SUMMARY:
The balloon remodeling technique was initially designed for the endovascular treatment of anatomically complex aneurysms, specifically wide-neck aneurysms. A nondetachable balloon is inflated in front of the aneurysm neck during coil deposition and removed at the end of the procedure. Some controversies regarding the safety of the technique were introduced by the recent publication of a series showing a much higher rate of complications with the remodeling technique compared with the standard coiling technique. However, recent data from the literature review and from the large ATENA and CLARITY series show that the safety of standard coiling and remodeling is quite similar. Anatomic results are also probably better after remodeling. Finally, due to equivalent safety and better anatomic results, the remodeling technique can be widely used in the management of both ruptured and unruptured aneurysms.
EVT with coils is widely used in the management of intracranial aneurysms.1 However, endovascular treatment can be technically difficult for anatomic reasons, particularly when the neck is wide or when the dome-to-neck ratio is not favorable. In 1994, Moret et al2 described the remodeling technique for extending the indications and feasibility of the endovascular treatment to wide-neck intracranial aneurysms. A few monocentric series were published analyzing clinical and anatomic results of this technique.3–9 However, in several of these series, no direct comparison between standard coiling and remodeling was available. Moreover, in most of the literature, ruptured and unruptured aneurysms were mixed, and a separate analysis of the safety and efficacy in both situations was not possible. A literature review was published in 2008.10 A direct comparison of the standard coiling technique and remodeling was recently conducted in both ruptured and unruptured aneurysms in 2 large multicentric prospective series.11,12
The publication by Sluzewski et al in 20069 suggested that the remodeling technique was associated with a high complication rate and should be used only if the standard coiling technique was impossible or had failed.
To know accurately the place of the remodeling technique (also called balloon-assisted coil embolization) in the endovascular treatment of intracranial aneurysms, a precise analysis of its feasibility, safety, and efficacy is now needed.
What is the Remodeling Technique?
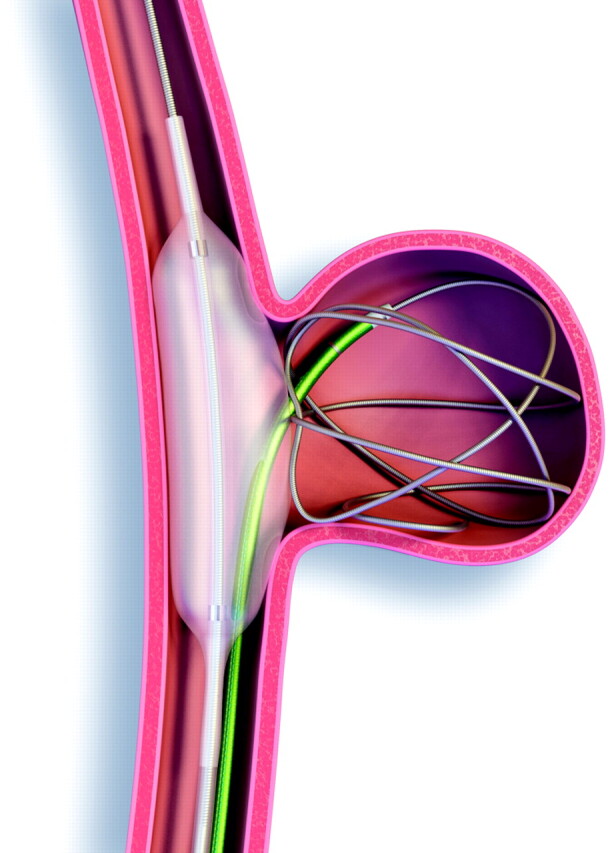
A nondetachable balloon is temporarily inflated in front of the neck of the aneurysm during each coil placement (Figs 1 and 2). At the end of the procedure, the remodeling balloon is removed and no device is left in place in the parent vessel (unless stent placement is subsequently performed).
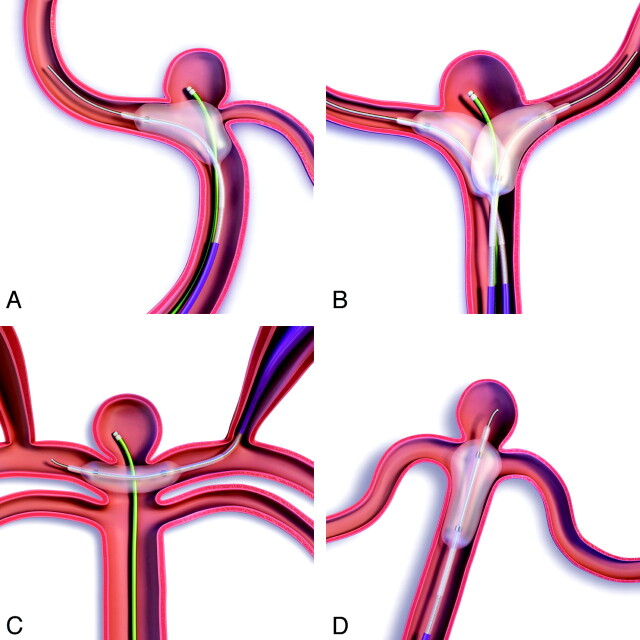
Fig 1.
Remodeling technique for sidewall aneurysms.
Fig 2.
Remodeling technique for bifurcation aneurysms. A, Use of a pear-shaped balloon. B, Double-balloon technique. C, Placement of the remodeling balloon parallel to the aneurysm neck by using circle of Willis anastomosis. D, Use of a double-lumen remodeling technique.
In sidewall aneurysms, the balloon is simply placed in the parent vessel in front of the aneurysm neck (Fig 1). In bifurcation aneurysms, the situation is more complex because it is necessary to completely protect the neck to avoid coil protrusion (Fig 2). In this situation, there are several options: 1) Place 1 balloon in the parent vessel and a bifurcation artery. Inflate the balloon sufficiently to completely cover the neck (some balloons are specifically designed for this purpose with a pear shape when inflated). 2) Place two balloons in front of the aneurysm neck. For example, for a basilar tip aneurysm, a balloon is placed in the basilar artery extending into the 1 posterior cerebral artery and another balloon is placed on the other side. 3) Place a balloon parallel to the neck of the aneurysm by navigating through the circle of Willis anastomosis. For example, in a carotid bifurcation aneurysm, the balloon is not navigated through the ipsilateral carotid artery but through the contralateral one and the anterior communicating artery. This technique is feasible if the anastomoses of the circle of Willis are present and sufficiently large. 4) Place a round balloon mounted on a microcatheter in front of the aneurysm neck. These balloon catheters are no longer available; therefore, this technique can no longer be used. 5) Place a double-lumen microcatheter remodeling balloon. It is placed in front of the neck with the microguidewire inside the neck. The coils are deposited in the aneurysm sac through the second lumen. In bifurcation aneurysms, the best option is decided according to the anatomy of the parent vessel (cervical and intracranial portions), the anatomy of the circle of Willis (confirm that posterior communicating and anterior communicating arteries are present), and the aneurysm anatomy (size and position of the neck, direction of the aneurysm sac, and relations between aneurysm neck and bifurcation branches).
Use and Feasibility of the Technique
In 3 small series, the rate of use of the remodeling technique was very heterogeneous: 8.6%,9 16.9%,5 and 33.0%.8 The remodeling technique was more frequently used in unruptured aneurysms (37.3%) than in ruptured aneurysms (20.5%), according to the analyses conducted in the ATENA and CLARITY series.12,13
According to the ATENA and CLARITY analyses,12,13 the remodeling technique was used in all aneurysm locations but less frequently in anterior communicating and anterior cerebral aneurysms. The navigation in the anterior arterial complex was, with the first generations of remodeling balloons, relatively difficult. The profile of the most recent balloons has been improved, and navigation in the anterior complex is now easier.
The feasibility of the remodeling technique has not been widely studied. Cottier et al4 reported a failure rate of 8%. In this series, the 2 causes of failure were the impossibility of placing the balloon in front of the aneurysm neck and rupture of the balloon during the procedure. Balloon navigation can be difficult in the case of tortuosity of the cervical or intracranial vessels or acute angle of the parent vessel. Another cause of failure of the remodeling technique is a completely unfavorable dome-to-neck ratio with a very wide neck. In this case, the stabilization of coils into the aneurysm sac can be impossible despite inflation of the balloon in front of the neck.
Complications
The 2 most frequent complications of the endovascular treatment of intracranial aneurysms are thromboembolic events and intraoperative rupture. In some series, no comparison was available regarding the rate of complications in both standard coiling and remodeling.2,4,5
In the Layton et al series,8 the rate of thrombus formation was not significantly different in patients treated with standard coiling compared with the remodeling technique (9% and 14%, respectively). Symptomatic thromboembolic events were also observed in a similar percentage of cases (5% in standard coiling and 7% in remodeling). Similarly, in the Brooks et al series,14 diffusion-weighted-imaging abnormalities were detected in 32% in the coiling group and 24% in the remodeling group. However, in the Sluzewski et al series,9 the rate of thromboembolic events was higher in the remodeling group (9.8%) compared with the coiling group (2.2%). In the Shapiro et al review,10 the rate of thromboembolic events was quite similar in patients treated with coiling (8.1%) and remodeling (8.0%). Symptomatic thromboembolic events were encountered in 4.6% of patients treated with coiling and 4.4% of patients treated with remodeling. Death related to thromboembolic events was reported as 1.2% for patients treated with coiling and 0.4% for patients treated with remodeling. In unruptured aneurysms (ATENA), the rate of thromboembolic events was lower in the remodeling group (5.4% versus 6.2% in coiling group), and the clinical outcome was similar in both groups.11 In ruptured aneurysms (CLARITY), the rate of thromboembolic events was also similar in both groups (12.7% in coiling group and 11.3% in remodeling group).12
The rate of intraoperative rupture was not evaluated as extensively. In the Sluzewski et al series,9 the rate of intraoperative rupture was higher in the remodeling (4.0%) compared with the coiling group (0.8%). In the Shapiro et al review,10 the rate of intraoperative rupture was 3.4% in ruptured aneurysms treated with standard coiling, 1.7% in ruptured aneurysms treated with the remodeling technique, 1.4% in unruptured aneurysms treated with standard coiling, and 1.8% in unruptured aneurysms treated with the remodeling technique. In ruptured aneurysms, the clinical outcome was a symptomatic event or death in 2.7% in the coiling group and 1.7% in the remodeling group. In unruptured aneurysms, clinical outcome was a symptomatic event or death in 0.6% in coiling group and 0.9% in remodeling group.
Similar results were reported in the analyses conducted in the ATENA and CLARITY series. In ATENA (unruptured aneurysms), the rate of intraoperative rupture was 3.2% in the remodeling group and 2.2% in the coiling group.11 Clinical consequences (permanent deficit or death) of the intraoperative rupture were encountered in 0.6% in the coiling group and 1.4% in the remodeling group. In ruptured aneurysms (CLARITY), the rate of intraoperative rupture was exactly the same in both groups (4.4%).12 The overall complication rate was 10.8% for standard coiling of unruptured aneurysms and 11.7% for remodeling of unruptured aneurysms; 17.4% for coiling of ruptured aneurysms and 16.9% for remodeling of ruptured aneurysms.11,12
Clinical Outcome
In the Cottier et al4 and Lefkowitz et al5 series, clinical outcome was favorable in all patients. However, death or dependency was encountered in 14.1% after remodeling and 3.0% after coiling in the Sluzewski et al series.9
In the ATENA series, overall morbidity was 2.2% in the coiling group and 2.3% in the remodeling group, whereas mortality was 0.9% in coiling group and 1.4% in remodeling group.11
In the CLARITY series,12 treatment morbidity was 3.9% in the coiling group and 2.5% in the remodeling group. Treatment mortality was 1.2% in coiling group and 1.3% in remodeling group. Global morbidity and mortality (including consequences of subarachnoid hemorrhage and its complications) were 7.1% and 12.5%, respectively, in the coiling group and 3.8% and 12.5% in the remodeling group.
Anatomic Results
In the Lefkowitz et al series,5 initial anatomic results in patients treated with the remodeling technique were quite good, with 100% occlusion in 83% of patients and 95%–100% occlusion in the remaining 17% of patients. During the period of follow-up (range: 1–26 months; median, 10 months), no patient required further treatment or developed a recurrent aneurysm neck or lumen.
In the series reported by Cottier et al,4 anatomic results after treatment with the remodeling technique were also quite good. Immediate posttreatment results reported total occlusion in 69% of cases, subtotal in 29% of cases, and incomplete in 2% of cases. The initial total occlusions remained stable during the follow-up in 90% of cases, and recanalization was observed in 10% of cases. The initial subtotal occlusions showed no modification in 69% of cases, improved to total occlusion in 15%, and displayed regrowth of the remnant in 15%. Initial incomplete occlusion was unchanged during follow-up. Five aneurysms were retreated by using the remodeling technique. Final results (last follow-up angiogram) reported complete occlusion in 67% of cases, subtotal occlusion in 24% of cases, and incomplete occlusion in 9% of cases.
In both the Lefkowitz et al5 and Cottier et al4 series, anatomic results were good, but no direct comparison with standard coiling was available. Packing attenuation was also not studied.
In the Sluzewski et al series,9 anatomic results were different. Packing attenuation was similar in aneurysms treated by standard coiling (24.1%) and the remodeling technique (22.7%). At 6-month follow-up, incomplete aneurysm occlusion was more frequently observed in aneurysms treated with remodeling (27.7%) than with standard coiling (16.9%). Additional treatment was also more frequently performed in aneurysms treated with remodeling (16.9% versus 9.0% for aneurysms treated with the remodeling and standard coiling techniques, respectively).
The Shapiro et al10 literature review does not confirm the Sluzewski et al9 findings. Both initial and follow-up aneurysm occlusion rates were higher in balloon-assisted cases. The initial occlusion rate was total occlusion in 73% of patients in the remodeling group and 49% of patients in the standard coiling group, subtotal occlusion in 22% in the remodeling group and 39% in the coiling group, and incomplete occlusion in 5% in the remodeling group and 13% in the coiling group. At follow-up, there were similar results: total occlusion in 72% of patients in the remodeling group and 54% of patients in the standard coiling group, subtotal occlusion in 17% in the remodeling group and 34% in the coiling group, and incomplete occlusion in 10% of the remodeling group and 11% of the coiling group.
According to the ATENA and CLARITY series,11,12 results are possibly different in unruptured and ruptured aneurysms. In the ATENA series (unruptured aneurysms), immediate anatomic results reported were complete occlusion in 59.8% of aneurysms in the standard coiling group and 59.8% of aneurysms in the remodeling group, neck remnant in 24.3% in the coiling group and 20.1% in the remodeling group, and aneurysm remnant in 16.0% in the coiling group and 20.1% in the remodeling group.11 In the CLARITY series (ruptured aneurysms), immediate anatomic results were different: complete occlusion in 46.9% of aneurysms in the standard coiling group and 50.0% of aneurysms in the remodeling group, neck remnant in 41.6% in the coiling group and 44.9% in the remodeling group, and aneurysm remnant in 11.5% in the coiling group and 5.1% in the remodeling group.12 Using a 2-point classification, the rate of adequate occlusion was significantly higher in the remodeling group (94.9% compared with 88.5% in coiling group, P = .017). The mean packing attenuation was 36.7% ± 23.2% in the coiling group and 39.3% ± 57.7% in the remodeling group (P = .577). In both the ATENA and CLARITY series, long-term anatomic results are not yet available.
Conclusions
All except 1 publication showed a similar safety profile in the standard coiling and the remodeling techniques. The literature review comparing the anatomic results in aneurysms treated by standard coiling and remodeling shows that immediate and follow-up results are better in the remodeling group.9 These results are partially confirmed in the CLARITY series (ruptured aneurysms), showing that adequate occlusion is significantly more frequent in the remodeling group.12 Despite the fact that aneurysms treated by the remodeling technique are different from aneurysms treated with standard coiling, the safety of both techniques is similar with a higher anatomic efficacy of the remodeling technique. Accordingly, wide use of the remodeling technique can be proposed.
For several years, the remodeling technique has competed with stent-assisted coiling for the treatment of anatomically difficult aneurysms, specifically those with a wide neck. However aneurysm stent placement seems to be associated with a higher mortality compared with coiling with or without remodeling.15 Accordingly, wide use of stents should probably not be recommended.
ABBREVIATIONS
- ATENA
Aneurysms Treated by Endovascular Approach
- CLARITY
clinical and anatomic results in the treatment of ruptured intracranial aneurysms
- CHU
Centre Hospitalier Universitaire
- EVT
endovascular treatment
References
- 1. Molyneux A, Kerr R, Stratton I, et al. , for the International Subarachnoid Aneurysm Trial (ISAT) Colaborative Group. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 2002;360:1262–63 [DOI] [PubMed] [Google Scholar]
- 2. Moret J, Cognard C, Weill A, et al. The “remodeling technique” in the treatment of wide neck intracranial aneurysms. Intervent Neuroradiol 1997;3:21–35 [DOI] [PubMed] [Google Scholar]
- 3. Aletich VA, Debrun GM, Misra M, et al. The remodeling technique of balloon assisted Guglielmi detachable coil placement in wide-necked aneurysms: experience at the University of Illinois at Chicago. J Neurosurg 2000;93:388–96 [DOI] [PubMed] [Google Scholar]
- 4. Cottier JP, Pasco A, Gallas S, et al. Utility of balloon-assisted Guglielmi detachable coiling in the treatment of 49 cerebral aneurysms: a retrospective, multicenter study. AJNR Am J Neuroradiol 2001;22:345–51 [PMC free article] [PubMed] [Google Scholar]
- 5. Lefkowitz MA, Gobin YP, Akiba Y, et al. Balloon-assisted Guglielmi detachable coiling of wide necked aneurysms. II. Clinical results. Neurosurgery 1999;45:531–37 [DOI] [PubMed] [Google Scholar]
- 6. Malek AM, Halbach VV, Phatouros CC, et al. Balloon-assisted technique for endovascular coil embolization of geometrically difficult intracranial aneurysms. Neurosurgery 2000;22:46:1396–406, discussion 1406–08 [DOI] [PubMed] [Google Scholar]
- 7. Nelson PK, Levy DI. Ballon-assisted coil embolization of wide-necked aneurysms of the internal carotid artery: medium term angiographic and clinical follow-up in 22 patients. AJNR Am J Neuroradiol 2001;22:19–26 [PMC free article] [PubMed] [Google Scholar]
- 8. Layton KF, Cloft HJ, Gray LA, et al. Balloon-assisted coiling of intracranial aneurysms: evaluation of local thrombus formation and symptomatic thromboembolic complications. AJNR Am J Neuroradiol 2007;28:1172–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sluzewski M, Von Rooij WJ, Beute GN, et al. Balloon-assisted coil embolization of intracranial aneurysms: incidence, complications, and angiography results. J Neurosurg 2006;105:396–99 [DOI] [PubMed] [Google Scholar]
- 10. Shapiro M, Babb J, Becske T, et al. Safety and efficacy of adjunctive balloon remodeling during endovascular treatment of intracranial aneurysms: a literature review. AJNR Am J Neuroradiol 2008;29:1777–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pierot L, Spelle L, Leclerc C, et al. Endovascular treatment of unruptured intracranial aneurysms: comparison of safety of remodeling technique and standard treatment with coils. Radiology 2009;251:846–55 [DOI] [PubMed] [Google Scholar]
- 12. Pierot L, Cognard C, Anxionnat R, et al. , for the CLARITY group. Remodeling technique for endovascular treatment of ruptured intracranial aneurysms had a higher rate of adequate postoperative occlusion than did conventional coil embolization with comparable safety. Radiology. 2011;258:546–53 [DOI] [PubMed] [Google Scholar]
- 13. Pierot L, Spelle, Vitry F, for the ATENA investigators. Immediate clinical outcome of patients harboring unruptured intracranial aneurysms treated by endovascular approach: results of the ATENA trial. Stroke 2008;39:2497–504. Epub 2008 Jul 10 [DOI] [PubMed] [Google Scholar]
- 14. Brooks NP, Turk AS, Niemann DB, et al. Frequency of thromboembolic events associated with endovascular aneurysm treatment: retrospective case series. J Neurosurg 2008;108:1095–100 [DOI] [PubMed] [Google Scholar]
- 15. Piotin M, Blanc R, Spelle L, et al. Stent-assisted coiling of intracranial aneurysm: clinical and angiographic results in 216 consecutive aneurysms. Stroke 2010;41:110–15 [DOI] [PubMed] [Google Scholar]