Abstract
Background
The emergency care of time-sensitive injuries and illnesses is increasingly recognized as an essential component of effective health care systems. However, many low- and middle-income countries (LMICs) lack healthcare providers formally trained in the care of emergency conditions. The Disease Control Priorities 3 project estimates that effective emergency care systems could avert up to half of all premature deaths in LMICs. Nigeria, a lower-middle income country of nearly 200 million people in Sub-Saharan Africa, could save approximately 100,000 lives per year with an effective emergency care system. The World Health Organization developed the Basic Emergency Care (BEC) course to train frontline healthcare workers in the management of emergency conditions in low resource settings. In this study we describe our work implementing the BEC course Nigeria.
Methods
This study was designed as a mixed methods research analysis comparing pre- and post- course examination results and surveys to evaluate participant knowledge acquisition and levels of confidence with management of various emergency conditions. Thirty-two participants were involved in the course which took place over four days at the Lagos University Teaching hospital. Quantitative data was analyzed using Stata 14.2 (College Station, TX). Paired data sets were analyzed using McNemar's chi-squared. Unpaired data sets were analyzed using a Wilcoxon signed-rank test.
Results
Post-course test scores showed significant improvement (p-value <0.001) as compared to pre-course. The average pre-course test score was 73% and average post-course score was 86.5%. Pre- and post-course questionnaires demonstrated significantly increased confidence in managing emergency conditions and agreement with course objectives.
Conclusions
The WHO Basic Emergency Care (BEC) course successfully increased the knowledge and confidence of frontline emergency care providers in Nigeria. The course was well received by participants. Future study should focus on BEC course scalability and long-term knowledge retention.
Keywords: Medical education, Basic emergency care, Short training courses, Emergency medicine in Nigeria
African relevance
-
•
This study focuses on teaching the the World Health Organization Basic Emergency Course that has been implemented in other African countries. The study looks to evaluate whether or not the short-term knowledge gains seen in other African countries are replicable in Nigeria.
-
•
This study teaches basic emergency principles to healthcare providers in a country without an emergency medicine training program. Many African countries do not have emergency medicine training programs and this study helps to evaluate the value of short courses as an introduction to emergency medicine.
Introduction
It is estimated that of the 1.6 million deaths recorded annually in Nigeria, 10-15% occur in emergency departments [1]. The Disease Control Priorities 3 project estimates that over half of all deaths in low and middle-income countries can be averted by effective emergency care delivery [2]. In Nigeria, that would translate to approximately 100,000 lives saved every year, 300 every day. Furthermore, effective emergency care also reduces the morbidity of time-sensitive illnesses and injuries [1]. The primary functions of a health system are to improve the health of the population, to respond to people’s expectations, and to provide financial protection against the costs of ill-health [3]. Basic emergency care is essential for all these functions. [4].
Effective emergency care requires a systematic approach that ensures that care is delivered in a consistently timely, organized way. There are multiple challenges to accomplishing this in low resource settings, including a lack of structural models, cost, and sustainability [2]. Like in many other countries around the world, Nigerian emergency departments are run by providers with little to no dedicated specialty training in emergency care [5]. While there are many challenges to creating a residency program, several studies have shown that supplemental training in emergency care improves provider skills and reduces the morbidity and mortality of populations in low- and middle-income countries [[6], 7., [8], 9.]. Studies show that this training ensures that patients have timely access to life-saving treatments by facilitating more efficient use of existing resources [[6], 7., [8], 9.]. However, many of the existing training courses (e.g. ATLS) are limited in scope and usually focus on one aspect of emergency care [7., [8], 9., [10], 11., 12., [13]]. Most courses are also cost prohibitive and are difficult to scale because that cannot be easily adapted for diverse audiences practicing in variable environments.
In response to requests from multiple countries and international partners for open-access, basic emergency care training materials, the World Health Organization (WHO), in collaboration with the International Committee of the Red Cross (ICRC) and the International Federation for Emergency Medicine (IFEM), developed a course for frontline emergency care providers—Basic Emergency Care: Approach to the acutely ill and injured (BEC). The BEC teaches a systematic approach to the initial assessment and management of time-sensitive conditions in which early intervention can save lives [14].
The BEC course was piloted in Uganda, United Republic of Tanzania and Zambia in partnership with the African Federation of Emergency Medicine. This pilot demonstrated a significant improvement in knowledge and confidence in managing emergency conditions among course participants [13]. In this article, we discuss our findings after implementing the BEC course in Lagos, Nigeria in partnership with the Lagos University Teaching Hospital, a 761-bed hospital in Surulere, Lagos, Nigeria.
Methods
Study design
This study was designed as a mixed-methods analysis using pre- and post - course examinations and surveys to evaluate participant knowledge acquisition after implementing the BEC course (primary objective), as well as to ascertain level of confidence and comfort with topics and skills taught in the BEC course (secondary objective).
Participants and study setting
The BEC course was conducted over four days in March 2020 at the Lagos University Teaching Hospital (LUTH) in Idi-Araba, Surulere, Lagos, Nigeria. The participants were a mix of medical students, nurses, medical officers and residents identified by local hospital leaders and the Lagos State Ministry of Health. Thirty-two participants were selected from the University of Lagos, College of Medicine, the Department of Family Medicine at LUTH, the Accident and Emergency Department at LUTH, the University College Hospital, Ibadan, and the Lagos State Ambulance Service.
Basic Emergency Care course
The BEC course is an open-access course for frontline healthcare providers who manage acute illness and injury in resource limited settings. The course is a mix of didactic lectures, small group sessions and skills stations and can be found at this site https://www.who.int/publications/i/item/basic-emergency-care-approach-to-the-acutely-ill-and-injured. To complete the course, all participants had to attend all sessions, complete all sections of their workbook, and score >75% on their post-course examination. Successful participants were awarded a certificate issued by the IFEM and the Society of Emergency Medicine Practitioners of Nigeria. The WeBelieve Foundation for Improved Medical Care, a local Nonprofit co-sponsored the course.
Data collection and analysis
Pre- and post-course closed book assessments were administered to gauge knowledge transfer to the participants over the duration of the course. Pre- and post-participation surveys were also administered to assess the level of comfort with the topics taught over the four days of the course. Surveys also elicited open-ended feedback from participants on their perceived strengths and limitations of the BEC course.
Due to the paired nature of the data, a Wilcoxon signed-rank test was used to evaluate the difference between median pre- and post- test scores. Means and 95% confidence intervals were calculated. The surveys regarding confidence with emergency care knowledge and skill areas and agreement with course objectives asked participants to rate their confidence/agreement on a likert scale of 1-4 with 4 indicating “very confident” or “strongly agree.” To analyze the survey responses, we calculated the proportion of participants who rated their confidence/agreement as a “4” prior to the course and compared it to the proportion who rated it as a “4” following the course. Since this data was paired, it was analyzed using McNemar's chi-squared for paired proportions with the exact McNemar significance probability. Counts, proportions, and 95% confidence intervals were reported. All analyses were performed using Stata 14.2 (College Station, TX). A p-value of <0.05 was considered significant.
Ethics and funding
The Institutional Review Board (IRB) at the Lagos University Teaching Hospital and at Beth Israel Deaconess Medical Center provided ethical approval for this study. Written consent was not required for this study. Funding for this study was provided by an Eleanor Miles Shore Foundation Grant at Beth Israel Deaconess Medical Center. All data was collected, stored and analyzed by representatives of the local institution.
Results
Demographics
A total of 32 participants participated in the course (Table 1). Participants were composed of twenty-two physicians, two medical students and eight nurses. Five facilitators taught the course, with a facilitator to participant ratio of 1:6.4. Four of the facilitators were emergency medicine-trained specialists, and one facilitator was a public health specialist. All facilitators were qualified as BEC course instructors and had previously completed a training of trainers course. Further information on the facilitators are as follows:
Attending Emergency Physician at Beth Israel Deaconess Medical Center, Boston, MA USA
Attending Emergency Physician at Brigham and Women’s Hospital, Boston, MA USA
Fellow in Emergency at Brigham and Women’s Hospital, Boston, MA USA
Resident Physician in Emergency Medicine at John’s Hopkin’s University, Baltimore, MD USA
Public Health Physician at the World Health Organization, Abuja Nigeria
Table 1.
BEC course participants.
| Participants (N=32) | N (%) |
|---|---|
| Resident, n (%) | 15 (47) |
| Medical officer, n (%) | 7 (22) |
| Medical student, n (%) | 2 (6) |
| Nurse, n (%) | 8 (25) |
The results were analyzed to show 2 objectives
-
1.
Primary objective – evaluate participant knowledge acquisition by analyzing pre- and post- course examination results
-
2.
Secondary objective – evaluate the change in participant confidence and comfort with topics and skills taught in the BED course by analyzing pre- and post- course surveys
Pre- and post-course test results (primary objective)
The median score on the pre-course performance test was 76% (IQR: 64%, 82%). The median score performance on the post-course assessment was significantly improved at 90% (IQR: 82%, 96%), p<0.001) (Fig. 1, Table 2). Four participants did not reach the passing goal of 75% on the post-course test and needed to retake the exam after a brief remediation session. All four participants passed the post-course performance test on retake. Only their original score, and not their score on retake, was included in the analysis.
Fig. 1.

Comparison of pre-and post-course scores.
Table 2.
Most commonly missed topics.
| Most commonly missed topics (N=32) | Pre-test N (%) | Post-test N (%) |
|---|---|---|
| Airway adjuncts: OPA/NPA indications and proper use | 23 (72%) | 10 (31%) |
| Management of shock in non-malnourished children | 21 (66%) | 9 (28%) |
| Management of opioid ingestion/overdose | 20 (63%) | |
| Initial approach: Scene safety/PPE | 19 (59%) | 8 (25%) |
| Initial ABCDE approach to the trauma patient | 15 (47%) | |
| Recognizing stridor versus wheezing | 15 (47%) | 17 (53%) |
| Clinical assessment of altered mental status: AVPU | 12 (38%) | N/A |
| Management of hemorrhagic wound | 10 (31%) | N/A |
| Recognizing pericardial tamponade | 9 (28%) | N/A |
| Recognizing heart attack | 9 (28%) | N/A |
| Management of increased intracranial pressure | 9 (28%) | N/A |
| Management of shock in malnourished children | 9 (28%) | N/A |
| Recognizing severe head injury | N/A | 12 (37%) |
| Recognizing different degrees of burn injury | N/A | 11 (34%) |
N/A represents questions NOT missed by >25% of participants.
The BEC pre-and post- course exams are composed of questions that evaluate 27 topics related to the assessment and management of the critically ill and injured (Appendix). 14 of the 27 topics evaluated on the pre-and post-course exams were missed by more than 25% (or at least 8) of the participants (Table 3). The question evaluating knowledge of airway adjuncts was most commonly missed on the pretest with 72% of participants missing this question. The most commonly missed question on the post-test evaluated participant’s ability to recognize the difference between wheezing and stridor, which was missed by 53% of participants. List 1 identifies the 4 topics, out of the total 27 topics evaluated, that were missed on both the pre-course and post-course exams by > 25% (or at least 8) participants.
Table 3.
Change in self-reported confidence with selected emergency care knowledge and skill areas. N refers to participants who felt they were ‘very confident’ with the topic.
| Pre course |
Post course |
|||||
|---|---|---|---|---|---|---|
| n (%) | CI (95%) | n (%) | CI (95%) | p-Value⁎ | ||
| A | Emergency management of the acutely ill adult | 6 (20) | 7.7%-38.6% | 20 (67) | 47.2%-82.7% | <0.001 |
| B | Emergency management of the acutely ill child | 2 (7) | 0.8%-22.1% | 12 (40) | 22.7%-59.4% | 0.002 |
| C | Emergency management of the injured adult | 10 (33) | 17.3%-52.8% | 23 (79) n=29 |
60.3%-92.0% | <0.001 |
| D | Emergency management of the injured child | 4 (13) | 3.8%-30.7% | 13 (43) | 25.5%-62.6% | 0.004 |
| E | Emergency Management of the patient with shock | 7 (23) | 9.9%-42.3% | 25 (83) | 65.3%-94.4% | <0.001 |
| F | Emergency management of the patient with altered mental status | 2 (7) | 0.8%-22.1% | 17 (57) | 37.4%-74.5% | <0.001 |
| G | Emergency management of the patient with difficulty in breathing | 3 (10) | 2.1%-26.5% | 17 (57) | 37.4%-74.5% | <0.001 |
| H | Understanding of emergency drugs | 1 (3) | 0.1%-17.2% | 17 (57) | 37.4%-74.5% | <0.001 |
| I | Have skills to manage an obstructed (blocked airway) | 1 (3) | 0.1%-17.2% | 16 (55) n=29 |
35.7%-73.6% | <0.001 |
| J | Have skills to manage a patient with difficulty in breathing | 1 (3) | 0.1%-17.2% | 20 (67) | 47.2%-82.7% | <0.001 |
| K | Have skills to manage a patient with bleeding problems | 3 (10) | 2.1%-26.5% | 25 (83) | 65.3%-94.4% | <0.001 |
| L | Have the skills to immobilize patients | 3 (11) n=28 |
2.2%-28.2% | 23 (77) | 57.7%-90.1% | <0.001 |
Used McNemar's chi-squared for paired proportions with the Exact McNemar significance probability
List 1.
Missed topics on both pre-and post-course test.
| Airway adjuncts: OPA/NPA indications and proper use Management of shock in non-malnourished children Initial approach: Scene safety/PPE Recognizing stridor versus wheezing |
Survey results (secondary objective)
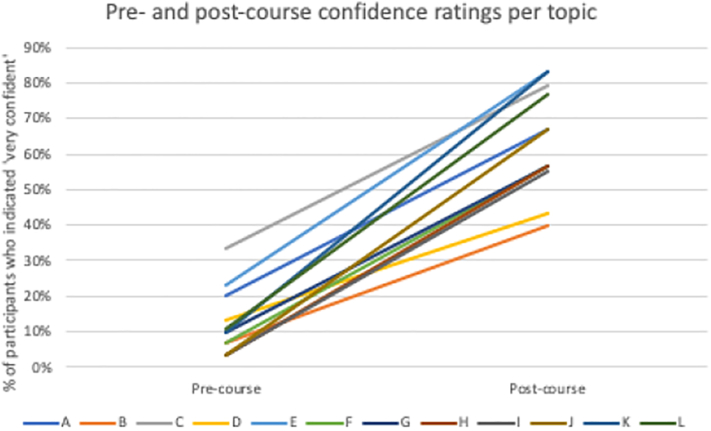
Participants’ confidence levels in key emergency care areas were also surveyed. Table 3 and Fig. 2 show the difference in the number of participants who felt that they were ‘very confident’ in evaluating the given topic before and after the course. All areas showed a statistically significant improvement in the confidence levels.
Fig. 2.
Change in self-reported confidence with selected emergency care knowledge and skill areas.
Participants were also surveyed about their level of comfort with managing patients in emergency situations. Table 4 and Fig. 3 show the difference in the number of participants who ‘strongly agreed’ with the statements before and after the course. All areas showed a statistically significant improvement.
Table 4.
Participant agreement with meeting course objectives.
| Pre Course |
Post Course |
|||||
|---|---|---|---|---|---|---|
| n (%) | CI (95%) | n (%) | CI (95%) | p-value⁎⁎ | ||
| A | I feel comfortable handling any patient requiring emergency care | 7 (23) | 9.9%-42.3% | 20 (69) N=29 |
49.2%-84.7% | <0.001 |
| B | I feel prepared to see emergency care patients in my clinical setting | 6 (21) N=29 |
8.0%-39.7% | 17 (57) | 37.4%-74.5% | 0.001 |
| C | I feel confident seeing very ill patients | 4 (14) N=28 |
4.0%-32.7% | 15 (52) N=29 |
32.5%-70.6% | 0.001 |
| D | I feel that I understand ABCDE's of basic emergency care | 6 (21) N=29 |
8.0%-39.7% | 26 (90) N=29 |
72.6%-97.8% | <0.001 |
| E | I feel like I have an organized approach that allows me to be prepared for all emergency care patients | 2 (7) | 0.8%-22.1% | 24 (80) | 61.4%-92.3% | <0.001 |
Used McNemar's chi-squared for paired proportions with the Exact McNemar significance probability.
Fig. 3.
Participant agreement with meeting course objectives.
The survey elicited feedback on the effectiveness of the course facilitators. Overall, the majority (29 out of 32 respondents, or 91%) rated the course instructors as “excellent.” The remaining three respondents rated the course instructors as “good.” Course participants also answered open-ended questions about their perceived strengths and opportunities for improvement. Representative quotes from participants to these questions are captured in Table 5.
Table 5.
Perceived strengths and limitations of the BEC course.
| What specific things did you like about the course? | “Quality of instructors, practical, hands on skills, repetition to solidify knowledge.” “Large information compressed into simple terms.” “Appropriate for Nigeria, good timing, good meals, great feedback sessions, excellent skills stations.” “Makes you save lives with limited resources, practical skills.” “Simplicity of the course, great workbook, wonderful facilitators.” “In depth knowledge concerning the management of critically ill and injured patients, great facilitators.” “Great and effective way of learning using the practical approach, small groups, interactive class.” |
| What would you change about the course? | “Include more skills sessions.” “Trainers should familiarize themselves with examples peculiar to place of training.” “Longer course duration to enable facilitators to go deeper into the integral aspects of the management of critically ill and injured patients.” “BLS and ATLS training should be included if possible.” “Time management.” |
Discussion
The administration of the WHO BEC course in Nigeria resulted in demonstrable knowledge gain as evidenced by the significant increase in pre- and post- course scores. Participants also reported that their enrollment in the course improved their level of comfort with the management of acutely ill patients.
Although there were improvements in the performance of the cohort across all topics covered during the course, there were four topics that were answered incorrectly by a substantial number of participants in the pre- and post- course assessments. Greater than 25% of our cohort did not enter correct answers on questions that tested their knowledge on scene safety and the use of PPE, airway adjuncts, recognizing respiratory sounds, and managing shock in a non-malnourished child.
Airway adjuncts discussed in the BEC course include nasopharyngeal airways (NPAs) and oropharyngeal airways (OPAs). Although recognizing these instruments from other formally taught courses such as Basic Life Support (BLS), many participants noted not having them in their clinical environment which may contribute to their misunderstanding of the indications for when to utilize an airway adjunct. Working with local providers and their supply chain to include these essential instruments in emergency clinical environments would improve provider understanding and use of airway adjuncts. It is also important that we work to incorporate supplies that are available locally in teaching the skills sessions for future iterations of the course. Adequate PPE is another valuable resource that is not always readily available in many resource-limited settings and might explain the performance of our cohort on this topic. Finally, all our participants tended primarily to adult populations and this might explain the test results on the topic of management of shock in a non-malnourished child. This data helps us identify topics that should be emphasized during future iterations of the BEC course in Nigeria, perhaps through content-specific didactics and/or additional skills stations.
Overall, the goal of the BEC course is to provide relevant teachings on the care of emergencies in resource-limited settings (12). Upon concluding our BEC course, the majority of participants endorsed comfort handling patients requiring emergent care; feeling prepared and confident in the evaluation of ill patients in a clinical setting; and applying an organized approach to the emergency patient seeking care. The participants provided positive feedback on the quality of the course instructors and the strengths of the BEC course. Additionally, participants presented useful recommendations for improving upon the limitations of the course. At the end of the course, 15 participants completed a training of trainers course, with the hope that they will in turn train others in Nigeria. Overall, the course met its goals and the expectations of Nigerian providers.
There are a number of important limitations to our study. First, participants in the course lived and worked primarily in the geographic areas surrounding Lagos and Ibadan which may limit the applicability of our results to other geographic areas in Nigeria. Second, four of the five instructors who taught the course had specialty training in Emergency Medicine. We postulate that the specialty training in Emergency Medicine may have enhanced the learning environment and led to higher post-test scores. Considering that there are few residency trained Emergency Physicians in Nigeria, future BEC courses in Nigeria may not produce similar results. In addition, an instructor/student ration of 1:6 was used, which allowed for more interaction between the instructors and participants particularly during the small groups and at the skill stations. This ratio may not be feasible in future iterations of the course. Also, the BEC course instructors administered the course evaluations which may have biased the results.
Finally, the implementation of this course misses out on the evaluation of 2 key areas – long-term knowledge retention and impact on clinical care/outcomes. Our plan for future courses is to focus on more specific topics such as trauma, and sepsis, especially those which have a systematic approach to management and standardized best practices. In this situation, we will be able to study adherence to certain clinical guidelines pre- and post- course and measure changes in patient mortality.
Nonetheless, we believe that the BEC course is effective in increasing short term knowledge, skills and confidence in the care of emergencies in resource-limited settings. Whether the course leads to long term retention of knowledge skills, or improvement in clinical outcomes is an important subject of future study.
Conclusion
To our knowledge, this is the first implementation of the BEC course in Nigeria, the most populous country in Africa. The course was well received by participants and significant improvement was found in all outcome measures. Future work should focus on training local trainers to lead additional implementations and incorporating the principles of the BEC course into the clinical care of patients in Nigeria. Additional assessments should evaluate the impact of BEC training on clinical outcomes. If successfully scaled, the BEC course has the potential to improve the knowledge and skills of Nigerian healthcare providers and significantly improve the care of acutely ill and injured patients in Nigeria.
CRediT authorship contribution statement
Authors contributed as follow to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: AO contributed 30%; AU and SK15% each; and CA, BA, JS and BA 10% each. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of competing interest
The authors declared no conflict of interest
Acknowledgments
Acknowledgments
We would like to thank Dr. Andi Tenner for her help facilitating formal issuance of the course through the International Federation for Emergency Medicine (IFEM). We would like to thank Dr. Efunbo Dosekun, with the Society of Emergency Medicine Practitioners of Nigeria (SEMPON), for certifying the course and maintaining the in-country records of current and future participants of the course. We would also like to thank Professor W. Adeyemo, the Chairman, Medical Advisory Committee at LUTH, and Professor Bode, the Chief Medical Director at LUTH for their support of this course, a key first step to improving knowledge for the care of the ill and injured in the country.
Funding
Beth Israel Deaconess, Department of Emergency Medicine Eleanor and Miles Shore Grant.
Dissemination of results
Results from this study were shared in an informal manner with the leadership and staff members at the data collection site – Lagos University Teaching Hospital.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.afjem.2021.02.004.
Appendix. Supplementary data
Supplementary material.
References
- 1.Obermeyer Z., Abujaber S., Makar M., Stoll S., Kayden S.R., Wallis L.A. Emergency care in 59 low- and middle-income countries: a systematic review. Bull World Health Organ. 2015;93(8):577–586G. doi: 10.2471/BLT.14.148338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.T. Reynolds, H. Sawe, A. Rubiano, et al. “Strengthening health systems to provide emergency care” In: Disease control priorities (third edition): Volume 9, Disease Control Priorities.
- 3.World Health Organization . World Health Organization; Geneva: 2000. The world health report 2000 – health systems: improving performance. [Google Scholar]
- 4.Razzak J.A., Kellermann A.L. Emergency medical care in developing countries: is it worthwhile? Bull World Health Organ. 2002;80(11):900–905. PMID: 12481213. [PMC free article] [PubMed] [Google Scholar]
- 5.DaCosta A., Osonuga A., Adesegun O. The urgent need for postgraduate medical training in emergency medicine in Nigeria. Afr J Emerg Med. 2020;10(1):1–2. doi: 10.1016/j.afjem.2019.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meaney P.A., Sutton R.M., Tsima B., Steenhoff A.P., Shilkofski N., Boulet J.R. Training hospital provid- ers in basic CPR skills in Botswana: acquisition, retention and impact of novel training techniques. Resuscitation. 2012;83(12):1484–1490. doi: 10.1016/j.resuscitation.2012.04.014. Dec. 22561463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arreola-Risa C, Vargas J, Contreras I, Mock C. Effect of emergency medical technician certification for all prehospital personnel in a Latin American city. J Trauma. 2007 Oct; 63(4):914–9. doi:10.1097/TA.0b013e31806bf141 PMID: 18090026. [DOI] [PubMed]
- 8.Null Zaeem-ul-Haq, Qureshi F., Hafeez A., Zafar S., Mohamud B.K., Southal D.P. Evidence for improve- ment in the quality of care given during emergencies in pregnancy, infancy and childhood following training in life-saving skills: a postal survey. JPMA J Pak Med Assoc. 2009 Jan;59(1):22–26. PMID: 19213372. [PubMed] [Google Scholar]
- 9.Mock CN, Tiska M, Adu-Ampofo M, Boakye G. Improvements in prehospital trauma care in an African country with no formal emergency medical services. J Trauma. 2002 Jul; 53(1):90–7. doi:10. 1097/00005373-200207000-00018 PMID: 12131396. [DOI] [PubMed]
- 10.Spiwak R., Lett R., Rwanyuma L., Logsetty S. Creation of a standardized burn course for low income countries: meeting local needs. Burns. 2014;40(7):1292–1299. doi: 10.1016/j.burns.2014.01.007. Nov 1. 24685348. [DOI] [PubMed] [Google Scholar]
- 11.Brennan MM, Fitzpatrick JJ, McNulty SR, Campo T, Welbeck J, Barnes G. Paediatric resuscitation for nurses working in Ghana: an educational intervention. Int Nurs Rev 2013 Mar 1; 60(1):136–43. doi:10.1111/j.1466-7657.2012.01033.x PMID: 23406249. [DOI] [PubMed]
- 12.Mirkuzie AH, Sisay MM, Bedane MM. Standard basic emergency obstetric and neonatal care training in Addis Ababa; trainees reaction and knowledge acquisition. BMC Med Educ. 2014 Sep 24; 14:201. doi: 10.1186/1472-6920-14-201 PMID: 25248410. [DOI] [PMC free article] [PubMed]
- 13.Tenner A.G., Sawe H.R., Amato S., Kalanzi J., Kafwamfwa M., Geduld H. Results from a World Health Organization pilot of the Basic Emergency Care course in sub Saharan Africa. PLoS One. 2019;14(11) doi: 10.1371/journal.pone.0224257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization . World Health Organization; 2018. BASIC EMERGENCY CARE: approach to the acutely ill and injured. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material.