Abstract
BACKGROUND AND PURPOSE:
Flow-diverting devices now offer a new treatment alternative for cerebral aneurysms. We present the results of a large single-center series of patients treated with the PED, including long-term follow-up.
MATERIALS AND METHODS:
Between November 2008 and September 2011, sidewall aneurysms with a wide neck (≥4 mm) or unfavorable dome-neck ratio (≤1.5); large/giant, fusiform, dissecting, blisterlike, and recurrent sidewall aneurysms; aneurysms at difficult angles; and aneurysms in which a branch was originating directly from the sac were treated with the PED. Patients were premedicated with dual antiplatelet medications. Data, including demographics, aneurysm features, clinical presentation, complications, results, and follow-up information, for up to 2 years are presented.
RESULTS:
Two hundred fifty-one aneurysms in 191 patients were treated. Of these, 96 (38.3%) were large or giant (≥10 mm). In 34/251 (13.5%), PEDs were used for retreatment. Adjunctive coiling was performed in 11 aneurysms (2.1%). The mean number of devices per aneurysm was 1.3. One aneurysm ruptured in the fourth month posttreatment (0.5%), and symptomatic in-construct stenosis was detected in 1 patient (0.5%) treated with percutaneous transarterial angioplasty. Any event rate was 27/191 (14.1%), with a permanent morbidity of 1% and mortality of 0.5%. Control angiography was available in 182 (95.3%) patients with 239 (95.2%) aneurysms. In 121 aneurysms (48.2%), 1- to 2-year control angiography was available. The aneurysm occlusion rate was 91.2% in 6 months, increasing to 94.6%.
CONCLUSIONS:
Use of the PED is safe, efficacious, and durable in cerebral aneurysm treatment, with low morbidity-mortality and high occlusion rates as confirmed with mid- to long-term control angiography.
Although endovascular coiling has been proved effective in the treatment of cerebral aneurysms,1,2 there are still limitations in the treatment of wide-neck, large or giant, and nonsaccular fusiform aneurysms. Although self-expandable stents enabled the endovascular treatment of some previously so-called “uncoilable” aneurysms,3–5 parent artery occlusion with or without accompanying bypass surgery still seems to be the only treatment for many challenging aneurysms.6 Moreover, there is recurrence of some aneurysms necessitating ≥1 retreatment for the endovascular techniques, which are almost exclusively focused on embolization of the sac with or without adjunctive stent placement.7–10
The concept of flow change resulting in spontaneous aneurysm thrombosis was reported in aneurysms treated with the sole implantation of ≥1 stent.11–14 Now, in recent years, flow diversion performed with dedicated devices has emerged as a new concept, and several articles, including in vitro studies,15,16 case presentations,17–19 and, lately, several series,20–24 have offered promising results.
The PED (ev3 Neurovascular, Irvine, California) is a self-expanding, microcatheter-delivered, cylindrical mesh device composed of 48 braided individual cobalt chromium and platinum strands.18 The device has a 30%–35% metal surface area coverage when fully deployed.
Herein, we present the treatment and follow-up results of ≤2 years in a series of 251 aneurysms in 191 patients who were treated with the PED. This is not only the largest single-center series in which flow diverters were used, but it also provides long-term results.
Materials and Methods
This retrospective study included 251 aneurysms treated with PEDs in 191 consecutive patients (mean age, 49.2 years; age range, 26–71 years; except for 1 pediatric patient who was 13 years of age) between November 2008 and September 2011. One hundred twenty-nine patients were female and 62 were male. Following ethics committee approval, 17 of the patients were included in the Pipeline for Uncoilable or Failed Aneurysms Study. Written informed consent was obtained from each patient. Sidewall aneurysms with wide necks (≥4 mm) or unfavorable dome-neck ratios (≤1.5) (Fig 1), large or giant aneurysms that might have or already had mass effect (Fig 2), fusiform aneurysms (Fig 3), blisterlike aneurysms (Fig 4), recurrent sidewall aneurysms, dissecting aneurysms (Fig 2), aneurysms at difficult angles to the parent artery (so that catheterization of the aneurysm and coiling may have increased risk) (Fig 5), and aneurysms in which a branch was originating directly from the sac (therefore endosaccular obliteration or clipping was likely to compromise the branch or result in a neck remnant) were treated with the PED (Figs 6 and 7). We intended to treat 1 patient with a giant, very wide-neck, cavernous ICA aneurysm presenting with mass effect symptoms by using a PED; however, we failed to bypass the neck of the aneurysm, resulting in treatment of the aneurysm with parent artery occlusion following a balloon occlusion test, without complications. This patient was not included in the study because a PED was not used. This was the only technical failure during the course of the series.
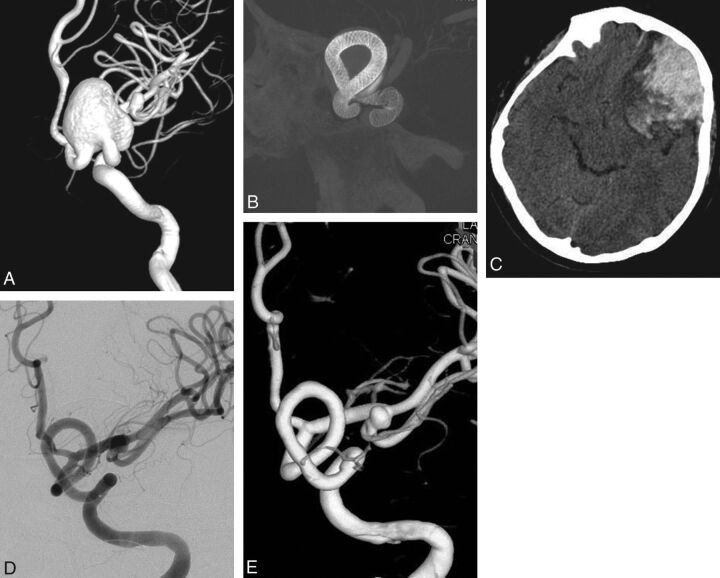
Fig 1.
Preoperative 3D angiogram (A) shows a very wide-neck large ICA aneurysm. It could be reconstructed with several overlapping devices, creating a new vessel wall within the sac as seen on the perioperative DynaCT image (B). Postoperative CT obtained the same evening (C) reveals ipsilateral frontal intraparenchymal hemorrhage. 2D (D) and 3D (E) views of 6-month control angiography demonstrate the reconstruction of the parent artery and total occlusion of the aneurysm.
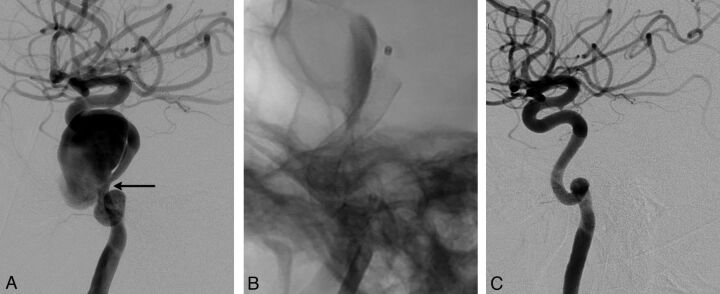
Fig 2.
Lateral angiogram shows a giant dissecting ICA aneurysm (A). The intraoperative view demonstrates PEDs (sizes, 4 × 202 and 4.5 × 16 mm) opening to the normal size of the parent artery at the dissected segment (arrow in A) without necessitating balloon angioplasty. Note the contrast stagnation within the sac (B). Six-month control angiography (C) shows total occlusion of the aneurysm and reconstruction of the parent artery.
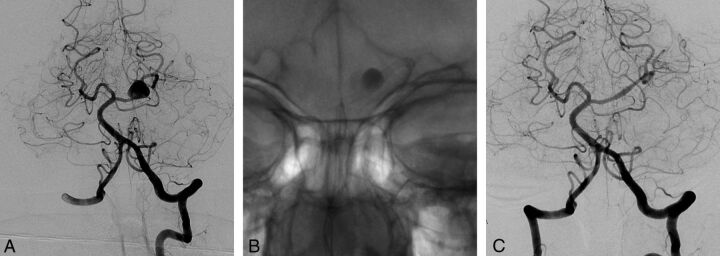
Fig 3.
Left vertebral angiogram (A) demonstrates the left PCA aneurysm, which presented with left thalamic infarct (not shown). Immediate postoperative view (B) shows the single PED (2.5 × 20 mm) placed in the left PCA, resulting in contrast stasis within the sac. Control angiography (C) after 6 months confirms total occlusion of the aneurysm with the PCA preserved.
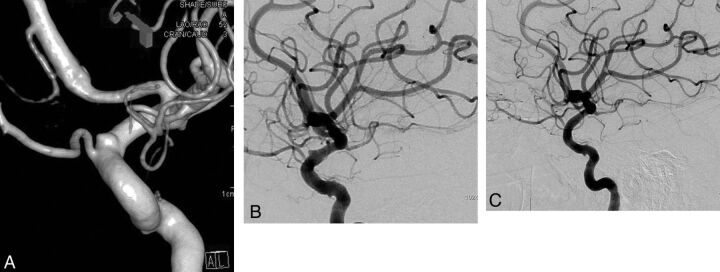
Fig 4.
3D image (A) and lateral angiography (B) show a left paraophthalmic bleb aneurysm in a patient who had a subarachnoid hemorrhage 3 months earlier. Lateral angiogram 6 months after placement of a single PED of 3.75 × 12 mm (C) demonstrates complete occlusion of the aneurysm.
Fig 5.
Right carotid angiogram (A) demonstrates a small carotid cave aneurysm in a patient who had an anterior communicating artery aneurysm previously treated with coiling following SAH. Six-month control angiography (B) shows occlusion of the aneurysm.
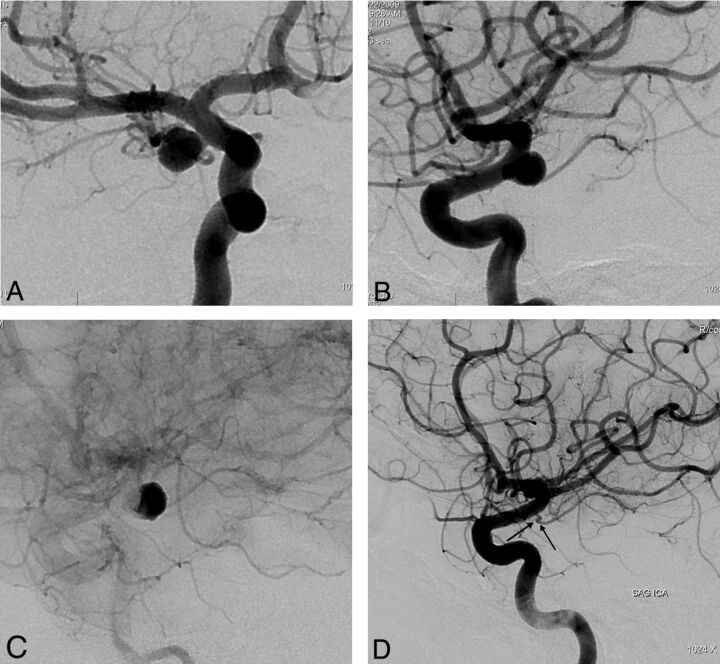
Fig 6.
Preoperative 2D (A and B) angiograms show the ICA aneurysm in which the anterior choroidal artery is originating from the aneurysm at the neck. A single PED is placed covering the neck, causing stagnation of the contrast within the sac (C). Six-month control angiography (D) demonstrates total occlusion of the aneurysm with the anterior choroidal artery preserved (arrow).
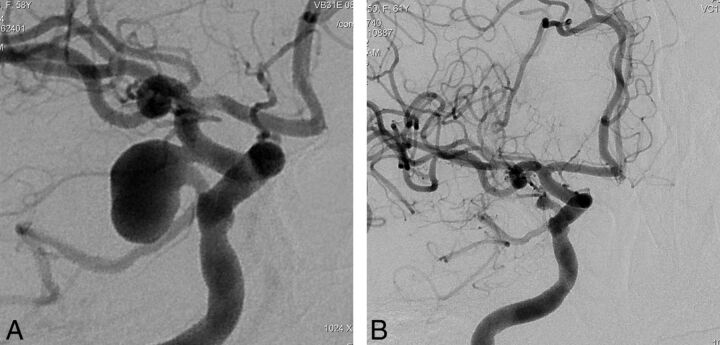
Fig 7.
Right internal carotid oblique angiogram (A) shows a right posterior communicating artery aneurysm (the ipsilateral P1 is aplastic and not shown) in a patient in whom previous endovascular attempts and clipping had failed, with surgical wrapping performed eventually. Two years after a single PED placement, the aneurysm is remodeled in the corresponding view (B).
The patients' initial clinical presentations are shown in Table 1. Twenty-eight patients had vision disturbances due to mass effect of the relevant aneurysm. One patient had a previous history of subarachnoid hemorrhage and had mass effect symptoms after recurrence of the aneurysm after receiving the PED as a retreatment. This patient is included in both groups (ie, the group of patients with previous hemorrhage and that of patients with visual findings due to mass effect) (Table 1). Among the 31 patients who had SAH due to the relevant aneurysm, 22 had PED as a retreatment. In the remaining 9 aneurysms, a PED was placed as the first treatment (Fig 4). Six patients were treated in the acute stage (at 8, 13, 14, 15, 15, and 20 days, respectively). Among them, coils were placed in addition to the PED in 1 patient.
Table 1:
Clinical presentations of the patients
| Presentation | No. of Patients | % |
|---|---|---|
| Incidentala | 23 | 12 |
| Headache | 83 | 43.5 |
| Subarachnoid hemorrhageb | 31c,d | 16.2 |
| Previous SAH from another aneurysm | 19 | 10 |
| Visual findings due to mass effect | 28d | 14.7 |
| Othere | 8 | 4.2 |
| Total | 191d | 100 |
Incidental group includes asymptomatic patients and patients with symptoms (excluding SAH) unrelated to the aneurysms treated with a PED (ie, index aneurysms).
SAH from the aneurysm treated with a PED.
Nine of these patients, 6 of whom were in the acute stage, were treated with the Pipeline as the first treatment; 22 patients had a PED in the retreatment.
One of these patients had visual findings after the initial treatment and received a PED as a retreatment; this patient is cited in both groups.
All symptoms (eg, ataxia, paresthesia, hemi-/quadriparesis, and so forth) other than those listed above, which may be due to mass effect and/or ischemia (such as perforator injury) and so forth.
Thirty-four aneurysms (34/251; 13.5%) in 32 patients (32/191; 16.8%) had PEDs as retreatment (Fig 6). Previous treatments are summarized in Table 2.
Table 2:
The previous treatments in the aneurysms that had Pipeline treatment for incomplete occlusion
| Previous Treatment | No. of Aneurysms/Patients |
|---|---|
| Coiling with bare coils | 18/17 |
| Coiling with surface modified coils | 2 |
| Stent-assisted coiling | 2 |
| Bare stenting | 2 |
| Onyx | 1 |
| Silk flow diverter | 2/1 |
| Failed surgery | 5 |
| Surgical remnant/regrowth | 2 |
| Total | 34/32 |
Thirty (12%) aneurysms were giant (>2.5 cm), 66 (26.3%) were large (25 mm ≥ aneurysm size ≥10 mm), and 155 (61.8%) were small (<10 mm). Two hundred twenty-three (88.8%) aneurysms were wide-neck (≥4 mm and/or dome-neck ratio ≤1.5), 21(8.4%) were fusiform, and only 7 (2.8%) had a narrow neck.
Distribution of the aneurysm locations is shown in Table 3. A majority, 232/251 (92.4%), of the aneurysms were located in the anterior circulation, with only 19 aneurysms (7.6%) seen in the posterior circulation (Fig 3).
Table 3:
Localizations of the aneurysms treated with PED
| Localization | No. of Aneurysms | Ratio (%) |
|---|---|---|
| Petrous ICA | 6 | 2.4 |
| Cavernous ICAa | 28 | 11.2 |
| Supraclinoid aneurysmb | 134 | 53.4 |
| PcomA aneurysms | 21 | 8.4 |
| AchoA aneurysms | 28 | 11.2 |
| ICA terminal bifurcation | 3 | 1.2 |
| M1 | 5 | 2 |
| MCA bifurcation | 2 | 0.8 |
| Basilar arteryc | 6 | 2.4 |
| Vertebral arteryd | 8 | 3.2 |
| Distal aneurysmse | 10 | 4 |
| Total | 251 | 100 |
Note:—AchoA indicates anterior choroidal artery.
If the aneurysm involved both petrous and cavernous segments, it is included in this group, and this definition applies to 12/28 aneurysms in this group.
The aneurysm is included in the supraclinoid group when it involves this segment, regardless of whether it extends to more than this segment proximally (eg, to the cavernous segment). The aneurysms at the posterior communicating and anterior choroidal artery origins and the terminal bifurcation are shown separately and are not included in this group.
This group includes 1 superior cerebellar artery origin aneurysm and 2 aneurysms involving the vertebrobasilar junction in addition to 3 basilar trunk aneurysms.
Three aneurysms at the origin of PICA are included in this group.
This group includes all aneurysms distal to the MCA bifurcation, all anterior cerebral artery aneurysms excluding the ones located at the ICA termination, and any aneurysm distal to basilar termination (ie, posterior cerebral artery aneurysms).
Treatment and Medication
All patients, including those treated during the acute period of SAH, were premedicated with a loading dose of 300–600 mg of clopidogrel (based on the duration of the premedication; the shorter the premedication period, the higher the loading dose), followed by 75 mg daily; additionally, all patients received 300 mg of aspirin daily. Thrombocyte inhibition levels were confirmed by using the VerifyNow P12Y12 assay (Accumetrics, San Diego, California) and a standard thrombocyte aggregation test. The patient was treated only if the thrombocyte inhibition level was above 30%. If the response was lower and without resistance, additional loading doses or increased daily doses (eg, 150 mg daily) were administered. If clopidogrel resistance was detected, clopidogrel was discontinued and ticlopidine was administered with a dose of 600 mg twice daily as occurred in 24 patients. In all patients, intravenous heparin was administered during the treatments to maintain an activated clotting time of 250–300 seconds (2–2.5 times the baseline value). Heparinization was not reversed at the conclusion of the procedure unless the platelet inhibition level exceeded 70%. All patients who had large or giant aneurysms received dexamethasone, with an initial dose of 8 mg given during the procedure and continued 4 times; 4 mg daily afterward, at least for 1 week of full dose up to 2 weeks; then, the dose was tapered within a similar period. A clopidogrel regimen of 75 mg or ticlopidine, 600 mg twice daily, in addition to ASA, 300 mg per day (or ASA 100 mg, if side effects were noted, eg, ecchymosis and so forth), was maintained after the treatment until the first control angiography at 6 months; then, clopidogrel (or ticlopidine) was discontinued while ASA was continued as a life-long regimen.
All treatments were performed with the patient under general anesthesia by using biplane angiography units. 3D rotational angiography was performed in all patients, and working projections were determined. Parent artery measurements were obtained with the utmost precision by using 3D reconstructions and 2D working projections, not only with automatic calibration but also with reference to microcatheter/guiding catheter size.
In all patients, a 6F introducer sheath (Super Arrow-Flex Percutaneous Sheath Introducer set; Teleflex, Limerick, Pennsylvania or Pinnacle Destination; Terumo, Tokyo, Japan) was placed proximally in the parent artery (ie, the common carotid or subclavian artery), and then, a 6F guiding catheter (Envoy; Cordis Neurovascular, Miami Lakes, Florida or Fargo and Fargomax; Balt, Montmorency, France or Neuron; Penumbra, Alameda, California) was placed in the internal carotid or vertebral artery as distal as possible. The microcatheter of 0.027 inches in diameter (Rebar 27, Marksman; Covidien-ev3) was then navigated over different microguidewires as necessary. The microcatheter tip was placed distal enough so that while one manipulated the PED, the tip of the delivery wire would not be pushed beyond the tip of the microcatheter, but the microcatheter could be retrieved while stabilizing the wire. In a few exceptional cases where the neck of the large/giant aneurysm was very wide and could not be primarily bypassed with the designated microcatheter, the “HyperForm-loop technique,” as described previously,25 was used.
The PED was deployed across the targeted landing zone through a process of repeating maneuvers, including microcatheter unsheathing, delivery-wire stabilization/advancement, and microcatheter loading. After the device was placed with full release, the microcatheter was advanced over the delivery wire until the capture coil marker was captured. The device apposition to the artery wall, both proximally and distally, was of extreme importance to avoid “unbalanced” flow into the sac (ie, the outflow being more restricted than the inflow), which may possibly increase the risk of aneurysm rupture. DynaCT angiography (Siemens, Erlangen, Germany) was performed when necessary to evaluate the device opening and apposition to the parent artery wall. In most cases, a single device was placed. Additional devices were deemed necessary when the device apposition distally and/or proximally was not favorable, if the aneurysm neck was not covered completely, if there was a 360° involvement of the parent artery wall, and if the flow into the aneurysm remained unchanged. Although the latter was not an absolute indication for multiple-device placement, it was taken into consideration, especially when the aneurysm was large or giant. When the aneurysm was small, a single device was considered sufficient. We tried to avoid covering a critical branch, such as the anterior choroidal artery, perforators, and so forth, with >1 device.
In 11 aneurysms, 6 of which were giant, 4 were large, and only 1 was small, coils were used adjunctively in the same session with the PED placement. In 1 giant fusiform vertebrobasilar junction aneurysm, coils were used primarily to occlude the contralateral vertebral artery flow. Two large aneurysms had nipples. Adjunctive coils were used in addition to PED placement when there was very high jet flow into the sac of a large/giant aneurysm with a relatively narrow neck (high aspect ratio) and the neck was located next to a sharp angle. However, there were no objective criteria with proved value for adjunctive coiling indications, to our knowledge. In the only small aneurysm within this group, coils were used adjunctively because this particular aneurysm was treated in the acute stage of subarachnoid hemorrhage. Additionally, in the group of patients who had Pipeline placement as the retreatment (Table 2), 20 other aneurysms (in 19 patients) had coils from the previous treatments. Moreover, there were self-expandable stents at the aneurysm neck in 4 patients, 2 of whom had additional coils within the sac from the previous treatment. Overall, 34 aneurysms had additional endosaccular material (coils; Onyx, ev3) either placed adjunctively in the current PED treatment (11 aneurysms) or from the previous treatments (23 aneurysms). In 1 patient, there was a previously placed Silk flow diverter (Balt) covering 2 aneurysms.
Follow-Up
A 3-month clinical control and a CT or MR angiography control were obtained, if a patient had ongoing headache, large/giant aneurysms with mass effect symptoms, or a previous history of SAH and so forth. All patients were designated to have a clinical control and DSA at 6 months. If the 6-month control angiography revealed incomplete occlusion of the aneurysm or any intimal change within the device, an additional control DSA was performed during the 12th month. All patients were scheduled for an 18- or 24-month control DSA accordingly (ie, 1 year after the previous angiography). Clopidogrel and ticlopidine were discontinued after the 6-month control DSA, with ASA continuing life-long, unless there was any intimal hyperplasia. If so, then dual antiplatelet medication was maintained for a minimum of another 6 months until the next control DSA.
Results
In 191 patients, 251 aneurysms were successfully treated with a total of 324 PEDs. Only 1 PED was used in 128 aneurysms, while in 120 patients, a single device was used to treat ≥1 aneurysm. One PED treated 2 aneurysms in 19 patients and 3 aneurysms in 3 instances. The mean number of devices per patient was 1.7, and that per aneurysm was 1.3.
Complications are summarized in Table 4. The overall adverse event rate was 27/191 (14.1%) with a permanent morbidity of 2/191 (1%) and mortality of 1/191 (0.5%).
Table 4:
Any clinical events during/immediately after or in the follow-up period
| Adverse Events | No. of Patients | Permanent Morbidity/Mortality |
|---|---|---|
| Due to medication | ||
| Intracranial hemorrhage | 2 | 1 |
| Aplastic anemiaa | 1 | No |
| Hematuria (requiring change in medical treatment) | 1 | No |
| GI bleeding (including the FU period) | 2 | No |
| Associated with intervention | ||
| Deep vein thrombosis | 1 | No |
| Retroperitoneal hematomab | 3 | No |
| Associated with aneurysm treatment | ||
| Due to mass effectc | 4 | 1 |
| SAH (aneurysm rupture) | 1 | Nod |
| In relation to PED | ||
| Perioperative thromboembolic event | 4 | 1) Mortality (jailed PCA occlusion) |
| 3) Symptoms resolved totallye | ||
| In-stent stenosisf | 8 | No |
| Mild | 5 No intervention | |
| Severe | 3 PTAs performedg | |
| Ischemic event in the FU period | 1e | |
| Total | 27 (14.1%)e | 2 (1%)/1 (0.5%) |
Note:—FU indicates follow-up; GI, gastrointestinal; PTA, percutaneous transarterial angioplasty.
Occurred in the patient who had resistance to clopidogrel and was on ticlopidine.
Included in the group of complications that are attributed to intervention, but antithrombocytic medication may also have contributed.
Any new symptom or increase in the findings are taken into consideration; 3 had deteriorating vision loss, of whom 2 also had visual field defects. In 2 patients, the symptoms regressed to their preoperative degree in the follow-up and caused permanent additional morbidity in 1. The remaining patient had symptoms due to mass effect on the brain stem, aggravated after the treatment, but resolved in 4 weeks' time.
This patient had subarachnoid hemorrhage 4 months after the treatment; imaging still showed filling of the aneurysm despite significant decrease. Initially she had had hemiparesis, but this resolved totally.
One patient had an ischemic attack in the postoperative 4 months after he discontinued clopidogrel without consulting his doctor. The patient was medicated with IV heparin, and clopidogrel was loaded again. The symptom of monoparesis resolved totally. The same patient woke up from the general anesthesia with monoparesis but immediately became asymptomatic after volume loading and raising the blood pressure.
Mild refers to any intimal thickening causing stenosis <50%. Severe refers to stenosis ≥50%.
In 2 patients, stenosis was discovered in the control angiography but PTA was performed because the stenosis was considered significant (>70%). The remaining patient had attacks of dysphasia which resolved after PTA, with no permanent morbidity.
One patient died due to thrombus formation in the right P1, resulting in brain stem infarct after placement of the PED extending from the left posterior cerebral artery to the basilar artery, jailing the right P1, to treat a wide-neck left superior cerebellar artery origin aneurysm.
Two patients developed ipsilateral remote intraparenchymal hematomas. The first patient's hematoma developed within the first 8 hours after treatment (Fig 1). This hematoma was attributed to overmedication. The patient was placed on subcutaneous low-molecular-weight heparin despite her very high response to clopidogrel (the VerifyNow level was 97%) because the artery was reconstructed by using 16 devices overlapping in a telescopic fashion and we were worried about thromboembolic complications due to metal overload. The patient did not have any permanent neurologic sequelae from this event and was discharged home after 1 week. Control angiography showed total obliteration of the aneurysm with the parent artery reconstruction.
The second patient, a woman with a small distal anterior cerebral artery aneurysm, was noted to have a hematoma 4 weeks posttreatment. The patient was admitted to the hospital with a GCS score of 11, and a control angiography showed total occlusion of the aneurysm with a VerifyNow level at admission of 98%. Clopidogrel was discontinued, and a craniectomy was performed to relieve the increased intracranial pressure on day 5. Her initial right hemiplegia and dysphasia improved during her stay of 2 months in the hospital, and she was discharged to a rehabilitation center, being able to walk. She improved clinically after the rehabilitation, and in the fourth month, she had a modified Rankin Scale score of 3, with remaining mild dysphasia and mild paresis on the left but was able to walk independently and use the upper extremities.
In this series, 1 patient had subarachnoid hemorrhage from the treated aneurysm, which happened within the fourth month after PED placement. The control CTA at 3 months had shown significant decrease in the filling of the aneurysm sac, but the aneurysm was not completely obliterated. The patient was admitted to another hospital with a GCS score of 13. Clopidogrel and aspirin were discontinued immediately on admission. The patient recovered well with no neurologic deficit and was transferred to our center. Following premedication, she was taken for retreatment where the diagnostic angiography showed some contrast filling at the neck region. Two additional PEDs were placed with no adverse events. The 6-month control angiography (according to the initial therapy) showed complete occlusion of the aneurysm.
One patient had dysphasia 8 weeks postoperatively after the treatment of a left supraclinoid large ICA aneurysm with 3 PEDs. MR imaging showed an acute ischemic lesion in the Broca area, and the patient was emergently taken for angiography where significant stenosis of the left ICA at the edge of the PED and within the devices was noted. Balloon angioplasty was successful, and good antegrade flow was restored. This patient currently has undergone several control angiographies during 2 years and remains on clopidogrel with no symptoms.
Twenty-eight patients presented with a vision abnormality attributed to mass effect (Fig 2). Three patients worsened immediately following treatment. Two of these 3 regressed to their preoperative presentations during follow-up; therefore, 2 patients did not receive any benefit from treatment. The remaining patient had permanent additional morbidity. The aneurysms of these 3 patients were completely occluded in the control angiographies. Seventeen patients had total recovery of symptoms, and an additional 8 patients improved during follow-up, though the symptoms did not resolve completely.
At least 1 control angiography was performed in 182 of the patients (95.3%) with 239 (95.2%) aneurysms. Eight patients with 11 aneurysms had the first DSA control of 6 months pending; and among them, at least 6 months passed since the treatment in 4 patients with 6 aneurysms. One patient died after treatment and did not have a control angiography. According to the latest control, 118 aneurysms (47%) of 95 patients (49.7%) had undergone a 6-month angiography; 52 aneurysms (20.7%) of 38 patients (19.9%) had 1-year and 69 aneurysms (27.5%) of 49 patients (25.7%) had 18-month or 2-year control angiographies.
This series included 46 aneurysms (Figs 6 and 7) in which a branch originated directly from the sac where endosaccular coiling or clipping at the neck would result in incomplete occlusion and/or compromise of the branch. Fusiform aneurysms, which involved perforating branches such as aneurysms of the basilar artery, distal vertebral artery, and the M1 segment of the middle cerebral artery, were not included in this group. This group is the subject of another study and will be analyzed there in detail. However, this group of aneurysms prompted us to find a new definition (ie, “remodeled artery”), which refers to an “infundibulum-like” appearance or a tortuous course of the branch resulting from the significant shrinkage of the aneurysm due to flow change (Fig 7). Sectional imaging confirmed the resolution of the sac in these patients with such large/giant aneurysms. In this subgroup of aneurysms, 42 of 46 aneurysms had at least 1 control angiography at 6 months. Among these 42 aneurysms, 8 showed a so-called “remodelling” pattern (Fig 7).
The 6-month control angiography results, according to the aneurysm size, are given in Table 5. These include 1 patient who had a retreatment after bleeding in the fourth month; 219/239 aneurysms were occluded for a total occlusion rate of 91.6%. With the exception of 1, all other aneurysms that did not show complete obliteration at the 6-month control angiography (20/239) decreased in size in the first control angiography; in these cases, follow-up angiography was scheduled after an interval of 6 months following discontinuation of the clopidogrel/ticlopidine. Among these 20 aneurysms, 7 showed further thrombosis and became completely occluded. Six are still pending the second control after discontinuation of the clopidogrel. The remaining 7 were retreated with additional PED placement; only 1 has undergone control angiography after retreatment so far and that showed complete obliteration. In the entire series, a total of 8 aneurysms were retreated, 1 on bleeding (retreatment rate, 3.2% among the aneurysms and 4.2% in the patient group). In this subgroup, there were 1 giant, 3 large, and 4 small aneurysms. Two (1 was before and the other was after the 6-month control angiography) have had control angiographies so far, and both have shown total occlusion. When we analyzed the 6-month control results according to the aneurysm size, small aneurysms had a very high total obliteration rate of 136/145 (93.8%), whereas complete obliteration occurred in 56/64 (87.5%) of the large and 27/30 (90%) of the giant aneurysms. According to the last control angiography, 227/239 (95%) aneurysms were totally obliterated, including the 2 aneurysms with retreatment. Total occlusion without retreatment was 94.6% in this series.
Table 5:
Six-month control angiography results in regard to aneurysm sizea
| Degree of Occlusion | Small | Large | Giant | Total No. | % |
|---|---|---|---|---|---|
| Total occlusion (%) | 136 (93.8%) | 56 (87.5%) | 27 (90%) | 219b | 91.6b–91.2c |
| Still filling | 9 | 8 | 3 | 20d | 8.4% |
| Total | 145 | 64 | 30 | 239a | 100 |
One patient with 1 aneurysm died after the treatment; 8 patients with 11 aneurysms (9 small and 2 large) have not yet undergone the 6-month control angiography. Therefore, a total of 12 aneurysms (4.8%) did not have control angiography.
Including 1 patient who had subarachnoid hemorrhage in the fourth month and was retreated with additional PEDs for her remaining aneurysm filling.
Represents the ratio of aneurysms that were occluded in the 6-month control without retreatment.
Seven were retreated. Seven of the remaining showed further thrombosis with resultant aneurysm occlusion, and 6 are pending the next control after the discontinuation of the clopidogrel.
Discussion
Endosaccular coiling has become an accepted treatment for cerebral aneurysms. However, the higher aneurysm recurrence after coiling than after clipping, which may result in an increased risk of rebleeding in the former group, is still a concern and causes a higher retreatment rate.10,26,27 Therefore, not only the stable occlusion of the treated aneurysm but also more durable retreatment methods afterward are being investigated. Involvement of the parent artery with the aneurysm wall to a higher degree apparently results in aneurysm recurrence more frequently. Because of this, a treatment targeting the diseased parent artery wall rather than sole occlusion of the sac is likely to be more effective. Methods reinforcing the parent artery wall, such as by using the liquid embolic Onyx28,29 or stent placement30–32 with or without endosaccular obliteration, have been used in the treatment of aneurysms that were more likely to recur. Excluding the treatment with covered stents,33 the first apparent evidence of long-term stability of parent artery reconstruction was noted in the treatment of large/giant aneurysms with the liquid embolic Onyx in conjunction with stents32; however, this technique had its own limitations.28,29
Alteration of flow quantity and direction has been a method for the treatment of some selected aneurysms. Previously it was limited to placement of a single or multiple stents or parent artery occlusion until the development of dedicated flow diverters (Pipeline and Silk). The results of previous PED studies are summarized in Table 6.20,21,23,24,34 In our series, the angiographic occlusion rates of 91.2% at 6 months and 94.6% at up to 24 months (without retreatment) were comparable with those in the previous PED series, and our results confirmed the superiority of the PED treatment over conventional endosaccular techniques in regard to its efficacy.7,10
Table 6:
Summary of previous Pipeline series in comparison with this series
| Series | No. of Patients/AA | No of AA W Previous TX Failurea (%) | No of AA Treated W Adjunctive Coilingb (%) | Morbidityc and Mortality | Complete Occlusion at 6-Month DSA (%) | Control Angiography (%) | Retx No of AA (%) | Peri-Post-Operative Intracranial Bleeding | Perforator Infarct | In-Stent Stenosis All %/Requiring TX % PAO |
|---|---|---|---|---|---|---|---|---|---|---|
| Lylyk et al 200920,d | 53/63 | 23/63 | 4/63 (6%) | 0 | 93% | 100% | 0 | 0 | 0 | 10%/0 |
| (37%) | 0% | PAO: 0 | ||||||||
| Szikora et al 201021,e | 18/19 | 1/19 | 10/19 (53%) | 5.6% | 94.4% | 94.7% | 0 | 1/18f | 0 | 0 |
| (5.3%) | 5.6% | 5.6% | PAO:5.6% | |||||||
| Nelson et al 201123 | 31/31 | 12/31 | 16/31 (52%) | 6.5% | 93.3% | 96.8% | 0 | 1/31g | 1/31 | 0 |
| (38.7%) | 0% | 3.2% | (3.2%) | PAO:0 | ||||||
| Fischer et al 201124 | 88/101 | 30/101) | 3/101 (3%) | 4% | 52% | 89% | 8/101 | 4/88h | 0 | 2.3%/0 |
| (29.7%) | 2% | 7.9% | 4.6% | PAO:2.3% | ||||||
| McAuliffe et al 201234 | 54/57 | 16/57 | 12/68 (18%) | 0 | 85.7% | 98.2% | 2/57i | 0 | 0 | 3.5%/0 |
| (28.1%) | 0% | 3.5% | PAO:0 | |||||||
| Saatci et al 2012 | 191/251 | 34/251 | 11/251 (4%) | 1% | 91.2 % | 95.2 % | 8/251 | 3/191j | 1/191 | 4.2%/1.6% |
| (13.5%) | 0.5% | 3.2% | 1.6% | 0.5% | PAO:0 |
Note:—AA indicates aneurysms; TX, treatment; W, with DSA; Retx retreatment.
Refers to the aneurysms that underwent previous endovascular or surgical treatment, including the failed treatment, incomplete treatment, and recurrences.
Refers to the aneurysms in which coiling was performed as an adjunctive treatment in the same session with PED placement.
Temporary deficits not included.
Six (d) and 9 (e) aneurysms of these series were also included in the PITA trial.
Refers to the rupture of a coexisting aneurysm.
Refers to an iatrogenic ICA rupture.
Includes 1 aneurysm rupture and 3 parenchymal hemorrhages.
Additional treatment required due to PED displacement in 2 aneurysms.
Includes 1 aneurysm rupture and 2 parenchymal hemorrhages.
There have been a few series reporting the results of Silk, another flow-diverter device for the treatment of cerebral aneurysms.22,35–37 Byrne et al22 reported the results in 70 aneurysms, the data of which were collected retrospectively as a multicenter registry (our institution also included cases in that registry). In that study, complete occlusion was 49% in the follow-up at a mean of 4 months. Berge et al37 reported a complete occlusion rate of 68% in 6 months, increasing to 84.5% in a year, with a permanent morbidity of 7.8% and mortality of 3% in a retrospective multicenter study.
Being technically “simple” or straightforward when there is sufficient collateral flow, PAO is another option for the treatment of large/giant ICA aneurysms, particularly when these present with mass effect.38 However, the stability and effectiveness of PAO may not be absolute for the treatment of large/giant ICA aneurysms; the aneurysms may still remain patent6,39 or may even bleed in the follow-up after PAO40,41 and mass effect symptoms may persist.39,42 Moreover, due to flow change, de novo aneurysms may develop or existing aneurysms may enlarge after PAO.39,43,44
More important, the PED is providing a solution for aneurysms that have a branch incorporated into the sac. These aneurysms are generally considered “uncoilable” in the endovascular approach, though there have been a few publications reporting the contrary.45,46 On the other hand, in such aneurysms, the flow through the flow diverters is maintained into the branch originating from the sac while occlusion of the aneurysm is still possible. Our series included 46 aneurysms in which a branch was originating from the sac. In none of these aneurysms was the relevant branch occluded, except for 5 PcomA aneurysms in which the PcomAs were occluded, with the ipsilateral PCA filling from the posterior circulation. On the basis of our experience in this group, we observed that the branch originating from the aneurysm sac, which is treated with a flow diverter, is kept patent when there is a flow demand through it. However, only 1 device was placed to cover the sac and the originating branch in this particular subgroup of our series. Therefore, the possible consequences of multiple-device coverage are indeterminate. Regarding this subgroup, we noted a particular appearance in some aneurysms, in which the aneurysm shrunk significantly, resulting in an “infundibula like” appearance at its origin or a tortuous takeoff from the parent artery in place of the initial aneurysm. For the purpose of definition, these are referred to as “remodeled aneurysms.” The detailed results of this subgroup of aneurysms are the subject of another article.
The peri- and postprocedural complications of endovascular aneurysm treatment with flow diverters include mainly hemorrhagic events, thromboembolic events, and mass effect symptoms, persisting or worsening after treatment. Hemorrhagic events may occur due to the double antiplatelet regimen, which is an inherent part of the treatment and should be continued for some time (eg, at least 6 months in our practice); due to manipulations during the intervention; and due to aneurysm rupture. Recently, early and delayed aneurysm ruptures following treatment with flow diverters, Silk or PED, have been reported in the literature.47–50 The underlying mechanism may be 1 of the following: changes in the wall shear stress at the aneurysm dome,51 unfavorable hemodynamic change (ie, outflow restricted more than the inflow),49 and autolysis of the aneurysm wall secondary to red thrombus formation with accompanying inflammation.48 Although the definite causes of the aneurysm rupture are not yet proved, Kulcsar et al47 suggested aggressive aneurysm thrombosis resulting in autolysis of the aneurysm wall as the cause of the delayed aneurysm rupture following flow-diverter treatment in their review of 13 aneurysms (all being ≥15 mm) ruptured after Silk flow-diverter placement. Ten of 13 aneurysms ruptured within 2–48 days (mean, 16 days) after the treatment; however, 3/13 aneurysms also showed rupture in the late phase (3–5 months). Of these 13 aneurysms, 11 were intradural, resulting in death in 9 patients and disabling morbidity in 1. In our series, we have encountered 1 delayed aneurysm rupture (1/191; 0.5%) that occurred in the fourth month after the PED treatment, and the patient survived with no permanent neurologic deficit. Even if the large and giant aneurysms are taken into account, on the basis of the fact that almost all (if not exclusively) ruptured aneurysms reported in the literature are large or giant, in this subgroup, the rate of bleeding becomes 1/96 (1%) in our series.
Adjuvant aneurysm filling with coils may be considered to prevent aneurysm rupture; however, there have been ruptured cases despite additional coiling. Moreover, to our knowledge, there is no criterion to define the degree of coil packing sufficient to spare the aneurysm from rupture. In our series, adjunctive coiling has been performed in only 4.4% of the aneurysms. If the 9 large/giant aneurysms in which sac coiling was performed adjunctively were excluded from the cohort, the bleeding rate becomes 1.2%.
Differing from many other series, corticosteroid treatment is mandatory in our practice if the aneurysm is large or giant, to suppress the inflammatory reaction that may be caused by the thrombosis of the sac. Moreover, the platelet response to dual premedication is always investigated to provide an optimal level of at least 30% platelet inhibition. We question whether the medication protocol may play a role in the progression of thrombosis and accompanying inflammatory reaction when present. This assumption does not progress beyond the level of hypothesis due to a lack of evidence. Regarding the other case series of PEDs, Fischer et al24 reported 1 aneurysm rupture among 88 patients (1.1%). In the other PED series with follow-up,20,21,23,34 there was no index aneurysm rupture (Table 6). The premedication with double antiplatelets was variable and corticosteroid administration was not determinate in these series.
Parenchymal hemorrhage was another complication reported following the flow-diverter treatment, with possible causes including wire perforation, aneurysm rupture, antiplatelet medication, hemorrhage within ischemic tissue, and so forth. We encountered parenchymal hemorrhage in 2 patients in our series (2/191; 1.1%). In both patients, the platelet inhibition level was high (≥97%), and one of the patients (Fig 1) received subcutaneous low-molecular-weight heparin after the treatment, experiencing parenchymal hemorrhage in the same evening following the administration of the drug. In the second patient with parenchymal hemorrhage, the hematoma was remote from the catheterized artery and occurred many days after the treatment, making wire perforation a less likely cause. In our evaluation, we attributed the parenchymal hemorrhages to a high response to antiplatelet medication with or without accompanying anticoagulation. Fischer et al24 also reported 3 parenchymal hemorrhages (3/88; 3.4%), suggesting microemboli and microinfarcts as the triggers.
Thromboembolic events may occur during the treatment, in the early follow-up, and also in the late phase.21,23,24,34,52–55 Possible causes include the following: 1) insufficient antiplatelet activity (low response or resistance, unauthorized drug discontinuation, and so forth), 2) the device not opening properly (ie, incomplete opening or poor apposition to vessel wall), 3) compromise of covered branches, and 4) in-stent stenosis and so forth. In our series, 1 patient died from the consequences of P1 thrombosis after the posterior cerebral artery was jailed by 1 PED, despite additional thrombolytic and platelet glycoprotein IIb-IIIa inhibitor drug administration. Apart from this event, there was no perforator infarct in this series. Parent artery occlusion was reported more frequently in Silk series22,37 than in PED series.21,24 Among the PED experience, there was a basilar fusiform aneurysm treated with PED resulting in PAO after 2 years, despite dual antiplatelet therapy continued for 18 months, as reported by Fiorella et al.53 There is no consensus regarding the duration of antiplatelet medication. In our practice, 6 months is the minimum time of dual antiplatelet administration. However, there is no controlled study to clarify this issue, to our knowledge.
In-stent stenosis may occur occasionally with many, if not all, of the devices currently in use.56,57 It has also been reported with flow diverters up to 33%.20,22,24,34,35 In our series, in-construct intimal hyperplasia was noted in 8/191 patients (4.2%). However, only 1 patient (0.5%) had clinical symptoms, which resolved totally following the percutaneous transarterial angioplasty, and the patient remained stable with clopidogrel not interrupted in the 30 months of follow-up.
Last, this series consisted of long-term evaluation data so that nearly half of the patients (87/191: 45.6%) had at least 1 year and up to 34 months of clinical follow-up and up to 2 years of DSA control with no unfavorable clinical event or deteriorating angiographic findings. This outcome supports the device safety.
Conclusions
PED provides a solution for wide-neck, large/giant, fusiform aneurysms; too small aneurysms; and also small-but-difficult-to-coil aneurysms such as the ones from which a branch is originating. Our series confirmed the safety of this technique with low morbidity-mortality as well as its efficacy with high angiographic complete occlusion rates and long-term durability.
ABBREVIATIONS:
- ASA
acetyl salicylic acid
- GCS
Glasgow Coma Scale
- PAO
parent artery occlusion
- PcomA
posterior communicating artery
- PED
Pipeline Embolization Device
Footnotes
Disclosures: Isil Saatci—UNRELATED: Consultancy: consulting agreement with ev3, Payment for Lectures (including service on Speakers Bureaus): (clarify), Payment for Development of Educational Presentations: honorium for meetings and preparation of videos or demo materials for training of PED devices. Saruhan Cekirge—UNRELATED: Consultancy: consulting agreement with ev3; Payment for Lectures (including service on Speakers Bureaus): honorium for lectures in scientific meetings. Payment for Development of Educational Presentations: honorium for meetings and preparation of videos or demo materials for training of PED devices. Other: consulting agreement with MicroVention.
References
- 1. Molyneux A, Kerr R, Stratton I, et al. , for the International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 2002; 360: 1267– 74 [DOI] [PubMed] [Google Scholar]
- 2. McDougall CG, Spetzler RF, Zabramski JM, et al. The Barrow Ruptured Aneurysm Trial. J Neurosurg 2012; 116: 135– 44 [DOI] [PubMed] [Google Scholar]
- 3. Lylyk P, Ferrario A, Pasbon B, et al. Buenos Aires experience with the Neuroform self-expanding stent for the treatment of intracranial aneurysms. J Neurosurg 2005; 102: 235– 41 [DOI] [PubMed] [Google Scholar]
- 4. Jahromi BS, Mocco J, Bang JA, et al. Clinical and angiographic outcome after endovascular management of giant intracranial aneurysms. Neurosurgery 2008; 63: 662– 74, discussion 674–75 [DOI] [PubMed] [Google Scholar]
- 5. Mocco J, Snyder KV, Albuquerque FC, et al. Treatment of intracranial aneurysms with the Enterprise stent: a multicenter registry. J Neurosurg 2009; 110: 35– 39 [DOI] [PubMed] [Google Scholar]
- 6. Elhammady MS, Wolfe SQ, Farhat H, et al. Carotid artery sacrifice for unclippable and uncoilable aneurysms: endovascular occlusion versus common carotid artery ligation. Neurosurgery 2010; 67: 1431– 36, discussion 1437. [DOI] [PubMed] [Google Scholar]
- 7. Raymond J, Guilbert F, Weill A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke 2003; 34: 1398– 403 [DOI] [PubMed] [Google Scholar]
- 8. Campi A, Ramzi N, Molyneux AJ, et al. Retreatment of ruptured cerebral aneurysms in patients randomized by coiling or clipping in the International Subarachnoid Aneurysm Trial (ISAT). Stroke 2007; 38: 1538– 44 [DOI] [PubMed] [Google Scholar]
- 9. Henkes H, Fischer S, Liebig T, et al. Repeated endovascular coil occlusion in 350 of 2759 intracranial aneurysms: safety and effectiveness aspects. Neurosurgery 2008; 62 (6 suppl 3): 1532– 37 [DOI] [PubMed] [Google Scholar]
- 10. Ferns SP, Sprengers ME, van Rooij WJ, et al. Coiling of intracranial aneurysms: a systematic review on initial occlusion and reopening and retreatment rates. Stroke 2009; 40: e523– 29 [DOI] [PubMed] [Google Scholar]
- 11. Doerfler A, Wanke I, Egelhof T, et al. Double-stent method: therapeutic alternative for small wide-necked aneurysm: technical note. J Neurosurg 2004; 100: 150– 54 [DOI] [PubMed] [Google Scholar]
- 12. Cantón G, Levy DI, Lasheras JC, et al. Flow changes caused by the sequential placement of stents across the neck of sidewall cerebral aneurysms. J Neurosurg 2005; 103: 891– 902 [DOI] [PubMed] [Google Scholar]
- 13. Zenteno MA, Santos-Franco JA, Freitas-Modenesi JM, et al. Use of the sole stenting technique for the management of aneurysms in the posterior circulation in a prospective series of 20 patients. J Neurosurg 2008; 108: 1104– 18 [DOI] [PubMed] [Google Scholar]
- 14. Park SI, Kim BM, Kim DI, et al. Clinical and angiographic follow-up of stent-only therapy for acute intracranial vertebrobasilar dissecting aneurysms. AJNR Am J Neuroradiol 2009; 30: 1351– 56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sadasivan C, Cesar L, Seong J, et al. An original flow diversion device for the treatment of intracranial aneurysms: evaluation in the rabbit elastase-induced model. Stroke 2009; 40: 952– 58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dorn F, Niedermeyer F, Balasso A, et al. The effect of stents on intra-aneurysmal hemodynamics: in vitro evaluation of a pulsatile sidewall aneurysm using laser Doppler anemometry. Neuroradiology 2011; 53: 267– 72 [DOI] [PubMed] [Google Scholar]
- 17. Kallmes DF, Ding YH, Dai D, et al. A new endoluminal, flow-disrupting device for treatment of saccular aneurysms. Stroke 2007; 38: 2346– 52 [DOI] [PubMed] [Google Scholar]
- 18. Fiorella D, Woo HH, Albuquerque FC, et al. Definitive reconstruction of circumferential, fusiform intracranial aneurysms with the Pipeline embolization device. Neurosurgery 2008; 62: 1115– 21, discussion 1120-21 [DOI] [PubMed] [Google Scholar]
- 19. Kulcsár Z, Wetzel SG, Augsburger L, et al. Effect of flow diversion treatment on very small ruptured aneurysms. Neurosurgery 2010; 67: 789– 93 [DOI] [PubMed] [Google Scholar]
- 20. Lylyk P, Miranda C, Ceratto R, et al. Curative endovascular reconstruction of cerebral aneurysms with the Pipeline embolization device: The Buenos Aires experience. Neurosurgery 2009; 64: 632– 43 [DOI] [PubMed] [Google Scholar]
- 21. Szikora I, Berentei Z, Kulcsar Z, et al. Treatment of intracranial aneurysms by functional reconstruction of the parent artery: The Budapest experience with the Pipeline embolization device. AJNR Am J Neuroradiol 2010; 31: 1139– 47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Byrne JV, Beltechi R, Yarnold JA, et al. Early experience in the treatment of intra-cranial aneurysms by endovascular flow diversion: a multicentre prospective study. PLoS One 2010; 5: pii: e12492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nelson PK, Lylyk P, Szikora I, et al. The Pipeline embolization device for the intracranial treatment of aneurysms trial. AJNR Am J Neuroradiol 2011; 32: 34– 40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fischer S, Vajda Z, Aguilar Perez M, et al. Pipeline embolization device (PED) for neurovascular reconstruction: initial experience in the treatment of 101 intracranial aneurysms and dissections. Neuroradiology 2011; 54: 369– 82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cekirge SH, Yavuz K, Geyik S, et al. HyperForm balloon-assisted endovascular neck bypass technique to perform balloon or stent-assisted treatment of cerebral aneurysms. AJNR Am J Neuroradiol 2007; 28: 1388– 90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Molyneux AJ, Kerr RSC, Birks J, et al. Risk of recurrent subarachnoid hemorrhage, death, or dependence and standardised mortality ratios after clipping or coiling of an intracranial aneurysm in the International Subarachnoid Aneurysm Trial (ISAT): long-term follow- up. Lancet Neurol 2009; 8: 427– 33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ringer AJ, Rodriguez-Mercado R, Veznedaroglu E, et al. Defining the risk of retreatment for aneurysm recurrence or residual after initial treatment by endovascular coiling: a multicenter study. Neurosurgery 2009; 65: 311– 15 [DOI] [PubMed] [Google Scholar]
- 28. Molyneux AJ, Cekirge S, Saatci I, et al. Cerebral Aneurysm Multicenter European Onyx (CAMEO) trial: results of a prospective observational study in 20 European centers. AJNR Am J Neuroradiol 2004; 25: 39– 51 [PMC free article] [PubMed] [Google Scholar]
- 29. Cekirge HS, Saatci I, Ozturk MH, et al. Late angiographic and clinical follow-up results of 100 consecutive aneurysms treated with Onyx reconstruction: largest single center experience. Neuroradiology 2006; 48: 113– 26 [DOI] [PubMed] [Google Scholar]
- 30. Lieber BB, Sadasivan C. Endoluminal scaffolds for vascular reconstruction and exclusion of aneurysms from the cerebral circulation. Stroke 2010; 41 (10 suppl): S21– 25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wanke I, Forsting M. Stents for intracranial wide-necked aneurysms: more than mechanical protection. Neuroradiology 2008; 50: 991– 98 [DOI] [PubMed] [Google Scholar]
- 32. Mawad ME, Cekirge S, Ciceri E, et al. Endovascular treatment of giant and large intracranial aneurysms by using a combination of stent placement and liquid polymer injection. J Neurosurg 2002; 96: 474– 82 [DOI] [PubMed] [Google Scholar]
- 33. Saatci I, Cekirge HS, Ozturk MH, et al. Treatment of internal carotid artery aneurysms with a covered stent: experience in 24 patients with midterm follow-up results. AJNR Am J Neuroradiol 2004; 25: 1742– 49 [PMC free article] [PubMed] [Google Scholar]
- 34. McAuliffe W, Wycoco V, Rice H, et al. Immediate and midterm results following treatment of unruptured intracranial aneurysms with the Pipeline embolization device. AJNR Am J Neuroradiol 2012; 33: 164– 70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lubicz B, Collignon L, Raphaeli G, et al. Flow-diverter stent for the endovascular treatment of intracranial aneurysms: a prospective study in 29 patients with 34 aneurysms. Stroke 2010; 41: 2247– 53 [DOI] [PubMed] [Google Scholar]
- 36. Leonardi M, Cirillo L, Toni F, et al. Treatment of intracranial aneurysms using flow-diverting Silk stents (Balt): a single center experience. Interv Neuroradiol 2011; 17: 306– 15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Berge J, Biondi A, Machi P, et al. Flow-diverter Silk stent for the treatment of intracranial aneurysms: 1-year follow-up in a multicenter study. AJNR Am J Neuroradiol 2012; 33: 1150– 55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ferns SP, van Rooij WJ, Sluzewski M, et al. Partially thrombosed intracranial aneurysms presenting with mass effect: long-term clinical and imaging follow-up after endovascular treatment. AJNR Am J Neuroradiol 2010; 31: 1197– 205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Clarençon F, Bonneville F, Boch AL, et al. Parent artery occlusion is not obsolete in giant aneurysms of the ICA: experience with very-long-term follow-up. Neuroradiology 2011; 53: 973– 82 [DOI] [PubMed] [Google Scholar]
- 40. Gurian JH, Vinuela F, Gobin YP, et al. Aneurysm rupture after parent artery sacrifice: treatment with Guglielmi detachable coil embolization via retrograde catheterization—case report. Neurosurgery 1995; 37: 1216– 21 [DOI] [PubMed] [Google Scholar]
- 41. Singh H, Thomas J, Hoe WL, et al. Giant petrous carotid aneurysm: persistent epistaxis despite internal carotid artery ligation. J Laryngol Otol 2008; 122: e18 [DOI] [PubMed] [Google Scholar]
- 42. Shimizu H, Matsumoto Y, Tominaga T. Parent artery occlusion with bypass surgery for the treatment of internal carotid artery aneurysms: clinical and hemodynamic results. Clin Neurol Neurosurg 2010; 112: 32– 39 [DOI] [PubMed] [Google Scholar]
- 43. Niiro M, Shimozuru T, Nakamura K, et al. Long term follow-up study of patients with cavernous sinus aneurysm treated by proximal occlusion. Neurol Med Chir (Tokyo) 2000; 40: 88– 97 [DOI] [PubMed] [Google Scholar]
- 44. Briganti F, Cirillo S, Caranci F, et al. Development of “de novo” aneurysms following endovascular procedures. Neuroradiology 2002; 44: 604– 09 [DOI] [PubMed] [Google Scholar]
- 45. Lubicz B, Lefranc F, Levivier M, et al. Endovascular treatment of intracranial aneurysms with a branch arising from the sac. AJNR Am J Neuroradiol 2006; 27: 142– 47 [PMC free article] [PubMed] [Google Scholar]
- 46. Kim BM, Park SI, Kim DJ, et al. Endovascular coil embolization of aneurysms with a branch incorporated into the sac. AJNR Am J Neuroradiol 2010; 31: 145– 51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kulcsar Z, Houdart E, Bonafe A, et al. Intra-aneurysmal thrombosis as a possible cause of delayed aneurysm rupture after flow-diversion treatment. AJNR Am J Neuroradiol 2011; 32: 20– 25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Turowski B, Macht S, Kulcsar Z, et al. Early fatal hemorrhage after endovascular cerebral aneurysm treatment with a flow-diverter (Silk-stent): do we need to rethink our concepts? Neuroradiology 2011; 53: 37– 41 [DOI] [PubMed] [Google Scholar]
- 49. Cebral JR, Mut F, Raschi M, et al. Aneurysm rupture following treatment with flow-diverting stents: computational hemodynamics analysis of treatment. AJNR Am J Neuroradiol 2011; 32: 27– 33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hampton T, Walsh D, Tolias C, et al. Mural destabilization after aneurysm treatment with a flow-diverting device: a report of two cases. J Neurointerv Surg 2011; 3: 167– 71 [DOI] [PubMed] [Google Scholar]
- 51. Trager AL, Sadasivan C, Seong J, et al. Correlation between angiographic and particle image velocimetry quantifications of flow diverters in an in vitro model of elastase-induced rabbit aneurysms. J Biomech Eng 2009; 131: 034506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kulcsár Z, Ernemann U, Wetzel SG, et al. High-profile flow diverter (Silk) implantation in the basilar artery: efficacy in the treatment of aneurysms and the role of the perforators. Stroke 2010; 41: 1690– 96 [DOI] [PubMed] [Google Scholar]
- 53. Fiorella D, Hsu D, Woo HH, et al. Very late thrombosis of a Pipeline embolization device construct: Case report. Neurosurgery 2010; 67 (3 suppl operative): onsE313-14, discussion onsE314 [DOI] [PubMed] [Google Scholar]
- 54. Klisch J, Turk A, Turner R, et al. Very late thrombosis of flow-diverting constructs after the treatment of large fusiform posterior circulation aneurysms. AJNR Am J Neuroradiol 2011; 32: 627– 32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. van Rooij WJ, Sluzewski M. Perforator infarction after placement of a Pipeline flow-diverting stent for an unruptured A1 aneurysm. AJNR Am J Neuroradiol 2010; 31: E43– 44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Fiorella D, Albuquerque FC, Woo H, et al. Neuroform in-stent stenosis: incidence, natural history, and treatment strategies. Neurosurgery 2006; 59: 34– 42 [DOI] [PubMed] [Google Scholar]
- 57. Mocco J, Fargen KM, Albuquerque FC, et al. Delayed thrombosis or stenosis following Enterprise-assisted stent-coiling: is it safe? Midterm results of the interstate collaboration of Enterprise stent coiling. Neurosurgery 2011; 69: 908– 14 [DOI] [PubMed] [Google Scholar]