Abstract
Over a year after the initial emergence of the disease, the COVID-19 pandemic continues to strain healthcare systems worldwide. The value of feedback and connection between clinical care, public health, and death investigation systems has never been more clear. To this end, knowledge of the radiologic and histopathologic features of fatal COVID-19 is critical for those working with the living and the dead. Most of the medical descriptions of COVID-19 are either focused on clinical in vivo medical imaging or autopsies performed following an intensive course of treatment over days to weeks prior to death, rather than deaths in the community prior to hospitalization. Here we report the postmortem computed tomography (PMCT) and lung histopathology in five fatal cases of COVID-19 that were subject to medicolegal death investigation. All individuals died in the community without medical treatment, or after a brief terminal admission to hospital. In these cases, the main PMCT findings included: diffuse lung changes including ground glass-type opacifications, a “crazy paving” appearance, variable areas of more dense consolidation, and relatively few areas of spared/less involved lung parenchyma. The unifying histopathology was diffuse alveolar damage in various stages of cellular evolution. In all cases, the pattern of PMCT and the lung histopathology corroborated the diagnosis of COVID-19. We propose the routine use of PMCT as a potential screening tool for the identification of COVID-19 related fatalities in the medicolegal setting where a paucity of historical information may not otherwise permit the identification of this disease prior to autopsy.
Keywords: SARS-CoV-2, COVID-19, Autopsy, Postmortem CT scan, Pandemic, Public health
1. Introduction
COVID-19 is a zoonotic viral pneumonitis caused by infection with the novel coronavirus, SARS-CoV-2. The COVID-19 pandemic has created a global public health emergency that has affected millions of people in nearly all countries of the world. The clinical progression of the disease is variable with most infected individuals proceeding with a self-limiting course while others develop progressive respiratory failure and death [1], [2]. The factors that are correlated with mortality include advanced age, male sex, and comorbidities [3], [4], [5], [6]. However, the widespread nature of community transmission also results in death of individuals without readily identifiable risk factors.
The clinical, radiologic and pathologic characteristics of COVID-19 have been well-documented, but most of diagnostic imaging and histopathologic descriptions of the disease have been made in patients who die in hospital after intensive treatment. There are few descriptions available of the postmortem computed tomography (PMCT) findings and histopathologic features in fatal cases of COVID-19 where death occurs in the community and a medicolegal death investigation is involved [7], [8], [9]. Of the few reports that are available, some are limited by prolonged postmortem intervals and effects of funerary preparations/embalming [10] or the lack of histopathologic correlation of PMCT findings [11].
We report a Canadian perspective on this ongoing threat to the global community with the description of 5 cases of fatal COVID-19 in Province of Ontario, Canada, with corresponding PMCT and histopathological findings. This description provides additional insight to the spectrum of disease in COVID-19 without the confounding impacts of intensive therapeutic intervention.
2. Materials and methods
In Ontario, deaths related to the COVID-19 pandemic are not routinely accepted into the death investigation system since death is due to a natural disease. But, in some circumstances, the coroner will accept jurisdiction for death investigation if there is a need to clarify the cause of death, due to potential outbreak exposure of other individuals, or if death occurred before COVID-19 could be confirmed or excluded during life. Another indication for medicolegal death investigation may be to address family concerns regarding the death of a loved one in the setting of a long-term care institution.
Five cases of fatal COVID-19 are described in this study. All cases originated in Ontario, Canada. In all cases, postmortem examinations commenced with a review of the scene, circumstances and medical history, as documented by the coroner. Based on this review, a pre-autopsy swab was collected for PCR analysis for SARS-CoV-2, due to suspicion about fatal COVID-19. All cases had positive nasopharyngeal and throat swabs for the SARS-CoV-2 envelope gene. A standard external examination of the body was conducted. Postmortem CT imaging was undertaken using unenhanced whole body helical postmortem computed tomography (PMCT) scans acquired on a GE Healthcare Optima 660 64-slice CT scanner at 120 kVp and 375 mA with reconstructions at 1.25 mm slice thickness and 0.8 mm increment.
Minimally invasive autopsies were performed using universal precautions, in an isolated autopsy suite with negative pressure ventilation. The bodies were opened with a Y-shaped incision and the chest plate removed using rib shears. Representative sections of all 5 lung lobes and, in most cases, samples from major organs were obtained and fixed in formalin. Tissues were prepared using routine methods and stained with hematoxylin and eosin.
3. Results
Table 1 summarizes the salient observations in the 5 cases. Radiologic and pathologic examination of the lungs revealed consistent findings, all attributable to viral pneumonitis (see Fig. 1, Fig. 2). Clinical, radiologic and pathologic evidence corroborated the diagnosis of COVID-19, in the setting of PCR evidence of SARS-CoV-2. In all cases death was attributed to COVID-19, often with significant contribution by chronic underlying disease.
Table 1.
Clinical, radiologic and pathologic findings in 5 cases of fatal COVID-19.
| Case | Age/sex | SARS-CoV-2 PCR | Postmortem imaging | Lung histo-pathology | Comorbidities |
|---|---|---|---|---|---|
| 1 | 77/M | + | GGO, ‘crazy paving’, increased interstitial markings | DAD | COPD, ASCVD, HTN |
| 2 | 57/M | + | GGO, ‘crazy paving’, increased interstitial markings | DAD | HTN, DM |
| 3 | 94/M | + | GGO, zones with ‘crazy paving’, increased interstitial markings | DAD | HTN, SSS, dementia, ASCVD, COPD, amyloid heart disease |
| 4 | 76/M | + | GGO, ‘crazy paving’, increased interstitial markings, mostly posterior | DAD | None known |
| 5 | 51/M | + | GGO, increased interstitial markings | DAD | HTN, DM, ASCVD |
GGO - ground glass opacifications, DAD – diffuse alveolar damage, DM - diabetes mellitus, COPD – chronic obstructive lung disease, ASCVD – atherosclerotic cardiovascular disease, HTN – hypertension, SSS - sick sinus syndrome.
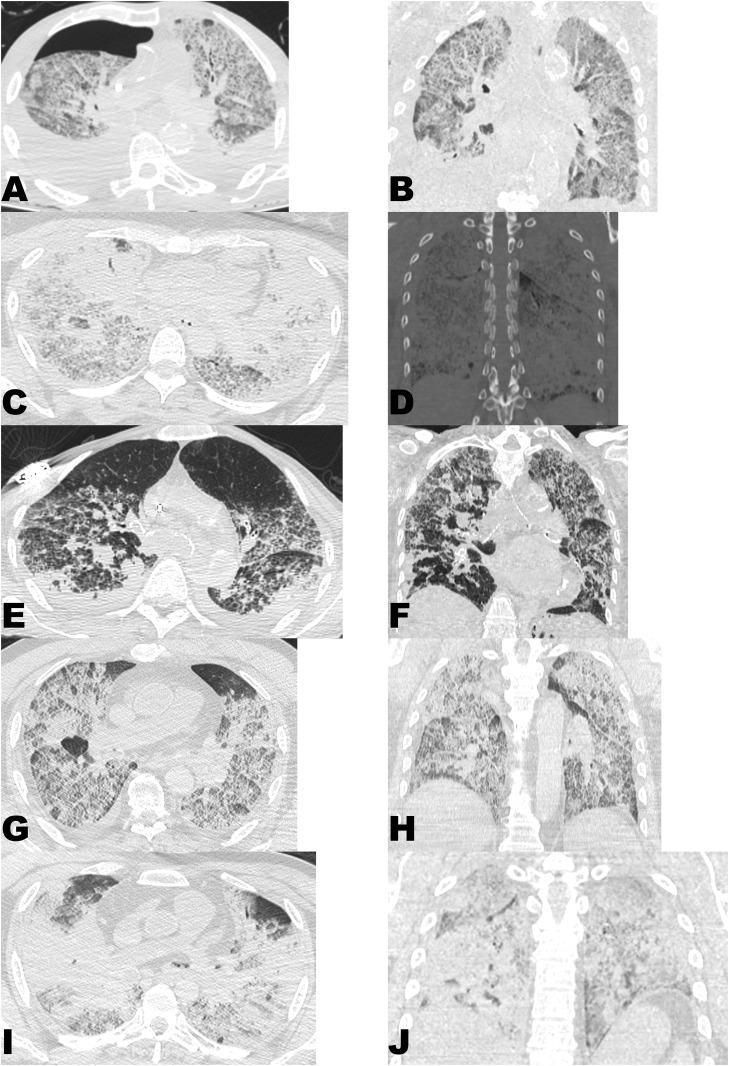
Fig. 1.
PMCT findings in COVID-19 related community deaths. Paired axial (A,C,E,G,I) and coronal (B,D,F,H,J) multiplanar reformats are presented for each of Cases 1 through 5 (A & B - Case 1; C & D - Case 2; E & F - Case 3; G & H - Case 4; I & J - Case 5). Each of the 5 cases showed similar PMCT findings, namely diffuse involvement, ground glass opacifications, increased interstitial markings, and a “crazy paving” appearance. Zones of sparing were quite limited in most cases and confined to the anterior-most portions of the lungs.
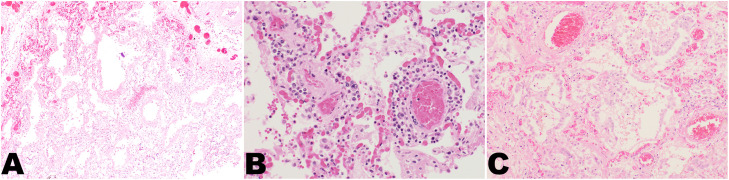
Fig. 2.
Lung histopathology in COVID-19. Representative examples from “Case 2”. A) Diffuse alveolar damage with pink, acellular hyaline membranes deposited along the walls of the alveoli (H&E, 40×). B) Perivascular chronic inflammatory infiltrate (H&E, 200×). C) Reactive type 2 pneumocytes with atypia. Rare mitotic figures are evident (right upper corner) (H&E, 100×).
3.1. Case 1
This was the index fatal case of COVID-19 in the Province of Ontario. This 77 year old man had a medical history of end-stage renal disease requiring dialysis, hypertension, hypercholesterolemia, type 2 diabetes, peripheral vascular disease, a repaired abdominal aortic aneurysm, coronary artery disease with previous percutaneous coronary intervention, previous myocardial infarct, and congestive heart failure. He reportedly had a 2-day history of weakness, shortness of breath, and possible fever. He was undergoing routine hemodialysis in a hospital-based outpatient clinic in the late afternoon when he was found to be less responsive. Dialysis was suspended and he was transferred to the emergency room where he was found to be dyspneic, tachypneic, hypoxic and hypotensive. A radiograph showed pleural effusion and bibasilar consolidation that was interpreted to represent either a pneumonia or congestive heart failure. Based on the totality of the clinical presentation, a diagnosis of community-acquired pneumonia was made. Due to previously expressed care wishes, no medical interventions were pursued, and he died the next day in the early afternoon. In the days following his death, a community contact of this man was found to test positive for SARS-CoV-2 by PCR. On this basis, a postmortem nasopharyngeal and throat swab were collected and were found to be positive for SARS-CoV-2 envelope gene, as was a percutaneous postmortem lung biopsy that was obtained prior to the minimally invasive autopsy.
PMCT demonstrated well-developed diffuse, bilateral ground glass opacifications, increased interstitial markings, “crazy paving” appearance, with interlobular septal thickening and traction bronchiectasis. There were variably more discrete areas of consolidation superimposed on this background. There were no zones of lung that appeared spared, only small zones of the anterior-most portions of the right middle and lower lobes that appeared slightly less markedly involved. There were bilateral effusions of moderate volume. Otherwise, there was a right pneumothorax from the known postmortem lung biopsy and a central venous catheter that was in place for this man’s long-standing dialysis-dependent end-stage kidney disease.
Pathologic examination revealed moderately severe diffuse centrilobular emphysema with secondary pulmonary arterial hypertension. Patchy areas of lung parenchyma, mostly centered on alveolar ducts, showed early diffuse alveolar damage characterized by hyaline membrane formation and early type 2 pneumocyte activation. There was a paucity of mononuclear cell inflammation. A secondary suppurative tracheitis and bronchiolitis was evident. Additional findings included atherosclerotic and hypertensive heart disease.
3.2. Case 2
This 57 year old woman had a medical history of hypertension, hypercholesterolemia, and diabetes mellitus. She was described to have recently developed a cough (the night prior to her death) but may have had a fever for up to a week prior. She was discovered deceased in bed. Resuscitation was attempted but was not successful. Pre-autopsy nasopharyngeal and throat swabs were positive for SARS-CoV-2.
PMCT images demonstrated marked, diffuse, bilateral ground glass opacifications, increased interstitial markings, “crazy paving” appearance, traction bronchiectasis, and larger zones of more dense consolidation bilaterally (especially marked in the upper lobes and right lateral lower lobe). There were no zones of lung that appeared spared, only small zones of the apical left upper lobe and anterior-most right middle lobe that appeared slightly less markedly involved. No significant effusions were evident. Otherwise, there were artefacts of attempted resuscitation.
Histologic examination revealed extensive diffuse alveolar damage characterized by extensive hyaline membrane formation, prominent alveolar macrophages, type 2 pneumocyte proliferation and a brisk perivascular and submucosal chronic inflammatory infiltrate. In addition, there was marked pulmonary edema and fibrin exudation within the alveoli.
3.3. Case 3
This 94 year old woman had a past medical history of hypertension, sick sinus syndrome with pacemaker, and dementia. She was a resident of a nursing home and had recently been experiencing ‘failure to thrive’, but no specific symptoms of respiratory illness were reported. She died at the nursing home and resuscitation was not attempted. A medicolegal autopsy was warranted for reasons peripheral to the COVID-19 pandemic, however, she was screened for SARS-CoV-2 prior to autopsy considering her primary residence was in a nursing home. Pre-autopsy nasopharyngeal and throat swabs were positive for SARS-CoV-2.
PMCT images demonstrated bilateral, peripheral and posterior ground glass opacifications involving all lobes of lungs, particularly marked in the apical upper lobes and the right lower lobe, with a degree of traction bronchiectasis. There were zones with increased interstitial markings and a “crazy paving” appearance. There were also more central, bronchocentric consolidations and fluid in the distal trachea and mainstem bronchi, likely representing agonal aspiration or postmortem relocation of gastric contents. The anterior-most and, to a degree, the basal aspects of the lungs were relatively spared. There were bilateral small volume effusions, relatively equal in volume. Otherwise, there was no evidence of any resuscitation efforts. A pacemaker was in situ.
Histologic examination of the lung showed patchy microfoci of acute diffuse alveolar damage characterized by hyaline membrane formation. In other areas of the lung there was aspiration pneumonia characterized by polymorphonuclear cell infiltrates in the alveoli mixed with food particles. Other findings included hypertensive, atherosclerotic and amyloid heart disease and pulmonary emphysema.
3.4. Case 4
This 76 year old man had no known medical history beyond undiagnosed, intermittent unilateral ear pain. He had developed worsening ear pain and fever in the 1–2 weeks prior to his death. He had been treated in the community (via virtual medical appointment/telemedicine) and prescribed amoxicillin that was changed to cefuroxime on the day prior to his death. He collapsed in his bathroom and was assisted to bed where he was described as acutely short of breath and complaining of feeling cold. He was found without vital signs shortly thereafter. Resuscitation was attempted but was not successful. Pre-autopsy nasopharyngeal and throat swabs were positive for SARS-CoV-2.
PMCT images demonstrated diffuse, bilateral ground glass opacifications with increased interstitial markings and a “crazy paving” appearance. The changes were most marked in the posterior lung fields. There were a few scattered foci of more dense consolidation, most conspicuous in the azygos and right upper lobe and situated peripherally in subpleural zones. Traction bronchiectasis could be appreciated. Small zones of the anterior-most aspects of the left upper and right middle and lower lobes were relatively spared. There were bilateral small volume effusions, slightly greater on the right. Otherwise, there were artefacts of attempted resuscitation and an incidental azygos lobe.
Histologic examination revealed diffuse bilateral viral pneumonia with diffuse alveolar damage, reactive pneumocytes and patchy clusters of mononuclear inflammatory infiltrate.
3.5. Case 5
This 51 year old man had a past medical history of diabetes, hypertension, and hyperlipidemia. He was also being treated with warfarin, however the underlying indication for this is not clear. His wife, with whom he resided, reportedly had tested positive for SARS-CoV-2 by nasopharyngeal swab 13 days prior to his death and both had been self-isolating at home per public health guidance. On the day of his death he had felt unwell in the morning, complaining of dizziness. He had multiple syncopal episodes in the mid-afternoon and did not regain consciousness after the final episode. Resuscitation was attempted but was not successful. Emergency medical services noted him to be febrile during their resuscitation efforts. Pre-autopsy nasopharyngeal and throat swabs were positive for SARS-CoV-2.
PMCT images demonstrated diffuse, bilateral mixed ground glass opacifications and foci of consolidation with increased interstitial markings and traction bronchiectasis. Findings predominantly involved posterior and peripheral lung fields, but central involvement was also present. Very small zones of the anterior-most aspects of the right and left upper lobes were relatively spared. No significant effusions were evident. Otherwise, there were artefacts of attempted resuscitation.
Histologic examination of the lungs showed diffuse alveolar damage, reactive type 2 pneumocytes and clusters of mononuclear inflammatory infiltrate. Other findings included chronic atherosclerotic and hypertensive heart disease.
4. Discussion
COVID-19 and other emergent zoonotic infections have challenged the world over the last 20 years. Unprecedented emergent diseases, such as those caused by coronaviruses, and periodically re-emerging diseases like the Ebola virus disease have revealed the lack of global preparedness to manage large-scale health emergencies. Medicolegal systems around the world have been challenged by COVID-19, largely on the basis of limited capacity to respond to managing large numbers of fatalities.
Access to medical autopsies is in decline around the world. This can hamper efforts to study new diseases, such as the novel coronavirus SARS-CoV-2 related disease (COVID-19). However, the medicolegal autopsy has emerged as the last stronghold of the postmortem examination and represents an important institutional contribution of death investigation systems at the time of infectious disease outbreaks. It is now becoming generally recognized that there is a pivotal role for forensic pathology to play in public health [9], [12]. The ability of forensic pathology services to contribute to the understanding of the pathology of COVID-19 by conducting autopsies is a good example of the important role of medicolegal autopsies in public health. Furthermore, autopsies performed on hospitalized patients may provide a skewed picture of the pathology of new diseases due to secondary complications that often arise during intensive care. For example, prolonged recumbency in intensive care units or hospital wards is recognized to cause deep venous thrombosis and fatal pulmonary thromboembolism. Therefore, defining the pathology of a new disease based upon postmortem findings in hospitalized patients presents challenges because some of the findings may not be truly representative of the disease due to modification by secondary processes associated with hospitalization and therapy. Therefore, postmortem examination of unexpected deaths in the community from emerging infectious diseases, such as COVID-19, provide a more complete picture of the natural history and pathology of the disease.
Our study of five fatal cases of COVID-19 in Ontario revealed consistent lung histopathology across all cases. The main histological pattern of lung injury was diffuse alveolar damage with conspicuous hyaline membranes and varying degrees of perivascular mononuclear cell infiltration. Type 2 pneumocyte activation and hyaline membrane formation likely represent the earliest phases of viral insult to the lung with increasing perivascular mononuclear cell infiltration signaling an early stage of fulminant infection. Although reported to be of high incidence in some series [13], there was no pulmonary thromboembolism in any of the reported cases, nor conspicuous evidence of diffuse pulmonary microvascular thrombosis. Detailed histologic and immunohistochemical studies of a larger, prospective postmortem series of COVID-19 cases is currently underway in Toronto. These cases are being preferentially collected from community-based deaths. In-depth study of these cases will clarify the variation in the clinical-pathological spectrum of COVID-19.
One of the most important aspects of this case series was the rather consistent radiologic appearance of the lungs on PMCT. In all cases the radiologic findings in the lung correlated with histopathologic evidence of diffuse alveolar damage. The most consistent PMCT finding was diffuse ground glass opacifications, interstitial changes, and a “crazy paving” appearance with relatively little, if any, spared lung parenchyma. This was distinguishable from postmortem artefacts as it was evident diffusely, not only in a gravity-dependent fashion. Based on this, there is a clear potential to identify fatal cases of SARS-CoV-2 prior to autopsy, as also suggested by Ducloyer et al. [7]. This may be especially useful in the medicolegal setting when community deaths occur and there is a paucity of available medical history or social contacts to alert death investigators to the possibility of COVID-19. If flagged by PMCT as suspicious for COVID-19, this would enable pre-autopsy screening to be performed, appropriate autopsy precautions to be taken, and trigger collection of lower respiratory tract specimens (such as lung tissue samples) for virological studies. Given the well-known limitations of pulmonary radiological findings in the postmortem setting [14], further study would be required to understand the sensitivity and specificity of PMCT for this purpose as, to the author’s knowledge, no such studies exist in the English literature. Interestingly, other authors have suggested correlation between the appearance of the lungs on clinical CT images and the stage of evolution of the underlying acute lung injury [15] and future studies should consider if such radiological-histopathological extrapolations remain valid in the postmortem setting. Further, the features reported in the clinical literature to be commonly correlated with COVID-19 related disease include ground glass opacifications or mixed ground glass opacifications and consolidation, vascular enlargement, traction bronchiectasis, peripheral distribution, bilateral involvement, lower lung predominant, and multifocality [16]. The range of appearances of postmortem artefacts may make such features much less useful in the postmortem setting and attention to these features and their sensitivity/specificity in the postmortem setting would be of value in future studies.
It is important to emphasize that all deaths included in this series were attributed to COVID-19 disease. Alternatively stated, all individuals in this study died of COVID-19 rather than with COVID-19. This underscores two important points about deciding whether COVID-19 was the actual cause of death. First, the pathological features of the lungs are insufficient alone to prove a diagnosis of COVID-19. This is because the basic pattern of most viral pneumonitis is diffuse alveolar damage with varying degrees of active inflammation and viral cytopathic change. It does not appear that the histologic changes alone are sufficient to differentiate between the different viruses that may cause interstitial pneumonitis [17]. Therefore, demonstration of SARS-CoV-2 either by PCR or immunohistochemistry is essential to conclusively establish that the viral pneumonitis pattern evident by microscopy is the result of SARS-CoV-2. Second, the simple presence of SARS-CoV-2 as determined by PCR testing from a nasopharyngeal swab is not sufficient to diagnose fatal COVID-19. On a pathological basis, histological evidence of a viral pneumonitis pattern in addition to confirmation of the presence of the virus is required to establish the diagnosis. Similarly, as previously reported in the literature, so-called “radiologically confirmed” COVID-pneumonia is entirely insufficient to definitively conclude a death was the result of COVID-19 disease [18]. Reliable diagnosis of fatal COVID-19 can only be established by a combination of clinical, radiologic, microbiologic, and histopathologic correlation, with the latter 2 being of the most discerning diagnostic value. An open question at this time is whether or not infection with SARS-CoV-2 can cause extrapulmonary manifestations, such as thrombotic microangiopathy in the absence of interstitial pneumonitis. These answers will become readily apparent as additional autopsies are conducted and the clinicopathological spectrum of COVID-19 is further explored.
Another role for the medicolegal autopsy in the latter stages of the COVID-19 pandemic will be to investigate deaths that may occur after vaccination against the SARS-CoV-2 virus. Specifically, new vaccine technology has been used in this pandemic to formulate mRNA based vaccines to the spike protein of the virus. Although there is no reason to anticipate complications from this new vaccine technology, it will be important to monitor deaths associated with vaccination to determine if any sudden deaths are related to a complication of vaccination, or are simply a coincidence and can be explained by other factors. For example, attempts to create a vaccine against the respiratory syncytial virus resulted in increased morbidity and mortality due to an immunopathological reaction in the lung in children who receive the vaccination [19]. Similarly, immunopathology has been demonstrated to occur in laboratory animals challenged with vaccines developed against the coronaviruses that caused severe respiratory distress syndrome and middle east respiratory distress syndrome [20].
In summary, we have presented the clinical, postmortem radiologic, and pathologic findings in five fatal cases of COVID-19 in Ontario. In all cases, there was viral pneumonitis characterized by diffuse alveolar damage. Our findings underscore the importance of medicolegal autopsies, including PMCT, as a tool to identify, diagnose, and understand the pathology and pathogenesis of new diseases. The COVID-19 pandemic is also an example of how forensic pathology can contribute to public health by aiding in the understanding of the true, pathologically proven morbidity and mortality associated with an emerging disease.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgments
The authors would like to acknowledge the contributions of all of the forensic pathologists, assistants, technologists, administrative staff, coroners and other members of the death investigation team that were involved in investigating these cases.
References
- 1.Barth R.F., Buja L.M., Parwani A.V. The spectrum of pathological findings in coronavirus disease (COVID-19) and the pathogenesis of SARS-CoV-2. Diagn. Pathol. 2020;15:85. doi: 10.1186/s13000-020-00999-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. J. Am. Med. Assoc. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.He F., Deng Y., Li W. Coronavirus disease 2019: what we know? J. Med. Virol. 2020;92:719–725. doi: 10.1002/jmv.25766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edler C., Schröder A.S., Aepfelbacher M., Fitzek A., Heinemann A., Heinrich F., Klein A., Langenwalder F., Lütgehetmann M., Meißner K., Püschel K., Schädler J., Steurer S., Mushumba H., Sperhake J.-P. Dying with SARS-CoV-2 infection-an autopsy study of the first consecutive 80 cases in Hamburg, Germany. Int. J. Leg. Med. 2020;134:1275–1284. doi: 10.1007/s00414-020-02317-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang J., Zheng Y., Gou X., Pu K., Chen Z., Guo Q., Ji R., Wang H., Wang Y., Zhou Y. Prevalence of comorbidities and its effects in coronavirus disease 2019 patients: a systematic review and meta-analysis. Int. J. Infect. Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ducloyer M., Gaborit B., Toquet C., Castain L., Bal A., Arrigoni P.P., Lecomte R., Clement R., Sagan C. Complete post-mortem data in a fatal case of COVID-19: clinical, radiological and pathological correlations. Int. J. Leg. Med. 2020;134:2209–2214. doi: 10.1007/s00414-020-02390-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Suess C., Hausmann R. Gross and histopathological pulmonary findings in a COVID-19 associated death during self-isolation. Int. J. Leg. Med. 2020;134:1285–1290. doi: 10.1007/s00414-020-02319-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Youd E., Moore L. COVID-19 autopsy in people who died in community settings: the first series. J. Clin. Pathol. 2020;19:1–5. doi: 10.1136/jclinpath-2020-206710. [DOI] [PubMed] [Google Scholar]
- 10.Heinrich F., Sperhake J.-P., Heinemann A., Mushumba H., Lennartz M., Nörz D., Glatzel M., Lütgehetmann M., Püschel K. Germany’s first COVID-19 deceased: a 59-year-old man presenting with diffuse alveolar damage due to SARS-CoV-2 infection. Virchows Arch. 2020;477:335–339. doi: 10.1007/s00428-020-02872-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cittadini F., De-Giorgio F., Cina A., Pascali V.L. Reliable postmortem computed tomography scan diagnosis of COVID-19 pneumonia. Am. J. Forensic Med. Pathol. 2020;41:239–240. doi: 10.1097/PAF.0000000000000594. [DOI] [PubMed] [Google Scholar]
- 12.Sperhake J.P. Autopsies of COVID-19 deceased? Absolutely! Leg. Med. 2020;47 doi: 10.1016/j.legalmed.2020.101769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wichmann D., Sperhake J.-P., Lütgehetmann M., Steurer S., Edler C., Heinemann A., Heinrich F., Mushumba H., Kniep I., Schröder A.S., Burdelski C., de Heer G., Nierhaus A., Frings D., Pfefferle S., Becker H., Bredereke-Wiedling H., de Weerth A., Paschen H.-R., Sheikhzadeh-Eggers S., Stang A., Schmiedel S., Bokemeyer C., Addo M.M., Aepfelbacher M., Püschel K., Kluge S. Autopsy findings and venous thromboembolism in patients with COVID-19. Ann. Intern. Med. 2020;173:268–277. doi: 10.7326/m20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Filograna L., Thali M.J. Post-mortem CT imaging of the lungs: pathological versus non-pathological findings. Radiol. Med. 2017;122:902–908. doi: 10.1007/s11547-017-0802-2. [DOI] [PubMed] [Google Scholar]
- 15.Barisione E., Grillo F., Ball L., Bianchi R., Grosso M., Morbini P., Pelosi P., Patroniti N.A., De Lucia A., Orengo G., Gratarola A., Verda M., Cittadini G., Mastracci L., Fiocca R. Fibrotic progression and radiologic correlation in matched lung samples from COVID-19 post-mortems. Virchows Arch. 2020 doi: 10.1007/s00428-020-02934-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao W., Zhong Z., Xie X., Yu Q., Liu J. Relation between chest CT findings and clinical conditions of coronavirus disease (covid-19) pneumonia: a multicenter study. Am. J. Roentgenol. 2020;214:1072–1077. doi: 10.2214/AJR.20.22976. [DOI] [PubMed] [Google Scholar]
- 17.Konopka K.E., Nguyen T., Jentzen J.M., Rayes O., Schmidt C.J., Wilson A.M., Farver C.F., Myers J.L. Diffuse alveolar damage (DAD) resulting from coronavirus disease 2019 infection is morphologically indistinguishable from other causes of DAD. Histopathology. 2020;77:570–578. doi: 10.1111/his.14180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.D’Onofrio V., Donders E., Vanden Abeele M.E., Dubois J., Cartuyvels R., Achten R., Lammens M., Dendooven A., Driessen A., Augsburg L., Vanrusselt J., Cox J. The clinical value of minimal invasive autopsy in COVID-19 patients. PLoS One. 2020;15:1–8. doi: 10.1371/journal.pone.0242300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim H.W., Canchola J.G., Brandt C.D., Pyles G., Chanock R.M., Jensen K., Parrott R.H. Respiratory syncytial virus disease in infants despite prior administration of antigenic inactivated vaccine. Am. J. Epidemiol. 1969;89:422–434. doi: 10.1093/oxfordjournals.aje.a120955. [DOI] [PubMed] [Google Scholar]
- 20.Te Tseng C., Sbrana E., Iwata-Yoshikawa N., Newman P.C., Garron T., Atmar R.L., Peters C.J., Couch R.B. Correction: immunization with SARS coronavirus vaccines leads to pulmonary immunopathology on challenge with the SARS virus. PLoS One. 2012;7 doi: 10.1371/journal.pone.0035421. Erratum in: PLoS One. 7 (2012). doi:10.1371/annotation/2965cfae-b77d-4014-8b7b-236e01a35492. [DOI] [PMC free article] [PubMed] [Google Scholar]