Abstract
BACKGROUND AND PURPOSE:
Dural fistulas with cortical venous drainage often present with hemorrhage or neurologic deficit, and prompt treatment is indicated. Occlusion of the draining vein by endovascular techniques or surgical disconnection is considered curative. We present our first endovascular experience with use of Onyx via the arterial route in these aggressive fistulas.
MATERIALS AND METHODS:
Between October 2008 and October 2009, 8 consecutive patients with a dural fistula with exclusive cortical venous drainage were treated with Onyx. Three patients presented with hemorrhage; 3, with hemianopsia; 1 with bruit; and 1 after incomplete coil occlusion of a benign sigmoid sinus dural fistula. Fistula location was the sigmoid sinus segment in 4, the occipital area in 2, the cavernous sinus in 1, and the torcula in 1.
RESULTS:
In all 8 patients, it was possible to occlude the proximal venous site of the fistula with Onyx via arterial feeders, resulting in complete cure in all. In 6 patients, a prolonged (17- to 29-minute) single middle meningeal artery injection was sufficient to occlude the venous site of the fistula with retrograde occlusion of other arterial feeders; in the other 2 patients, 2 injections in supplying arteries were needed. Follow-up angiograms after 6–12 weeks confirmed lasting complete occlusion of the fistulas. All patients were clinically cured, there were no complications.
CONCLUSIONS:
In this small series, curative embolization of dural fistulas with exclusive cortical venous drainage by using Onyx via the arterial route was possible in all patients.
Intracranial DAVFs with retrograde cortical venous drainage are aggressive lesions that can present with intracranial hemorrhage, seizures, progressive neurologic deficit, intracranial hypertension, or dementia.1–4 Because the natural history of untreated lesions is associated with a poor prognosis, prompt treatment is indicated.5,6 Dural fistulas are considered multiple-hole fistulas with multiple arterial feeders draining into 1 single vein. Treatment of DAVFs with cortical venous drainage is aimed at occlusion of the venous drainage or occlusion of all arterial supply and can be surgical, endovascular, or a combination.7–13 Endovascular treatment has traditionally included embolization via an arterial or venous route with use of acrylic glue, particles, coils, or a combination. Recently, the use of Onyx (ev3, Irvine, California) via the arterial route has been reported with promising results.14–18 We report our initial experience with arterial injection of Onyx in the endovascular treatment of dural fistulas with drainage exclusively into the cortical veins.
Materials and Methods
Between October 2008 and October 2009, 8 consecutive patients with dural fistulas with exclusive cortical venous drainage were treated with Onyx. Patient characteristics are summarized in the Table. There were 5 men and 3 women with a mean age of 57 years (range, 36–67 years). Three patients presented with hemorrhage; 3, with hemianopsia; and 1, with bruit. One patient was referred after incomplete coil occlusion of a benign sigmoid sinus dural fistula with residual shunt on a trapped sinus segment. Fistula location was the sigmoid sinus segment in 4, the right occipital area in 2, the left cavernous sinus in 1, and the torcula in 1. Diagnosis was confirmed after angiography of all cerebral vessels on a biplane angiographic unit (Integris Allura Neuro; Philips Healthcare, Best, the Netherlands).
Patient and treatment characteristics of 8 patients with DAVFs with exclusive cortical venous drainage that were treated with intra-arterial Onyx injection
| No./Sex/Age (yr) | Presentation | DAVF Location | Principal Arterial Supply | Site, No., and Duration of Onyx Injections |
|---|---|---|---|---|
| 1/M/58 | Subarachnoid hemorrhage | Torcula | Occipital, middle meningeal, and posterior meningeal arteries, | Middle meningeal artery, 1 injection, 28 minutes |
| 2/M/36 | Right temporal IPH | Right sigmoid sinus segment | Middle meningeal and occipital arteries | Middle meningeal artery, 1 injection, 29 minutes |
| 3/M/62 | Hemianopsia | Right occipital | Middle meningeal artery | Middle meningeal artery, 1 injection, 24 minutes |
| 4/F/67 | Bruit | Left cavernous sinus | Maxillary and middle meningeal arteries | Maxillary artery balloon protection, 2 injections, 32 minutes for 2 injections |
| 5/F/59 | Right occipital IPH | Right occipital | Middle meningeal artery | Middle meningeal artery, 1 injection, 21 minutes |
| 6/M/54 | Hemianopsia | Right sigmoid sinus segment | Middle meningeal and occipital arteries | Middle meningeal artery, 1 injection, 20 minutes |
| 7/M/64 | Converted type I DAVF after incomplete sinus coiling | Right sigmoid sinus segment | Occipital artery | Occipital artery, 2 injections, 44 minutes for 2 injections |
| 8/F/57 | Hemianopsia | Left sigmoid sinus segment | Middle meningeal, occipital, and posterior meningeal arteries | Middle meningeal artery, 1 injection, 17 minutes |
Endovascular treatment was performed with the patient under general anesthesia. A 4F or 5F catheter was positioned in the external carotid artery, and an Onyx-compatible microcatheter (Rebar 105-5081-153, ev3) was coaxially advanced in a dural feeding artery as close as possible to the fistula site. Then, Onyx 18 was slowly injected. When reflux occurred, the injection was paused for 1–3 minutes. Usually, reflux occurred several times before Onyx would advance into the fistula site. In some cases with middle meningeal artery injection, more than a 5-cm reflux was accepted. Once Onyx advanced, it was intermittently injected until the draining veins were filled and all feeders were filled retrograde, thereby completely occluding the fistula. In 1 patient with a cavernous sinus DAVF supplied by branches of the maxillary artery, the maxillary artery was blocked with a microballoon (HyperForm, ev3) to prevent reflux and promote advancement of Onyx into the cavernous sinus.18 The duration of Onyx injections was calculated from time prints on angiographic images. Follow-up angiography was scheduled after 6–12 weeks in all patients. After the procedure, pain was controlled with medication as needed, including morphine or fentanyl. Illustrative cases are provided in Figs 1–3.
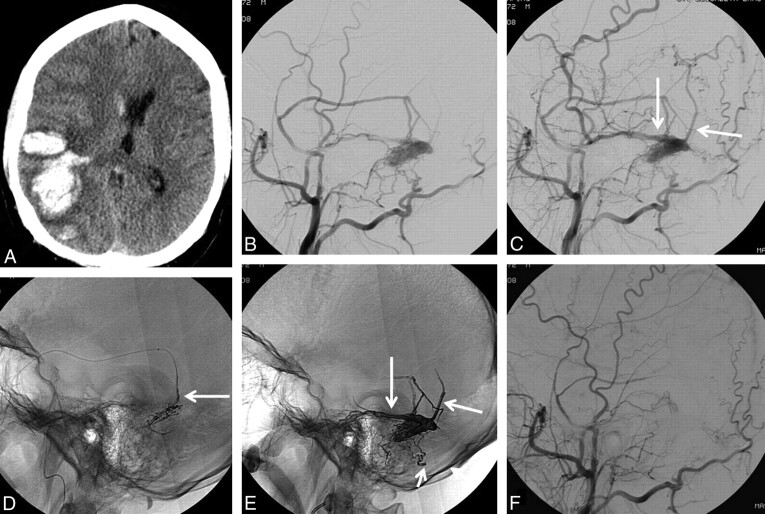
Fig 1.
A 58-year-old man (patient 1) with a good-grade (Hunt and Hess II) subarachnoid hemorrhage from a torcular DAVF that was cured with a single Onyx injection from the middle meningeal artery. A and B, Left external carotid angiograms in arterial (A) and venous (B) phases demonstrate a DAVF located on the torcula supplied by the middle meningeal and occipital arteries with marked congestion of cerebellar and even perimedullary veins. C, Supply to the DAVF by the posterior meningeal artery arising from the right vertebral artery. D, Microcatheter distally in the middle meningeal artery close to the fistula used for Onyx injection. E, AP view of selective angiography of the posterior meningeal artery (arrow) arising from the right vertebral artery. F, Same view as in E shows an Onyx cast in the draining vein and retrograde in the posterior meningeal artery (double arrows). G–I, Lateral views of Onyx cast (G), external carotid (H), and right vertebral (I) angiogams 10 weeks after embolization demonstrate complete occlusion of the DAVF.
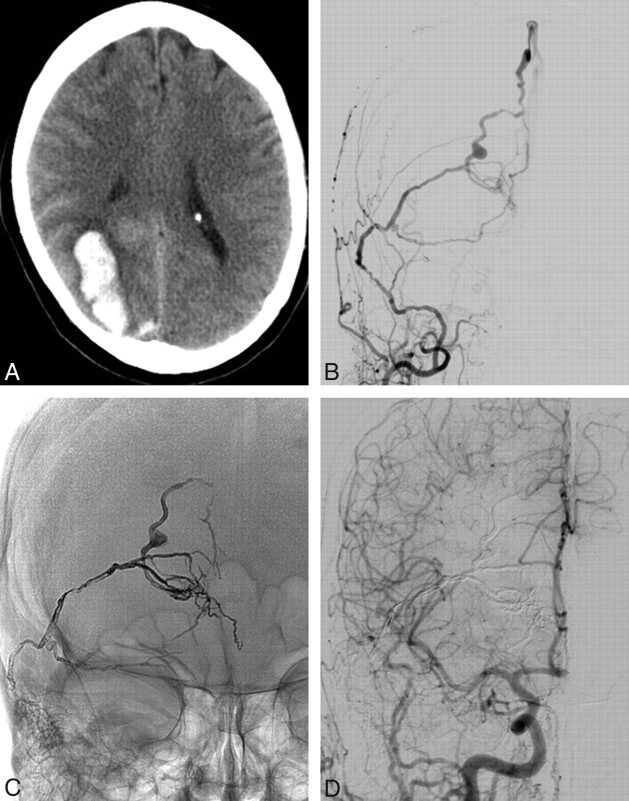
Fig 2.
A 36-year-old man (patient 2) with a parenchymal hemorrhage from a DAVF. A, CT scan demonstrates a right parenchymal hematoma. B and C, Early (B) and later (C) phases of a right external carotid angiogram reveal a DAVF located on an isolated open segment of an occluded transverse sinus. The fistula is supplied by the middle meningeal, posterior auricular, and occipital arteries with drainage to the vein of Labbé and a posterior cortical vein (arrows in C). D, Early phase of Onyx injection through a microcatheter, which was positioned close to the fistula in the middle meningeal artery (arrow). Onyx is injected slowly and first fills the dural feeders in the sinus wall. E, Note the Onyx cast at end of injection. The open sinus segment, the proximal draining veins (long arrows), and dural supply from the occipital artery (short arrow) are occluded. F, Complete occlusion of the DAVF is confirmed by postprocedural and follow-up angiography.
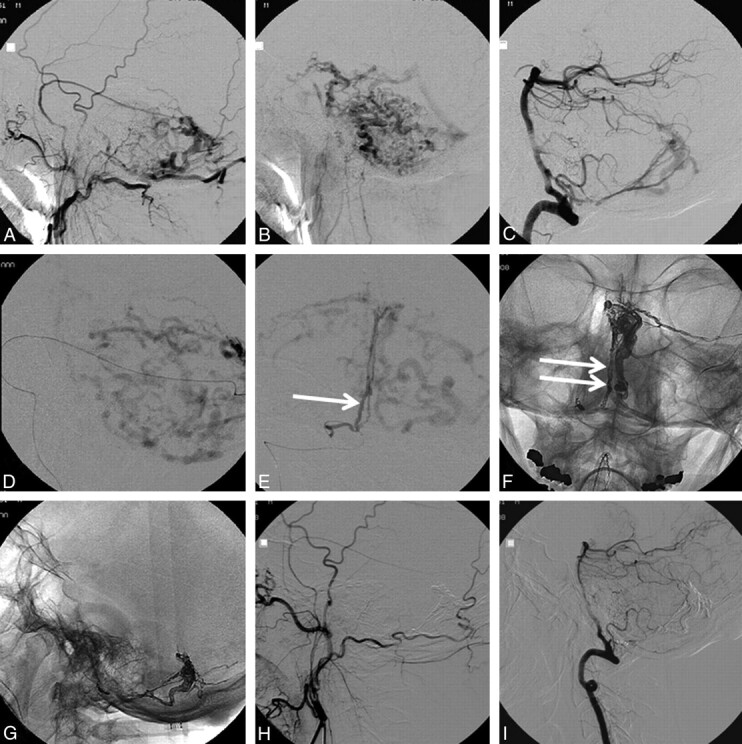
Fig 3.
A 59-year-old woman (patient 5) with a right occipital parenchymal hemorrhage from a DAVF. A, CT scan demonstrates a right parenchymal hematoma. B, AP view of a right external carotid angiogram shows a DAVF mainly supplied by the middle meningeal artery. Note the aneurysm on the occipital draining vein. C, Onyx cast after embolization through the middle meningeal artery. All dural supply and the draining veins together with the venous aneurysm are occluded. D, Follow-up carotid angiogram after 12 weeks confirms complete occlusion of the DAVF.
Results
All DAVFs could be cured in a single session, in 6 patients with a single Onyx injection and in 2 patients with 2 injections each. The duration of the Onyx injection in the 6 patients with a single injection was 17–29 minutes (mean, 23 minutes). In all cases, removal of the microcatheter was uneventful, despite sometimes long segments of reflux. Follow-up angiography in all patients confirmed durable obliteration. There were no complications of treatment. Radiation-induced hair loss did not occur. Six patients experienced postprocedural pain, probably because of dural ischemia. Morphine was needed in 2 patients. and fentanyl, in 1 to control the pain. Patients treated electively were discharged home the day following embolization. At the time of follow-up angiography, all patients were pain-free without medication. In 3 patients with hemianopsia as a result of venous congestion in the occipital lobe, visual fields were restored to normal within 12 weeks.
Discussion
Our initial experience in a small patient group by using Onyx for DAVFs with cortical venous drainage is hopeful and confirms the good results reported by others.14–18 Since we adopted Onyx as treatment of choice for these aggressive and rare lesions, all patients could be cured in a single session and mostly with only 1 Onyx injection of less than a half-hour duration. The technique we used to inject Onyx in DAVFs is comparable with the technique for the treatment of brain arteriovenous malformations19: Once a distal position of the tip of the microcatheter in a dural feeder close to the fistula is reached, reflux is slowly built up with a 1- to 3-minute pause between injection attempts until the feeding artery is plugged and Onyx starts to advance into the fistula and the draining veins. Sometimes 5–15 attempts are needed before Onyx advances; thus, patience is required. When in a long feeding vessel (mostly the anterior division of the middle meningeal artery), a distal position is obtained, reflux of 5 cm or even more can be accepted, and many injection attempts are possible. Even after injections of almost half an hour with a long segment of reflux, the Rebar microcatheter could be retrieved without difficulty. Thus, the length of reflux in these dural arteries is not directly related to the possibility of removal of the microcatheter. Onyx does not react with or stick to the vessel wall; it merely fills the vessel lumen.20 Therefore, it is important to completely fill all vessels involved in the fistulous complex; deposition of Onyx in the proximal draining vein only may not be sufficient to completely occlude the fistula or may give rise to recurrence at follow-up.
We suspend the injection for a short period of time when Onyx starts to fill the veins. With repeated injection, additional Onyx often initially is deposited more proximally, including retrograde filling of other dural feeders, before further distal advancement in the veins. This technique can be repeated several times, thereby slowly achieving complete occlusion of the fistula, all dural feeders, and the proximal draining veins with complete luminal filling. In selected cases, a microballoon proximal to the tip of the Onyx microcatheter can help in this injection process by preventing reflux and stimulating advancement of the Onyx.18 In our experience, confirmed by others,15,17 the middle meningeal artery is the most suitable for Onyx injection; it is often involved in dural fistulas and can be readily catheterized to a distal position, and long segments of reflux can be accepted because microcatheter removal proved to be easy in such cases. Whenever this artery contributes to the fistula, we try to use it for embolization.
Other vessels such as the occipital artery are mostly more tortuous and less easy to catheterize. When the tentorial artery is involved and has to be used as access for embolization, we probably still prefer injection of acrylic glue under protection of a microballoon across the origin in the internal carotid artery.21 Although we had no complications of treatment, postprocedural pain was experienced by most patients, and adequate pain medication was needed in some patients. Pain is probably related to ischemia of the dura as a result of occlusion of dural arteries. Pain usually gradually decreased in the following days to weeks, and at the time of follow-up angiography after 6–12 weeks, no patients used analgesics.
Another matter of concern is the radiation dose. Often many angiographic runs are necessary to document the dural fistula. In addition, prolonged Onyx injection during fluoroscopy adds to this dose. For dose reduction, we avoid simultaneous biplane fluoroscopy, and we approximate the flat panels as near as possible to the patient's head.
As with other embolic agents, complications with Onyx may occur. Ischemic damage to the trigeminal and facial nerve may be associated with too proximal reflux of Onyx in the middle meningeal artery beyond the foramen spinosum when occlusion of cavernous and petrosal branches may occur. Reflexive bradycardia may be associated with the treatment of tentorial DAVFs. When anastomoses of external carotid artery branches to the vertebrobasilar system remain unrecognized, migration of Onyx may cause posterior circulation infarctions.22–24 However, in our opinion, with proper technique and sufficient anatomic knowledge, these complications can mostly be avoided.
Conclusions
In conclusion, our limited experience with the use of Onyx for arterial embolization of DAVFs with cortical venous drainage is encouraging, with complete cure in all 8 patients without complications.
Abbreviations
- AP
anteroposterior
- DAVF
dural arteriovenous fistula
- IPH
intraparenchymal hemorrhage
References
- 1. Cognard C, Gobin YP, Pierot L, et al. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology 1995;194:671–80 [DOI] [PubMed] [Google Scholar]
- 2. Mullan S. Reflections upon the nature and management of intracranial and intraspinal vascular malformations and fistulae. J Neurosurg 1994;80:606–16 [DOI] [PubMed] [Google Scholar]
- 3. Cognard C, Casasco A, Toevi M, et al. Dural arteriovenous fistulas as a cause of intracranial hypertension due to impairment of cranial venous outflow. J Neurol Neurosurg Psychiatry 1998;65:308–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hurst RW, Bagley LJ, Galetta S, et al. Dementia resulting from dural arteriovenous fistulas: the pathologic findings of venous hypertensive encephalopathy. AJNR Am J Neuroradiol 1998;19:1267–73 [PMC free article] [PubMed] [Google Scholar]
- 5. van Dijk JM, terBrugge KG, Willinsky RA, et al. Clinical course of cranial dural arteriovenous fistulas with long-term persistent cortical venous reflux. Stroke 2002;33:1233–36 [DOI] [PubMed] [Google Scholar]
- 6. Duffau H, Lopes M, Janosevic V, et al. Early rebleeding from intracranial dural arteriovenous fistulas: report of 20 cases and review of the literature. J Neurosurg 1999;90:78–84 [DOI] [PubMed] [Google Scholar]
- 7. Hoh BL, Choudhri TF, Connolly ES, Jr, et al. Surgical management of high-grade intracranial dural arteriovenous fistulas: leptomeningeal venous disruption without nidus excision. Neurosurgery 1998;42:796–804 [DOI] [PubMed] [Google Scholar]
- 8. van Dijk JM, TerBrugge KG, Willinsky RA, et al. Selective disconnection of cortical venous reflux as treatment for cranial dural arteriovenous fistulas. J Neurosurg 2004;101:31–35 [DOI] [PubMed] [Google Scholar]
- 9. Nelson PK, Russell SM, Woo HH, et al. Use of a wedged microcatheter for curative transarterial embolization of complex intracranial dural arteriovenous fistulas: indications, endovascular technique, and outcome in 21 patients. J Neurosurg 2003;98:498–506 [DOI] [PubMed] [Google Scholar]
- 10. Defreyne L, Vanlangenhove P, Vandekerckhove T, et al. Transvenous embolization of a dural arteriovenous fistula of the anterior cranial fossa: preliminary results. AJNR Am J Neuroradiol 2000;21:761–65 [PMC free article] [PubMed] [Google Scholar]
- 11. Kallmes DF, Jensen ME, Cloft HJ, et al. Percutaneous transvenous coil embolization of a Djindjian type 4 tentorial dural arteriovenous malformation. AJNR Am J Neuroradiol 1997;18:673–76 [PMC free article] [PubMed] [Google Scholar]
- 12. Layton KF, Nelson MD, Kallmes DF. Transarterial coil embolization of the venous component of aggressive type 4 dural arteriovenous fistulas. AJNR Am J Neuroradiol 2006;27:750–52 [PMC free article] [PubMed] [Google Scholar]
- 13. van Rooij WJ, Sluzewski M, Beute GN. Dural arteriovenous fistulas with cortical venous drainage: incidence, clinical presentation, and treatment. AJNR Am J Neuroradiol 2007;28:651–55 [PMC free article] [PubMed] [Google Scholar]
- 14. Stiefel MF, Albuquerque FC, Park MS, et al. Endovascular treatment of intracranial dural arteriovenous fistulae using Onyx: a case series. Neurosurgery 2009;65(6 suppl):132–39 [DOI] [PubMed] [Google Scholar]
- 15. Macdonald JH, Millar JS, Barker CS. Endovascular treatment of cranial dural arteriovenous fistulae: a single-centre, 14-year experience and the impact of Onyx on local practise. Neuroradiology 2010;52:387–95 [DOI] [PubMed] [Google Scholar]
- 16. Huang Q, Xu Y, Hong B, et al. Use of Onyx in the management of tentorial dural arteriovenous fistulae. Neurosurgery 2009;65:287–92 [DOI] [PubMed] [Google Scholar]
- 17. Chew J, Weill A, Guilbert F, et al. Arterial Onyx embolisation of intracranial DAVFs with cortical venous drainage. Can J Neurol Sci 2009;36:168–75 [DOI] [PubMed] [Google Scholar]
- 18. Shi ZS, Loh Y, Duckwiler GR, et al. Balloon-assisted transarterial embolization of intracranial dural arteriovenous fistulas. J Neurosurg 2009;110:921–28 [DOI] [PubMed] [Google Scholar]
- 19. van Rooij WJ, Sluzewski M, Beute GN. Brain AVM embolization with Onyx. AJNR Am J Neuroradiol 2007;28:172–77 [PMC free article] [PubMed] [Google Scholar]
- 20. Van Loock K, Menovsky T, Voormolen MH, et al. Microsurgical removal of Onyx HD-500 from an aneurysm for relief of brainstem compression. J Neurosurg 2009. November 6. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21. van Rooij WJ, Sluzewski M, Beute GN. Tentorial artery embolization in tentorial dural arteriovenous fistulas. Neuroradiology 2006;48:737–43 [DOI] [PubMed] [Google Scholar]
- 22. Lv X, Jiang C, Zhang J, et al. Complications related to percutaneous transarterial embolization of intracranial dural arteriovenous fistulas in 40 patients. AJNR Am J Neuroradiol 2009;30:462–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schaller B, Cornelius JF, Prabhakar H, et al. The trigemino-cardiac reflex: an update of the current knowledge. J Neurosurg Anesthesiol 2009;21:187–95 [DOI] [PubMed] [Google Scholar]
- 24. Geibprasert S, Pongpech S, Armstrong D, et al. Dangerous extracranial-intracranial anastomoses and supply to the cranial nerves: vessels the neurointerventionalist needs to know. AJNR Am J Neuroradiol 2009;30:1459–68 [DOI] [PMC free article] [PubMed] [Google Scholar]