Abstract
Background:
Cardiovascular disease (CVD) risks are of concern among immigrants and refugees settling in affluent host countries. The prevalence of CVD and risk factors among Somali African immigrants to the U.S. has not been systematically studied.
Methods:
In 2015–2016, we surveyed 1156 adult Somalis in a Midwestern metropolitan area using respondent-driven sampling to obtain anthropometric, interview, and laboratory data about CVD and associated risk factors, demographics, and social factors.
Results:
The prevalence of diabetes and low physical activity among men and women was high. Overweight, obesity, and dyslipidemia were also particularly prevalent. Levels of calculated CVD risk across the community were greater for men than women.
Conclusion:
Though CVD risk is lower among Somalis than the general U.S. population, our results suggest significant prevalence of risk factors among Somali immigrants. Comparison with prior research suggests that CVD risks may be increasing, necessitating thoughtful intervention to prevent adverse population outcomes.
Keywords: cardiovascular disease, risk factors, diabetes, obesity, Somali, immigrant, refugee, acculturation
Background and Conceptual Framework
Cardiovascular disease (CVD) and its risk factors are leading causes of preventable morbidity and mortality in the United States and other developed countries. Ethnic minorities in the U.S. are disproportionally affected by CVD and associated risk factors.1 For new immigrants settling in the U.S., acculturation often increases the risks and burdens of CVD. For example, rapid weight gain due to changes in diet and activity is a common trend among immigrants.2 These worsening changes in disease risks and profiles as new immigrants and refugees are exposed to new environments in receiving countries have been previously termed “the healthy immigrant effect.”3–5
Over the last few decades, substantial social and epidemiologic changes on the African continent have shifted health concerns to include the increased prevalence of non-communicable conditions like obesity, dyslipidemia, diabetes, hypertension, and smoking that lead to cardiovascular disease.6–8 Prior studies have suggested that CVD risks are of particular concern among African refugees settling in affluent host countries like the U.S.9,10 These new risks result from the combination of genetics and a new environment that brings with it new diet, activities, and habits. Somali immigrants are one of the largest populations of African immigrants in the U.S., but their CVD risk factors have not been well documented.11,12 The largest and longest-standing population of Somali immigrants and refugees in the U.S. is in Minnesota, primarily in the metropolitan area of Minneapolis and St. Paul (MSP). In 2001, approximately 10,000 Somalis lived in Minnesota. According to the American Communities Survey (ACS), approximately 21,000 Somalis lived in Minnesota in 2011–13.13 The population continues to be fast-growing due to births, continued refugee resettlement, and secondary migration of U.S. Somalis to Minnesota. Thus, according to ACS data, there were roughly 27,000 Somalis living in Minnesota in 2016.14
Several prior studies have suggested that CVD risks might be of concern among Somali immigrants and refugees, but results have been mixed. Surveys in United States, Norway, Finland, and New Zealand have reported high rates of overweight and obesity in female Somali immigrants.15–17 In a recent systematic chart review from a clinic system in Minnesota, high rates of obesity, pre-diabetes, and diabetes were also reported.12 In a detailed 2009 survey of smoking habits in the Somali community, cigarette use was 44% among men while only 4% among women. Comparing Somali immigrants’ CVD risk and major heart disease outcomes with long-term residents in Canada, between 2002 and 2011, Somali immigrants had significantly lower incidence of major cardiovascular events than long-term Canadian residents and many other Canadian immigrant groups.18 Similarly, Somalis appeared overall healthier in a self-report survey comparing the CVD risk factors among six different groups of African immigrants in Minnesota.19 These mixed findings suggest a need for further exploration of health and risk factors among Somalis immigrants.
Methods
To understand the CVD risks facing the Somali community in the MSP metropolitan area, we conducted a cross-sectional epidemiologic study of 1,156 Somalis residing in MSP from late 2015 through early 2016. We obtained anthropometric, survey, and laboratory data about demographics, CVD risk factors, acculturation, and social factors. Our efforts were inspired by a 2001 study of CVD risk among a cluster-randomized sample of 253 Somalis residing in Minneapolis, conducted by members of our study team.20 Our aim in the current study was to determine the areas of greatest concern for CVD risk and of greatest potential for prevention within the Somali community. The Institutional Review Board of the HealthPartners’ Institute reviewed and approved this study. Participants signed written informed consent translated into Somali for non-English speakers.
Community-Based Participatory Research
To ensure respectful and culturally-informed study processes, we employed community-based participatory research techniques (Table 1).21 Engagement began prior to grant submission, as the study team met with community leaders to identify mutually beneficial goals and priorities, which were written into the research proposal. To ensure the study maintained fidelity to community needs and priorities, researchers regularly met with community leaders, including those with public health experience. Our community partners shared important cultural insights and assisted in the recruitment of other community members for listening sessions with Somali community leaders and liaisons. To provide a broader base of opinion and consultation, we developed a Community Advisory Panel (CAP) that included members of the listening sessions as well as Somali media, medical, and religious leaders identified by our community partners. After extensive explanations of the purpose and methods of the study, CAP members assisted in the development of study procedures, including adapting previously developed survey questions for cultural relevance. They also consulted on acceptable means of obtaining survey, anthropometric and laboratory data, including the engagement of gender and ethnicity-concordant Community Health Workers (CHW’s) and the use of finger-stick blood spots rather than venous blood samples. As the study proceeded, CAP members were briefed roughly quarterly about details of study progress, offering their interpretations and advice on surmounting challenges encountered, primarily with recruitment. As results were finalized, the CAP received presentations and helped disseminate results to the Somali community.
Table 1:
Study Execution of CBPR Principles, 2015–2016
| Community Based Participatory Research Principle | Study Strategy |
|---|---|
| Recognize Community as a unit of identity | Community leaders, Somali media, community’s medical and religious leaders actively engaged throughout the study. The enhanced social link recruitment strategy allowed metro wide participations beyond the community’s major residential areas. |
| Facilitates collaborative partnerships in all phases of the research | Shared decision-making strategy community team members throughout the study. Community research partners written into grants and hired at management levels to assist in study administration. |
| Promotes a co-learning and empowering process that attends to social in-equalities | Collaborative team and community meetings provide opportunities for both researchers and community members to learn from each other. Researchers learning cultural nuances pertaining to the study, while community members learn the procedures and policies of conducting community research. |
| Involves a cyclical and iterative process | Study team is developing the scientific research skill of the community through mentoring and research skill building of doctorate public health students from the study population. NIH supplement grant to develop community researcher skills. Study employed numerous staff members. The team also aims to sustain established relationships for long term commitments and explore next steps after data is analyzed. |
| Builds on strength and resources within the community | Community researchers are part of all meeting groups and actively participate in all regular meetings. Major decisions regarding the study are made during these meetings |
| Disseminates finding and knowledge gained to all partners | Feedback provided orally to ALL study participants to inform them on their bio results and CVD risk factors through a phone call by a well-respected and well known Somali physician from the community who is also part of the research study team. |
Participants and Data Collection
Since their original arrival in the mid-1990s, the Somali population has grown and spread throughout the MSP metropolitan area while remaining somewhat culturally isolated. The study team and partners therefore determined that respondent-driven sampling (RDS) was the most appropriate sampling strategy for our study. RDS is a chain-referral sampling and recruitment process appropriate for use with hidden populations or those for whom no adequate sampling frame exists.22 RDS can produce an asymptotically unbiased sample even in the presence of complex ethnographic issues.23 RDS recruitment begins with a small convenience sample of “seed” individuals as initial participants.24 Members of the study team recruited eleven seed participants (age ≥ 18, balanced between men and women across a range of ages) from social connections in the local Somali community. “Seeds” were asked to identify and recruit the first “wave” of additional participants from their social networks, who were then asked to recruit from their social networks, and so on. Theory and RDS best-practices guided our decisions about the initial number of seeds, the number of social contacts each participant could recruit (from 3 to 5 depending on the wave), and the minimum number of recruitment waves to complete from each seed (5 to 7) in order to approach a random sample.22,23,25,26 Participation and recruitment were each incentivized with department store and VISA gift cards. Trained ethnicity- and gender-concordant CHWs conducted face-to-face interviews in Somali or English, recording anthropometric measurements and obtaining blood-spot samples. Consistent with RDS best practices, recruitment was monitored and adjusted to ensure representativeness as the study proceeded. We ultimately recruited 1,156 Somali adults residing in the MSP metropolitan area, obtaining a participation rate of 61% (Supplemental Table 4). With 21,000 adult Somalis in MSP around 2012, this sample represents about 5.5% of the population.
Measures
Anthropometric measures included height, weight, waist circumference, and blood pressure (BP) from which we derived and computed variables (Table 2). Interviews and physical measures were obtained in the participant’s home or a convenient and private community site. CHW’s measured height and weight (shoes off and lightly clothed with Seca Portable Stadiometer and Scale). Waist circumference was measured standing up, over bare skin, at the narrowest level between the superior borders of the iliac crest and below the 10th rib. A sphygmomanometer with appropriately-sized arm cuff was used to measure 3 consecutive BP measurements while each participant rested quietly in a seated position for 5 minutes and once the participant’s maximum inflation level was determined. The averages of 3 systolic blood pressure (SBP) and 3 diastolic blood pressure (DBP) outputs were recorded. Blood samples were obtained for measures of diabetes (hemoglobin A1c) and cholesterol (total and high density lipoprotein). Finger-stick samples were collected on bloodspot cards and analyzed by Core Medical Laboratories, LLC (Lee’s Summit, Missouri).27,28
Table 2:
CVD Risk Factor Measures, 2015–2016
| CVD Risk Factors | |
|---|---|
| Hypertension (HTN) | |
| Pre-Hypertension | 130/80mmHg ≤ BP <140/90mmHg |
| Hypertension | Self-report of diagnosis or BP>140/90mmHg |
| Diabetes | |
| Pre-Diabetes | 5.7% ≤ HgbAlc < 6.5% and self-report denying diagnosis and not on DM meds |
| Diabetes | Self-report of diagnosis or HgbAlc ≥ 6.5% |
| Dyslipidemia | |
| Low HDL | Men<40 mg/dl, Women<50 mg/dl |
| Dyslipidemia | Self-report of diagnosis or TC/HDL ratio ≥ 5 (male), ≥ 4.5 (female), or TC ≥ 200 mg/dl |
| Body mass index (BMI) | Weight (kg)/Height (M2) |
| Overweight | BMI 25–29.9 |
| Obese | BMI ≥30 |
| Waist circumference (WC) | WHO indicator cut-points |
| Increased CVD risk | Men>=94cm, Women>=80cm |
| Smoker | “Yes” response to “Do you currently smoke tobacco on a daily basis or less than daily…?” |
| Physical Activity | Self-report of obtaining at least 150 minutes/wk of moderate or vigorous physical activity* |
| Physical Inactivity | Self-report of work or leisure exercise less than 5 times per month** |
| ≥3 CVD risk factors | ≥ 3 of the risk factors above |
| History of CVD | Self-report of diagnosis of heart disease |
Survey data obtained using the World Health Organization’s General Physical Activity Questionnaire as adapted based on CAP input for use in an urban Somali immigrant population. Calculated and reported according to the AHA 2020 measure of ideal physical activity.
Physical inactivity data as calculated according to the World Health Organization’s General Physical Activity Questionnaire for comparison with 2001 Somali CVD Study data.
Analysis
We report the percentage of participants in the sample with each health condition, as determined by survey, anthropometric, and lab measures, weighted to the age and sex distribution of the Somali population of the MSP metropolitan area in the closet three year28combined American Communities survey (Figure 1), after adjusting for clustering. Pregnant women (16) were excluded from analyses of physical and laboratory data.
Figure 1:
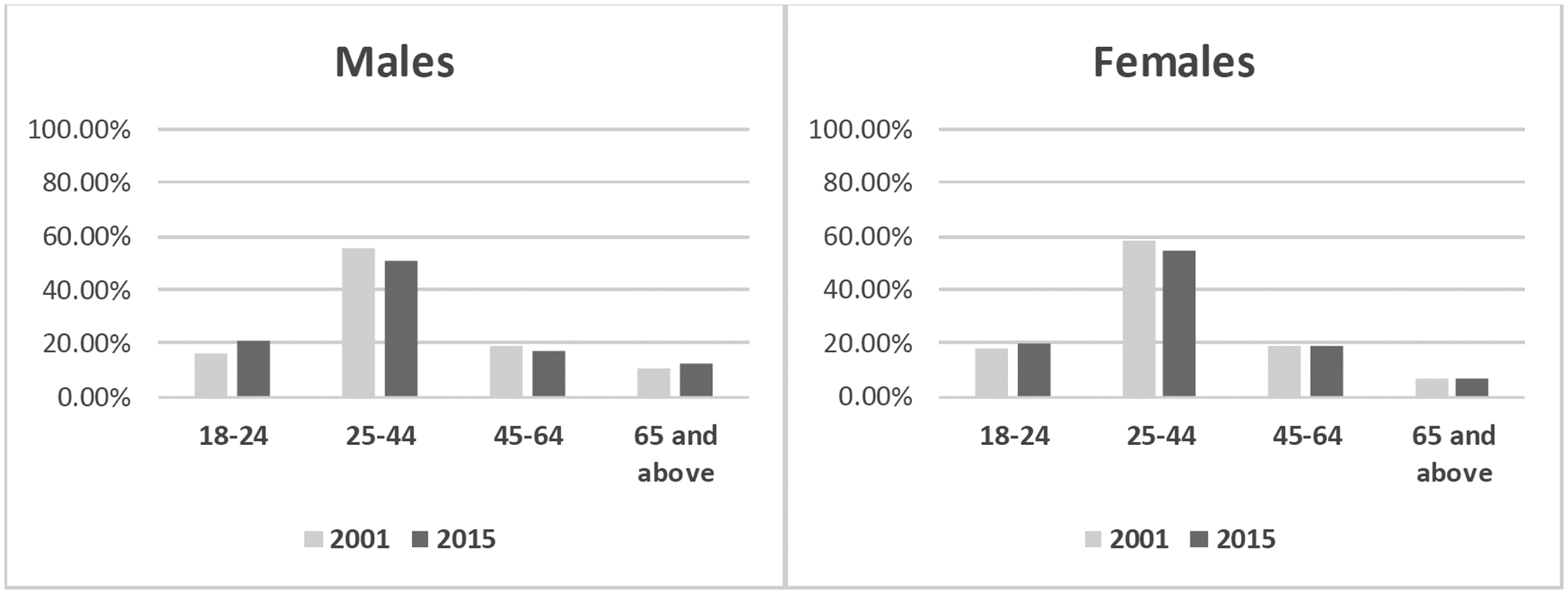
Age and Gender distributions weighted by US Census Community Data
Clustering in the study resulted from our use of RDS. Such clustering of observations means that, for statistical testing purposes, effective sample sizes are smaller than the observed sample sizes. While this is known to lead to underestimation of standard errors, it generally does not result in any significant mis-estimation of means.29–33 In addition to clustering due to the similarities of individuals in social-networks, RDS leads to a sample in which an individual’s likelihood of being included depends on the size of the social network from which they are being recruited, and the efficiency of recruitment within that network. To correct for this, we used RDSAT 7.1 software34 to generate individual-level sample weights that are inverse to the probability of an individual being included in the sample and re-scaled so the total weighted sample size equals the original unweighted sample size. Sampling weights were informed by respondent estimates of their social network size, estimates of the size of the total population, and information about connections between respondents. The resulting weights range from 0.14 to 9.32.
Results
Sample Characteristics
Females represented 62% of the study sample (Table 3). The average length of residence in the U.S. was 7 years for men and 8 years for women. Educational attainment was predominately less than a high school degree (61% of men and 75% of women), with completion of a high school degree being the next most frequent category (24% of women and 35% of men). Less than 2% of women and less than 4% of men had attained any college or higher education. Labor force participation, either full- or part-time was 45% among women and only 35% among men. Among women, only 30% of our sample reported fluency in English language, while 45% of men reported fluency. Women in our sample reported both higher levels of health insurance coverage (either private or publicly provided) and having a regular primary care provider (80% and 52%, respectively) than did men (72% and 30%, respectively).
Table 3:
Sample Demographics, 2015–2016
| Female | Male | |
|---|---|---|
| Proportion of Sample | 62.97% | 37.03% |
| Years of US Residence | 8.41 | 7.32 |
| Mean Educational Status | ||
| Less than High School | 75.17% | 60.76% |
| High School | 23.56% | 34.98% |
| College | 1.24% | 3.25% |
| Graduate/Professional | 0.00% | 0.64% |
| Employed Currently | 44.95% | 34.82% |
| Health Insurance, yes | 79.90% | 71.70% |
| Primary care, yes | 52.14% | 29.78% |
| Fluent in English | 30.14% | 44.60% |
CVD Risk Factors
We found that 21% of females in our sample were pre-hypertensive, while another 18% had frank hypertension (Table 4). These proportions were higher among men, 27% and 29%, respectively. Prediabetes was 21% among women and 25% among men, while frank diabetes was 15% and 21%, respectively. Dyslipidemia rates of low HDL were 49% among males and 32% among females, while rates of hyperlipidemia were 63% among females and 49% among males. While 25% of females were overweight, based on their BMI, this was true for 29% of males. In contrast, obesity was more than twice as high among females compared to males (57% vs 24%). Only 30% of females and 39% of males met American Heart Association guidelines for getting at least 150 minutes/week of moderate to vigorous physical activity.35 Females were more than twice as likely as males to have a waist circumference that put them at elevated risk of CVD (85% and 40%, respectively). Only 2% of females reported being current smokers, while this was true of 15% of males. The proportion of individuals with more than three CVD risk factors was 72% among females, and 47% among males. Self-reported history of CVD was 5% among females and 7% among males.
Table 4:
Modifiable CVD Risk Factors by Gender in Somali Adults, 2015–2016
| CVD and Risk Factors | Female | Male |
|---|---|---|
| Hypertension (HTN) | ||
| Pre-Hypertension (BP≥130/80mmHg and BP<140/90 mmHg) |
21.49% | 27.04% |
| Diagnosis or BP>140/90 mmHg | 17.76% | 29.18% |
| Diabetes | ||
| Pre-Diabetes (HgbAlc ≥5.7% & HgbA1c <6.5%) |
20.92% | 24.94% |
| Diagnosis or HgbA1c≥6.5% | 14.56% | 21.08% |
| Dyslipidemia | ||
| Low HDL (Men<40 mg/dl, Women<50 mg/dl) | 49.20% | 31.54% |
| Diagnosis or Total Cholesterol/HDL Ratio (Men>5, Female>4.5) or Total Cholesterol >200 mg/dl |
62.54% | 49.00% |
| Diagnosis, Total Cholesterol >= 200 mg/dl, or High ratio of Total of Cholesterol/HDL | 62.54% | 49.00% |
| Body mass index | ||
| Overweight (BMI 25–29.9 kg/m2) | 24.54% | 28.96% |
| Obese (BMI ≥30 kg/m2) | 56.82% | 23.96% |
| Waist circumference | ||
| High risk (Men≥94 cm, Women≥80 cm) | 85.21% | 40.02% |
| Smoker | 1.98% | 14.66% |
| Physical Activity | 30.43% | 38.63% |
| Physical Inactivity | 75.04% | 69.55% |
| ≥3 CVD risk factors | 71.62% | 46.60% |
| History of CVD | 4.86% | 6.87% |
Discussion
This is the first major epidemiologic study to describe the prevalence Somali immigrant and of CVD risk factors in a refugee community in the U.S. Our data suggest that among adult Somalis in the MSP metropolitan area there is a substantial prevalence of overweight, obesity, diabetes, low physical activity, and CVD risk.36 Comparing our data to the National Health and Nutrition Examination Survey, several contrasts are evident.37 Most notably, the prevalence of diabetes was higher in both Somali women (14.6%) and men (21.2%) than for women and men nationally overall (12.6%, 15.9%). The prevalence of physical activity was also lower in both Somali women (30%) and men (39%) than for women and men nationally overall (43%, 46%). Though rates of overweight by among Somalis (24.5% women, 29% men) were somewhat lower than national averages (27.2% women, 36.7% men), the rate of obesity among women was notably higher (56.8% vs 41.5%). Similarly, the rate of dyslipidemia among Somali women (62.5%) was substantially higher than the national rate for women overall (53.4%). The prevalence of obesity and dyslipidemia among Somali men, and the prevalence of hypertension and smoking among both genders was lower than national rates.
As previously noted, the currently study was inspired by a 2001 effort conducted by members of our study team. These studies used comparable measures, survey questions, and definitions of cardiovascular disease risk factors (supplemental materials). Due to different sampling methodologies, the potential unaccounted participation of individuals in both studies, and an evolving population with ongoing in-migration, formal statistical comparisons between the studies are not possible. However, given that the 2001 study constitutes the most similar epidemiologic survey of the Somali population to date, it provides a useful reference point. To facilitate descriptive comparisons between these two serial cross-sectional surveys, we also weighted the 2001 sample to the age and sex distribution of the Somali population of the MSP metropolitan area in the American Communities Survey (Figure 1).
Prehypertension was minimally higher for women and lower for men in our study (Table 3 and Supplement Table 3), while rates of hypertension were more than twice as high for men and women. While prediabetes was slightly higher in the current study, rates of diabetes were more than twice as high for both males and females. Rates of low HDL improved among males, while rates of dyslipidemia are higher among women in 2015. Rates of overweight were slightly lower in our 2015 study, while rates of obesity and physical inactivity were substantially higher among both men and women. Overall smoking rates were similar in both studies. The proportion of individuals with more than three CVD risk factors was slightly lower for males and slightly higher for females in the 2015 sample. While no females in the 2001 study had a history of CVD, nearly 5% did in 2015, and the number of males with CVD nearly was nearly twice as high. While some CVD risk factors were substantially higher in the 2015 sample, the rates are still lower than in the U.S. population overall for whom 36.6% of individuals have some form of CVD.36
Demographic characteristics of the population may have also changed. The average length of residence in the U.S. was about 4 years in 2001 and 8 years in 2015, suggesting the ongoing addition of new immigrants and refugees to the population. The proportion of the sample populations with high school education was higher in 2015, and the proportion who had a college or advanced degrees was substantially lower. Self-reported fluency in English was lower in the 2015 sample. Education and fluency differences were more prominent for males. Rates of health insurance and established primary care were slightly lower in the 2015 sample. Though concerning, connections to and enrollment in services may decline as individuals reside in the U.S. for longer periods and lose organized assistance offered to new refugees and immigrants.38 These differences in demographics and social factors may contribute to differences in CVD risk factors. The potential increases in the rates of hypertension, diabetes, and obesity, and physical inactivity noted above parallel results from a prior clinic study12 as well as general trends among other minorities experiencing health disparities in the U.S.39,40
Limitations
The primary limitation of our study is its respondent-driven sample. RDS can vary in relation to individuals’ willingness to participate and recruit, which may be related to their particular social positions. We experienced similar variability as well as difficulty recruiting young men due to concurrent FBI investigations in Minnesota of potential links between some Somalis and terrorist groups. With CAP input, we initiated additional young male seeds and CHW interviewers encouraged their recruitment to enhance sample representativeness even prior to RDS statistical weighting.
The study is also potentially limited by its use of dried blood spot lab data instead of venous blood samples. Our use of dried blood spot tools for lab sampling resulted from our listening sessions and CAP recommendations based on cultural concerns about obtaining and storing larger volume blood samples. Though early generation blood spot tools had some variability, relatively recent techniques have demonstrated improved reliability and concordance with lab measures from venous blood samples as well as practical utility in large epidemiologic studies.27,28
Finally, comparability with data from the NHANES and 2001 Somali community studies is limited by differences in study methodologies. To fully account for changing cultural and environmental forces that might contribute to CVD risk, a longitudinal cohort study would be preferable. Though we have standardized sample data to ACS age and sex estimates of the Somali population in MSP, differences between the two samples on other characteristics may be attributable to changes in either the prevalence of those characteristics or the composition of the underlying population or both. Due to our inability to distinguish between these factors, we remain uncertain as to the significance and causes of these potential trends.
Conclusion
The substantial and potentially increasing prevalence of CVD risk factors among Somali immigrants need to be considered against environment and population health changes in the U.S. as well as evolving immigration patterns, as individuals shift from new immigrant and refugee status to more stable situations. The unique aspects of Somali culture and Muslim religion may contribute to cohesive families and communities with unique diet and activities, but overall the refugee experience is associated with low socioeconomic status due in part to challenges of fluency, acculturation, education, and employment that can influence both good and detrimental health habits, a topic beyond the scope of the current paper.38
This study highlights the need to focus on CVD risk prevention, detection and treatment across the Somali population, including obesity and dyslipidemia among women, smoking among men, as well as diabetes and physical inactivity among both. Focused efforts to maintain insurance and primary-care relationships within the Somali community may allow for the improvement of risk profiles through good clinical care. Further research may also improve understanding and interventions upon environmental and behavioral factors that contribute to CVD risk among Somali refugees and immigrants. Ultimately, innovative public health solutions on the part of the community, institutions, and providers will be needed to prevent worsening CVD risks and future adverse outcomes in the Somali population.41–44
Supplementary Material
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- 1.Kurian AK, Cardarelli KM. Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethn Dis. 2007;17(1):143–152. [PubMed] [Google Scholar]
- 2.Terrazas A African immigrants in the United States, Migration Information Source, Migration Policy Institute. 2009; https://www.migrationpolicy.org/article/african-immigrants-united-states-0. Accessed September 4, 2019.
- 3.O’Connor MY, Thoreson CK, Ricks M, et al. Worse cardiometabolic health in African immigrant men than African American men: reconsideration of the healthy immigrant effect. Metab Syndr Relat Disord. 2014;12(6):347–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Venters H, Gany F. African immigrant health. J Immigr Minor Health. 2011;13(2):333–344. [DOI] [PubMed] [Google Scholar]
- 5.McDonald JT, Kennedy S. Insights into the ‘healthy immigrant effect’: health status and health service use of immigrants to Canada. Soc Sci Med. 2004;59(8):1613–1627. [DOI] [PubMed] [Google Scholar]
- 6.Tollman SM, Kahn K, Sartorius B, Collinson MA, Clark SJ, Garenne ML. Implications of mortality transition for primary health care in rural South Africa: a population-based surveillance study. Lancet. 2008;372(9642):893–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.BeLue R, Okoror TA, Iwelunmor J, et al. An overview of cardiovascular risk factor burden in sub-Saharan African countries: a socio-cultural perspective. Glob Health. 2009;5:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Research Council. The continuing epidemiological transition in Sub-Saharan Africa: a workshop summary. Washington, D. C.: The National Academies Press; 2012. [PubMed] [Google Scholar]
- 9.Peacock JM, Fashanu O, Styles E, Lindgren P. Foreign-born African-Americans and the impact on racial disparities in cardiovascular disease mortality in Minnesota, 2001–2015. Paper presented at: Council of State and Territorial Epidemiologists (CSTE)2017; Boise, ID. [Google Scholar]
- 10.Commodore-Mensah Y, Sampah M, Berko C, et al. The Afro-cardiac study: cardiovascular disease risk and ccculturation in West African immigrants in the United States: rationale and study design. J Immigr Minor Health. 2016;18(6):1301–1308. [DOI] [PubMed] [Google Scholar]
- 11.Kumar R, Einstein G. Cardiovascular disease in Somali women in the diaspora. Curr Cardiovasc Risk Rep. 2012;6(3):229–237. [Google Scholar]
- 12.Njeru JW, Tan EM, St Sauver J, et al. High rates of diabetes mellitus, pre-diabetes and obesity among Somali immigrants and refugees in Minnesota: a retrospective chart review. J Immigr Minor Health. 2016;18(6):1343–1349. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Census Bureau American FactFinder. Place of birth for the foreign-born population in the United States. Foreign-born population excluding population born at sea: 2007–2011 American Community Survey 5-year estimates [dataset]. Washington, D. C.: U.S. Department of Commerce; 2019. September 4. [Google Scholar]
- 14.U.S. Census Bureau American FactFinder. Place of birth for the foreign-born population in the United States. Foreign-born population excluding population born at sea: 2012–2016 American Community Survey 5-year estimates [dataset]. Washington DC: U.S. Department of Commerce; 2019. September 9. [Google Scholar]
- 15.Gele AA, Mbalilaki AJ. Overweight and obesity among African immigrants in Oslo. BMC research notes. 2013;6:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kinnunen TI, Skogberg N, Harkanen T, Lundqvist A, Laatikainen T, Koponen P. Overweight and abdominal obesity in women of childbearing age of Russian, Somali and Kurdish origin and the general Finnish population. J Public Health (Oxf). 2018;40(2):262–270. [DOI] [PubMed] [Google Scholar]
- 17.Guerin PB, Elmi FH, Corrigan C. Body composition and cardiorespiratory fitness among refugee Somali women living in New Zealand. J Immigr Minor Health. 2007;9(3):191–196. [DOI] [PubMed] [Google Scholar]
- 18.Tu JV, Chu A, Rezai MR, et al. The Incidence of major cardiovascular events in Immigrants to Ontario, Canada: The CANHEART immigrant study. Circ. 2015;132(16):1549–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sewali B, Harcourt N, Everson-Rose SA, et al. Prevalence of cardiovascular risk factors across six African Immigrant Groups in Minnesota. BMC Public Health. 2015;15:411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dalmar A, Pryce D, Grim CE, Jama S, Magan S. Overweight and obesity in Somali immigrants to the United States. Ethn Dis. 2006;16:S4–35. [Google Scholar]
- 21.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. [DOI] [PubMed] [Google Scholar]
- 22.Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Soc Probl. 1997;44(2):174–199. [Google Scholar]
- 23.Salganik MJ, Heckathorn DD. Sampling and estimation in hidden populations using respondent-driven sampling. Sociol Methodol. 2004;34:193–239. [Google Scholar]
- 24.Rudolph AE, Crawford ND, Latkin C, et al. Individual, study, and neighborhood level characteristics associated with peer recruitment of young illicit drug users in New York City: optimizing respondent driven sampling. Soc Sci Med. 2011;73(7):1097–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gile KJ, Handcock MS. Respondent-driven sampling: an assessment of current methodology. Sociol Methodol. 2010;40(1):285–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heckathorn DD. Respondent-driven sampling II: deriving valid population estimates from chain-referral samples of hidden populations. Soc Probl. 2002;49(1):11–34. [Google Scholar]
- 27.Samuelsson LB, Hall MH, McLean S, et al. Validation of Biomarkers of CVD Risk from Dried Blood Spots in Community-Based Research: Methodologies and Study-Specific Serum Equivalencies. Biodemography Soc Biol. 2015;61(3):285–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fokkema MR, Bakker AJ, de Boer F, Kooistra J, de Vries S, Wolthuis A. HbA1c measurements from dried blood spots: validation and patient satisfaction. Clin Chem Lab Med. 2009;47(10):1259–1264. [DOI] [PubMed] [Google Scholar]
- 29.Bland JM, Kerry SM. Statistics notes. Trials randomised in clusters. BMJ. 1997;315(7108):600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Donner A, Birkett N, Buck C. Randomization by cluster. Sample size requirements and analysis. Am J Epidemiol. 1981;114(6):906–914. [DOI] [PubMed] [Google Scholar]
- 31.Wejnert C An empirical test of respondent-driven sampling: point estimates, variance, degree measures, and out-of-equilibrium data. Sociol Methodol. 2009;39(1):73–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goel S, Salganik MJ. Assessing respondent-driven sampling. Proc Natl Acad Sci U S A. 2010;107(15):6743–6747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Simpson JM, Klar N, Donnor A. Accounting for cluster randomization: a review of primary prevention trials, 1990 through 1993. Am J Public Health. 1995;85(10):1378–1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spiller MW, Cameron C, Heckathorn DD, Barash V, Volz E, Degani I. Respondent-driven sampling analysis tool (RDSAT) Version 7.1. Ithaca, NY: Cornell University; 2012. [Google Scholar]
- 35.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. [DOI] [PubMed] [Google Scholar]
- 36.Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circ. 2017;135(10):e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.National Center for Health Statistics. National Health and Nutrition Examination Survey (NHANES) - National Cardiovascular Disease Surveillance System. Atlanta, GA: Centers for Disease Control and Prevention (CDC); 2019. [Google Scholar]
- 38.Warfa N, Curtis S, Watters C, Carswell K, Ingleby D, Bhui K. Migration experiences, employment status and psychological distress among Somali immigrants: a mixed-method international study. BMC Public Health. 2012;12:749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bell CN, Thorpe RJ Jr., Bowie JV, LaVeist TA. Race disparities in cardiovascular disease risk factors within socioeconomic status strata. Ann Epidemiol. 2018;28(3):147–152. [DOI] [PubMed] [Google Scholar]
- 40.Pool LR, Ning H, Lloyd-Jones DM, Allen NB. Trends in racial/ethnic disparities in cardiovascular health among US Adults from 1999–2012. Journal of the American Heart Association. 2017;6(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Commodore-Mensah Y, Himmelfarb CD, Agyemang C, Sumner AE. Cardiometabolic health in African immigrants to the United States: a call to re-examine research on African-descent populations. Ethn Dis. 2015;25(3):373–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hauck FR, Corr KE, Lewis SH, Oliver MN. Health and health care of African refugees: an underrecognized minority. J Natl Med Assoc. 2012;104(1–2):61–71. [DOI] [PubMed] [Google Scholar]
- 43.Read JG, Emerson MO, Tarlov A. Implications of black immigrant health for U.S. racial disparities in health. J Immigr Health. 2005;7(3):205–212. [DOI] [PubMed] [Google Scholar]
- 44.Mohamed AA, Hassan AM, Weis JA, Sia IG, Wieland ML. Physical activity among Somali men in Minnesota: barriers, facilitators, and recommendations. Am J Mens Health. 2014;8(1):35–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


