the primary, supplementary, and pre-supplementary motor areas: a retrograde multiple labeling study in the macaque monkey. Neurosci Res 2001;39:39–49 [DOI] [PubMed] [Google Scholar]
- 48. Schuff N, Rooney WD, Miller R, et al. Reanalysis of multislice (1)H MRSI in amyotrophic lateral sclerosis. Magn Reson Med 2001;45:513–16 [DOI] [PubMed] [Google Scholar]
- 49. Sarchielli P, Pelliccioli GP, Tarducci R, et al. Magnetic resonance imaging and 1H-magnetic resonance spectroscopy in amyotrophic lateral sclerosis. Neuroradiology 2001;43:189–97 [DOI] [PubMed] [Google Scholar]
- 50. Gredal O, Rosenbaum S, Topp S, et al. Quantification of brain metabolites in amyotrophic lateral sclerosis by localized proton magnetic resonance spectroscopy. Neurology 1997;48:878–81 [DOI] [PubMed] [Google Scholar]