SUMMARY:
Palatal tumors are often treated with palatectomy or maxillectomy. The resulting surgical defect produces an oroantral communication. An obturator is a removable prosthesis used to close the palatal or maxillectomy defect. Fifteen patients who had undergone palatectomy or maxillectomy for carcinoma and subsequent obturator prosthesis placement were retrospectively studied. Obturators were characterized by Hounsfield units and were subdivided into 3 CT imaging groups: either hyperattenuated, hollow (air-containing), or heterogeneous (isoattenuated to hyperattenuated with internal foci of air). Eight patients had hyperattenuated obturators either representing acrylic resin or Trusoft. Four patients had hollow obturators also composed of acrylic resin or Trusoft. Three patients had heterogeneous obturators, which were composed of only Trusoft. The postoperative imaging of patients treated for palatal or maxillary tumors can be complicated by the presence of obturator prostheses. The intent of this article was to familiarize the reader with the CT imaging features of obturator prostheses.
Patients with palatal or maxillary carcinoma may be treated with palatectomy or maxillectomy, which can result in significant functional and cosmetic impairment. The hard and soft palates are structures that have important roles in speech and deglutition.1 Maxillary defects may produce hypernasal or incomprehensible speech due to alterations in sound production intraorally or may result in intranasal reflux with liquid or food entering the maxillary sinuses and nasal cavity.2
Obturator prosthetic rehabilitation is divided into 3 types, including the surgical obturator, the interim obturator, and the definitive obturator.3 The surgical obturator is placed immediately after surgery to close the surgical defect, support the surgical packing material, and reduce the incidence of oral contamination of the wound. The interim obturator is placed on approximately postoperative days 5–10. This is worn until the wound is completely healed. Finally, a definitive obturator is placed 3–6 months after surgery.3 Obturators at our institution are composed of Trusoft (H.J. Bosworth Co, Skokie, Illinois) or acrylic resin material. Trusoft is a pliable rubbery material, typically used in interim obturator fabrication. Acrylic resin obturators are constructed from acrylic resin, which is a hard typically pink plastic that is commonly used to construct dentures and definitive obturators.
Obturators are often inadvertently left in place when patients undergo postoperative surveillance CT imaging. Obturators have a complex and varied appearance, which may make interpretation of postoperative imaging difficult. The purpose of our study was to familiarize the reader with the CT imaging appearances of obturators.
Case Series
Materials and Methods
A retrospective analysis of 15 patients at our institution who had undergone palatectomy or maxillectomy for carcinoma and subsequent obturator prosthesis placement was performed with axial contrast-enhanced CT (120–140 kV[peak]; 220 mA; section thickness, 1.25 mm). The obturators were subdivided into 3 groups based on CT imaging features: hyperattenuated, hollow (air-containing), or heterogeneous (isoattenuated to hyperattenuated with internal foci of air). The internal densities of the obturators were measured by CT Hounsfield units. The images were reviewed by 2 head and neck radiologists (V.A.K. and L.E.G.). CT Hounsfield unit attenuation values of the obturators were obtained by region-of-interest analysis at the center of the obturator. Approval for this retrospective Health Insurance Portability and Accountability Act−compliant study was obtained from the Institutional Board of Research Associates, with waiver of informed consent.
Results
Eight patients had hyperattenuated obturators (range, +105 to +155 HU; mean, +126 ± 15 HU), either constructed of acrylic resin or Trusoft material. Three patients had heterogeneous obturators (range, +44 to +72 HU; mean, +60 ± 14 HU), which were composed of Trusoft. Four patients had air-containing hollow obturators (range, −935 to −989 HU; mean, −963 ± 23 HU) composed of either acrylic resin or Trusoft (Table). In 1 case, a hyperattenuated Trusoft obturator was confused with an enhancing tumor recurrence (Fig 1).
CT imaging appearance of obturator prostheses
| Patient No. | Age (yr) | Sex | Tumor Type | Surgery Type | Obturator | Imaging Appearance | HU |
|---|---|---|---|---|---|---|---|
| 1 | 71 | M | Recurrent columella cancer | Limited maxillectomy and palatectomy | Acrylic | Hyperdense | 105 |
| 2 | 53 | M | Palate SCC | Subtotal maxillectomy | Trusoft | Hyperdense | 116 |
| 3 | 69 | M | Malignant spindle cell sarcomtaoid cancer of maxillary sinus | Subtotal maxillectomy | Acrylic | Hyperdense | 116 |
| 4 | 68 | M | Adenoid cystic carcinoma of palate | Subtotal maxillectomy | Trusoft | Hyperdense | 136 |
| 5 | 74 | M | SCC of maxilla | Subtotal maxillectomy | Acrylic | Hyperdense | 134 |
| 6 | 21 | F | Maxillary epitheloid hemangioendothelioma | Subtotal maxillectomy | Acrylic | Hyperdense | 124 |
| 7 | 83 | F | SCC of maxilla | Complete maxillectomy | Acrylic | Hyperdense | 155 |
| 8 | 32 | F | Mucoepidermoid carcinoma of the palate | Partial palatectomy | Acrylic | Hyperdense | 123 |
| 9 | 82 | M | Melanoma of sinonasal cavity | Subtotal maxillectomy | Trusoft | Heterogeneous | 72 |
| 10 | 83 | F | Lymphoma of the sinonasal cavity with palatal fistula | Partial palatectomy | Trusoft | Heterogeneous | 44 |
| 11 | 56 | M | Mucoepidermoid Ca of palate | Subtotal maxillectomy | Trusoft | Heterogeneous | 64 |
| 12 | 62 | M | SCC of maxilla | Total maxillectomy | Hollow | Air | −960 |
| 13 | 43 | M | Radiation-induced sarcoma of maxilla | Subtotal maxillectomy | Hollow | Air | −989 |
| 14 | 79 | F | Maxillary alveolar ridge carcinoma | Subtotal maxillectomy | Hollow | Air | −971 |
| 15 | 69 | F | Maxillary carcinoma | Subtotal maxillectomy | Hollow | Air | −935 |
Fig 1.
A and B, A 32-year-old woman status post partial palatectomy for mucoepidermoid Ca and placement of a Trusoft obturator at the palatal defect (black arrow). The obturator bulb (white arrow) is seen extending to the level of the left choana. The bulb is the part of the obturator that inserts into the palatal defect. The postcontrast CT image shows the rounded hyperattenuated appearance of this obturator bulb, which was mistaken for enhancing tumor recurrence.
Discussion
Palatal tumors are often treated with palatectomy or maxillectomy. The surgical defect produces an oroantral communication. An obturator is a removable prosthesis used to close the palatal defect and improve the anatomy and function of the palate. Obturators are composed of different materials such as Trusoft and acrylic resin.
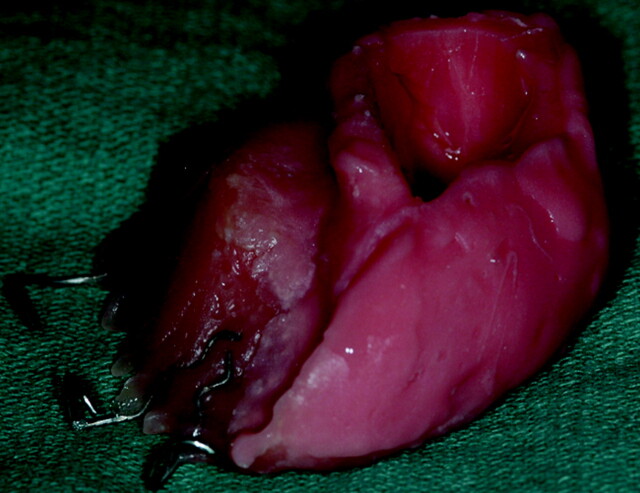
Trusoft is a denture tissue conditioner that is a soft pliable material often used in interim obturators (Fig 2). It comes as a liquid and powder composed of polymethylmethacrylate with a plasticizer and is mixed in the clinic and contoured intraorally. It is molded over a thin plate of acrylic resin, which acts as a support base. Trusoft obturators may have a heterogeneous appearance (isoattenuated to hyperattenuated with internal foci of air) or a hyperattenuated appearance. If foci of air are trapped within the Trusoft obturator, the CT appearance may be perplexing and potentially can be mistaken for focal infection (Fig 3). In most cases, these Trusoft obturators, while appearing unusual on CT, are correctly diagnosed as foreign-body prostheses (Fig 4). If no air is trapped in the Trusoft obturator, it has a hyperattenuated uniform appearance. A hyperattenuated Trusoft obturator has a CT appearance that can be confused with enhancing tumor recurrence (Fig 1).
Fig 2.
The interim obturator is constructed primarily of Trusoft and is formulated to remain soft for 6–10 weeks. The elasticity of Trusoft ensures against pressure pain. It is adjusted and contoured approximately every 2 weeks as the surgical site heals.
Fig 3.
An 83-year-old woman with sinonasal lymphoma status post chemoradiation therapy, who developed osteoradionecrosis and underwent partial palatectomy and Trusoft obturator placement. A postcontrast CT image shows that the obturator projects into the right nasal cavity (arrow). Foci of air may get trapped in the Trusoft obturator, creating a confusing imaging appearance, which can be mistaken for infection.
Fig 4.
Axial postcontrast CT images demonstrate 2 other examples of patients status post maxillectomy for tumor resection, with Trusoft obturators (arrows) containing trapped internal foci of air.
Acrylic resin obturators are constructed from a hard pink plastic material that is commonly used to construct dentures (Fig 5). It comes as a powder and liquid that is cured and processed in stone molds in a laboratory. If the patient is partially or completely edentulous, denture teeth may also be incorporated into the obturator design. The CT appearance of acrylic resin obturators is uniformly hyperattenuated (Fig 6). We found that hyperattenuated Trusoft obturators and hyperattenuated acrylic resin obturators were sometimes difficult to distinguish by visualization and by CT Hounsfield unit measurements. When the surgical site has had adequate time to heal, the mold of the Trusoft interm obturator can be “jumped” or converted into an acrylic resin definitive obturator.
Fig 5.
An example of a definitive obturator made of acrylic resin, with a closed hollow obturator bulb (arrow) molded to fill the palatal defect.
Fig 6.
A 21-year-old woman with maxillary hemangioendothelioma status post left subtotal maxillectomy (left image) and subsequent acrylic obturator placement (right image with arrow), as shown on axial postcontrast CT images.
Hollow obturators can be made of Trusoft or acrylic resin and can be used as interim obturators and definitive obturators. If the patient has a large maxillectomy or palatal defect, a sizeable obturator can be created to fill the defect. However, large obturators can be heavy and uncomfortable for the patient. They can be hollowed to decrease their weight (Fig 7). Hollow obturators can be designed with open (Fig 2) or closed (Fig 5) bulbs. The bulb is the part of the obturator that inserts into the maxillary or palatal defect. Patients with open bulbs may have food or fluid accumulation within the bulb, which can result in halitosis. To prevent debris accumulations in open hollow obturator bulbs, a closed obturator bulb can be constructed.
Fig 7.
A 69-year-old patient with SCC of the right maxilla status post subtotal maxillectomy. An axial postcontrast CT image shows a hollow obturator (arrow) in place.
Conclusions
We observed 3 CT imaging features of obturators: hyperattenuated, heterogeneous, and hollow. Hyperattenuated or hollow obturators were fabricated with either Trusoft or acrylic resin material. The heterogeneous obturators studied were composed of Trusoft only. Patients may be reluctant to remove obturators when undergoing follow-up CT imaging. However, it is important that radiologists instruct CT technologists to have patients remove their obturator prosthesis. If the obturator is left in, familiarity with the various appearances of obturator prostheses is useful in evaluating patients following maxillary or palatal resections. This may improve visualization of subtle tumor recurrence and avoid the potential misdiagnosis of hyperattenuated obturators as tumors and heterogeneous obturators as focal infections.
Abbreviations
- Ca
cancer
- SCC
squamous cell carcinoma
Footnotes
Paper previously presented at: 43rd Annual Meeting of the American Society of Head and Neck Radiology, September 9–13, 2009; New Orleans, Louisiana.
References
- 1. Ortegon SM, Martin JW, Lewin JS. A hollow delayed surgical obturator for a bilateral subtotal maxillectomy patient: a clinical report. J Prosthet Dent 2008;99:14–18 [DOI] [PubMed] [Google Scholar]
- 2. Keyf F. Obturator prostheses for hemimaxillectomy patients. J Oral Rehabil 2001;28:821–29 [DOI] [PubMed] [Google Scholar]
- 3. Beumer J, III, Curtis TA, Marunick MT. Maxillofacial Rehabilitation: Prosthodontic and Surgical Considerations. St. Louis: Ishiyaku EuroAmerica; 1996:240–85 [Google Scholar]