Tectorial membrane injury is uncommon and may be associated with the presence of retroclival epidural hematoma. These authors retrospectively reviewed 10 children with this type of epidural hematoma to determine the rate of tectorial membrane rupture and correlated it with imaging and clinical findings. Seventy percent of subjects showed tectorial membrane damage, none had injuries to the brain stem, spinal cord, vertebrae, or subluxations, and symptoms were minimal. Although most tectorial membrane injuries initially may be managed conservatively, some will necessitate craniocervical fixation to avoid instability.
SUMMARY:
REHs and tectorial membrane injuries are rare complications of pediatric head and neck injuries. We aim to describe the neuroimaging findings in pediatric REHs, to summarize the mechanism of injury, and to correlate the imaging findings with the clinical presentation. We retrospectively evaluated CT and/or MR imaging studies of 10 children with traumatic REH. Most patients were involved in MVAs. The tectorial membrane was injured in 70% of patients, and REHs were medium to large in 80%. None of the patients had a focal spinal cord or brain stem injury, craniocervical junction dislocation, or vertebral fractures. Tectorial membrane disruption was diagnosed in most patients without craniocervical junction−related symptoms. Tectorial membrane lesions and REHs were seen in young children who sustained high-speed head and neck injuries. Clinical symptoms may be minimal or misleading. The radiologist should be aware of these injuries in children. MR imaging appears to be more sensitive than CT.
REH and tectorial membrane injuries are rare complications of traumatic head-neck injuries. Only 1.2%–12.9% of all posterior fossa epidural hematomas are located in the retroclival epidural space.1–5 REHs have only been reported in a few children and even more rarely in the adult population.6,7 Most pediatric traumatic REHs are seen in children involved in MVAs.8 Tectorial membrane disruption has been reported to be 1 of the most important factors resulting in the formation of a REH. None of the previous reports, however, have systematically studied the simultaneous occurrence of REH and tectorial membrane injuries in children.6
Conventional radiography and CT are typically used in acute trauma to exclude injury to the brain or cervical spine. Conventional radiography and CT may, however, not always detect craniocervical junction injuries adequately or may underestimate the degree and extent of injury. MR imaging is the technique of choice for the detailed assessment of craniocervical junction injuries. MR imaging also allows the evaluation of the lower brain stem and cervical spinal cord with higher sensitivity and specificity.6,9
The goals of our report are the following: 1) to describe the CT and MR imaging features in children with confirmed traumatic REH, 2) to specifically assess the frequency of simultaneous REH and tectorial membrane injury, and 3) to correlate the imaging findings with the clinical presentation.
Materials and Methods
Ten children with confirmed REH by CT and/or MR imaging were included in the study. All children had experienced an acute significant head and neck injury and were seen at the Johns Hopkins Hospital between June 2006 and July 2010. The age and sex of all patients were recorded. The electronic patient records were reviewed for the following: 1) the mechanism of trauma (eg, fall, MVA), and 2) clinical signs on the scene or on admission (eg, level of consciousness, focal neurologic deficit, nausea).
CT and MR imaging were performed by using the standard departmental protocols. Axial helical CT datasets were collected from the head and entire cervical spine by using a 64-section CT scanner (Sensation 64; Siemens, Erlangen, Germany). Axial 0.75-mm-thick sections were reconstructed in both soft-tissue and bone algorithms. Additional sagittal and coronal multiplanar reconstructions were calculated from the original dataset. MR imaging was typically performed on a 1.5T MR imaging unit (Avanto, Siemens) by using the head and neck coil. The standard sequences included sagittal and axial T1- and T2-weighted MR imaging sequences as well as T2-weighted STIR sequences. The spatial resolution was optimized for the patient's age, and the section thickness varied between 2.5 and 3 mm. In selected cases, an additional coronal T2-weighted sequence of the craniocervical junction was added. All images were reviewed by 2 experienced pediatric neuroradiologists in consensus.
The CT and MR images were assessed for their overall quality. Images were graded into 3 categories: 1) highly diagnostic: good delineation of all soft tissue and bony structures, no artifacts; 2) moderately diagnostic: most of the anatomic structures identified, however mildly limited image detail, mild degree of artifacts; and 3) low diagnostic quality: poor differentiation between soft tissue and bony structures, significant artifacts obscuring image detail.
The craniocervical junction was evaluated for the integrity of the tectorial membrane and the presence of a REH. The tectorial membrane was considered torn when the normal T2 hypointense band of the membrane was interrupted and stretched when the T2 signal intensity was increased or the intact membrane was elevated by an adjacent REH. Depending on the anteroposterior diameter, we classified the REHs as small (<2 mm), medium (2–4 mm), or large (>4 mm). In addition, we systematically evaluated the superior longitudinal band of the cruciform ligament, anterior atlanto-occipital ligament, apical ligament of the dens, posterior atlanto-occipital membrane, transverse ligament of the atlas, posterior and anterior longitudinal ligaments at the C2-C6 levels, and the cervical ligamentum flavum.
Additionally, we evaluated the presence or absence of the following: 1) focal spinal cord or lower brain stem lesions, 2) craniocervical junction dislocations, 3) osseous lesions (bone marrow edema, fractures), 4) pre- and paravertebral hematomas, and 5) vessel injuries (eg, traumatic dissections).
The brain was evaluated for the presence of extra-axial hemorrhages (epidural, subdural, or subarachnoid), intraparenchymal contusions and hematomas, and shear injuries.
We reviewed patients' medical records for the following: 1) the mechanism of trauma (eg, fall, MVA), 2) clinical signs on the scene or on admission (eg, level of consciousness, focal neurologic deficit, nausea), 3) performed treatment (eg, conservative with neck collar versus surgery), and 4) global outcome.
Results
Ten patients (6 females, 4 males), 21 months to 15 years of age (median age, 6 years) were included in the study. The mechanism of trauma, clinical signs/symptoms on admission, applied diagnostic technique (CT/MR imaging), associated injuries, treatment, and outcome of all patients are summarized in the Table.
Mechanism of trauma, diagnostic modality, clinical signs and symptoms on admission, associated injuries, treatment, and outcome in 10 children with traumatic REH
| No. | Sex/Age | Mechanism of Injury | Diagnostic Modality | Clinical Signs/Symptoms on Admission | Associated Injuries | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | M/4 yr | MVA | CT/MR | GCS score, 6; left sixth cranial nerve palsy | Multiple skull fractures; intraparenchymal and subdural hematoma; shear injuries; left internal carotid artery dissection; transverse ligament injury | Conservative (Miami J collar) | Neurologic impairment related to DAI |
| 2 | F/15 yr | Cattle roping | CT/MR | GCS score, 7 | Intracranial hematoma; cerebral contusions; extra-axial hemorrhage; shear injuries | Conservative (Miami J collar) | Neurologic impairment related to DAI |
| 3 | M/6 yr | Fall | CT | GCS score, 15; unremarkable | Stretched tectorial membrane; apical ligament injury; mild compression of the brain stem | Conservative | Full recovery |
| 4 | F/9 yr | MVA | CT/MR | GCS score, 6; left fourth, sixth, tenth, twelfth cranial nerve palsy; paresis of the left arm; bilateral upgoing toes | Tectorial membrane disruption; left occipital condylar fracture with subluxation of C-spine; moderate compression of the brain stem; intraparenchymal hematoma; cerebral contusion, extra-axial hemorrhage | Surgical fixation C0-C2 | Neurologic impairment related to DAI |
| 5 | F/6 yr | MVA | CT/MR | GCS score, 13; nausea, headache; bilateral sixth, ninth, twelfth cranial nerve palsy | Tectorial membrane disruption | Conservative (Miami J collar) | Full recovery |
| 6 | F/21 mo | Fall | CT/MR | GCS score, 14; nausea, headache | Tectorial membrane disruption; skull fracture; extra-axial hemorrhage; apical ligament injury | Conservative (Miami J collar) | Full recovery |
| 7 | M/13 yr | Go-cart accident | CT | GCS score, 15; mild nausea | Stretched tectorial membrane; left occipital condylar fracture | Conservative (Miami J collar) | Full recovery |
| 8 | F/6 yr | MVA | CT/MR | GCS score, 15; cervical pain | Tectorial membrane disruption; mild compression of the brain stem | Conservative (Miami J collar and thoracic lumbar sacral orthosis brace) | Full recovery |
| 9 | F/9 yr | MVA | CT/MR | GCS score, 5 | Stretched tectorial membrane | Conservative (Miami J collar) | Full recovery |
| 10 | M/2 yr | Car versus pedestrian | CT/MR | GCS score, 13; left femur fracture | Apical and posterior atlanto-occipital membrane injury; skull fracture | Conservative (Miami J collar) | Full recovery |
Six patients had experienced MVAs (60%), and 3 were injured by falls (30%). One patient had a cattle rope accident. The clinical symptoms on the scene or on admission were mild in 5 patients (transitory concussive symptoms, mild nausea, and minor pain). Three patients were unconscious at the scene (GCS score, 6–7) and arrived intubated to the hospital. Two patients presented with symptoms suggestive of craniocervical junction injury: lower cranial nerve palsies (IX, X, and XII).
All 10 patients underwent CT examinations on arrival. Most CT studies were highly diagnostic (n = 8, 80%). Two studies were graded as moderately diagnostic (n = 2, 20%). Acute MR imaging (within 48 hours) was performed in 8 patients. The studies were graded as highly diagnostic in 5 (62.5%) and moderately diagnostic in 3 (37.5%) patients.
Overall, tectorial membrane injury was diagnosed by CT or MR imaging in 7 children (70%). Tectorial membrane injury (disruption and/or stretching) was shown by CT in 3 (3/10, 30%) and by MR imaging in 5 (5/8, 62.5%) patients. Tectorial membrane stretching was seen in 1 patient on CT and was confirmed by MR imaging. The other 2 stretched tectorial membranes that were seen on CT did not have an MR imaging confirmation.
MR imaging showed disruption of the tectorial membrane in 4 patients (4/8, 50%). CT showed a raised (stretched) tectorial membrane (clival detachment) in 3 (3/10, 30%), whereas MR imaging showed tectorial membrane stretching in 1 patient (1/8, 12.5%) (Figs 1–3). A REH was present in all cases: It was seen by CT in 9 (9/10, 90%) and by MR imaging in 8 children (8/8, 100%). Two of the REHs were classified as small (2/10, 20%); 5, as medium (5/10, 50%); and 3, as large (3/10, 30%). Disruption was seen in the following craniocervical ligaments: the apical ligament of the dens in 4 (4/10, 40%) and the anterior atlanto-occipital and transverse ligaments of the atlas in 1 patient (1/10, 10%), respectively.
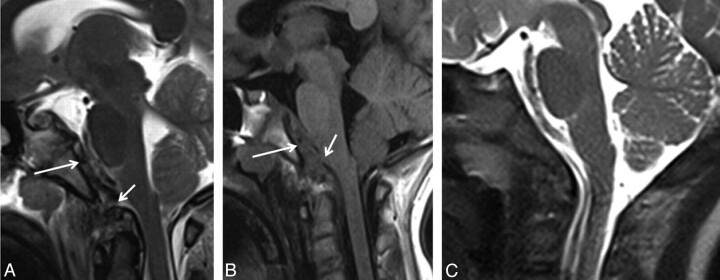
Fig 1.
Sagittal T2- (A) and T1-weighted (B) MR images of a 9-year-old girl (patient 4) who presented with craniocervical junction−related symptoms after an MVA show a REH (white arrow) with associated tectorial membrane disruption (short white arrow) and posterior dislocation of the dens. C, Sagittal T2-weighted MR image of an age-matched healthy control patient for comparison.
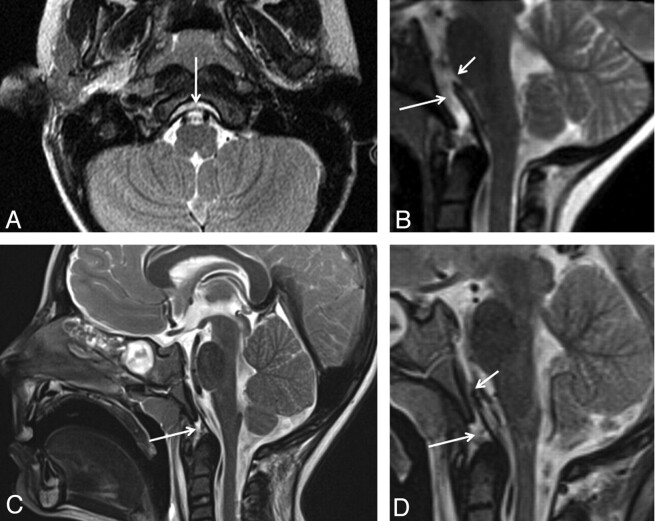
Fig 2.
A, Axial T2- weighted MR image of a 6-year-old girl (patient 5) who presented with craniocervical junction−related symptoms (GCS = 13) after a MVA shows a retroclival hyperintense fluid collection with stretching of the tectorial membrane (white arrow). B, Sagittal T2-weighted image of a 6-year-old girl (patient 8) who presented with cervical pain (GCS = 15) after an MVA demonstrates REH (white arrow) and an associated tectorial membrane disruption (short white arrow). C and D, Sagittal T2-weighted MR images of a 4-year-old boy (patient 1) who presented with a sixth cranial nerve palsy (GCS = 6) after a MVA shows an apical ligament injury (white arrow) with associated tectorial membrane disruption (D, short white arrow).
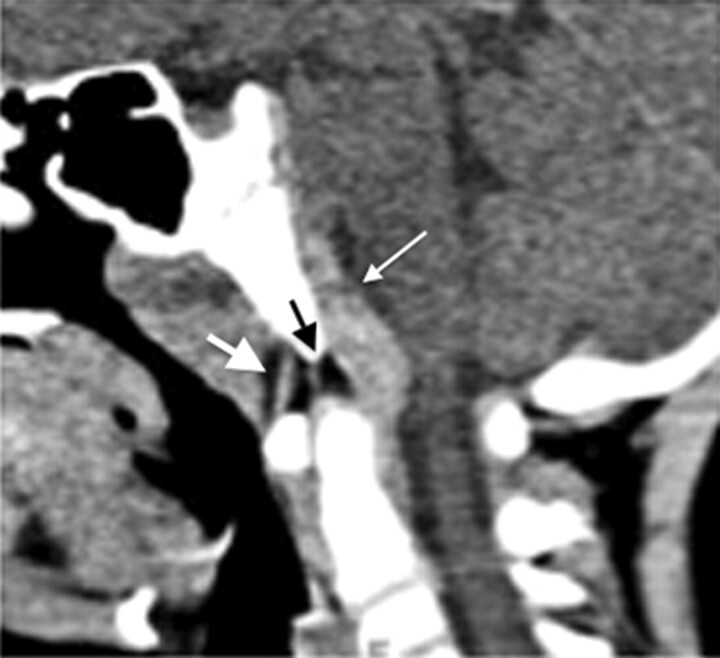
Fig 3.
Sagittal reconstruction of a CT scan of a 6-year-old boy (patient 3) after a fall (GCS = 15) demonstrates an REH (thick white arrow), which causes mild compression of the spinal cord. CT scan also shows the anterior atlanto-occipital ligament (thin white arrow) and a suspected apical ligament disruption (black arrow).
In none of the patients was a focal spinal cord or brain stem injury, craniocervical junction dislocation, or vertebral fracture detected. MR imaging showed bone marrow edema involving the upper cervical vertebral bodies in 4 patients (4/8, 50%). Paravertebral soft-tissue edema and hematomas were seen by CT in 4 (4/10, 40%) and by MR imaging in 7 (7/8, 87.5%) patients. In 1 patient, MR imaging showed left internal carotid artery dissection (1/8, 12.5%). The ventral perimedullary cisterns and lower brain stem appeared mildly effaced/compressed on CT in 4 (4/10, 40%) and on MR imaging in 3 patients (3/8, 37.5%) (Fig 1A, -B; Fig 2A, -B; and Fig 3)
MR imaging showed extra-axial hemorrhages in 5 patients (5/8, 62.5%) and intraparenchymal contusions, intraparenchymal hematomas, and shear injuries in 3 (3/8, 37.5%), respectively. CT demonstrated extra-axial hemorrhages in 3 patients (3/10, 30%), intraparenchymal contusions in 2 patients (2/10, 20%), intraparenchymal hematomas in 3 patients (3/10, 30%), and shear injuries in 1 patient (1/10, 10%).
Tectorial membrane disruption was diagnosed in all patients (2/2) with clinical symptoms suggestive of craniocervical junction injury and in 62.5% (5/8) of patients without craniocervical junction symptoms.
Most patients were treated conservatively with a neck collar (Miami J; Össur, Foothill Ranch, California). One patient had an occipitocervical fixation (C0-C2). In 6 patients, the outcome was excellent without focal deficits or craniocervical junction instability. Three patients with diffuse axonal injury required neurorehabilitation (Table). The GCS score on admission did not correlate with the imaging findings.
Discussion
Tectorial membrane injury with development of an REH is a rare entity in the pediatric population. High-speed MVAs are the predominant cause of injury, as was also shown in our case series. Young children are more at risk for cervical injury, especially in the occipitoatlantoaxial region.10 Age-specific anatomic and biomechanical characteristics of the developing pediatric craniovertebral junction predispose children to injuries in this region. Specifically, the pediatric neck musculature is relatively weak, the pediatric head is large and heavy in relation to the torso, the occipital condyles are smaller in children than in adults, and the pediatric ligaments are laxer. The resulting relative craniocervical junction hypermobility increases the risk for ligamentous craniocervical junction injuries in children. Abrupt acceleration/decelerations in combination with craniocervical junction hyperextension/hyperflexion (eg, in MVAs) is believed to be causative of pediatric tectorial membrane injury with REH.11
The tectorial membrane, transverse ligament, and alar ligaments play an important role in stabilizing the craniocervical junction. The tectorial membrane, a superior extension of the posterior longitudinal ligament, extends to the anterior margin of the foramen magnum and covers the caudal portion of the clivus. The tectorial membrane is the major craniocervical stabilizer and plays an essential role in the pathogenesis of REH.12 The postulated mechanism for tectorial membrane injury is sagittal dislocation of the odontoid process associated with disruption of the transverse ligament that detaches the tectorial membrane from the clivus. In children, the dura matter and tectorial membrane are not firmly attached to the skull; stripping tectorial membrane injury could result in traction damage to the adjacent vascular structures such as the basilar venous plexus and dorsal meningeal branch of the meningohypophyseal trunk. This may result in the accumulation of blood in the retroclival epidural space.1,11,13 Based on this postulated mechanism, tectorial membrane tear is the most likely causative factor for the occurrence of REH.
Although, to our knowledge, the imaging characteristics of tectorial membrane injuries have not yet been systematically described, ligamentous injuries can be directly evaluated in MR imaging. Overt disruption is represented by a loss of tectorial membrane continuity. Indirect features of tectorial membrane injuries are stretching and detachment, with elevation of the membrane from the clivus and a simultaneous fluid collection extending to the apex of the dens. In our patients, the tectorial membrane was injured in 70% of cases. CT did not allow direct visualization of tectorial membrane disruption, and the diagnosis of tectorial membrane injury relied on elevation of the tectorial membrane by a REH. As expected, MR imaging had better sensitivity for the diagnosis of tectorial membrane injury in our series and was also able to differentiate tectorial membrane disruption and stretching. The paucity of publications studying traumatic REH and tectorial membrane injury suggests, however, that these lesions are being under-recognized. The retroclival area should consequently always be included in the imaged volume when performing MR imaging evaluation of the craniocervical junction, and the radiologist should actively rule out a REH, especially if the child was involved in a high-speed MVA.
An additional benefit of MR imaging is its ability to better diagnose and delineate associated craniocervical junction injuries. Paravertebral soft-tissue edema and hematomas were more frequently seen on MR imaging compared with CT. MR imaging also allowed identification of a vascular dissection localized in the petrous segment of the left internal carotid artery in 1 patient, which had been undetected on CT angiography. In addition, STIR imaging is highly sensitive for the identification of bone marrow edema. In our series, MR imaging identified bone marrow edema in 50% of patients. This information may facilitate detection of adjacent craniocervical junction ligamentous injuries.
Most interesting, in none of our patients was a focal spinal cord or brain stem lesion noted. The REH effaced the perimedullary cisterns and lower brain stem in 4 patients. One patient had multiple cranial nerve palsies associated with subtle left upper limb paresis. The patient also had multiple cerebral shear injuries, but no spinal cord lesion or cervicomedullary junction injury was seen.
In addition, craniocervical junction dislocation was only seen in 1 patient of our group who had a simultaneous occipital condylar fracture. In all other patients, no craniocervical junction dislocation or vertebral fracture was seen, despite the fact that skull and skull base fractures were detected in 5 patients. Tubbs et al6 had reported an association with craniocervical junction dislocation and spinal cord injury. This may be explained by the larger mobility and ligamentous flexibility of the craniocervical junction in children, which indirectly “protects” the osseous structures of the craniocervical junction but enhances ligamentous injuries. In addition, differences in the mechanism of trauma (rollover versus direct impact), speed on impact, kind of restraining devices, and the smaller sample size may also explain our relative lack of associated craniocervical junction and spinal cord injuries.
Most of our patients (80%) had medium-to-large-sized REHs diagnosed on imaging studies. The primary treatment in isolated cases without fractures is conservative; however, because the retroclival space has a potential for rapid blood accumulation, close imaging follow-up is important.
The percentage of highly diagnostic MR imaging studies was slightly lower compared with the CT studies. This difference may be explained by the longer acquisition times of MR imaging as well as the higher sensitivity for artifacts related to external devices such as neck collars.
Most interesting, higher rates of patients who had no craniocervical junction−related symptoms on admission were diagnosed with craniocervical junction injuries on diagnostic imaging studies. Moreover, these patients presented with no neurologic deficits and minimal clinical findings. This fact is of crucial importance because it illustrates how critical findings such as craniocervical junction injuries can go clinically undetected.
Only 1 patient underwent a C0-C2 surgical fixation. Most patients were managed conservatively. This finding is in agreement with previous reports that showed that conservative management should be the first line of treatment for nondislocated craniocervical junction injuries without fractures.6
One significant limitation of our study is the selection bias. We studied children with a CT-and/or MR imaging−confirmed REH. Consequently, the true incidence of traumatic REH and tectorial membrane injury cannot be determined. In addition, small tectorial membrane injuries may have been overlooked. Future studies should systematically evaluate large series of children who sustained high-speed head and neck injuries to better estimate the true incidence of tectorial membrane injuries and REHs. In addition, due to the retrospective design of our study, the mechanism of injury and the initial and follow-up clinical signs and symptoms have not been systematically recorded. Moreover, no high-resolution imaging studying the craniocervical ligaments and no serial follow-up examinations have been collected. Hence, we were not able to determine the short- and long-term sequelae of craniocervical injury, the temporal evolution of REHs, the recovery of ligamentous injury, the degree of residual craniocervical stability, and the degree of accelerated degenerative disease of the cervical spine.14
The paucity of articles discussing the occurrence of tectorial membrane injuries in children after high-speed MVAs suggests that these injuries are frequently underestimated or even overlooked. Injury of the tectorial membrane and other craniocervical junction ligaments may have a significant impact on the stability of the craniocervical junction. The presence of tectorial membrane disruption on MR imaging should raise the suspicion of a potential craniocervical instability. Moreover, the documentation of ligamentous injury may aid in the decision to immobilize the patient, because ligamentous injuries generally heal poorly with immobilization, or to perform surgical stabilization.
In the light of our results, we emphasize the importance of a systemic and thorough evaluation of the craniocervical junction in children admitted to the emergency department after high-speed injuries. In such circumstances, high-resolution CT and/or MR imaging studies should rule out tectorial membrane injuries and REH. If only a head CT is performed, the craniocervical junction should be included. Similarly, if a cervical spine study is requested, the craniocervical junction should also be included. In addition, if a CT study is performed, we recommend reconstruction of sagittal soft-tissue and bone algorithm images of the craniocervical junction. A high window-level setting may facilitate detection of a hyperattenuated REH next to the hyperattenuated osseous clivus. MR imaging should be performed in all patients suspected of a craniocervical junction injury. Sagittal images are especially beneficial to study the craniocervical junction, high-resolution heavily T2-weighted sequences may allow study of the multiple ligaments of the craniocervical junction, and STIR images may show posttraumatic bone marrow edema.
Conclusions
Tectorial membrane injuries and REH are typically seen in young children who sustain a high-speed head and neck injury. The higher mobility of the pediatric craniocervical junction compared with that in adult patients is believed to facilitate craniocervical junction injuries. The radiologist should be aware of these kinds of injuries in the pediatric population. CT and MR imaging studies should always include this region when the mechanism of trauma is suggestive of craniocervical junction injury. Sagittal soft-tissue and bone algorithm reconstructions are helpful to identify these lesions on CT studies. MR imaging is more sensitive than CT and allows thorough evaluation of craniocervical junction ligaments in better detail. Clinical symptoms may be minimal or misleading.
Abbreviations
- DAI
diffuse axonal injury
- GCS
Glasgow Coma Scale
- MVA
motor vehicle accident
- REH
retroclival epidural hematoma
- STIR
short T1 inversion recovery
Footnotes
Disclosures: Ayelet Eran: Consultant: Orsan Medical Technologies.
References
- 1. Ratilal B, Castanho P, Vara Luiz C, et al. Traumatic clivus epidural hematoma: case report and review of the literature. Surg Neurol 2006;66:200–02 [DOI] [PubMed] [Google Scholar]
- 2. Cordobes F, Lobato RD, Rivas JJ, et al. Observations on 82 patients with extradural hematoma: comparison of results before and after the advent of computerized tomography. J Neurosurg 1981;54:179–86 [DOI] [PubMed] [Google Scholar]
- 3. Hooper R.. Observations on extradural haemorrhage. Br J Surg 1959;47:71–87 [DOI] [PubMed] [Google Scholar]
- 4. Jamieson KG, Yelland JD.. Extradural hematoma: report of 167 cases. J Neurosurg 1968;29:13–23 [DOI] [PubMed] [Google Scholar]
- 5. McKissock W, Taylor JC.. A comparison of supratentorial intracranial meningiomas operated upon with and without induced hypothermia. Br J Surg 1960;48:155–57 [DOI] [PubMed] [Google Scholar]
- 6. Tubbs RS, Griessenauer CJ, Hankinson T, et al. Retroclival epidural hematomas: a clinical series. Neurosurgery 2010;67:404–06 [DOI] [PubMed] [Google Scholar]
- 7. Coleman CC.. War wounds of the nervous system. Ann Surg 1941;113:712–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Agrawal D, Cochrane DD.. Traumatic retroclival epidural hematoma: a pediatric entity? Childs Nerv Syst 2006;22:670–73 [DOI] [PubMed] [Google Scholar]
- 9. Yama N, Kano H, Nara S, et al. The value of multidetector row computed tomography in the diagnosis of traumatic clivus epidural hematoma in children: a three-year experience. J Trauma 2007;62:898–901 [DOI] [PubMed] [Google Scholar]
- 10. Sun PP, Poffenbarger GJ, Durham S, et al. Spectrum of occipitoatlantoaxial injury in young children. J Neurosurg 2000;93:28–39 [DOI] [PubMed] [Google Scholar]
- 11. Kwon TH, Joy H, Park YK, et al. Traumatic retroclival epidural hematoma in a child: case report. Neurol Med Chir (Tokyo) 2008;48:347–50 [DOI] [PubMed] [Google Scholar]
- 12. Werne S.. Studies in spontaneous atlas dislocation. Acta Orthop Scand Suppl 1957;23:1–150 [PubMed] [Google Scholar]
- 13. Mizushima H, Kobayashi N, Sawabe Y, et al. Epidural hematoma of the clivus: case report. J Neurosurg 1998;88:590–93 [DOI] [PubMed] [Google Scholar]
- 14. Benedetti PF, Fahr LM, Kuhns LR, et al. MR imaging findings in spinal ligamentous injury. AJR Am J Roentgenol 2000;175:661–65 [DOI] [PubMed] [Google Scholar]