What is the natural history of pain in patients treated with vertebroplasty vs those treated conservatively? In this article, the authors analyzed data from patients enrolled in the VERTOS II trial. The end point was 1 year from treatment in 95 conservatively managed patients. Most had sufficient pain relief during the initial 3 months, but at 1 year a substantial portion had disabling pain despite stronger medication. No predicting factors were found. Patients with pain after 3 months may be candidates for vertebroplasty.
Abstract
BACKGROUND AND PURPOSE:
We analyzed the natural course of conservatively treated osteoporotic vertebral compression fractures from VERTOS II, a randomized trial of vertebroplasty and conservative therapy in 202 patients with vertebral compression fractures. We assessed the proportion of patients who developed chronic back pain and possible risk factors.
MATERIALS AND METHODS:
In VERTOS II, the VAS score was assessed at regular intervals until 1 year follow-up. We followed 95 conservatively treated patients until sufficient pain relief, defined as a VAS score ≤3. These patients were censured at the involved follow-up interval. In addition, baseline clinical and imaging data, and class of pain medication used in patients with a VAS score ≤3 at any follow-up interval were compared with those in patients with a VAS score >3 at every follow-up by using logistic regression analysis.
RESULTS:
During 1 year of follow-up, 57 of 95 patients (60%) had sufficient pain relief with VAS scores ≤3. Thirty-eight patients (40%) still had pain with VAS-scores ≥4 at the last follow-up interval of 12 months, despite the use of higher class pain medication. Statistical analysis showed no risk factors.
CONCLUSIONS:
In the VERTOS II trial, most conservatively treated patients with acute osteoporotic compression fractures had sufficient pain relief during the first 3 months. However, after 1 year, a substantial proportion of patients still had disabling pain despite higher class pain medication used. There were no predictors for the development of chronic pain. Patients with continuing pain ≥3 months after the fracture may be candidates for vertebroplasty.
Little is known about the natural course of conservatively treated osteoporotic VCFs. Not all patients with osteoporotic vertebral fractures will have sufficient pain relief. It is assumed that approximately 1 in 5 of these patients eventually will develop chronic back pain as a direct result of the fracture.1,2 In a recent study,3 one-third of patients still had severe pain necessitating pain medication and physical therapy almost 2 years after an acute fracture. In this study, no predictors for transition from acute to chronic pain could be identified.
In VERTOS II,4 an open-label randomized controlled trial comparing vertebroplasty with conservative treatment in patients with osteoporotic vertebral fractures, we found that almost a quarter of conservatively treated patients had no significant pain relief after 1 year.
In the present study, we further analyzed the conservatively treated patients from VERTOS II. In particular, we assessed the proportion of patients who developed chronic back pain. In addition, we evaluated the possible risk factors for the transition from acute to chronic pain.
Materials and Methods
The patients for this study participated in the VERTOS II trial.4 This trial was an open-label randomized controlled trial comparing vertebroplasty and conservative therapy for osteoporotic vertebral fractures in 202 patients. Between October 2005 and June 2008, 202 patients were randomized and 101 patients were assigned to conservative therapy. Informed consent was withdrawn after randomization by 6 patients. The remaining 95 patients were the subjects of the present study.
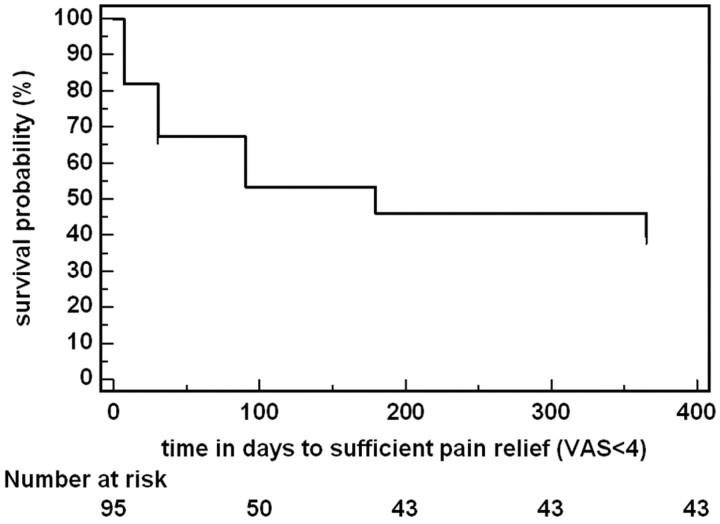
In VERTOS II, the VAS score was assessed at 1 day, 1 week, 1 month, 3 months, 6 months, and 1 year. For the purpose of this study, we followed these conservatively treated patients until sufficient pain relief was achieved, defined as a VAS score ≤3. These patients were censured at the involved follow-up interval. Results were analyzed with Kaplan-Meier survival analysis.
In addition, patients with a VAS score ≤3 at any follow-up interval were compared with patients with a VAS score >3 at every follow-up interval by using logistic regression analysis. We evaluated the following factors: mean age, sex, and baseline data (duration of back pain, VAS score, RMD,5 bone mineral attenuation, number of prevalent fractures, fracture severity, and fracture type according to Genant et al6). In addition, the class of pain medication used at every follow-up interval was compared between patients with VAS >3 and VAS ≤3 by using the Pearson χ2 test. Pain medication was categorized according to World Health Organization classification as the following: 0, no medication; 1, nonopiates (paracetamol, nonsteroidal anti-inflammatory agents); 2, weak opiate derivatives; and 3, strong opiate derivatives.
Results
During 1 year of follow-up, 57 of 95 patients (60%) had sufficient pain relief with VAS scores ≤3. The time intervals until this significant clinical improvement are shown in Fig 1. Most patients had sufficient pain relief during the first 3 months; after this interval, the likelihood of good clinical outcome was very low. On the other hand, 38 patients (40%) still had pain with VAS scores ≥4 at the last follow-up interval of 12 months.
Fig 1.
Kaplan-Meier curve showing the time until significant clinical improvement.
The results of logistic regression analysis comparing patients with a VAS score ≤3 with patients with a VAS score >3 are shown in the Table. There were no significant differences in the evaluated clinical and imaging factors.
Baseline characteristics in relation to clinical outcome
| VAS Score ≤3 | VAS Score >3 | P Value | |
|---|---|---|---|
| No. of patients | 57 | 38 | |
| Age (yr) | 77.7 ± 8.0 | 80.6 ± 8.6 | .30 |
| Female sex (%) | 37 (57) | 28 (61) | .41 |
| Duration of back pain (days) | 29.3 ± 17.1 | 26.8 ± 16.0 | .46 |
| VAS | 7.4 ± 1.5 | 7.9 ± 1.4 | .08 |
| RMD score | 17.8 ± 3.7 | 16.9 ± 4.5 | .32 |
| Number of VCFs | 2.1 ± 1.5 | 2.2 ± 1.5 | .97 |
| Genant et al6 | |||
| Grade 1 | 24 | 12 | .87 |
| Grade 2 | 19 | 12 | |
| Grade 3 | 22 | 7 | |
| Wedge | 46 | 29 | .48 |
| Biconcave | 8 | 7 | |
| Crush | 0 | 0 | |
| Bone density (t-score) | −3.0 ± 1.17 | −3.0 ± 1.02 | .44 |
Patients with VAS >3 used a significantly higher class of pain medication at 1-, 6-, and 12-month follow-up intervals. At the other intervals, this difference was not significant.
Discussion
In this study, we found that 40% of conservatively treated patients with acute osteoporotic compression fractures still had disabling pain after 1 year, despite the higher class of pain medication used at various intervals. Optimal pain medication and supportive therapy were apparently not sufficient for pain relief in a large proportion of these conservatively treated patients. On the other hand, 60% of patients had sufficient pain relief with conservative therapy, almost all within 3 months after the acute fracture. We could not find any predictors for the development of chronic pain. In particular, baseline pain scores, number of fractures, and the degree or shape of vertebral compression had no influence on the development of chronic pain.
The proportion of patients with chronic pain after conservative treatment in the present study is higher than that in previous studies. This can partly be explained by differences in the definition of chronic pain: We defined chronic pain as VAS scores ≥4, while in other studies, including VERTOS II, patients with insufficient decrease in VAS scores were considered to have chronic pain. In these studies,4,11,12 patients with sufficient pain relief could have absolute VAS scores at follow-up of ≥4.
In the natural history of pain after an acute vertebral compression fracture, the time point of 3 months may be of clinical significance. Patients with continuing pain at this time point may be candidates for vertebroplasty.
The effectiveness of vertebroplasty is currently under debate. Most results are based on retrospective observational studies.7–10 Recently, 3 randomized controlled trials concerning vertebroplasty have been published with conflicting results. Investigators in 2 trials11,12 concluded that there is no benefit to vertebroplasty over a sham placebo procedure involving the injection of local anesthetic into the area adjacent to the fracture. In the study by Buchbinder et al,12 78 patients with 1 or 2 painful osteoporotic VCFs were randomized to receive either vertebroplasty or a sham procedure, which included infiltration of anesthetic into the pedicular periosteum. The primary measured outcome was overall pain at 3 months. Despite significant reductions in overall pain in both groups, there was no significant advantage of vertebroplasty over the sham procedure.
In the study by Kallmes et al,11 131 patients with 1–3 painful osteoporotic VCFs were randomized to undergo either vertebroplasty or a simulated sham procedure, which included infiltration of anesthetic into the periosteum of the posterior lamina. The primary outcomes were RMD scores and average pain intensity during the preceding 24 hours at 1 month. Treatment-group crossover was permitted at 1 month. At this time, there was no significant difference between the 2 groups in either the RMD score or the pain rating. In the third trial, VERTOS II,5 vertebroplasty was compared with optimal conservative treatment in 202 patients with VCFs with bone edema on MR imaging, back pain for ≤6 weeks, and a VAS score for pain of ≥5. The primary outcome was pain relief at 1 month and 1 year. The authors concluded that in a subgroup of patients with acute osteoporotic vertebral compression fractures and persistent pain, vertebroplasty is effective and safe. Pain relief after vertebroplasty is immediate, is sustained for at least a year, and is significantly greater than that achieved with conservative treatment, at an acceptable cost.
Next to the lack of blinding in VERTOS II, the most important difference between the 2 sham studies and VERTOS II is patient selection. In the sham studies, both acute and chronic fractures were included, while in VERTOS II, only acute fractures were eligible. In addition, bone edema in the affected vertebra was not a consistent inclusion criterion in the sham studies. The sham studies lacked a control group without intervention. The discordant results from the sham studies, on the one hand, and VERTOS II, on the other hand, have incited much debate. Apparently clinicians still do not know how to best treat their patients. Medical societies understand the need for further randomized trials to support treatment decisions. Until then, on the basis of our findings, we believe it is justified to offer vertebroplasty to patients with compression fractures with insufficient pain relief after 3 months of conservative treatment.
Conclusions
In the VERTOS II trial, most conservatively treated patients with acute osteoporotic compression fractures had sufficient pain relief during the first 3 months. However, after 1 year, a substantial proportion of patients still reported disabling pain. There were no predictors for the development of chronic pain. Patients with continuing pain ≥3 months after the fracture may be candidates for invasive therapy such as vertebroplasty.
ABBREVIATIONS:
- RMD
Roland-Morris Disability score
- VAS
Visual Analog Scale
- VCF
vertebral compression fracture
Footnotes
Disclosures: Caroline Klazen—RELATED: Grant: ZonMW, Cook Medical, Comments: The VERTOS II study was sponsored by ZonMW and a grant from Cook Medical.
References
- 1. Voormolen MH, Mali WP, Lohle PN, et al. Percutaneous vertebroplasty compared with optimal pain medication treatment: short-term clinical outcome of patients with subacute or chronic painful osteoporotic vertebral compression fractures—the VERTOS study. AJNR Am J Neuroradiol 2007; 28: 555– 60 [PMC free article] [PubMed] [Google Scholar]
- 2. Ploeg WT, Veldhuizen AG, The B, et al. Percutaneous vertebroplasty as a treatment for osteoporotic vertebral compression fractures: a systematic review. Eur Spine J 2006; 15: 1749– 58. Epub 2006 Jul 6 [DOI] [PubMed] [Google Scholar]
- 3. Klazen CA, Verhaar HJ, Lohle PN, et al. Clinical course of pain in acute osteoporotic vertebral compression fractures. J Vasc Interv Radiol 2010; 21: 1405– 09 [DOI] [PubMed] [Google Scholar]
- 4. Klazen CA, Lohle PN, de Vries J, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet 2010; 376: 1085– 92. Epub 2010 Aug 9 [DOI] [PubMed] [Google Scholar]
- 5. Roland M, Morris R. A study of the natural history of low-back pain. Part II. Development of guidelines for trials of treatment in primary care. Spine 1983; 8: 145– 50 [DOI] [PubMed] [Google Scholar]
- 6. Genant HK, Wu CY, van Kuijk C, et al. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 1993; 8: 1137– 48 [DOI] [PubMed] [Google Scholar]
- 7. Zoarski GH, Snow P, Olan WJ, et al. Percutaneous vertebroplasty for osteoporotic compression fractures: quantitative prospective evaluation of long-term outcomes. J Vasc Interv Radiol 2002; 13: 139– 48 [DOI] [PubMed] [Google Scholar]
- 8. McGraw JK, Lippert JA, Minkus KD, et al. Prospective evaluation of pain relief in 100 patients undergoing percutaneous vertebroplasty: results and follow-up. J Vasc Interv Radiol 2002; 13: 883– 86 [DOI] [PubMed] [Google Scholar]
- 9. Legroux-Gerot I, Lormeau C, Boutry N, et al. Long-term follow-up of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Clin Rheumatol 2004; 23: 310– 17 [DOI] [PubMed] [Google Scholar]
- 10. Voormolen MH, Lohle PN, Lampmann LE, et al. Prospective clinical follow-up after percutaneous vertebroplasty in patients with painful osteoporotic vertebral compression fractures. J Vasc Interv Radiol 2006; 17: 1313– 20 [DOI] [PubMed] [Google Scholar]
- 11. Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 2009; 361: 569– 79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 2009; 361: 557– 68 [DOI] [PubMed] [Google Scholar]