Abstract
BACKGROUND AND PURPOSE:
Intra-arterial chemotherapy is a very effective treatment option for intraocular retinoblastoma. However, direct catheterization of the OA is not always possible. The purpose of this work was to report our initial results with intra-arterial chemotherapy for intraocular retinoblastoma when delivery of the drug was not via direct catheterization of the OA.
MATERIALS AND METHODS:
Retrospective review of 110 eyes (89 patients) undergoing a total of 351 intra-arterial treatments at our institution between 2006 and 2010 identified 18 eyes (14 patients) that received at least 1 infusion via a vascular route other than direct OA catheterization. Alternatives included catheterization of the orbital branch of the MMA and temporary balloon occlusion of the ICA.
RESULTS:
Tumor control was observed in 17 of 18 eyes at a mean follow-up of 18.9 months (median, 17.5 months; range, 8–36 months). The mean number of intra-arterial infusions was 3.7 per eye (median, 3; range, 2–9). Treatment routes included the following: MMA only, 3 eyes; MMA + OA, 4 eyes; MMA + balloon, 2 eyes; balloon only, 1 eye; balloon + OA, 7 eyes; balloon + OA + MMA, 1 eye. Intra-arterial chemotherapies included melphalan, topotecan, and carboplatin. Complications were all transient. ERG readings were the following: stable, 10 eyes; improved, 3 eyes; reduced, 5 eyes. One patient died from a second malignancy (pinealoblastoma).
CONCLUSIONS:
This initial experience shows that when direct OA catheterization is not possible, using alternative routes of intra-arterial chemotherapy saves eyes and preserves vision with acceptable side effects.
In our center and many others, intra-arterial chemotherapy has become the first-line treatment for eyes with advanced intraocular retinoblastoma.1–5 Ophthalmic intra-arterial chemotherapy is not new, being first put into practice by Reese et al,6 with direct ICA injections of the alkylating agent triethylenemelamine in 1954,7 but the methodology of intra-arterial chemotherapy delivery to the eye continues to evolve as increasing numbers of children receive this treatment.
As more children receive intra-arterial chemotherapy, we have learned that direct catheterization of the OA is not always possible for a number of reasons. In young children, the OA is sometimes too small for catheterization by the usual microcatheters. Anatomic variations are common within the orbit, and rarely, the primary blood supply to the globe comes from another artery, most often the MMA,8 making it impossible to catheterize with the standard direct OA technique. The angle of the OA take off from the ICA can also make catheterization difficult. Even in cases in which previous catheterization of the OA has been successful, subsequent catheterization attempts may fail secondary to a variety of factors, including vasospasm, and alternative delivery of chemotherapy becomes necessary.
This article describes 2 alternative access routes other than the direct OA catheterization technique and presents their angiographic and clinical results.
Materials and Methods
A retrospective review, approved by the Memorial Sloan-Kettering Cancer Center Institutional Review Board, of 110 consecutive eyes with a diagnosis of retinoblastoma receiving intra-arterial chemotherapy from May 2006 to November 2010 was performed. Subjects included in this study had unilateral or bilateral retinoblastoma that could not be treated by using local treatments such as laser and cryotherapy, and many had failed previous treatments including brachytherapy, XRT, and periocular or systemic chemotherapy.
Detailed chart reviews, including review of angiographic operative procedure notes, identified patients who had received at least 1 intra-arterial chemotherapy infusion by alternative routes to direct catheterization of the OA. The technique of superselective intra-arterial chemotherapy via the OA has been previously described in detail by Abramson et al.1,3,5 In our experience, the 2 other vascular routes for therapy include infusion via the MMA (branch of the external carotid artery) and temporary balloon occlusion of the ICA distal to the origin of the OA.9
Procedures
All procedures were performed on an outpatient basis. All patients required general anesthesia with intubation. A 4F micropuncture set was used to access the common femoral artery with subsequent placement of an arterial sheath. The patient was then anticoagulated with intravenous heparin (70 IU/kg). During the first procedure, direct catheterization of the OA was always attempted before considering alternative routes of therapy.5 Once the treatment session was complete, the catheters were removed, the femoral sheath was pulled, and the groin puncture was closed with manual pressure. Anesthesia was discontinued, and the child was observed for 4–6 hours and was discharged the same day.
If direct catheterization of the OA was not possible or there was inadequate injection of the OA with no visualization of the choroidal crescent, then treatment via the OA was abandoned. According to the flow pattern in the OA and the angioanatomy (Fig 1A, -B), alternative routes of chemotherapy delivery, through the MMA or by balloon assistance, were then performed.
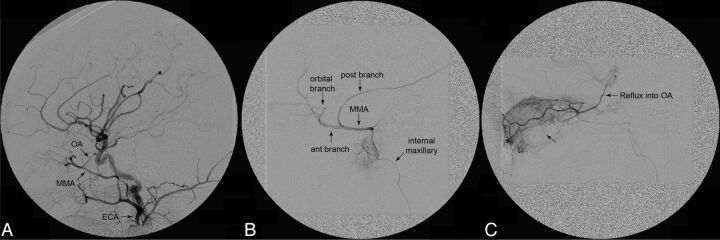
Fig 1.
Procedural angiograms: catheterization of the MMA. A, Common carotid angiogram, lateral view, shows both the OA arising from the ICA and the MMA arising from the external carotid artery. The microcatheter was first placed into the OA, but because of its small size, there was stagnation of contrast (flow arrest). Therefore, the decision was made to treat via the MMA. B, Preliminary lateral angiogram showing the vascular anatomy of the MMA and its orbital branch. C, Lateral angiogram showing excellent choroidal crescent (arrow without label) and reflux into the OA after radiopaque contrast injection via the orbital branch of the MMA.
Catheterization through the MMA
The microcatheter was advanced from the aortic arch into the external carotid artery and guided into the MMA via the internal maxillary artery (Figs 1 and 2), where an angiogram was performed to visualize the orbital branch of the MMA. If it was well-developed, then the orbital branch was catheterized (Fig 1B), another angiogram was performed to visualize the choroidal blush (Fig 1C, arrow without label), and chemotherapy infusion was initiated.
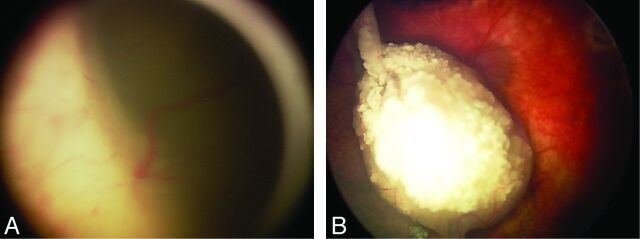
Fig 2.
External carotid artery orbital vascular anatomy. A, Superior view of the orbital vascular supply via the MMA. B, Anterior view of the orbit, the lacrimal foramen (also known as the Hytl foramen), located superolateral to the superior orbital fissure, is the route by which the orbital branch of the MMA may enter the orbit. C, A lateral view of the vascular supply to the orbit via the MMA (zygomatic, frontal, temporal, and greater wing of the sphenoid bones partially cut away; additionally the lesser wing of sphenoid bone to the anterior clinoid process has been cut away to show the OA entering the orbit).
Balloon-Assisted Infusion
Alternatively, if the ophthalmic anastomosis of the MMA was not well-developed, then the decision was made to infuse chemotherapy by using temporary balloon occlusion of the ICA just distal to the branch point for the OA. The technique is similar to the one used by Yamane et al,9 except that our balloon microcatheter is guidewire-directed instead of flow-guided. In summary, a 5F femoral sheath was placed, and a 5F guide catheter was advanced into the ICA. The balloon microcatheter (HyperForm 4 × 7; ev3, Irvine, California) was advanced into the guide catheter and into the supraophthalmic segment of the ICA (Fig 3). The balloon was carefully inflated under fluoroscopy to match the diameter of the ICA, so as to redirect all internal carotid flow into the OA. Angiography was performed to look for the choroidal crescent (Fig 3B, arrow). Infusion of drugs was then performed, alternating 4-minute balloon inflation (infusion time) and 2-minute balloon deflation (reperfusion time). With balloon assistance, drugs were each diluted in 6 mL of normal saline and infused during 4 minutes (infusion time). This procedure limits the number of balloon inflations to a maximum of 3 during a single treatment session if 3 drugs are used.
Fig 3.
Procedural angiograms: balloon-assisted method. A, Unsubtracted lateral view showing the inflated balloon catheter in the ICA, just distal to the origin of the OA. Note the ocular prosthetic after enucleation of the contralateral eye. B, Subtracted ICA angiogram, lateral view, balloon-inflated, showing the exclusive filling of the OA by the radiopaque contrast. Notice filling of contrast into the OA and consequent choroidal blush (arrow).
When we used these alternative routes, no patient failed to receive intra-arterial chemotherapy during any planned treatment session.
A detailed description of chemotherapy drug dose determination and appropriate combination drug treatment has been previously described.5,10 In brief, chemotherapeutic agents included melphalan, 2.5–7.5 mg, carboplatin, 30–50 mg, and topotecan, 0.15–0.5 mg. The highest dose of chemotherapy administered in a session to a single eye was melphalan, 7.5 mg, + carboplatin, 50 mg, + topotecan, 0.5 mg. Dosage, combination of chemotherapy administered, and number of treatment sessions were determined by age, individual angioanatomy10 of the OA and its branches, patient weight, extent of disease (with particular attention to the extent of vitreous seeding), and clinical response to previous intra-arterial treatments.
Following each intra-arterial treatment session, tumor regression pattern, decrease in tumor size, improvement of tumor seeding (either diminution or calcification), and resolution of retinal detachment were used as objective measures to determine the effectiveness of individual treatment sessions.
Ophthalmic examinations were performed every 3–4 weeks after treatment and included external examination, visual acuity testing, intraocular pressure measurement, pupil and motility evaluation, and a complete fundus examination with the patient under anesthesia, including RetCam III digital photography (Massie Industries, Dublin, California), B-scan sonography with the OTI unit (Ophthalmic Technologies, Toronto, Ontario, Canada), and ERG testing under photopic and scotopic conditions in accordance with modified International Society for Clinical Electrophysiology of Vision standards as described in a previous publication.11 The amplitude of the response to a 30-Hz flicker, measured in microvolts, was compared from visit to visit. ERG readings were grouped according to 6 categories: none (0.0 mV), poor (0.2–25 mV), fair (25.1–50.0 mV), good (50.1–75.0 mV), very good (75.1–100 mV), and excellent (>100 mV). An absolute change of ≥25 mV compared with previous readings was considered to be a notable change. Systemic evaluation included interval history, height and weight measurements, and CBC 7–14 days after the procedure.
Statistical Analysis
A 2-tailed paired t test comparing ERG readings before and after intra-arterial treatment was performed by using GraphPad Prism, Version 5.00 for Windows (GraphPad Software, San Diego, California; www.graphpad.com).
Results
Ocular Survival
Tumor control was observed in 17 of 18 eyes (94.4%) at a mean follow-up of 18.9 months. One eye was enucleated 18 months after initial intra-arterial treatment session due to inadequate tumor control.
Patient Survival
Thirteen of 14 patients (92.9%) are alive. One patient with bilateral retinoblastoma died 29 months after the first intra-arterial treatment session due to a second malignancy (pinealoblastoma).
Of the 110 consecutive eyes treated with intra-arterial chemotherapy (Table 1), we identified 18 eyes (16%, 18/110) that received at least 1 intra-arterial treatment through an alternative route to the OA. These 18 eyes received 67 intra-arterial infusions: 23 were by direct OA catheterization, 27.5 by catheterization of the MMA, and 16.5 by balloon-assisted infusion (Table 1). On 1 occasion, the orbital branch of the MMA was successfully catheterized and the first drug was successfully infused, but midway through infusion of the second drug, fluoroscopy demonstrated retrograde migration of the catheter into the proximal anterior segment of the MMA. At this point, the microcatheter was repositioned in the orbital branch of the MMA. However, subsequent contrast injections performed under fluoroscopy demonstrated unstable microcatheter position due to the small size of the arterial branch, and a decision was then made to switch to the balloon occlusion technique. Given the infusion of chemotherapy via both the MMA and the balloon-assisted method during this 1 treatment session, this procedure was ascribed a 0.5 treatment session value via the MMA and a 0.5 treatment session value via the balloon-assisted method for purposes of quantification in this study.
Table 1:
IA treatment characteristics of cohort
| Characteristic | No. |
|---|---|
| Cumulative eyes treated with IA | 110 |
| Cumulative patients treated with IA | 89 |
| Cumulative IA treatments | 351 |
| Eyes treated with alternative to OA (study cohort) | 18 |
| Patients treated with alternative to OA (study cohort) | 14 |
| Total alternatives to OA injections | 67 |
| Total OA infusions | 23 |
| Total MMA infusions | 27.5 |
| Total balloon infusions | 16.5 |
| Eyes treated other than via OA with previous IV chemotherapy/cryotherapy/laser | 16 |
Note:—IA indicates intra-arterial.
Among all intra-arterial treatments (n = 351) reviewed during the time of this study, overall 12.5% (n = 44 of 351 infusions) of infusions occurred through an alternative route to the OA, 7.8% (n = 27.5 of 351 infusions) via the MMA and 4.7% (n = 16.5 of 351 infusions) via balloon-assisted infusion. A summary of the treatment routes is detailed in Table 2. Eyes underwent 2–9 intra-arterial treatment sessions each (mean, 3.7; median, 3). RetCam images before and after treatment for 1 case treated via the MMA are presented in this report (Fig 4). Chemotherapy regimens used at individual treatment sessions are detailed in Table 3; the most common regimens used included single-agent melphalan in 23 sessions and a combination of melphalan + topotecan in 24 treatment sessions—together these 2 drug treatment regimens represent 70% of the treatments administered in this cohort.
Table 2:
Routes and frequency of administration of IA chemotherapya
| Route | Eyes | Mean Total Tx | Median Total Tx | Min Tx | Max Tx |
|---|---|---|---|---|---|
| MMA Only | 3 | 4 | 3 | 3 | 6 |
| MMA + OA | 4 | 4.75 | 4 | 2 | 9 |
| MMA + balloon | 2 | 3 | 3 | 2 | 4 |
| Balloon only | 1 | 3 | 3 | 3 | 3 |
| Balloon + OA | 7 | 3.29 | 3 | 2 | 5 |
| Balloon + OA + MMA | 1 | 4 | 4 | 4 | 4 |
| Total | 18 | 3.72 | 3 | 2 | 9 |
Note:—IA indicates intra-arterial; MMA, IA infusion via the orbital branch of the MMA; Balloon, IA infusion via the OA through a balloon-assisted method; Min, minimum; Max, maximum; Tx, treatment session.
All values listed as No.
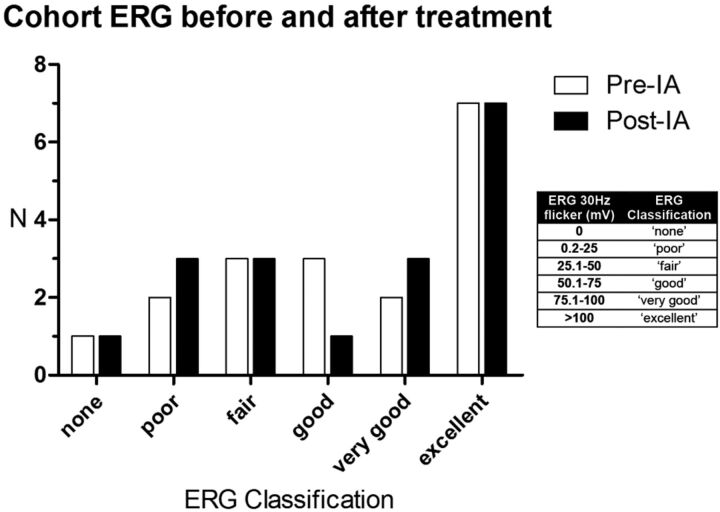
Fig 4.
RetCam images before and after intra-arterial treatment only via the MMA. The left eye of a child with bilateral retinoblastoma successfully treated with 6 intra-arterial chemotherapy infusions (melphalan + topotecan × 3, melphalan × 2, melphalan + topotecan + carboplatin × 1) via the MMA. No significant change in ERG function was noted after 6 treatment sessions. Left, pretreatment image; right, after 6 intra-arterial infusions.
Table 3:
Summary of chemotherapeutic agents used at individual treatment sessionsa
| Chemotherapeutic Agent | Number of Tx |
|---|---|
| Melphalan + topotecan | 24 |
| Melphalan | 23 |
| Melphalan + topotecan + carboplatin | 11 |
| Carboplatin + topotecan | 7 |
| Carboplatin | 2 |
| Total IA infusions | 67 |
Note:—IA indicates intra-arterial; Tx, single IA treatment session.
All values listed as No.
Mean follow-up was 18.9 months (median, 17.5 months; range, 8–36 months). Mean age at follow-up was 39.4 months (median, 37 months; range, 11–83 months). The RE included: RE II, 3 eyes; RE III, 4 eyes; and RE V, 11 eyes (International Classification of Retinoblastoma: group B, 5 eyes; group C, 3 eyes; and group D, 10 eyes). Retinoblastoma was bilateral in 79% of patients.
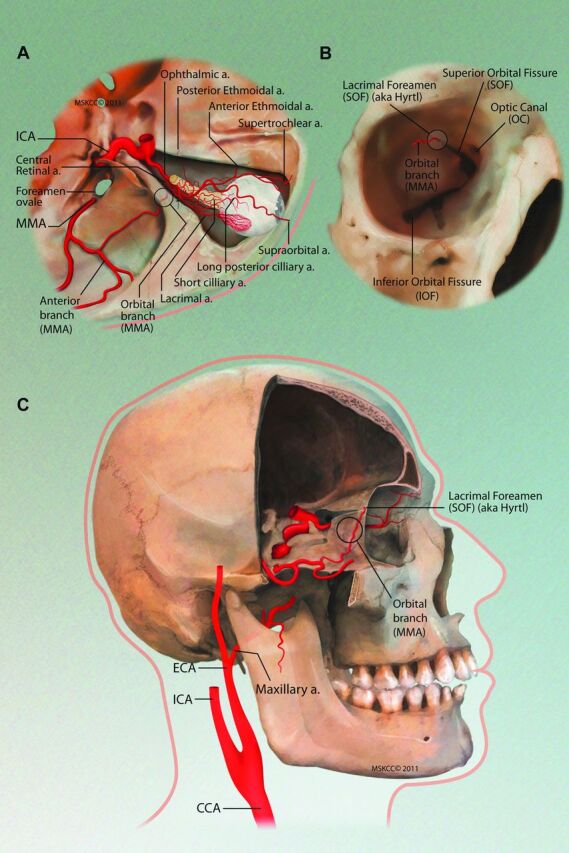
ERGs
ERGs performed before and after most recent intra-arterial treatments were available for all 18 eyes. Most (10 eyes) maintained stable ERG readings after treatment, and 3 eyes showed improvement. A decreased ERG reading posttreatment was noted in 5 eyes compared with pretreatment reading. A distribution of the ERG classification of this cohort of eyes before and after treatment is shown in Fig 5.
Fig 5.
Cohort ERG before and after intra-arterial treatment sessions. Graph showing ERG classification of all eyes included in this study before and after all intra-arterial treatments.
A paired 2-tailed t test comparing the ERG readings before and after intra-arterial treatment of the entire cohort showed no significant change (P = .3395). Likewise, a paired 2-tailed t test comparing the ERG readings before and after intra-arterial treatment for the subgroup of 6 eyes treated solely through alternatives to OA catheterization showed no significant change (P = .9354).
Ocular and Systemic Complications
There were no adverse effects on ocular motility, cornea, anterior chamber, lens, or orbit. There were no cases of central retinal artery occlusion. Local complications included transient medial forehead hyperemia (3.0%, n = 2), nasal loss of lashes (3.0%, n = 2), and lid edema (1.5%, n = 1) after individual intra-arterial treatment sessions, constant with previous reports of these temporary side effects of intra-arterial chemotherapy.12 Bronchospasm (significant 13.4%, n = 9; mild, 6.0%, n = 4) was noted in a minority of cases during the angiographic procedure and was adequately treated with injection of epinephrine bitartrate intravenously.5 No episodes of sustained bradycardia were observed. There were no neurologic deficits or any other complications.
Neutropenia (Common Terminology Criteria for Adverse Events, v3.0, grade 3 or higher; http://bioportal.bioontology.org/ontologies/1415) was observed after 15 of 40 (for those with available CBC results) intra-arterial treatment sessions (37.5%), most commonly when the melphalan dose exceeded 0.4 mg/kg of body weight, which most often occurred during tandem treatment sessions. The toxicity was grade 3 (absolute neutrophil count, 500–1000 mm3) in 12 cases and grade 4 (absolute neutrophil count, <500 mm3) in 3 cases. One patient previously treated with 6 cycles of systemic intravenous chemotherapy was hospitalized after 2 intra-arterial treatment sessions. The first hospitalization was for intravenous fluid hydration due to poor oral intake secondary to mucositis. The second hospitalization was for neutropenic (grade 4) fever requiring intravenous antibiotics and transfusion of blood products (1 unit of packed red blood cells, 1 unit of platelets). No other patients in this series were hospitalized, experienced febrile neutropenia, or required transfusion after intra-arterial treatment.
Discussion
Prior studies have demonstrated that the OA catheterization technique can be used successfully as a primary therapy,3 especially with advanced disease,1,5,13 in bilateral cases (treating both eyes),2 and in eyes that have previously failed conventional management.1,5,13 This article shows that 2 alternative routes to OA catheterization (by using the MMA or temporary balloon occlusion of the ICA) are feasible and safe for the treatment of intraocular retinoblastoma. Two case reports have also examined other routes aside from direct OA catheterization for the delivery of intra-arterial chemotherapy for the treatment of retinoblastoma.14,15
In 1968, Kiribuchi and Hasegawa16 compared the tissue concentration of mitomycin in dogs when treated intra-arterially via the common carotid artery and the external OA by way of the infraorbital artery. Despite an equal dose of 2 mg of mitomycin, they reported universally higher doses in the aqueous, vitreous, and retina/uvea when injected via the infraorbital artery compared with the common carotid artery. When the chemotherapy was injected via the common carotid artery, there was no detectable mitomycin level in the vitreous body. This finding highlights the potential advantage of selective infusion to deliver higher concentrations of drug to the eye, especially the vitreous.
In humans, the MMA may form an anastomosis with the lacrimal artery soon after it branches off the OA (Fig 2); this anastomosis is called the orbital branch of the MMA and enters the orbit through the Hyrtl foramen or, when this foramen is not separated from it, through the most lateral aspect of the superior orbital fissure. When this orbital branch is developed enough to be catheterized, contrast or chemotherapy drugs can be injected to fill the lacrimal artery and reflux into the OA, resulting in flow of chemotherapy to the eye through the normal ciliary and retinal circulation. Additionally, the most prevalent (but rare) alternative origin of the OA, reported as early as 1887, is from the MMA,8,17 which can be another alternative anatomic route for delivery of intra-arterial chemotherapy to the eye.
Tumor control was achieved in 17 of 18 eyes at a mean follow-up of 18.9 months. One eye with advanced intraocular disease (RE group Vb) that had previously failed systemic chemotherapy required enucleation due to tumor progression despite intra-arterial treatment. One patient with bilateral intraocular retinoblastoma died due to a second malignancy (pinealoblastoma). A limitation of this study is that 16 of 18 eyes had received previous intravenous chemotherapy or concomitant therapies including cryotherapy and local laser photocoagulation, potentially confounding the effect of intra-arterial treatment, but these eyes were referred for intra-arterial treatment due to failure of these previous treatments. The alternative routes to direct OA catheterization are able to achieve excellent tumor control. For instance, an eye with advanced disease that failed treatment with intravenous chemotherapy (carboplatin + vincristine sulfate) achieved tumor control and globe preservation with 6 intra-arterial treatments via the MMA and 1 session of focal laser photocoagulation (Fig 4).
Intra-arterial chemotherapy was well-tolerated. Local side effects were transient and minor. We observed no vitreous hemorrhage or arteriopathy (choroidal or intraretinal) after intra-arterial treatment. No neutropenia was noted after a majority (62.5%) of treatment sessions, which is consistent with a larger recent study from Gobin et al.5 One child who failed to achieve tumor reduction with 6 cycles of intravenous vincristine, etoposide, and carboplatin was subsequently treated at our center with 4 cycles of intra-arterial chemotherapy. The final 2 intra-arterial treatments resulted in 2 hospitalizations: the first for 1 day of intravenous hydration secondary to poor oral intake due to mucositis and the second for neutropenic fever that necessitated prophylactic intravenous antibiotics along with transfusion of blood products (1 unit of packed red blood cells, 1 unit of platelets). In this case, the small dose of chemotherapy used intra-arterially caused myelosuppresion, perhaps because the patient had been treated before with extensive systemic chemotherapy. No other child required any transfusion of blood products, had fever with neutropenia, or was hospitalized for treatment-related complications. No severe systemic complications including nausea, vomiting, alopecia, severe systemic infection requiring intravenous antibiotics, or failure to thrive, which commonly occur with intravenous chemotherapy,18 were observed.
XRT, the oldest form of ocular salvage therapy, is able to save up to 53.4% of advanced (RE group Vb) eyes at 10-year follow-up, but most (52.4%) patients are plagued with significant side effects, including cataract, vitreous hemorrhage, radiation retinopathy, radiation optic neuropathy, and facial bone hypoplasia among others.19 XRT also increases the risk of second nonocular cancers (sarcomas), particularly in patients with heritable retinoblastoma.20,21 In low-grade retinoblastoma (RE group I-II), focal therapy in combination with systemic therapy can offer good tumor control, with Murphree et al22 reporting 100% tumor control for these eyes. Another study reported 100% tumor control for RE group I-III eyes with chemoreduction and focal therapy, but for RE group IV eyes only 66% avoided enucleation or XRT.23 Shields et al24 report that RE group I-IV eyes treated with chemoreduction and focal therapy required additional XRT in 10% of cases and enucleation in 15% at 5-year follow-up. Among RE group V eyes, however, 47% required XRT and 53% required enucleation at 5 years, highlighting the inadequacy of this treatment technique for patients with advanced disease. In comparison, a large study investigating intra-arterial chemotherapy for eyes with advanced RE group V retinoblastoma showed that the Kaplan-Meier estimate of ocular event-free survival at 2 years for all group V eyes was 80.5% when used as a primary treatment and was still 51.5% when used as an alternative to enucleation after failure of previous treatments with intravenous chemotherapy or XRT.5
Moreover, intravenous chemotherapy is not without significant side effects regardless of stage of disease. Adverse effects of systemic chemotherapy include nausea, vomiting, alopecia, severe myelosuppresion,18 failure to thrive,25 otoxicity,26 and acute myelogenous leukemia.27 In contrast, minimal side effects are observed with intra-arterial chemotherapy, given the small amount of chemotherapeutic administered. Intra-arterial chemotherapy for advanced retinoblastoma is an important alternative treatment, given its preliminary success and lack of frequent severe systemic side effects.
Conclusions
For the 16% of eyes in which direct catheterization of the OA is not possible, alternative techniques, such as the balloon technique or access through the MMA, appear to be safe and effective routes for administering local chemotherapy for the treatment of intraocular retinoblastoma.
Acknowledgments
We thank Tony Riley and the Medical Illustration Department of Memorial Sloan-Kettering Cancer Center for their artistic skill in creating an illustration.
ABBREVIATIONS:
- CBC
complete blood count
- ERG
electroretinogram
- MMA
middle meningeal artery
- OA
ophthalmic artery
- RE
Reese-Ellsworth group
- XRT
external beam radiation therapy
Footnotes
Disclosures: Michael A. Klufas—RELATED: Support for Travel to Meetings for the Study or Other Purposes: Memorial Sloan-Kettering Cancer Center provided funding for travel to present this work at the International Society of Ocular Oncology Biennial Meeting, November 14–17, 2011, in Buenos Aires, Argentina.
This work was supported in part by a grant from the Fund for Ophthalmic Knowledge Inc, New York, New York, and the Alcon Research Institute, Fort Worth, Texas.
Paper previously presented at: Biennial Meeting of the International Society of Ocular Oncology, November 14–17, 2011; Buenos Aires, Argentina.
References
- 1. Abramson DH, Dunkel IJ, Brodie SE, et al. A phase I/II study of direct intraarterial (ophthalmic artery) chemotherapy with melphalan for intraocular retinoblastoma initial results. Ophthalmology 2008; 115: 1398– 404, 1404.e1. Epub 2008 Mar 14. [DOI] [PubMed] [Google Scholar]
- 2. Abramson DH, Dunkel IJ, Brodie SE, et al. Bilateral superselective ophthalmic artery chemotherapy for bilateral retinoblastoma: tandem therapy. Arch Ophthalmol 2010; 128: 370– 72 [DOI] [PubMed] [Google Scholar]
- 3. Abramson DH, Dunkel IJ, Brodie SE, et al. Superselective ophthalmic artery chemotherapy as primary treatment for retinoblastoma (chemosurgery). Ophthalmology 2010; 117: 1623– 29. Epub 2010 Apr 9 [DOI] [PubMed] [Google Scholar]
- 4. Abramson DH. Super selective ophthalmic artery delivery of chemotherapy for intraocular retinoblastoma: ‘chemosurgery' the first Stallard lecture. Br J Ophthalmol 2010; 94: 396– 99 [DOI] [PubMed] [Google Scholar]
- 5. Gobin YP, Dunkel IJ, Marr BP, et al. Intra-arterial chemotherapy for the management of retinoblastoma: four-year experience. Arch Ophthalmol 2011; 129: 732– 37 [DOI] [PubMed] [Google Scholar]
- 6. Reese AB, Hyman GA, Merriam GR, Jr, et al. Treatment of retinoblastoma by radiation and triethylenemelamine. AMA Arch Ophthalmol 1954; 53: 505– 13 [DOI] [PubMed] [Google Scholar]
- 7. Hyman GA, Reese AB. Combination therapy of retinoblastoma with triethylene melamine and radiotherapy. J Am Med Assoc 1956; 162: 1368– 73 [DOI] [PubMed] [Google Scholar]
- 8. Hayreh SS. Orbital vascular anatomy. Eye (Lond) 2006; 20: 1130– 44 [DOI] [PubMed] [Google Scholar]
- 9. Yamane T, Kaneko A, Mohri M. The technique of ophthalmic arterial infusion therapy for patients with intraocular retinoblastoma. Int J Clin Oncol 2004; 9: 69– 73 [DOI] [PubMed] [Google Scholar]
- 10. Gobin YP, Cloughesy TF, Chow KL, et al. Intra-arterial chemotherapy for brain tumors by using a spatial dose fractionation algorithm and pulsatile delivery. Radiology 2001; 218: 724– 32 [DOI] [PubMed] [Google Scholar]
- 11. Brodie SE, Gobin YP, Dunkel IJ, et al. Persistence of retinal function after selective ophthalmic artery chemotherapy infusion for retinoblastoma. Doc Ophthalmol 2009; 119: 13– 22 [DOI] [PubMed] [Google Scholar]
- 12. Marr B, Gobin PY, Dunkel IJ, et al. Spontaneously resolving periocular erythema and ciliary madarosis following intra-arterial chemotherapy for retinoblastoma. Middle East Afr J Ophthalmol 2010; 17: 207– 09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vajzovic LM, Murray TG, Aziz-Sultan MA, et al. Supraselective intra-arterial chemotherapy: evaluation of treatment-related complications in advanced retinoblastoma. Clin Ophthalmol 2011; 5: 171– 76. Epub 2011 Feb 10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cooke D, Farid H, Kim W, et al. Zygomatico-orbital intra-arterial melphalan infusion for intraocular retinoblastoma. J Neurointerv Surg 2012; 4: e16 [DOI] [PubMed] [Google Scholar]
- 15. Pham CT, Blanc R, Rouic LL, et al. Access to the ophthalmic artery by retrograde approach through the posterior communicating artery for intra-arterial chemotherapy of retinoblastoma. Neuroradiology 2011. November 18. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 16. Kiribuchi M, Hasegawa H. Retrograde infusion of anti-cancer drugs to the ophthalmic artery for intra ocular malignant tumors [in Japanese]. Iryo 1968; 22: 772– 76 [PubMed] [Google Scholar]
- 17. Hayreh SS, Dass R. The ophthalmic artery. I. Origin and intra-cranial and intra-canalicular course. Br J Ophthalmol 1962; 46: 65– 98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Benz MS, Scott IU, Murray TG, et al. Complications of systemic chemotherapy as treatment of retinoblastoma. Arch Ophthalmol 2000; 118: 577– 78 [PubMed] [Google Scholar]
- 19. Abramson DH, Beaverson KL, Chang ST, et al. Outcome following initial external beam radiotherapy in patients with Reese-Ellsworth group Vb retinoblastoma. Arch Ophthalmol 2004; 122: 1316– 23 [DOI] [PubMed] [Google Scholar]
- 20. Abramson DH, Melson MR, Dunkel IJ, et al. Third (fourth and fifth) nonocular tumors in survivors of retinoblastoma. Ophthalmology 2001; 108: 1868– 76 [DOI] [PubMed] [Google Scholar]
- 21. Wong FL, Boice JD, Jr, Abramson DH, et al. Cancer incidence after retinoblastoma: radiation dose and sarcoma risk. JAMA 1997; 278: 1262– 67 [DOI] [PubMed] [Google Scholar]
- 22. Murphree AL, Villablanca JG, Deegan WF, 3rd, et al. Chemotherapy plus local treatment in the management of intraocular retinoblastoma. Arch Ophthalmol 1996; 114: 1348– 56 [DOI] [PubMed] [Google Scholar]
- 23. Friedman DL, Himelstein B, Shields CL, et al. Chemoreduction and local ophthalmic therapy for intraocular retinoblastoma. J Clin Oncol 2000; 18: 12– 17 [DOI] [PubMed] [Google Scholar]
- 24. Shields CL, Honavar SG, Meadows AT, et al. Chemoreduction plus focal therapy for retinoblastoma: factors predictive of need for treatment with external beam radiotherapy or enucleation. Am J Ophthalmol 2002; 133: 657– 64 [DOI] [PubMed] [Google Scholar]
- 25. Rizzuti AE, Dunkel IJ, Abramson DH. The adverse events of chemotherapy for retinoblastoma: what are they? Do we know? Arch Ophthalmol 2008; 126: 862– 65 [DOI] [PubMed] [Google Scholar]
- 26. Jehanne M, Lumbroso-Le Rouic L, Savignoni A, et al. Analysis of ototoxicity in young children receiving carboplatin in the context of conservative management of unilateral or bilateral retinoblastoma. Pediatr Blood Cancer 2009; 52: 637– 43 [DOI] [PubMed] [Google Scholar]
- 27. Gombos DS, Hungerford J, Abramson DH, et al. Secondary acute myelogenous leukemia in patients with retinoblastoma: is chemotherapy a factor? Ophthalmology 2007; 114: 1378– 83 [DOI] [PubMed] [Google Scholar]