Abstract
Pistol grip deformity (PGD) may be the main factor in femoroacetabular impingement development. This study aimed to clarify the epidemiological indices and factors related to PGD in Japanese people. This population-based cohort study included 1575 local Japanese residents. PGD, center edge angle, and joint space width were measured radiographically. We investigated the relationship between PGD and spino-pelvic parameters. Factors associated with PGD were examined using multiple logistic regression analysis, with the presence/absence of PGD as an objective variable, and sex, age, body mass index (BMI), and the presence/absence of hip pain or spino-pelvic parameters as explanatory variables. In the entire cohort, 4.9% (10.6% men, 2.1% women) had PGD on at least one side. A trend was observed between PGD and increasing age in both men and women (men: p < 0.0001, women: p = 0.0004). No relationship was observed between PGD and hip pain (risk ratio 1.0 [95% confidence interval 0.97–1.03]). Factors significantly associated with PGD were age, sex, and BMI in the multivariate model. Acquired factors may be related to PGD in Japanese people as the PGD prevalence increased with age and PGD was not significantly associated with hip pain. This study provides new insights into the etiology and clinical significance of PGD.
Subject terms: Medical research, Signs and symptoms
Introduction
Patients with primary osteoarthritis of the hip often experience swelling in the lateral part of the femoral head-neck junction. This occurrence is termed pistol grip deformity (PGD)1,2. PGD has attracted significant attention since several authors have reported the disease concept of femoroacetabular impingement (FAI)3–6. There are three types of hip impingements: cam, pincer, and combined. The cam-type is due to an abnormal morphology of the junction between the femoral head and neck, while the pincer type is due to an excessively deep acetabular floor. PGD is presumably the main factor of cam-type FAI in European countries and the United States7. In recent years, many reports have suggested FAI as an etiology of hip pain and primary/idiopathic osteoarthritis8,9. PGD is considered a congenital deformity10. In addition, several studies have suggested an association between PGD and spino-pelvic parameters, including pelvic incidence11,12.
Owing to technical advances in magnetic resonance imaging (MRI) diagnostics and hip arthroscopy, the presence and pathology of FAI have begun to attract attention in Japan, where secondary osteoarthritis of the hip due to acetabular dysplasia is common13. However, the epidemiology of PGD remains unclear, and the association between PGD and hip pain or primary osteoarthritis has not been elucidated among the Japanese population. Further, the relationship between PGD and spino-pelvic parameters is unknown in this population.
This study aimed to clarify the prevalence of PGD in different age groups and sexes and elucidate related factors, including hip pain, osteoarthritis, and spino-pelvic parameters, in a Japanese population.
Results
Prevalence of pistol grip deformity
Table 1 shows the prevalence of PGD in the overall population and the subgroups of age, classified by sex. In the overall population, the prevalence of PGD was 73/1481 (4.9%). The prevalence of PGD in men (52/491; 10.6%) was significantly higher than that in women (21/990; 2.1%). The risk ratio for men was 4.99 (95% confidence interval (CI) 3.04–8.19), which was higher than that for women. Moreover, the prevalence of PGD significantly increased with age for both sexes (Supplementary Figure S1).
Table 1.
Prevalence of PGD by sex and five age groups.
| Men | Women | |
|---|---|---|
| Age groups (years) | ||
| ≤ 49 | 4/59 (6.7%) | 0/117 (0%) |
| 50–59 | 0/78 (0%) | 0/186 (0%) |
| 60–69 | 5/130 (3.9%) | 5/292 (1.7%) |
| 70–79 | 21/135 (15.6%) | 11/278 (4.0%) |
| ≥ 80 | 22/89 (24.7%) | 0.0 (4.3%) |
| Total | 52/491 (10.6%) | 0.0 (2.1%) |
The prevalence of PGD tends to increase with age group in both sexes (Cochran-Armitage test; men: p < 0.0001, women: p = 0.0004).
PGD pistol grip deformity.
Comparison of the demographics between the groups with and without pistol grip deformity
The PGD-positive group had a significantly higher proportion of men, older age, and higher body weight and body mass index (BMI) than the PGD-negative group (Table 2).
Table 2.
Comparison of the demographics between the groups with and without PGD.
| PGD (+) | PGD (−) | p-value | |
|---|---|---|---|
| Number of participants (hips) | 73 (102) | 1408 (2860) | |
| Demographics | |||
| Sex (men vs. women) | 52 vs. 21 | 439 vs. 969 | < 0.0001 |
| Age (years) | 75.3 ± 11 (72.6–77.9) | 64.8 ± 12.8 (64.1–65.5) | < 0.0001 |
| Height (cm) | 157.4 ± 9.8 (155.1–159.7) | 156.2 ± 9.1 (155.7–156.7) | 0.2687 |
| Weight (kg) | 59.5 ± 11 (56.9–62.1) | 56.3 ± 11.2 (55.7–56.9) | 0.0172 |
| BMI (kg/m2) | 23.9 ± 3.4 (23.1–24.7) | 23.0 ± 3.5 (22.8–23.1) | 0.0231 |
| Hip pain | 2/102 (2.0%) | 56/2860 (2.0%) | 0.9984 |
| Hip parameters | |||
| CE angle (° ) | 31.3 ± 6.3 (30.1–32.6) | 28.9 ± 6.4 (28.7–29.2) | < 0.0001 |
| mJSW (mm) | 4.0 ± 0.9 (3.8–4.2) | 3.9 ± 0.8 (3.9–3.9) | 0.5042 |
| Spinopelvic parameters | |||
| LL (°) | 40.8 ± 18 (36.5–44.9) | 45.7 ± 13.3 (45.0–46.4) | 0.0023 |
| SS (°) | 28.8 ± 11 (26.3–31.2) | 31.9 ± 9.0 (31.4–32.4) | 0.0042 |
| PT (°) | 21.9 ± 11 (19.4–24.5) | 18.0 ± 9.1 (17.5–18.5) | 0.0003 |
| PI (°) | 50.7 ± 12.5 (47.8–53.6) | 49.9 ± 10.6 (49.4–50.5) | 0.5287 |
Prevalence of hip pain and hip parameters are calculated from 2962 hips.
PGD pistol grip deformity, BMI body mass index, CE angle center–edge angle, mJSW mean joint space width, LL lumbar lordosis, SS sacral slope, PT pelvic tilt, PI pelvic incidence.
Data are means ± standard deviation (95% confidence interval). Bold values indicate statistically significant differences between the two groups.
Association of pistol grip deformity with hip pain
Among the 102 PGD-positive hips, only two participants (2.0%) experienced hip pain on the affected side. No significant association was observed between PGD and hip pain (risk ratio 1.0 [95% CI 0.97–1.03]) (Table 2).
Association of pistol grip deformity with hip parameters
The PGD-positive group had a significantly larger center edge (CE) angle than the PGD-negative group (Table 2). However, multiple logistic regression analysis, including sex, age, BMI, CE angle, and medial joint space width (mJSW) as explanatory variables, revealed that the presence of PGD was not significantly associated with CE or mJSW. Male sex, age, and BMI were significantly associated with the presence of PGD in this model (Table 3).
Table 3.
Association of PGD with hip parameters (multivariate analysis).
| Reference | Odds ratio | 95% CI | p-value | |
|---|---|---|---|---|
| Sex | Men vs. women | 4.54 | 2.85–7.25 | < 0.0001 |
| Age | + 1 year | 1.09 | 1.07–1.12 | < 0.0001 |
| BMI | + 1 kg/m2 | 1.12 | 1.06–1.19 | 0.0002 |
| CE angle | + 1° | 1.03 | 0.99–1.07 | 0.1252 |
| mJSW | + 1 mm | 0.91 | 0.68–1.22 | 0.537 |
Odds ratios are calculated by multiple logistic regression analysis on 2962 hips.
PGD pistol grip deformity, 95% CI 95% confidence interval, BMI body mass index, CE angle center–edge angle, mJSW mean joint space width.
Bold values indicate a statistically significant association with PGD.
Association of pistol grip deformity with spino-pelvic parameters
Regarding the comparison of spino-pelvic parameters, the lumbar lordosis (LL), sacral slope (SS), and pelvic tilt (PT) were found to be significantly different between the groups with and without PGD. Pelvic incidence (PI) was not significantly different between the two groups (Table 3). Subsequently, we conducted a multiple logistic regression analysis wherein the LL, PT, and PI served as explanatory variables, and age, sex, and BMI served as adjusted variables. SS was not included in this model to avoid multicollinearity because we used the algorithm “PI = PT + SS.” Moreover, the propensity score for the objective variable was calculated from the adjusted variables and treated as one variable to avoid overfitting. The presence of PGD was not significantly associated with any of the spino-pelvic parameters; however, PT demonstrated a positive odds ratio (95% CI 1.00–1.10) (Table 4).
Table 4.
Association of PGD with spino-pelvic parameters (multivariate analysis).
| Reference | Odds ratio | 95% CI | p-value | |
|---|---|---|---|---|
| LL | + 1° | 1.00 | 0.97–1.03 | 0.7812 |
| PT | + 1° | 1.04 | 1.00–1.10 | 0.0746 |
| PI | + 1° | 0.99 | 0.95–1.04 | 0.8963 |
Bold values indicate a positive association with PGD.
Odds ratios are calculated by multiple logistic regression analysis after adjustment by age, sex and body mass index on 1481 participants. In creating the model, the propensity score for the objective variable is calculated from the adjusted variables and treated as one variable.
PGD pistol grip deformity, 95% CI 95% confidence interval, LL lumbar lordosis, PT pelvic tilt, PI pelvic incidence.
Discussion
The most notable result of this study was that the prevalence of PGD increased with age in both men and women. In addition, PGD was significantly associated with weight and BMI. These findings may suggest that the etiology of PGD involves acquired factors in addition to congenital morphological anomalies of the femoral neck, at least in the Japanese population.
In this study, the overall prevalence of PGD was 4.9% (10.6% in men and 2.1% in women). To the best of our knowledge, this is the first study to successfully elucidate the epidemiological indices of PGD and the related factors in a large (approximately 1500) Asian population. A previous study by Goodman et al. examined 2665 cadavers and found 215 cadavers with PGD (8%)14. In another study by Doherty et al., the overall prevalence of PGD was 3.61% (6.37% in men and 0.39% in women)15. That study included people who had been in the hospital for intravenous urography, with no radiographic hip osteoarthritis. Consistent with their findings, our results suggested that the prevalence of PGD in the Asian participants (Japanese) was relatively lower than that in Europe and the United States. Similar to our results, several previous studies have reported that PGD is more common in men than in women16,17. Goodman et al. have reported 122 cadavers with a bilateral PGD incidence of 56.7%14, which is considerably high, similar to that in our study (29/71; 40.8%).
Interestingly, the most notable result of this study was that the prevalence of PGD increased with age in both men and women. No past studies have reported a correlation between the prevalence of PGD and age; rather, it has been reported that the prevalence of PGD in men tended to reduce with age15. Allen et al. have examined 113 cases with cam-type FAI and reported that a deformity of the head-neck junction could be congenital18. However, our findings suggest that the etiology of PGD involves acquired factors in addition to congenital morphological anomalies of the femoral neck in the Japanese population. Only racial differences could cause variations in the correlation of age with PGD. However, regarding the relationship between PGD and spino-pelvic parameters, only PT showed a possible correlation with PGD in our study. An increase in PT indicates pelvic retroversion with age. Thus, instability due to decreased coverage of the antero-lateral femoral head, resulting from pelvic retroversion between the acetabulum and femoral head, might result in PGD as a physiological response.
Another notable result of this study was that the presence of PGD alone was not correlated with either hip pain or joint space narrowing. Based on previous studies from Western countries, PGD is considered susceptible to impingement between the anterior femoral neck and the adjacent acetabulum, which is a common cause of hip pain, labral tears, and osteoarthritis5,15,18–20. The difference between our study results and those of previous reports is probably due to the differences in hip joint morphology between Japanese and Western people. Nakamura et al. have evaluated 254 normal hip joints on radiographs and reported that the acetabular roofs of Japanese people are shallower than those of Europeans and Americans21. Moreover, Takeyama et al. reported that the anteroposterior diameter of the femoral neck is smaller in the Japanese than in Europeans and Americans, and an impingement between the anterior femoral neck and the adjacent acetabulum is less likely in this population22. Our findings suggest that the pathological significance of PGD differs between Japan and Western countries. We should consider that this study excluded patients who had hip osteoarthritis (Kellgren-Lawrence grade ≥ 3) and those who had undergone total hip arthroplasty or bilateral hip arthroplasty. Symptoms might not necessarily appear until PGD progresses to hip osteoarthritis. However, historically, Takeyama et al. retrospectively investigated 946 hip joints of patients who underwent hip surgery and reported the prevalence of characteristic findings of FAI (≒PGD) to be 0.6% in Japan22. The actual prevalence of FAI and associated factors, such as hip pain, remain unclear because only a few epidemiological studies on PGD have been conducted in Japan.
This study had several limitations. First, causal relationships between the evaluated variables were not determined because of the cross-sectional study design. Follow-up with a longitudinal study is needed in this cohort. Second, a selection bias might have existed. Among the participants, the proportion of elderly individuals was high because the Research on Osteoarthritis/Osteoporosis Against Disability (ROAD) study was instituted to elucidate the epidemiology of degenerative diseases of locomotive organs. Moreover, regional selection bias should be considered because the subjects (voluntary participants) were recruited from only two regions. However, Yoshimura et al. reported that the participants of the ROAD study are considered representative of the Japanese population23. Thus, these findings may not be generalizable to other populations. Applying the results of this study to different races or countries with different lifestyles would require careful judgment. In the future, we will prospectively investigate the percentage of PGD-positive patients who gradually develop osteoarthritis of the hip and factors affecting the transition from PGD to osteoarthritis of the hip using subsequent ROAD study data.
This study clarified the epidemiological index of PGD and related factors in a general population of Japan. PGD has been considered a congenital morphological variation. However, the results of this study indicate that several acquired factors can be associated with PGD, at least in Japanese people, because the prevalence of PGD increases with age. Moreover, PGD was not significantly associated with hip pain. Although the study is limited by its cross-sectional design and potential selection bias, we believe our results provide new insights into the etiology and clinical significance of PGD.
Materials and methods
Participants
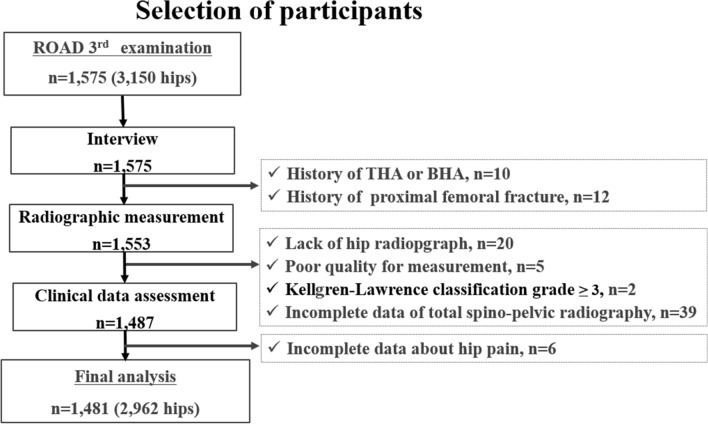
The ROAD study is a nationwide prospective study of bone and joint diseases comprising population-based cohorts from several communities in Japan. The representative bone and joint diseases of the ROAD study are osteoarthritis and osteoporosis. A detailed profile of the ROAD cohort has been previously reported23–28. Briefly, the participants in this study included those recruited during the 3rd examination of the ROAD study, which was conducted from October 2012 to December 2013. In addition to the previous participants, inhabitants of the mountainous area in Hidakagawa (with a population of 11,300 people/330 km2) and coastal areas in Taiji (3,500 people/6 km2) in the Wakayama prefecture (987,500 people/4725 km2) of Japan who were willing to participate in the ROAD survey were also included during this 3rd examination. Overall, 1575 individuals (513 men, 1062 women) participated in the 3rd examination of the ROAD study. Of these participants, 20 (1.3%) did not undergo plain radiography, 7 (0.4%) could not read, 12 (0.8%) had proximal femur fracture, 10 (0.6%) had undergone total hip arthroplasty or bilateral hip arthroplasty, and 2 (0.1%) had hip osteoarthritis (Kellgren-Lawrence grade ≥ 3). In total, 94 individuals, including 43 participants (2.7%) with incomplete spine or hip data, were excluded. The remaining 2962 hips of 1481 participants (94.0%) aged 19–94 years (mean 65.3 years) were included in this study (Fig. 1). The characteristics of the participants are shown in Table 5.
Figure 1.
Flow diagram depicting the study enrollment strategy. Participants in the study are recruited from the residents who participated in the 2012 and 2013 examinations for clinical evaluation, as a part of the Research on Osteoarthritis/Osteoporosis Against Disability (ROAD) study. THA, total hip arthroplasty; BHA, bipolar hip arthroplasty.
Table 5.
Characteristics of the participants.
| Total | Men | Women | |
|---|---|---|---|
| Number of participants (hips) | 1481 (2962) | 491 (982) | 990 (1980) |
| Demographics | |||
| Age (years) | 65.3 ± 13.0 (64.7–66.0) | 66.2 ± 13.8 (65.0–67.4) | 64.9 ± 12.5 (64.1–65.7) |
| Height (cm) | 156.3 ± 9.1 (155.8–156.7) | 164.8 ± 7.2 (164.2–165.5) | 152.0 ± 6.6 (151.6–152.4) |
| Weight (kg) | 56.4 ± 11.3 (55.8–57.0) | 64.6 ± 11.4 (63.6- 65.6) | 52.4 ± 8.7 (51.8–52.9) |
| BMI (kg/m2) | 23 ± 3.5 (22.8–23.2) | 23.7 ± 3.5 (23.4–24.0) | 22.7 ± 3.5 (22.4–22.9) |
| Hip parameters | |||
| CE Angle (° ) | 29.0 ± 6.4 (28.8–29.3) | 29.9 ± 6.0 (29.6–30.3) | 28.6 ± 6.5 (28.3–28.9) |
| mJSW (mm) | 3.9 ± 0.8 (3.9–3.9) | 4.2 ± 0.8 (4.1–4.2) | 3.8 ± 0.7 (3.7–3.8) |
| Spinopelvic parameters | |||
| LL (°) | 45.4 ± 13.7 (44.7–46.1) | 44.1 ± 12.9 (43.0–45.3) | 46.1 ± 14.0 (45.2–47.0) |
| SS (°) | 31.8 ± 9.1 (31.3–32.2) | 31.5 ± 8.7 (30.8–32.3) | 31.9 ± 9.4 (31.3–32.5) |
| PT (°) | 18.2 ± 9.2 (17.7–18.7) | 15.6 ± 7.8 (14.9–16.3) | 19.5 ± 9.6 (18.9–20.0) |
| PI (°) | 49.9 ± 10.7 (49.4–50.5) | 47.2 ± 9.9 (46.3–48.0) | 51.3 ± 10.8 (50.7–52.0) |
Data are means ± standard deviation (95% confidence interval of the mean).
Hip parameters were calculated from 2962 hips.
BMI body mass index, LL lumbar lordosis, S sacral slope, PT pelvic tilt, PI pelvic incidence.
Radiographs of the pelvis, including the hip joints and lumbar spine, were available for the 1481 participants (491 men, 990 women).
The participants completed an interviewer-administered questionnaire, which included questions on family history, medical history, and previous history of hip injury. Anthropometric measurements included height and weight, from which the BMI (weight [kg]/height [m2]) was calculated. Furthermore, all participants were interviewed by well-experienced orthopedists regarding pain in both hips. The orthopedists asked, “Have you experienced right hip pain on most days in the past month, in addition to now?” and “Have you experienced left hip pain on most days in the past month, in addition to now?” Participants who answered “yes” were considered to have hip pain.
Radiographic evaluation
All participants underwent radiographic examination of both hips using the anteroposterior view with weight-bearing and the feet internally rotated. Fluoroscopic guidance with a horizontal anteroposterior X-ray beam was used to properly visualize the joint space. The hip radiographs were read by three well-experienced orthopedic surgeons who were blinded to the participant's clinical status. The following parameters were measured: existence of PGD20,29, CE angle, and mJSW30. Based on past reports by Tannast et al.31 and Fukushima et al.32, we defined PGD as a prominent lateral offset of the femoral head-neck junction. By drawing a circle around the femoral head on the anteroposterior view, the overhang was measured. Instances wherein the femoral head overhang was small were similarly considered PGD-positive cases (Fig. 2).
Figure 2.

Schema of the definition of a PGD-positive case. The overhang is measured by drawing a circle around the femoral head on the anteroposterior view. Even a small overhang of the femoral head (R > r) is considered a PGD-positive case. PGD, pistol grip deformity.
To evaluate the intra-observer variability of the hip parameters, 50 randomly selected radiographs of the hip were analyzed by the same observer > 1 month after the first reading. Additionally, 50 other radiographs were analyzed by the three orthopedic surgeons using the same atlas for interobserver variability. The intra-class and inter-class correlation coefficients for the CE angle were 0.94 and 0.85, respectively, and 0.97 and 0.97, respectively, for mJSW. The interobserver variability for the center of the femoral head was confirmed by kappa analysis to be sufficient for assessment (κ = 1).
Moreover, for spino-pelvic alignment parameters, standing lateral radiographs of the whole spine and pelvis were taken. Each radiograph was aligned such that the edge of the film was the reference for vertical alignment. On the standing lateral radiographs, the following parameters were measured: LL (the Cobb angle from the upper endplate of L1 to the lower endplate of S1), SS (the angle between the tangent line to the superior endplate of S1 and the horizontal plane), PT (the angle between the line connecting the midpoint of the sacral plate to the axes of the femoral heads and the vertical axis), and PI (the angle between the line perpendicular to the sacral plate at its midpoint and the line connecting this point to the axes of the femoral heads) (Fig. 3)33,34.
Figure 3.
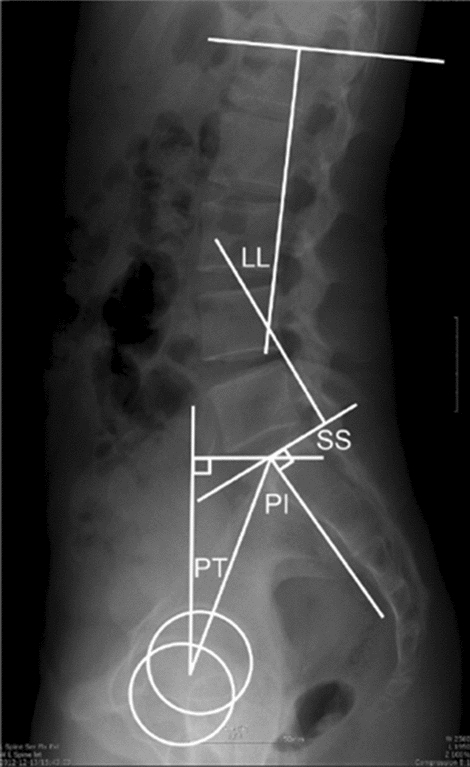
Schema of the measuring methods for each spino-pelvic parameter on a standing radiograph of the whole spine and pelvis. LL, lumbar lordosis; SS, sacral slope; PI, pelvic incidence; PT, pelvic tilt.
Statistical analysis
Statistical analyses were performed using JMP (version 14; SAS Institute Inc., Cary, NC). Continuous variables are expressed as the mean ± standard deviation (SD) and 95% CIs. The participants were classified into five age groups based on birth-year decade: (1) less than 50 years, (2) 50–59 years, (3) 60–69 years, (4) 70–79 years, and (5) 80 years and older. The Cochran-Armitage test was conducted to determine the trend of PGD prevalence among the five age groups. Differences in age, height, weight, BMI, hip parameters, and spino-pelvic parameters were examined between men and women or between the PGD-positive and PGD-negative groups using a non-paired t-test. A chi-square test was conducted to compare the prevalence of PGD between men and women or between the groups (with versus without hip pain). The association of the variables, including age, BMI, sex, spino-pelvic parameters, and hip parameters, with the presence/absence of PGD was examined via multiple logistic regression analysis. Risk ratios or odds ratios are provided with 95% CIs.
Ethics declarations
All participants provided written informed consent for their participation and for the publication of the study in print and in electronic form.
The study was conducted with the approval of the appropriate ethics committees. The establishment of a cohort related to this study has been approved by the Research Ethics Review Committee of the University of Tokyo (No. 1326). The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Supplementary Information
Acknowledgements
The authors wish to thank Dr. Naoki Hirabayashi of the Kawakami Clinic in the town of Hidakagawa; Mrs. Tomoko Takajiri, Mrs. Rie Takiguchi, Mrs. Kyoko Maeda, and other members of the town office in Hidakagawa Town; Dr. Shinji Matsuda of the Shingu Public Health Center; and Mrs. Tamako Tsutsumi, Mrs. Kanami Maeda, Mrs. Megumi Takino, Mrs. Shuko Okada, Mrs. Kazuyo Setoh, Mrs. Chise Ryouno, Mrs. Miki Shimosaki, Mrs. Chika Yamaguchi, Mrs. Yuki Shimoji, and the other members of the town office in the town of Taiji for their assistance in locating and scheduling participants for examinations.
Author contributions
Conception and design of the study: T.T., H.H., K.N., H.K., M.Y., S.T., H.Y., and N.Y. Analysis and interpretation of data: T.T., H.H., W.T., and H.O. Collection and assembly of data: T.T., T.H., T.I., H.H., Y.A., S.M., T.A., and N.Y. Drafting of the article: T.T., and W.T. Critical revision of the article for important intellectual content: T.T., H.H., N.Y., and H.Y. Final approval of article: T.T., H.H., N.Y., and H.Y. T.T. takes responsibility for the integrity of the work in its entirety.
Funding
This work was supported by a Grant-in-Aid for H17-Men-eki-009 (Director, Kozo Nakamura), H20-Choujyu-009 (Director, Noriko Yoshimura), H23-Choujyu-002 (Director, Toru Akune), H25-Choujyu-007 (Director, Noriko Yoshimura), and H25-Nanchitou (Men)-005 (Director, Sakae Tanaka) of the Ministry of Health, Labour and Welfare. Support was also received from Scientific Research, 24659317 (to Noriko Yoshimura); B23390356, C20591774, and Challenging Exploratory Research 23659580 (to Shigeyuki Muraki); Challenging Exploratory Research 24659666 and 21659349, and Young Scientist A18689031 (to Hiroyuki Oka); B23390357 and C20591737 (to Toru Akune); and Collaborating Research with NSF 08033011-00262 (Director, Noriko Yoshimura); from the Ministry of Education, Culture, Sports, Science and Technology in the Japan Osteoporosis Society (2006-1), (Noriko Yoshimura, Shigeyuki Muraki, Hiroyuki Oka, and Toru Akune). Finally, a research aid was obtained from the Japanese Orthopedic Association (JOA-Subsidized Science Project Research 2006-1 and 2010-2; Director, Hiroshi Kawaguchi). The study sponsors played no role in the study design; the collection, analysis, and interpretation of data; the writing of the report; or the decision to submit the paper for publication.
Data availability
All data generated or analyzed during this study are available from the corresponding author upon reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Teiji Harada, Toshiko Iidaka, Hiroshi Yamada and Noriko Yoshimura.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-85521-x.
References
- 1.Murray RO. The aetiology of primary osteoarthritis of the hip. Br. J. Radiol. 1965;38:810–824. doi: 10.1259/0007-1285-38-455-810. [DOI] [PubMed] [Google Scholar]
- 2.Stulberg, S.D. Unrecognized childhood hip disease a major cause of idiopathic osteoarthritis of the hip. In The Hip, Proceedings of the Third Open Scientific Meeting of the Hip Society (eds. Cordell, L.D. et al.) 212–228 (St. Louis MO CV Mosby1975).
- 3.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin. Orthop. Relat. Res. 1999;363:93–99. doi: 10.1097/00003086-199906000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Leunig M, et al. Slipped capital femoral epiphysis: Early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop. Scand. 2000;71:370–375. doi: 10.1080/000164700317393367. [DOI] [PubMed] [Google Scholar]
- 5.Ganz R, et al. Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin. Orthop. Relat. Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 6.Beck M, et al. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin. Orthop. Relat. Res. 2004;481:67–73. doi: 10.1097/00003086-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Agricola R, et al. Cam impingement causes osteoarthritis of the hip: A nationwide prospective cohort study (CHECK) Ann. Rheum. Dis. 2013;72:918–923. doi: 10.1136/annrheumdis-2012-201643. [DOI] [PubMed] [Google Scholar]
- 8.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J. Bone Joint Surg. Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.0810281. [DOI] [PubMed] [Google Scholar]
- 9.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: An integrated mechanical concept. Clin. Orthop. Relat. Res. 2008;466:264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aprato A, et al. Magnetic resonance arthrography for femoroacetabular impingement surgery: Is it reliable? J. Orthop. Traumatol. 2013;14:201–206. doi: 10.1007/s10195-013-0227-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weinberg DS, Gebhart JJ, Liu RW, Salata MJ. Radiographic signs off femoroacetabular impingement are associated with decreased pelvic incidence. Arthroscopy. 2016;32:806–813. doi: 10.1016/j.arthro.2015.11.047. [DOI] [PubMed] [Google Scholar]
- 12.Gebhart JJ, Weinberg DS, Bohl MS, Liu RW. Relationship between pelvic incidence and osteoarthritis of the hip. Bone Joint Res. 2016;5:66–72. doi: 10.1302/2046-3758.52.2000552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clarke MT, Arora A, Villar RN. Hip arthroscopy: Complications in 1054 cases. Clin. Orthop. Relat. Res. 2003;406:84–88. doi: 10.1097/00003086-200301000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Goodman DA, et al. Subclinical slipped capital femoral epiphysis. Relationship to osteoarthrosis of the hip. J. Bone Joint Surg. Am. 1997;79:1489–1497. doi: 10.2106/00004623-199710000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Doherty M, et al. Nonspherical femoral head shape (pistol grip deformity), neck shaft angle, and risk of hip osteoarthritis: A case-control study. Arthritis Rheum. 2008;58:3172–3182. doi: 10.1002/art.23939. [DOI] [PubMed] [Google Scholar]
- 16.Laborie LB, et al. Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology. 2011;260:494–502. doi: 10.1148/radiol.11102354. [DOI] [PubMed] [Google Scholar]
- 17.Lung R, et al. The prevalence of radiographic femoroacetabular impingement in younger individuals undergoing total hip replacement for osteoarthritis. Clin. Rheumatol. 2012;31:1239–1242. doi: 10.1007/s10067-012-1981-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allen D, Beaulé PE, Ramadan O, Doucette S. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J. Bone Joint Surg. Br. 2009;91:589–594. doi: 10.1302/0301-620X.91B5.22028. [DOI] [PubMed] [Google Scholar]
- 19.Wisniewski SJ, Grogg B. Femoroacetabular impingement: An overlooked cause of hip pain. Am. J. Phys. Med. Rehabil. 2006;85:546–549. doi: 10.1097/01.phm.0000219148.00549.e8. [DOI] [PubMed] [Google Scholar]
- 20.Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: The role of hip impingement. Clin. Orthop. Relat. Res. 2004;429:170–177. doi: 10.1097/01.blo.0000150119.49983.ef. [DOI] [PubMed] [Google Scholar]
- 21.Nakamura S, Ninomiya S, Nakamura T. Primary osteoarthritis of the hip joint in Japan. Clin. Orthop. Relat. Res. 1989;241:190–196. [PubMed] [Google Scholar]
- 22.Takeyama A, Naito M, Shiramizu K, Kiyama T. Prevalence of femoroacetabular impingement in Asian patients with osteoarthritis of the hip. Int. Orthop. 2009;33:1229–1232. doi: 10.1007/s00264-009-0742-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yoshimura N, et al. Cohort profile: Research on osteoarthritis/osteoporosis against disability study. Int. J. Epidemiol. 2010;39:988–995. doi: 10.1093/ije/dyp276. [DOI] [PubMed] [Google Scholar]
- 24.Oka H, et al. Normal and threshold values of radiographic parameters for knee osteoarthritis using a computer-assisted measuring system (KOACAD): The ROAD study. J. Orthop. Sci. 2010;15:781–789. doi: 10.1007/s00776-010-1545-2. [DOI] [PubMed] [Google Scholar]
- 25.Muraki S, et al. Prevalence of radiographic knee osteoarthritis and its association with knee pain in the elderly of Japanese population-based cohorts: The ROAD study. Osteoarthr. Cartil. 2009;17:1137–1143. doi: 10.1016/j.joca.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 26.Yoshimura N, et al. Prevalence of knee osteoarthritis, lumbar spondylosis, and osteoporosis in Japanese men and women: The research on osteoarthritis/osteoporosis against disability study. J. Bone Miner. Metab. 2009;27:620–628. doi: 10.1007/s00774-009-0080-8. [DOI] [PubMed] [Google Scholar]
- 27.Iidaka T, et al. Prevalence of radiographic hip osteoarthritis and its association with hip pain in Japanese men and women: The ROAD study. Osteoarthr. Cartil. 2016;24:117–123. doi: 10.1016/j.joca.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 28.Iidaka T, et al. Radiographic measurements of the hip joint and their associations with hip pain in Japanese men and women: The Research on Osteoarthritis/osteoporosis Against Disability (ROAD) study. Osteoarthr. Cartil. 2017;25:2072–2079. doi: 10.1016/j.joca.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 29.Castañeda P, Ponce C, Villareal G, Vidal C. The natural history of osteoarthritis after a slipped capital femoral epiphysis/the pistol grip deformity. J. Pediatr. Orthop. 2013;33(Suppl 1):S76–82. doi: 10.1097/BPO.0b013e318277174c. [DOI] [PubMed] [Google Scholar]
- 30.Conrozier T, et al. Quantitative measurement of joint space narrowing progression in hip osteoarthritis: A longitudinal retrospective study of patients treated by total hip arthroplasty. Br. J. Rheumatol. 1998;37:961–968. doi: 10.1093/rheumatology/37.9.961. [DOI] [PubMed] [Google Scholar]
- 31.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: Radiographic diagnosis–what the radiologist should know. AJR Am. J. Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 32.Fukushima K, et al. Prevalence of radiographic findings of femoroacetabular impingement in the Japanese population. J. Orthop. Surg. Res. 2014;9:25. doi: 10.1186/1749-799X-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: How much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine. 2010;35:2224–2231. doi: 10.1097/BRS.0b013e3181ee6bd4. [DOI] [PubMed] [Google Scholar]
- 34.Asai Y, et al. Sagittal spino-pelvic alignment in adults: The Wakayama Spine Study. PLoS ONE. 2017;12:e0178697. doi: 10.1371/journal.pone.0178697. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are available from the corresponding author upon reasonable request.